BGDA Practical 12 - Abnormalities
| Practical 12: Embryo to Fetus | Second Trimester | Third Trimester | Birth | Neonatal | Abnormalities |
Introduction
Prenatal diagnosis are the clinical tools used to determine both normal and abnormal development. There are a growing number of both prenatal and neonatal clinical screening methods for many disorders of development.
Chromosomal Anomalies
The 2018 Australian Clinical Practice Guidelines - Pregnancy Care[1] recommends a combined first trimester test comprising:
- ultrasound measurement of fetal nuchal translucency thickness between 11 weeks and 13 weeks 6 days gestation (when the fetus has a crown-rump length of 45–84 mm) combined with
- maternal plasma testing of pregnancy-associated placental protein-A (PAPP-A) and free beta-human chorionic gonadotrophin (b-hCG) between 9 weeks and 13 weeks, 6 days gestation.
Statistics - Top Ten
The ten most frequently reported birth defects in Victoria between 2003-2004 (More? Australian Statistics)
- hypospadias
- Obstructive Defects of the Renal Pelvis or Obstructive Genitourinary Defects
- ventricular septal defect
- developmental hip dysplasia
- Trisomy 21 or Down syndrome
- hydrocephalus
- cleft palate
- Trisomy 18 or Edward Syndrome - multiple abnormalities of the heart, diaphragm, lungs, kidneys, ureters and palate 86% discontinued.
- Renal Agenesis/Dysgenesis - reduction in neonatal death and stillbirth since 1993 may be due to the more severe cases being identified in utero and being represented amongst the increased proportion of terminations (approximately 31%).
- Cleft Lip and Palate - occur with another defect in 33.7% of cases.
| Male External | Palate and Lip | Palate Formation |
Abnormalities Interactive Component
| Attempt the Quiz - Abnormalities | ||
|---|---|---|

Here are a few simple Quiz questions that relate to Abnormalities from the practical.
|
| Practical 12: Embryo to Fetus | Second Trimester | Third Trimester | Birth | Neonatal | Abnormalities |
Additional Information
| Additional Information - Content shown under this heading is not part of the material covered in this class. It is provided for those students who would like to know about some concepts or current research in topics related to the current class page. |
Genetic
The Royal Hospital for Women (2014) Trisomy 21 Screening, Including Non-Invasive Prenatal Testing (Nipt) PDF
NSW - Congenital Conditions Register
Scheduled congenital conditions (section 2) detected during pregnancy or in infants up to one year of age in NSW are required to be reported under the NSW Public Health Act 1991.
Scheduled congenital conditions include:
- All structural malformations. Examples include spina bifida, microcephaly, transposition of the great vessels, ventricular septal defects, pulmonary agenesis, polycystic lungs, duodenal atresia, exomphalos, hypospadias, cleft lip/palate, microphthalmia, limb reductions, polydactyly, birthmarks greater than 4 cms diameter, cystic hygroma and multisystem syndromes including at least one structural malformation.
- Chromosomal abnormalities. Examples include Down syndrome and unbalanced translocations.
- Four medical conditions: cystic fibrosis, phenylketonuria, congenital hypothyroidism and thalassaemia major.
Congenital conditions that are not notifiable include:
- Minor anomalies occurring in isolation (Examples of minor anomalies include skin tags, deviated nasal septum, tongue tie, benign heart murmurs, clicky non-dislocating hips, sacral dimples, positional talipes, abnormal palmar creases, dysmorphic features).
- Birth injuries.
- Congenital infections which do not result in a structural malformation.
- Tumours and cysts.
- Conditions arising from prematurity or asphyxiation.
Links: NSW Health - Congenital Conditions Register - Reporting Requirements 2012 | PDF
Environmental
While genetic abnormalities will have well-defined impacts upon development, environmentally derived effects can be harder to define and often variable depending on many different factors (timing, exposure level, and the combination effects with other factors). This combination effect can also be seen between genetic and environmental interacting to give an even broader spectrum of both major and minor abnormalities.
Monitoring the health impacts of mandatory folic acid and iodine fortification 2016
Decrease in neural tube defects since folic acid added to bread[2]
|
Folic acid and iodine fortification (2016) |
| USA Statistics | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| European Statistics | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Links: abnormal development
The links below are to more detailed information about some of the current prenatal diagnostic techniques and their applications.
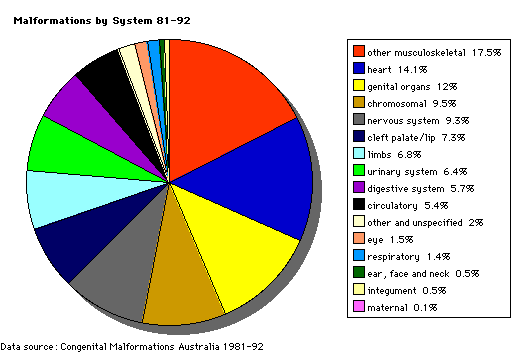
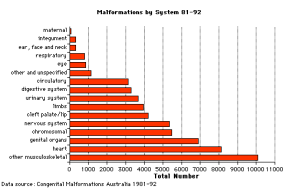
Australian Congenital Anomalies Monitoring System
The following text is from AIHW National Perinatal Epidemiology and Statistics Unit Australian Congenital Anomalies Monitoring System (ACAMS)
- "The Australian Congenital Anomalies Monitoring System (ACAMS) contains data based on notifications of major congenital anomalies to birth defects registers in New South Wales, Victoria, Western Australia and South Australia and on data collected on congenital anomalies in Queensland, Tasmania and the Australian Capital Territory. The Northern Territory is currently unable to provide data in a format enabling it to be compiled with data from the other states and territories. Some summary data have been provided by the Northern Territory for inclusion in the ACAS. Congenital anomalies are mainly notified from data collected as part of perinatal collections. Other sources of data include perinatal death certificates, cytogenetic or pathology reports, admitted patient data, maternal and child health nurses and medical officers.
- Information is included on live births and stillbirths of 20 weeks gestational age or more or 400 grams birthweight or more (including induced abortions) with a congenital anomaly for all states and the Australian Capital Territory. Information on induced abortions of less than 20 weeks gestational age and less than 400 grams weight with a congenital anomaly is only available for four states and is included for: New South Wales, Victoria, Western Australia and South Australia. Births included in the ACAS are also included in the National Perinatal Data Collection.
- The period of notification varies among the state and territory collections and ranges from prenatal diagnosis to notification up to 15 years of age. For New South Wales, the data include births with congenital anomalies notified up to 1 year of age. The data for Victoria, Western Australia and South Australia include births with congenital anomalies notified up to 15 years, 6 years and 5 years of age respectively. The data for Queensland, Tasmania, and the Australia Capital Territory include births with congenital anomalies notified in the perinatal period.
- Data items relating to the woman, including demographic characteristics and factors relating to the birth, and data items relating to the baby, including, birthweight, gestational age and sex, are included. Congenital anomalies are coded using the British Paediatric Association Classification of Diseases (ICD-9-BPA), which is based on the International Classification of Diseases, 9th Revision (ICD-9).
- ACAS supersedes the National Congenital Malformations and Birth Defects Data Collection (NCM&BD), which commenced in 1981 in response to claims of increased incidence of congenital anomalies in small areas of Australia. Data were provided by four jurisdictions in 1998–1985 and all states and territories provided data from 1986. Data are included up to and including the 1997 birth cohort. The NCM&BD data collection was reviewed in 2004 and the development of the ACAS was a recommendation of the review."
| Previous - Australian Birth Anomalies System |
|---|
(Modified from Australian Institute of Health and Welfare (AIHW)) |
Congenital Anomalies in Australia 2002-2003
- Links: Australian Congenital Anomalies Monitoring System (ACAMS) | Australian Institute of Health and Welfare (AIHW)
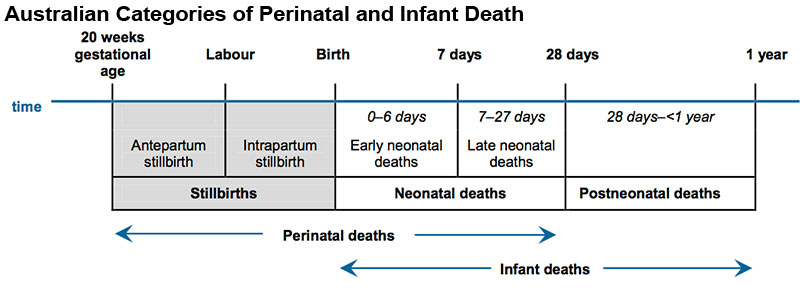
Perinatal and Infant Death
|
| Australian Categories of Perinatal and Infant Death[3] |
References
- ↑ Department of Health (2018) Clinical Practice Guidelines: Pregnancy Care. Canberra: Australian Government Department of Health. (5 June 2019)
- ↑ AIHW 2016. Monitoring the health impacts of mandatory folic acid and iodine fortification 2016. Cat. no. PHE 208. Canberra: AIHW. PDF
- ↑ AIHW: Hilder L, Li Z, Zeki R & Sullivan EA 2014. Stillbirths in Australia 1991-2009. Perinatal statistics series no. 29. Cat. no. PER 63. Canberra: AIHW.
BGDA: Lecture 1 | Lecture 2 | Practical 3 | Practical 6 | Practical 12 | Lecture Neural | Practical 14 | Histology Support - Female | Male | Tutorial
Glossary Links
- Glossary: A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | Numbers | Symbols | Term Link
Cite this page: Hill, M.A. (2026, March 1) Embryology BGDA Practical 12 - Abnormalities. Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/BGDA_Practical_12_-_Abnormalities
- © Dr Mark Hill 2026, UNSW Embryology ISBN: 978 0 7334 2609 4 - UNSW CRICOS Provider Code No. 00098G