BGDA Practical Placenta - Abnormalities
| Practical 14: Implantation and Early Placentation | Villi Development | Maternal Decidua | Cord Development | Placental Functions | Diagnostic Techniques | Abnormalities |
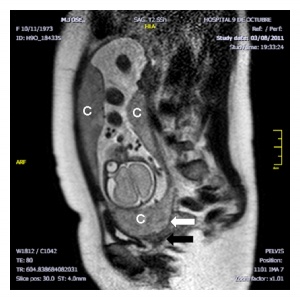
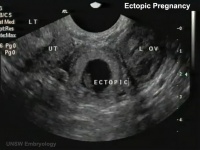
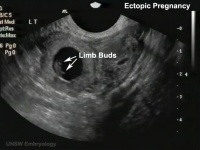
Ectopic Implantation
Commences early stages of placentation.
- Usually identified by ultrasound.
- Presence of trophoblast cells in tube used to pathologically identify implantation.
| Tubal Ectopic | Bicornuate Uterus Ectopic | ||||||
|---|---|---|---|---|---|---|---|
|
|
|

|
|

|
| USA Statistics | |
|---|---|
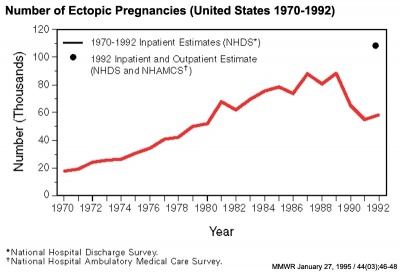
Ectopic Pregnancies- United-States 1970-1992[1] |
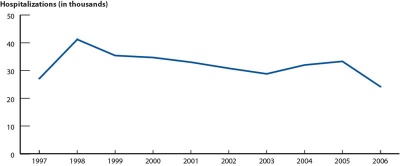
Ectopic Pregnancies- United-States 1997-2006 |
- Links: Ectopic Implantation | ultrasound
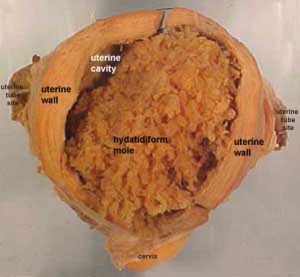
Hydatidiform Mole
Another type of abnormality is when only the conceptus trophoblast layers proliferates and not the embryoblast, no embryo develops, this is called a "hydatidiform mole" (HM), which is due to the continuing presence of the trophoblastic layer, this abnormal conceptus can also implant in the uterus. The trophoblast cells will secrete human chorionic gonadotropin (hCG), as in a normal pregnancy, and may appear maternally and by pregnancy test to be "normal". Prenatal diagnosis by ultrasound analysis demonstrates the absence of a embryo.
There are several forms of hydatidiform mole: partial mole, complete mole and persistent gestational trophoblastic tumor.
- Complete Mole - Only paternal chromosomes, chromosomal genetic material from the ovum (egg) is lost, by an unknown process.
- Partial Mole - Ultrasound of partial mole confirmed by triploidy, chromosomal (genetic) material from the ovum (egg) is retained and the egg is fertilized by one or two sperm.
On ultrasound the tumour has a "grape-like" placental appearance without enclosed embryo formation. Following a first molar pregnancy, there is approximately a 1% risk of a second molar pregnancy.
- The incidence of hydatidiform mole varies between ethnic groups, and typically occurs in 1 in every 1500 pregnancies.
- All hydatidiform mole cases are sporadic, except for extremely rare familial cases.
- Links: hydatidiform mole | Week 2 - Abnormalities
Implantation Abnormalities
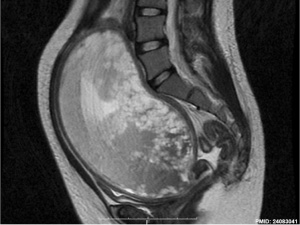
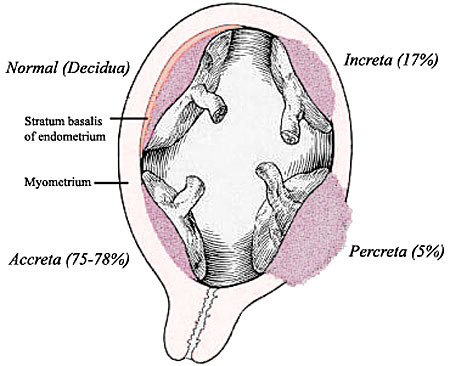
Morbidly adherent placenta (MAP) is the general clinical term used to describe the different forms of abnormal placental implantation (Accreta, Increta and Percreta).
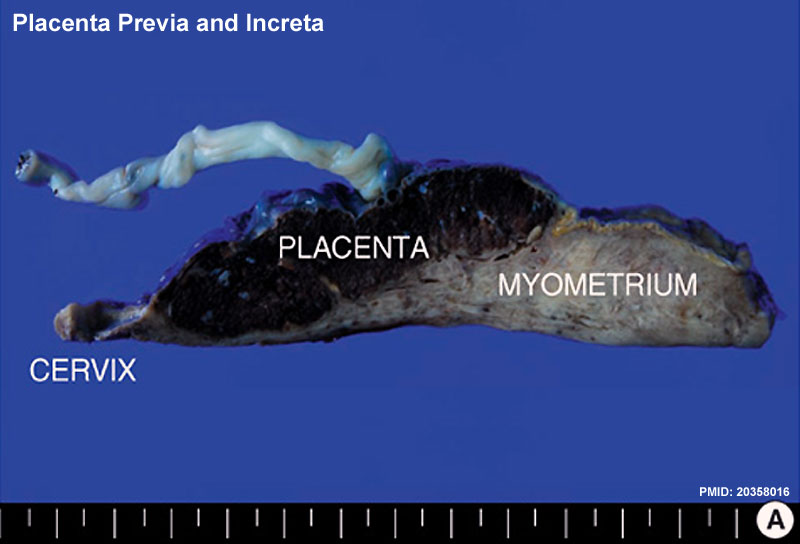
Placenta previa and increta
The placenta is a mateno-fetal organ which begins developing at implantation of the blastocyst and is delivered with the fetus at birth. As the fetus relies on the placenta for not only nutrition, but many other developmentally essential functions, the correct development of the placenta is important to correct embryonic and fetal development.
Abnormalities can range from anatomical associated with degree or site of inplantation, structure (as with twinning), to placental function, placento-maternal effects (pre-eclampsia, fetal erythroblastosis) and finally mechanical abnormalities associated with the placental (umbilical) cord.
- Placenta Accreta - abnormal adherence, with absence of decidua basalis. The incidence of placenta accreta also significantly increases in women with previous cesarean section compared to those without a prior surgical delivery.
- placenta increta - occurs when the placenta attaches deep into the uterine wall and penetrates into the uterine muscle, but does not penetrate the uterine serosa. Placenta increta accounts for approximately 15-17% of all cases.
- placenta percreta - placental villi penetrate myometrium and through to uterine serosa.
- placenta previa - In this placenatal abnormality, the placenta overlies internal os of uterus, essentially covering the birth canal. This condition occurs in approximately 1 in 200 to 250 pregnancies. In the third trimester and at term, abnormal bleeding can require cesarian delivery and can also lead to Abruptio Placenta. Ultrasound screening programs during 1st and early 2nd trimester pregnancies now include placental localization. Diagnosis can also be made by transvaginal ultrasound.
- vasa previa - (vasa praevia) placental abnormality where the fetal vessels lie within the membranes close too or crossing the inner cervical os (opening). Two main associations; 1. velamentous insertions (25–62%) and 2. vessels crossing between lobes in succenturiate or bilobate placentas (33–75%)
- Multilobed Placenta Succenturiata - an accessory portion attached to the main placenta by an artery or vein.
- Abruptio Placenta - a retroplacental blood clot formation, abnormal haemorrhage prior to delivery.
- Chronic Intervillositis - (massive chronicintervillositis, chronic histiocytic intervillositis) Rare placental abnormality and pathology defined by inflammatory placental lesions, mainly in the intervillous space (IVS), with a maternal infiltrate of mononuclear cells (monocytes, lymphocytes, histiocytes) and intervillous fibrinoid deposition.
Cord Abnormalities
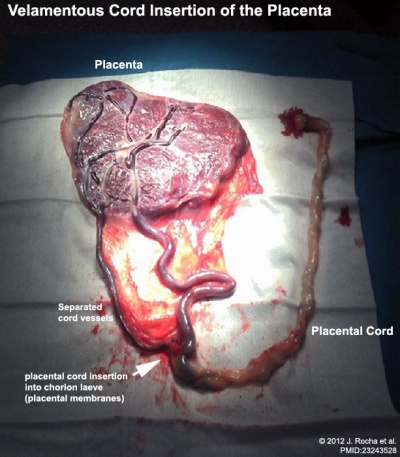
Velamentous Cord Insertion of the Placenta
|
The placental cord inserts into the chorion laeve (placental membranes) away from the edge of the placenta.[2]
The placental vessels are therefore unprotected by Wharton's jelly where they traverse the membranes before they come together into the umbilical cord.
This can also be associated with vasa previa (see above) or haemorrhage caused if the vessels are damaged when the membranes are ruptured prior to birth. The condition is more common in monozygotic twins (15%) and triplets. |
Cord Vessel Number

Cord with only one artery and one vein. |
Persistent Right Umbilical Vein
A fairly rare anomaly, a study of 15,237 obstetric ultrasound examinations performed after 15 weeks' gestation identified only 33 cases of persistent right umbilical vein.[3] Some studies have identified associated fetal anomalies with this condition[4], including cardiac abnormalities.[5] |
Cord Length
Excessively short or long cords (see additional information on cord page). Abnormally long cords may wrap around either extremities or neck of the fetus.
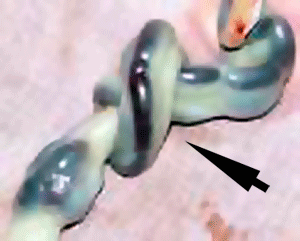
Cord Knotting
|
Placental cord true knot
Cord knotting can occur (1%) in most cases these knots have no effect. In some cases of severe knotting, this can prevents the passage of placental blood. |
Umbilical cord torsion
Rare umbilical cord torsion, even without knot formation can also affect placental blood flow, even leading to fetal demise.
Placental Infections
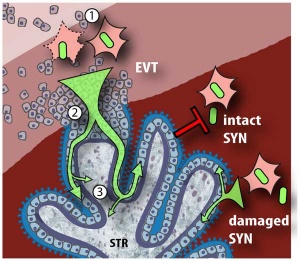
Listeria maternal-fetal barrier |
Several infective agents may cross into the placenta from the maternal circulation, as well as enter the embryo/fetal circulation. The variety of bacterial infections that can occur during pregnancy is as variable as the potential developmental effects, from virtually insignificant to a major developmental, abortive or fatal in outcome.
A study in mouse model has shown that lipopolysaccharide-induced maternal inflammation causes an inflammatory response that is mirrored in the placenta. Placental histology showed structural changes without affecting placental blood flow, though also induced an indirect intestinal injury in the offspring lasting beyond the neonatal period.[6] Lipopolysaccharide is found in the outer membrane of Gram-negative bacteria. |
Cytomegalovirus Placentitis
Clinical term for the cytomegalovirus infection of the placenta. Cytomegalovirus (CMV) is the most common congenital viral infection, causing sensory (hearing, visual) and psychomotor impairment.
A earlier histological study[7] identified fixed connective tissue cells predominantly infected cell type in placental tissue. In addition, endothelial cells, macrophages and in some cases trophoblast infection. While a more recent in vitro study[8]> suggests that all villi cell types are likely to be infected.
Placental Herpesvirus
A study has identified using an in vitro model that human herpesvirus 8 (HHV-8) can infect the placenta[9]
Placental Malaria
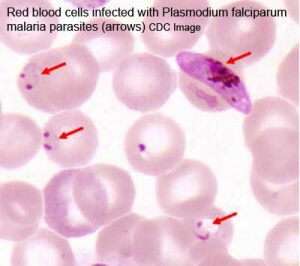
Malaria (plasmodium falciparum) |
Pregnant women have an increased susceptibility to malaria infection.
Malarial infection of the placenta by sequestration of the infected red blood cells leading to low birth weight and other effects. There are four types of malaria caused by the protozoan parasite Plasmodium falciparum (main), Plasmodium vivax, Plasmodium ovale, Plasmodium malariae). This condition is common in regions where malaria is endemic with women carrying their first pregnancy (primigravida).
|
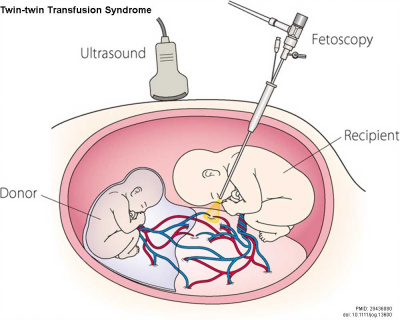
Twin–Twin Transfusion Syndrome
| Twin–Twin Transfusion Syndrome (TTTS) occurs with intrauterine blood transfusion from one twin (donor) to another twin (recipient) where there is an imbalance of blood flow from the donor twin to the recipient twin. Condition occurs in about 10% of monochorionic twins and clinically diagnosed by the alternate presence of polyhydramnios in one fetus and oligohydramnios in the co-twin. (More? twinning | Twin-twin transfusion syndrome)
|
|
Placentation Abnormalities Interactive Component
| Attempt the Quiz - Placentation Abnormalities | ||
|---|---|---|

Here are a few simple Quiz questions that relate to Placentation Abnormalities from the practical.
|
| Practical 14: Implantation and Early Placentation | Villi Development | Maternal Decidua | Cord Development | Placental Functions | Diagnostic Techniques | Abnormalities |
Additional Information
| Additional Information - Content shown under this heading is not part of the material covered in this class. It is provided for those students who would like to know about some concepts or current research in topics related to the current class page. |
Bilobed Placenta with Velamentous Cord Insertion
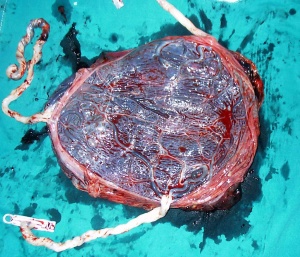
Placenta Examination
Royal Hospital for Women
Placenta Examination[11]
- "A one-minute examination of the placenta performed in the delivery room provides information that may be important to the care of both mother and infant. The findings of this assessment should be documented in the delivery records. During the examination, the size, shape, consistency and completeness of the placenta should be determined, and the presence of accessory lobes, placental infarcts, hemorrhage, tumors and nodules should be noted. The umbilical cord should be assessed for length, insertion, number of vessels, thromboses, knots and the presence of Wharton's jelly. The color, luster and odor of the fetal membranes should be evaluated, and the membranes should be examined for the presence of large (velamentous) vessels. Tissue may be retained because of abnormal lobation of the placenta or because of placenta accreta, placenta increta or placenta percreta. Numerous common and uncommon findings of the placenta, umbilical cord and membranes are associated with abnormal fetal development and perinatal morbidity. The placenta should be submitted for pathologic evaluation if an abnormality is detected or certain indications are present."
Gestational hypertension-preeclampsia
- also known as gestational proteinuric hypertension
- common pregnancy complication, with an incidence ranging from 2–8%.
- lack of blood flow from the uterus to the placenta is always observed.
- pathogenesis of eclamptic convulsions remains unknown and women with a history of eclampsia are at increased risk of eclampsia (1-2%) and preeclampsia (22-35%) in subsequent pregnancies.
A large population study in Norway has shown a strong generational association such that daughters of women who had pre-eclampsia during pregnancy had more than twice the risk of pre-eclampsia themselves. The paper concludes "Maternal genes and fetal genes from either the mother or father may trigger pre-eclampsia. The maternal association is stronger than the fetal association. The familial association predicts more severe pre-eclampsia."[12]
Diabetes
Maternal Type 1 diabetes can alter placental vascular development. Effects may be due to either maternal hyperglycaemia or fatal hyperinsulinaemia with high glucose and insulin shown in other systems to alter vascularity, increasing vascular endothelial growth factor (VEGF), nitric oxide (NO) and protein kinase C (PKC).[13][14]
Features of the placental vessels include:
- Increased angiogenesis
- altered junctional maturity and molecular occupancy
- increased leakiness
Diabetes insipidus (DI) is a rare complication of pregnancy occurring in 1 in 30,000 pregnancies. Vasopressinase secreted by placental trophoblasts destroys maternal anti-diuretic hormone (ADH, vasopressin}.[15]
Multiple Pregnancy
| Monochorionic twin pregnancies | Monochorionic triamniotic triplet pregnancy placenta |
|---|---|

|
|
Twin-twin Transfusion Syndrome
Chochrane database 2014 review[16] "Twin-twin transfusion syndrome, a condition affecting monochorionic twin pregnancies, is associated with a high risk of perinatal mortality and morbidity. A number of treatments have been introduced to treat the condition but it is unclear which intervention improves maternal and fetal outcome. ...Endoscopic laser coagulation of anastomotic vessels should continue to be considered in the treatment of all stages of twin-twin transfusion syndrome to improve neurodevelopmental outcomes.Further research targeted towards assessing the effect of treatment on milder (Quintero stage 1 and 2) and more severe (Quintero stage 4) forms of twin-twin transfusion syndrome is required. Studies should aim to assess long-term outcomes of survivors."
Quintero staging system[17] - established in 1999 a sonographic and clinical parameter staging system for TTTS.
Maternal Diet
Effects of micronutrients on placental function: evidence from clinical studies to animal models[18]
- "Micronutrient deficiencies are common in pregnant women due to low dietary intake and increased requirements for fetal development. ...Interestingly, there is emerging evidence that deficiencies in all micronutrients examined induce a pro-inflammatory state in the placenta, drawing parallels with the inflammation detected in FGR, pre-eclampsia, stillbirth and preterm birth. Beneficial effects of supplementation are apparent in vitro and in animal models, and for combined micronutrients in clinical studies. However, greater understanding of the roles of these micronutrients, and insight into their involvement in placental dysfunction, combined with more robust clinical studies, is needed to fully understand ascertain the potential benefits of supplementation in pregnancy."
Placental Weight
A 2009 longitudinal Norwegian study suggests an association between large placenta relative to fetal size "disproportionately large placenta relative to birth weight was associated with increased risk of (adult) cardiovascular disease death."[19] See also DOHAD hypothesis.
A recent 2019 study has also shown an associations between the features of gross placental morphology and birthweight.[20]
- "The placenta plays a critical role in regulating fetal growth. Recent studies suggest that there may be sex-specific differences in placental development. The purpose of our study was to evaluate the associations between birthweight and placental morphology in models adjusted for covariates and to assess sex-specific differences in these associations. We analyzed data from the Stillbirth Collaborative Research Network's population-based case-control study conducted between 2006 and 2008, which recruited cases of stillbirth and population-based controls in 5 states. Our analysis was restricted to singleton live births with a placental examination (n = 1229). Characteristics of placental morphology evaluated include thickness, surface area, difference in diameters, shape, and umbilical cord insertion site. We used linear regression to model birthweight as a function of placental morphology and covariates. Surface area had the greatest association with birthweight; a reduction in surface area of 83 cm2, which reflects the interquartile range, is associated with a 260.2-g reduction in birthweight (95% confidence interval, -299.9 to -220.6), after adjustment for other features of placental morphology and covariates. Reduced placental thickness was also associated with lower birthweight. These associations did not differ between males and females. Our results suggest that reduced placental thickness and surface area are independently associated with lower birthweight and that these relationships are not related to sex." birthweight
Other Online Resources
2013 Meeting Presentation- Placenta Circulation
| Placenta Terms (expand to view) |
|---|
with an incidence of about 2.8 per 1,000 pregnancies, there is also a rarer form of extra-abdominal varices.PMID 24883288
with an incidence of about 2.8 per 1,000 pregnancies, there is also a rarer form of extra-abdominal varices. PMID 24883288
|
| Other Terms Lists |
|---|
| Terms Lists: ART | Birth | Bone | Cardiovascular | Cell Division | Endocrine | Gastrointestinal | Genital | Genetic | Head | Hearing | Heart | Immune | Integumentary | Neonatal | Neural | Oocyte | Palate | Placenta | Radiation | Renal | Respiratory | Spermatozoa | Statistics | Tooth | Ultrasound | Vision | Historic | Drugs | Glossary |
References
- ↑ Centers for Disease Control and Prevention (CDC). (1995). Ectopic pregnancy--United States, 1990-1992. MMWR Morb. Mortal. Wkly. Rep. , 44, 46-8. PMID: 7823895
- ↑ Rocha J, Carvalho J, Costa F, Meireles I & do Carmo O. (2012). Velamentous cord insertion in a singleton pregnancy: an obscure cause of emergency cesarean-a case report. Case Rep Obstet Gynecol , 2012, 308206. PMID: 23243528 DOI.
- ↑ Hill LM, Mills A, Peterson C & Boyles D. (1994). Persistent right umbilical vein: sonographic detection and subsequent neonatal outcome. Obstet Gynecol , 84, 923-5. PMID: 7970470
- ↑ Weichert J, Hartge D, Germer U, Axt-Fliedner R & Gembruch U. (2011). Persistent right umbilical vein: a prenatal condition worth mentioning?. Ultrasound Obstet Gynecol , 37, 543-8. PMID: 20922781 DOI.
- ↑ Lide B, Lindsley W, Foster MJ, Hale R & Haeri S. (2016). Intrahepatic Persistent Right Umbilical Vein and Associated Outcomes: A Systematic Review of the Literature. J Ultrasound Med , 35, 1-5. PMID: 26635256 DOI.
- ↑ Fricke EM, Elgin TG, Gong H, Reese J, Gibson-Corley KN, Weiss RM, Zimmerman K, Bowdler NC, Kalantera KM, Mills DA, Underwood MA & McElroy SJ. (2018). Lipopolysaccharide-induced maternal inflammation induces direct placental injury without alteration in placental blood flow and induces a secondary fetal intestinal injury that persists into adulthood. Am. J. Reprod. Immunol. , 79, e12816. PMID: 29369434 DOI.
- ↑ Sinzger C, Müntefering H, Löning T, Stöss H, Plachter B & Jahn G. (1993). Cell types infected in human cytomegalovirus placentitis identified by immunohistochemical double staining. Virchows Arch A Pathol Anat Histopathol , 423, 249-56. PMID: 8236822
- ↑ Tao L, Suhua C, Juanjuan C, Zongzhi Y, Juan X & Dandan Z. (2011). In vitro study on human cytomegalovirus affecting early pregnancy villous EVT's invasion function. Virol. J. , 8, 114. PMID: 21392403 DOI.
- ↑ Di Stefano M, Calabrò ML, Di Gangi IM, Cantatore S, Barbierato M, Bergamo E, Kfutwah AJ, Neri M, Chieco-Bianchi L, Greco P, Gesualdo L, Ayouba A, Menu E & Fiore JR. (2008). In vitro and in vivo human herpesvirus 8 infection of placenta. PLoS ONE , 3, e4073. PMID: 19115001 DOI.
- ↑ Report of the New South Wales Chief Health Officer, 2004 accessed 19Oct05
- ↑ Yetter JF. (1998). Examination of the placenta. Am Fam Physician , 57, 1045-54. PMID: 9518951
- ↑ Skjaerven R, Vatten LJ, Wilcox AJ, Rønning T, Irgens LM & Lie RT. (2005). Recurrence of pre-eclampsia across generations: exploring fetal and maternal genetic components in a population based cohort. BMJ , 331, 877. PMID: 16169871 DOI.
- ↑ Leach L. (2011). Placental vascular dysfunction in diabetic pregnancies: intimations of fetal cardiovascular disease?. Microcirculation , 18, 263-9. PMID: 21418381 DOI.
- ↑ Leach L, Taylor A & Sciota F. (2009). Vascular dysfunction in the diabetic placenta: causes and consequences. J. Anat. , 215, 69-76. PMID: 19563553 DOI.
- ↑ Rodrigo N & Hocking S. (2018). Transient diabetes insipidus in a post-partum woman with pre-eclampsia associated with residual placental vasopressinase activity. Endocrinol Diabetes Metab Case Rep , 2018, . PMID: 29850023 DOI.
- ↑ Roberts D, Neilson JP, Kilby MD & Gates S. (2014). Interventions for the treatment of twin-twin transfusion syndrome. Cochrane Database Syst Rev , , CD002073. PMID: 24482008 DOI.
- ↑ Quintero RA, Morales WJ, Allen MH, Bornick PW, Johnson PK & Kruger M. (1999). Staging of twin-twin transfusion syndrome. J Perinatol , 19, 550-5. PMID: 10645517
- ↑ Baker BC, Hayes D & Jones RL. (2018). Effects of micronutrients on placental function: evidence from clinical studies to animal models. Reproduction , , . PMID: 29844225 DOI.
- ↑ Risnes KR, Romundstad PR, Nilsen TI, Eskild A & Vatten LJ. (2009). Placental weight relative to birth weight and long-term cardiovascular mortality: findings from a cohort of 31,307 men and women. Am. J. Epidemiol. , 170, 622-31. PMID: 19638481 DOI.
- ↑ Freedman AA, Hogue CJ, Marsit CJ, Rajakumar A, Smith AK, Goldenberg RL, Dudley DJ, Saade GR, Silver RM, Gibbins KJ, Stoll BJ, Bukowski R & Drews-Botsch C. (2019). Associations Between the Features of Gross Placental Morphology and Birthweight. Pediatr. Dev. Pathol. , 22, 194-204. PMID: 30012074 DOI.
BGDA: Lecture 1 | Lecture 2 | Practical 3 | Practical 6 | Practical 12 | Lecture Neural | Practical 14 | Histology Support - Female | Male | Tutorial
Glossary Links
- Glossary: A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | Numbers | Symbols | Term Link
Cite this page: Hill, M.A. (2026, March 13) Embryology BGDA Practical Placenta - Abnormalities. Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/BGDA_Practical_Placenta_-_Abnormalities
- © Dr Mark Hill 2026, UNSW Embryology ISBN: 978 0 7334 2609 4 - UNSW CRICOS Provider Code No. 00098G