Lecture - Placenta Development
| Embryology - 28 Apr 2024 |
|---|
| Google Translate - select your language from the list shown below (this will open a new external page) |
|
العربية | català | 中文 | 中國傳統的 | français | Deutsche | עִברִית | हिंदी | bahasa Indonesia | italiano | 日本語 | 한국어 | မြန်မာ | Pilipino | Polskie | português | ਪੰਜਾਬੀ ਦੇ | Română | русский | Español | Swahili | Svensk | ไทย | Türkçe | اردو | ייִדיש | Tiếng Việt These external translations are automated and may not be accurate. (More? About Translations) |
Introduction
This lecture is an introduction to the development and functions of the placenta.
The placenta (Greek, plakuos = flat cake) named on the basis of this organs appearance. The placenta a mateno-fetal organ which begins developing at implantation of the blastocyst and is delivered with the fetus at birth. Only recently have we begun to understand the many different functions this organ carries out in addition to its role in embryonic nutrition.
If you have time after working through this online lecture page, have a look at the Medicine practical class, 7 pages the students work through in 2 hours.
The placenta and placental blood at birth has recently been seen as a new source for stem cells in bone marrow replacement therapy in many diseases. The topic of stem cells will be covered later in this current course.
Lecture Objectives
- Understanding of placental villi development
- Understanding of placental structure
- Understanding of placental functions
- Brief understanding of placental abnormalities
Lecture Resources
| Movies | |||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
| ||||||||||||||||||
| 2016 Lecture Video Recording |
|---|
| This 2016 lecture video recording may differ from the the current 2018 online lecture. |
| <html5media height="600" width="820">File:2016Lecture-Placenta.mp4</html5media> Click Here to play on mobile device |
Nutrition
- Histiotrophic - describes the intital transfer of nutrition from maternal to embryo.
- occurs before implantation and during early implantation mainly from uterine glands.
- Haemotrophic - describes the later blood-borne nutrition.
- occurs in the embryonic and fetal period after placenta development.
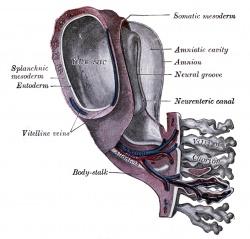
Fetal Membranes
Villi Stages
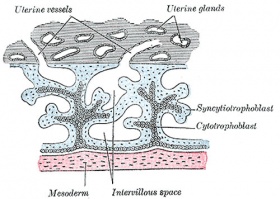
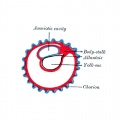
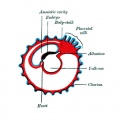
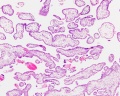
Primary villi Week 2 - first stage of chorionic villi development, trophoblastic shell cells (syncitiotrophoblasts and cytotrophoblasts) form finger-like extensions into maternal decidua. |
Secondary villi Week 3 - second stage of chorionic villi development, extraembryonic mesoderm grows into villi, covers entire surface of chorionic sac. |
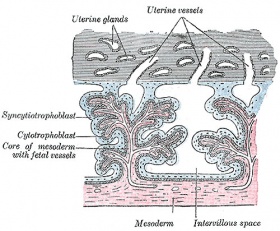
Tertiary villi Week 4 - third stage of chorionic villi development, mesenchyme differentiates into blood vessels and cells, forms arteriocapillary network, fuse with placental vessels, developing in connecting stalk. Basal region will form chorionic plate. |
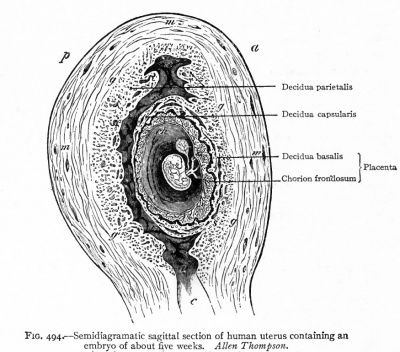
Chorionoic Villi Location
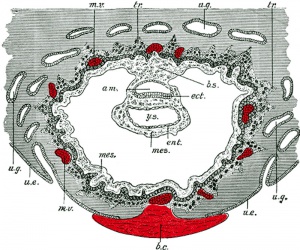
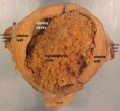
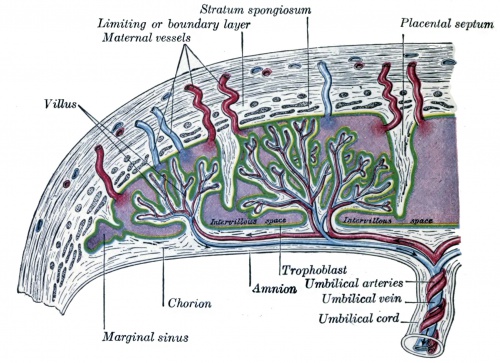
Historic - Semi-diagramatic sagittal section of human uterus containing an embryo. Note the villi locations and the names for different maternal decidual regions.
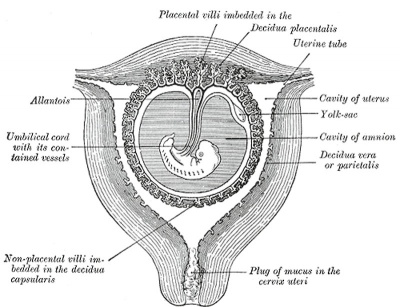
|
|
Originally cover entire chorionic surface and become restricted to decidua basalis region forming 2 regions:
| Week 4 - Carnegie stage 11 | |||||||
|---|---|---|---|---|---|---|---|
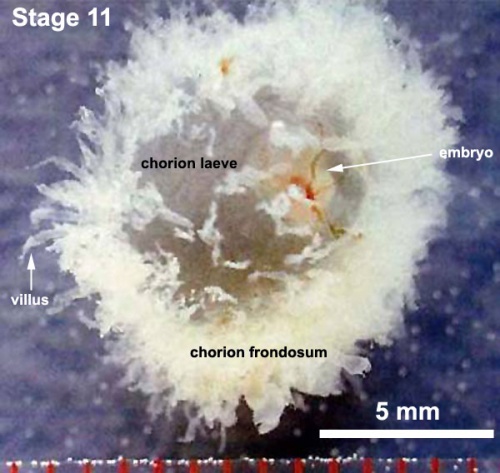
| |||||||
| Week 5 - Carnegie stage 14 | |||||||
|
| ||||||
| Week 7 - Carnegie stage 18) | |||||||

|
Villi Terms
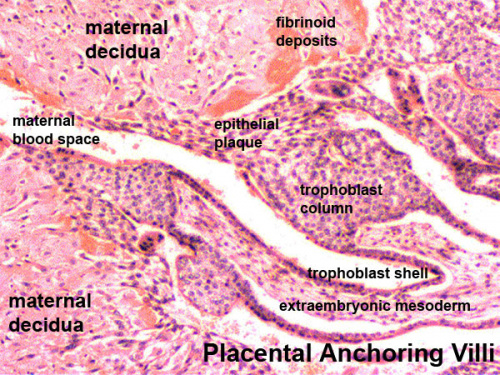
- primary villi - week 2, first stage of chorionic villi development, trophoblastic shell cells (syncitiotrophoblasts and cytotrophoblasts) form finger-like extensions into maternal decidua.
- secondary villi - week 3, second stage of chorionic villi development, extraembryonic mesoderm grows into villi, covers entire surface of chorionic sac.
- tertiary villi third stage of chorionic villi development, mesenchyme differentiates into blood vessels and cells, forms arteriocapillary network, fuse with placental vessels, developing in connecting stalk
- stem villi - or anchoring villi, cytotrophoblast cells attached to maternal tissue.
- branched villi - or terminal villi, grow from sides of stem villi, region of main exchange, surrounded by maternal blood in intervillous spaces.
- terminal villi - not active outgrowths caused by proliferation of the trophoblast. Passive protrusions induced by capillary coiling due to growth of the fetal capillaries within the mature intermediate villi (third trimester).
- chorionic plate - region of membrane at the base of the villi through which placental arteries and vein passes.
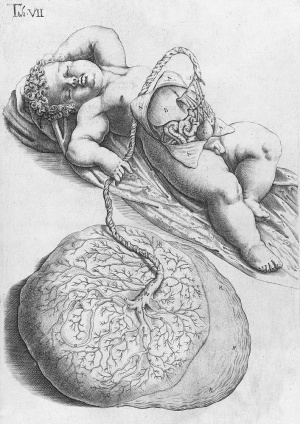
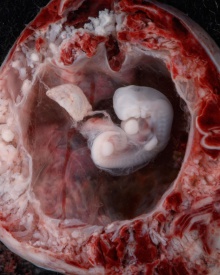
Placenta at Birth
- Placenta (Greek, plakuos = flat cake)
- embryonic/maternal organ
- villous chorion/decidua basalis
- continuous with amniotic and chorionic sacks
Dimensions
- at birth - discoid up to 20cm diameter and 3 cm thick (term) and weighs 500-600 gm
- Shapes - accessory placenta, bidiscoid, diffuse, horseshoe
- maternal and embryonic surface, both delivered at parturition
- retention may cause uterine hemorrhage

| |
| Fetal Surface | Maternal Surface |
|---|---|
|
|
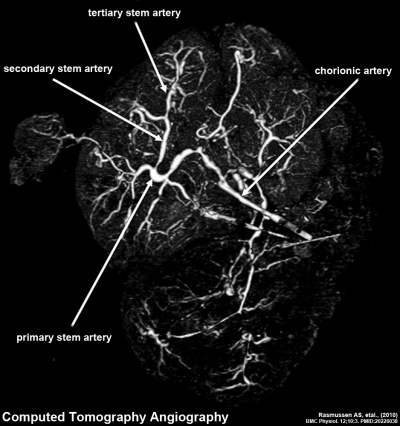
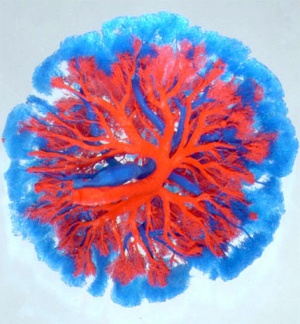
CT term placental blood vessels showing branching pattern of placental artery.
Placental Classification
Classification of placenta is on the basis of histological (microscopic) structural organization and layers between fetal and maternal circulation, giving 3 main groups:
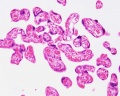
- Haemochorial - placenta where the chorion comes in direct contact with maternal blood (human)
- Endotheliochorial - maternal endometrial blood vessels are bare to their endothelium and these comes in contact with the chorion. (dogs, cats)
- Epitheliochorial - maternal epithelium of the uterus comes in contact with the chorion.considered as primitive (pigs, cows)
The presence of these three differing types of placenta have also been used to describe the pattern mammalian evolution. See also Placental Layers
Haemochorial human placenta
Placental Types
- Discoid in humans, mouse, insectivores, rabbit, rat, and monkeys.
- Zonary in dog, cat, bears and seals.
- Cotyledenary in cow, deer, goat, and giraffe.
- Diffuse in horse, pig, camels, lemurs, opossums, kangaroo, and whales
- Links: Comparative Placentation
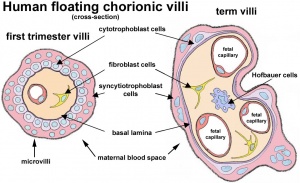
Chorionoic Villi Trimester Development
- Trimester 1 and 2 - immature intermediate villi, developmental steps towards the stem villi.
- Trimester 3 - mature intermediate villi develop during the last trimester, produce numerous terminal villi.
- Terminal villi are not active outgrowths caused by trophoblast proliferation, passive protrusions induced by capillary coiling due to excessive longitudinal growth of the fetal capillaries within the mature intermediate villi.
- Capillary bed arrangement in the terminal villi can vary from simple U-like loops to branched network, due to capillary elongation and sprouting. (Data from[1])
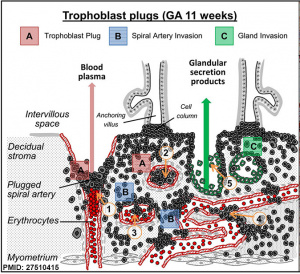
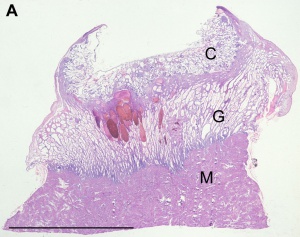
First trimester spiral artery trophoblast plug.[2] |
|
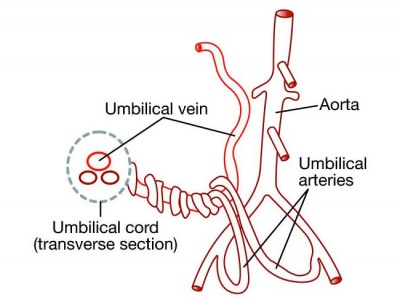
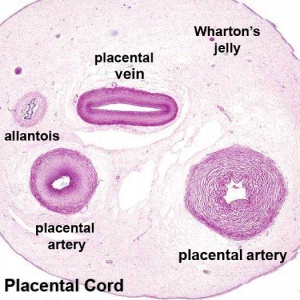
Placental Cord Blood Vessels
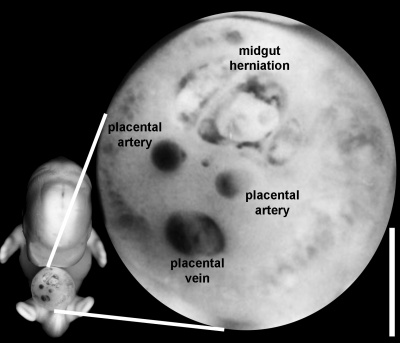
|
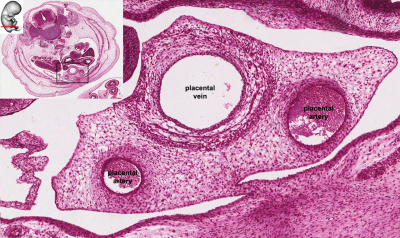
|
| Week 6 Umbilicus containing initial placental cord. | Week 8 Embryo showing the placental blood vessels within the ventral body wall. |
|
|
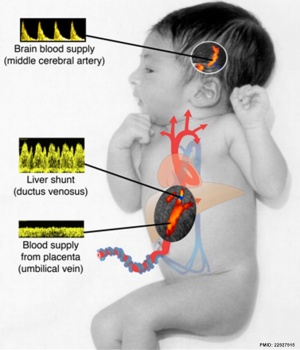
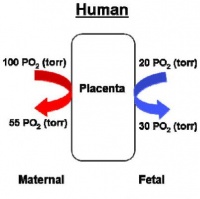
Placental Function
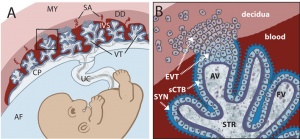
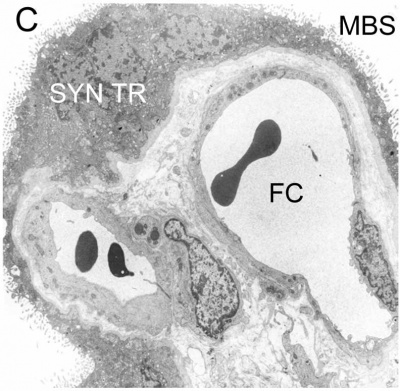
- 4 layers separate maternal and fetal blood: syncitiotrophoblast, cytotrophoblast, villi connective tissue and fetal capillary endothelium
- 3 main functions: metabolism, transport and endocrine
Placental Metabolism
Synthesizes: glycogen, cholesterol, fatty acids
- provides nutrient and energy
Placental Transport
gases and nutrition
- oxygen, carbon dioxide, carbon monoxide
- water, glucose, vitamins
- hormones, mainly steroid not protein
- electrolytes
- maternal antibodies
- waste products - urea, uric acid, bilirubin
- drugs and their metabolites (fetal drug addiction)
- infectious agents (cytomegalovirus, rubella, measles, microorganisms)
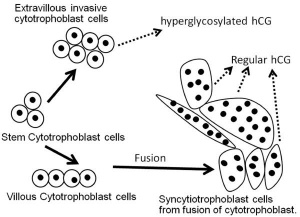
Placental Endocrine
- Human chorionic gonadotrophin (hCG) - like leutenizing hormone, supports corpus luteum
- Human chorionic somatommotropin (hCS) (or placental lactogen) - hormone level increases in maternal blood through pregnancy, decreases maternal insulin sensitivity (raising maternal blood glucose levels and decreasing maternal glucose utilization) aiding fetal nutrition ("anti-insulin" function)
- Human chorionic thyrotropin (hCT) - Peptide placental hormone, similar to anterior pituitary released thyroid stimulating hormone (TSH), which along with human chorionic gonadotrophin (hCG) is thought to act on maternal thyroid. There is little recent research published on this hormone, its level and activities.
- Human chorionic corticotropin (hCACTH) - placental hormone thought to have corticotropin (ACTH)-like activity, increasing maternal cortisol levels.
- Steroid Hormones
- progestins - progesterone, support of the endometrium and suppress uterine smooth muscle contractility.
- estrogens - estriol, stimulate growth of the myometrium and mammary gland development.
- both hormones support maternal endometrium
- Relaxin - Humans high levels early in pregnancy than at birth promotes angiogenesis probably plays a role in development of the uterus/ placenta than in the birth process
Fetal Placenta
Trophoblast cells are the major source of placental hormones.
Placental growth hormone (PGH) is mainly expressed in the syncytiotrophoblast cells (PGH differs from pituitary derived growth hormone by 13 amino acids). extravillous cytotrophoblast - arise from anchoring villi invade the uterine spiral arteries, generating fibrinoid material and endovascular trophoblastic cells. syncytiotrophoblast
Fetal Blood Vessels At least 2 phases of development during pregnancy driven by vascular endothelial growth factor (VEGF):
- Initially cytotrophoblasts are the cellular stimulus to vasculogenesis and angiogenesis.
- Later Hofbauer (lacental villi macrophages of mesenchymal origin) and stromal cells take over the stimulation of blood vessel development.
Placenta Human chorionic gonadotrophin (hCG) After implantation cells within the developing placenta (syncitiotrophoblasts) synthesize and secrete Human chorionic gonadotrophin (hCG) into the maternal bloodstream. The main function of serum hCG is to maintain the corpus luteum in the maternal ovary and therefore maintain the early pregnancy, that is block the menstrual cycle. Later the placenta itself supports the pregnancy.
Maternal Placenta
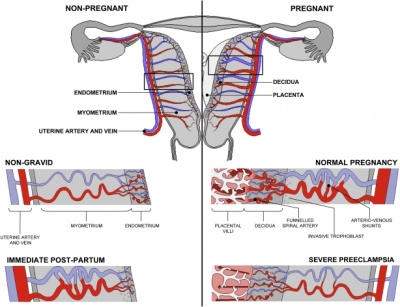
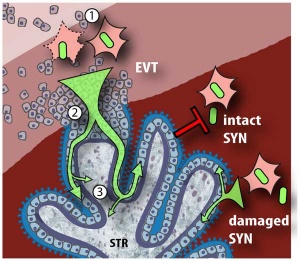
|
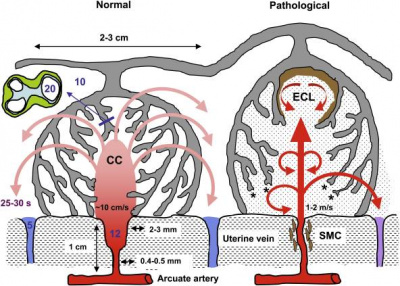
|
| Uterine and placental vasculature | Placenta spiral artery conversion |
Fibrinoid - said to exist as 2 forms of extracellular matrix:
- Fibrin-type fibrinoid is a maternal blood-clot product which replaces degenerative syncytiotrophoblast
- Matrix-type fibrinoid is secreted by invasive extravillous trophoblast cells.
Fibrinoid layer (Nitabuch's layer) is thought to act to prevent excessively deep implantation.
| Decidualization
Process of endometrial stromal cells (fibroblast-like) change in morphology (polygonal cells) and protein expression and secretion (specific decidual proteins: prolactin, insulin-like growth factor binding protein-1, tissue factor, interleukin-15, and VEGF).
|
|
Artery Dilatation - due to extravillous trophoblast cells invading uterine wall and maternal spiral arteries replacing both smooth muscle with fibrinoid material and part of vessel endothelium. There is also a proliferation of maternal blood vessels.
Other changes
- Endoreplication - rounds of nuclear DNA replication without intervening cell or nuclear division (mitosis).
- Cytokines - of maternal origin also act on placental development.
- Natural Killer (NK) cells - 30% of all the decidual cells towards the end of the first trimester of pregnancy. These lymphocytes are present in the maternal decidua in large numbers (70%, normal circulating blood lymphocytes 15%) close to the extravillous trophoblast cells. Have a cytolytic potential against virus-infected and tumor-transformed cells.
- ↑ Castellucci M, Scheper M, Scheffen I, Celona A & Kaufmann P. (1990). The development of the human placental villous tree. Anat. Embryol. , 181, 117-28. PMID: 2327595
- ↑ Weiss G, Sundl M, Glasner A, Huppertz B & Moser G. (2016). The trophoblast plug during early pregnancy: a deeper insight. Histochem. Cell Biol. , 146, 749-756. PMID: 27510415 DOI.
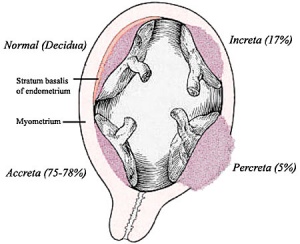
Placental Abnormalities
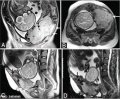
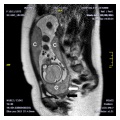
- Placenta Accreta - abnormal adherence, with absence of decidua basalis. The incidence of placenta accreta also significantly increases in women with previous cesarean section compared to those without a prior surgical delivery.
- Placenta Increta - occurs when the placenta attaches deep into the uterine wall and penetrates into the uterine muscle, but does not penetrate the uterine serosa. Placenta increta accounts for approximately 15-17% of all cases.
- Placenta Percreta - placental villi penetrate myometrium and through to uterine serosa.
- Placenta Previa - In this placenatal abnormality, the placenta overlies internal os of uterus, essentially covering the birth canal. This condition occurs in approximately 1 in 200 to 250 pregnancies. In the third trimester and at term, abnormal bleeding can require cesarian delivery and can also lead to Abruptio Placenta. Ultrasound screening programs during 1st and early 2nd trimester pregnancies now include placental localization. Diagnosis can also be made by transvaginal ultrasound.
- Vasa Previa - (vasa praevia) placental abnormality where the fetal vessels lie within the membranes close too or crossing the inner cervical os (opening). This occurs normally in 1:2500-5000 pregnancies and leads to complications similar too those for Placenta Previa.Type II is defined as the condition where the fetal vessels are found crossing over the internal os connecting either a bilobed placenta or a succenturiate lobe with the main placental mass. Some recent evidence of successful in utero laser ablation of type II vasa previa at 22.5 weeks of gestation.
- Abruptio Placenta - a retroplacental blood clot formation, abnormal hemorrhage prior to delivery.
- Chronic Intervillositis - (massive chronicintervillositis, chronic histiocytic intervillositis) Rare placental abnormality and pathology defined by inflammatory placental lesions, mainly in the intervillous space (IVS), with a maternal infiltrate of mononuclear cells (monocytes, lymphocytes, histiocytes) and intervillous fibrinoid deposition.
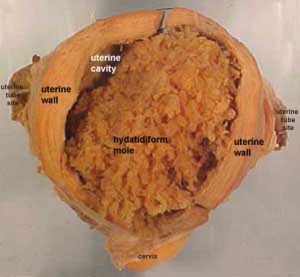
- Hydatidiform mole - placental tumor with no embryo development. Several forms of hydatidiform mole: partial mole, complete mole and persistent gestational trophoblastic tumor. Many of these tumours arise from a haploid sperm fertilizing an egg without a female pronucleus (the alternative form, an embryo without sperm contribution, is called parthenogenesis). The tumour has a "grape-like" placental appearance without enclosed embryo formation. Following a first molar pregnancy, there is approximately a 1% risk of a second molar pregnancy.
- Placenta Abnormalities
- Links: Placenta - Abnormalities
Placental Cord Abnormalities
There are few abnormalities associated with umbilical cord development, other that abnormally short or long cords, which in most cases do not cause difficulties. In some cases though, long cords can wrap around limbs or the fetus neck, which can then restrict blood flow or lead to tissue or nerve damage, and therefore effect develoment.
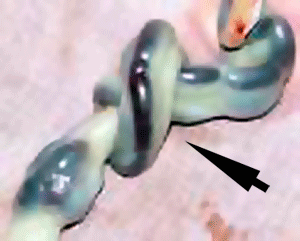
- Cord knotting - can also occur (1%) in most cases these knots have no effect, in some cases of severe knotting this can prevents the passage of placental blood.
- Cord torsion - Rare event where even without knot formation can also affect placental blood flow, even leading to fetal demise.
Placental Infections
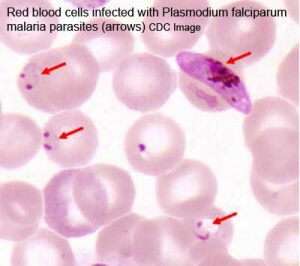
|
|
| Malaria (plasmodium falciparum) | Listeria maternal-fetal barrier |
- Several infective agents may cross into the placenta from the maternal circulation, as well as enter the embry/fetal circulation. The variety of bacterial infections that can occur during pregnancy is as variable as the potential developmental effects, from virtually insignificant to a major developmental, abortive or fatal in outcome.
- Pregnant women have an increased susceptibility to malaria infection. Malarial infection of the placenta by sequestration of the infected red blood cells leading to low birth weight and other effects. There are four types of malaria caused by the protozoan parasite Plasmodium falciparum (main), Plasmodium vivax, Plasmodium ovale, Plasmodium malariae). This condition is common in regions where malaria is endemic with women carrying their first pregnancy (primigravida).
Placental Pathology
MH - content in this section is not examinable.
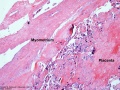
- Chronic Villitis - can occur following placental infection leading to maternal inflammation of the villous stroma, often with associated intervillositis. The inflammation can lead to disruption of blood flow and necrotic cell death.
- Massive Chronic Intervillositis (MCI) - maternal blood-filled space is filled with CD68-positive histiocytes and an increase in fibrin, occuring more commonly in the first trimester.
- Meconium Myonecrosis - prolonged meconium exposure leads to toxic death of myocytes of placental vessels (umbilical cord or chorionic plate).
- Neuroblastoma - a fetal malignancy that leads to an enlarged placenta, with tumor cells in the fetal circulation and rarely in the chorionic villi.
- Thrombophilias - (protein C or S deficiency, factor V Leiden, sickle cell disease, antiphospholipid antibody) can generate an increased fibrin/fibrinoid deposition in the maternal or intervillous space, this can trap and kill villi.
Additional Images
| Virtual Slides | |||||||
|---|---|---|---|---|---|---|---|
|
| ||||||
| Tertiary Villi cross-section | Abnormal placenta | ||||||
Historic - Fetal Membranes Images
External Links
External Links Notice - The dynamic nature of the internet may mean that some of these listed links may no longer function. If the link no longer works search the web with the link text or name. Links to any external commercial sites are provided for information purposes only and should never be considered an endorsement. UNSW Embryology is provided as an educational resource with no clinical information or commercial affiliation.
- Comparative Placentation
- University of Ottawa - Histology - Placenta
- Virtual Microscopy Histology
Placenta Terms
| Placenta Terms (expand to view) |
|---|
with an incidence of about 2.8 per 1,000 pregnancies, there is also a rarer form of extra-abdominal varices.PMID 24883288
with an incidence of about 2.8 per 1,000 pregnancies, there is also a rarer form of extra-abdominal varices. PMID 24883288
|
| Other Terms Lists |
|---|
| Terms Lists: ART | Birth | Bone | Cardiovascular | Cell Division | Endocrine | Gastrointestinal | Genital | Genetic | Head | Hearing | Heart | Immune | Integumentary | Neonatal | Neural | Oocyte | Palate | Placenta | Radiation | Renal | Respiratory | Spermatozoa | Statistics | Tooth | Ultrasound | Vision | Historic | Drugs | Glossary |
| 2018 ANAT2341 - Timetable | Course Outline | Moodle | Tutorial 1 | Tutorial 2 | Tutorial 3 |
Labs: 1 Preimplantation and Implantation | 2 Reproductive Technology Revolution | 3 Group Projects | 4 GM manipulation mouse embryos | 5 Early chicken eggs | 6 Female reproductive tract | 7 Skin regeneration | 8 Vertebral development | 9 Organogenesis Lab | 10 Cardiac development | 11 Group projects | 12 Stem Cell Journal Club |
|
Lectures: 1 Introduction | 2 Fertilization | 3 Week 1/2 | 4 Week 3 | 5 Ectoderm | 6 Placenta | 7 Mesoderm | 8 Endoderm | 9 Research Technology | 10 Cardiovascular | 11 Respiratory | 12 Neural crest | 13 Head | 14 Musculoskeletal | 15 Limb | 16 Renal | 17 Genital | 18 Endocrine | 19 Sensory | 20 Fetal | 21 Integumentary | 22 Birth | 23 Stem cells | 24 Revision |
| Student Projects: Group Projects Information Project 1 | Project 3 | Project 4 | Project 5 | 2018 Test Student | Copyright |