Abnormal Development - Toxoplasmosis
| Embryology - 27 Apr 2024 |
|---|
| Google Translate - select your language from the list shown below (this will open a new external page) |
|
العربية | català | 中文 | 中國傳統的 | français | Deutsche | עִברִית | हिंदी | bahasa Indonesia | italiano | 日本語 | 한국어 | မြန်မာ | Pilipino | Polskie | português | ਪੰਜਾਬੀ ਦੇ | Română | русский | Español | Swahili | Svensk | ไทย | Türkçe | اردو | ייִדיש | Tiếng Việt These external translations are automated and may not be accurate. (More? About Translations) |
Introduction
In 2003, the global annual incidence of congenital toxoplasmosis was estimated to be 190,100 cases, equivalent to a burden of 1.20 million disability-adjusted life years. High burdens were seen in South America and in some Middle Eastern and low-income countries.[1]
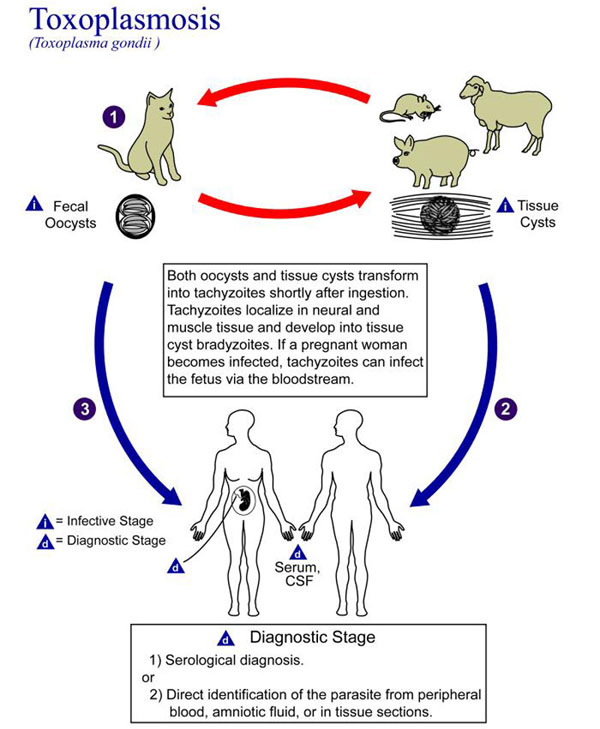
The causal agent of toxoplasmosis is the protist Toxoplasma gondii (T. gondii). This unicellular eukaryote is a member of the phylum Apicomplexa which includes other parasites responsible for a variety of diseases (malaria, cryptosporidiosis). The diagnosis and timing of an infection are diagnostically based on serological tests. During a period of acute maternal infection, transplacental transmission can occur, and the rate of congenital toxoplasmosis with risk for severe fetal varies from 15 to 68%, depending on gestational age and the transmission rate is highest in the later stages of pregnancy. The congenital disease is characterized by a wide range of clinical manifestations (neural, vision, and systemic involvement). Within the central nervous system infection causes extensive areas of randomly distributed necrosis and ventricular involvement may cause hydrocephalus. Within the eye chorioretinitis occurs, an inflammation of the choroid pigmented vascular coat of the eye. A "bradyzoite" is the term used for the T. gondii dormant stage.
A recent survey identified a low infection knowledge among doctors and nurses providing prenatal care in an endemic region.[2] Some findings suggest that pre-pregnancy immunization against toxoplasmosis may not protect against reinfection by atypical strains.
| Historic Embryology |
| Toxoplasma gondii (toxoplasmosis) was initially described in 1908 in Tunis by Nicolle and Manceaux (1908) and in Brazil by Splendore (1908).[3]
Currently every 3 years experts from many areas meet at the ICOCT – IV "International Congress on Congenital Toxoplasmosis" (last held in 2019 Casa Cava, Italy). |
Some Recent Findings
|
| More recent papers |
|---|
|
This table allows an automated computer search of the external PubMed database using the listed "Search term" text link.
More? References | Discussion Page | Journal Searches | 2019 References | 2020 References Search term: Developmental Toxoplasmosis | Toxoplasmosis | Toxoplasmosis Necrosis | chorioretinitis |
| Older papers |
|---|
| These papers originally appeared in the Some Recent Findings table, but as that list grew in length have now been shuffled down to this collapsible table.
See also the Discussion Page for other references listed by year and References on this current page.
|
Toxoplasmosis Lifecycle
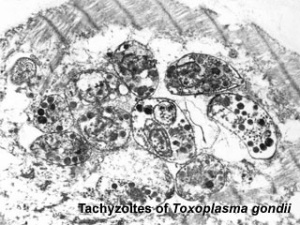
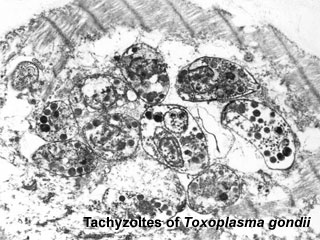
Toxoplasma Tachyzoites
European Congenital Toxoplasmosis Surveillance
See the recent 2008 article.[10]
- Denmark - neonatal screening programme based on neonatal Guthrie card testing for toxoplasma-specific IgM was implemented in 1999 but discontinued on 31 July, 2007.
- France - a surveillance system for congenital toxoplasmosis was initiated in May 2007.
- Germany - congenital toxoplasmosis cases have been notifiable since 2001 implemented under the Protection Against Infection Act.
- Italy - surveillance is confined to a regional programme in the Campania region initiated in 1997.
- Bulgaria, Cyprus, Czech Republic, England and Wales, Estonia, Ireland, Latvia, Lithuania, Malta, Poland, Scotland, and Slovakia - surveillance (congenital or not), as defined by the European Union (symptomatic toxoplasmosis cases serologically confirmed) is considered a notifiable disease and subject to continuous data collection.
Ocular Toxoplasmosis
Clinical episodes of ocular toxoplasmosis can represent either acquire toxoplasmosis after birth or a reactivation of an infection that was acquired in utero.
Ocular toxoplasmosis is the commonest identifiable cause of posterior uveitis.
- Links: PubMed Health - Uveitis
References
- ↑ Torgerson PR & Mastroiacovo P. (2013). The global burden of congenital toxoplasmosis: a systematic review. Bull. World Health Organ. , 91, 501-8. PMID: 23825877 DOI.
- ↑ da Silva LB, de Oliveira Rde V, da Silva MP, Bueno WF, Amendoeira MR & de Souza Neves E. (2011). Knowledge of toxoplasmosis among doctors and nurses who provide prenatal care in an endemic region. Infect Dis Obstet Gynecol , 2011, 750484. PMID: 21747644 DOI.
- ↑ Weiss LM & Dubey JP. (2009). Toxoplasmosis: A history of clinical observations. Int. J. Parasitol. , 39, 895-901. PMID: 19217908 DOI.
- ↑ Wallon M, Fricker-Hidalgo H, Chapey E, Bailet C, Dard C, Brenier-Pinchart MP & Pelloux H. (2020). Performance of a Toxo IgM prototype assay for the diagnosis of maternal and congenital Toxoplasma infections. Clin. Chem. Lab. Med. , , . PMID: 32333648 DOI.
- ↑ Teimouri A, Mohtasebi S, Kazemirad E & Keshavarz H. (2020). Role of Toxoplasma gondii IgG avidity testing in discriminating between acute and chronic toxoplasmosis in pregnancy. J. Clin. Microbiol. , , . PMID: 32321784 DOI.
- ↑ Fanigliulo D, Marchi S, Montomoli E & Trombetta CM. (2020). Toxoplasma gondii in women of childbearing age and during pregnancy: seroprevalence study in Central and Southern Italy from 2013 to 2017. Parasite , 27, 2. PMID: 31934847 DOI.
- ↑ Burgdorf KS, Trabjerg BB, Pedersen MG, Nissen J, Banasik K, Pedersen OB, Sørensen E, Nielsen KR, Larsen MH, Erikstrup C, Bruun-Rasmussen P, Westergaard D, Thørner LW, Hjalgrim H, Paarup HM, Brunak S, Pedersen CB, Torrey EF, Werge T, Mortensen PB, Yolken RH & Ullum H. (2019). Large-scale study of Toxoplasma and Cytomegalovirus shows an association between infection and serious psychiatric disorders. Brain Behav. Immun. , , . PMID: 30685531 DOI.
- ↑ Pomares C, Ajzenberg D, Bornard L, Bernardin G, Hasseine L, Darde ML & Marty P. (2011). Toxoplasmosis and horse meat, France. Emerging Infect. Dis. , 17, 1327-8. PMID: 21762609 DOI.
- ↑ Vilibic-Cavlek T, Ljubin-Sternak S, Ban M, Kolaric B, Sviben M & Mlinaric-Galinovic G. (2011). Seroprevalence of TORCH infections in women of childbearing age in Croatia. J. Matern. Fetal. Neonatal. Med. , 24, 280-3. PMID: 20476874 DOI.
- ↑ Bénard A, Petersen E, Salamon R, Chêne G, Gilbert R & Salmi LR. (2008). Survey of European programmes for the epidemiological surveillance of congenital toxoplasmosis. Euro Surveill. , 13, . PMID: 18445459
Reviews
Kim K. (2018). The Epigenome, Cell Cycle, and Development in Toxoplasma. Annu. Rev. Microbiol. , 72, 479-499. PMID: 29932347 DOI.
Montoya JG & Remington JS. (2008). Management of Toxoplasma gondii infection during pregnancy. Clin. Infect. Dis. , 47, 554-66. PMID: 18624630 DOI.
Montoya JG & Liesenfeld O. (2004). Toxoplasmosis. Lancet , 363, 1965-76. PMID: 15194258 DOI.
Jones J, Lopez A & Wilson M. (2003). Congenital toxoplasmosis. Am Fam Physician , 67, 2131-8. PMID: 12776962
Stegmann BJ & Carey JC. (2002). TORCH Infections. Toxoplasmosis, Other (syphilis, varicella-zoster, parvovirus B19), Rubella, Cytomegalovirus (CMV), and Herpes infections. Curr Womens Health Rep , 2, 253-8. PMID: 12150751
Articles
da Silva LB, de Oliveira Rde V, da Silva MP, Bueno WF, Amendoeira MR & de Souza Neves E. (2011). Knowledge of toxoplasmosis among doctors and nurses who provide prenatal care in an endemic region. Infect Dis Obstet Gynecol , 2011, 750484. PMID: 21747644 DOI.
Search Pubmed
Search Pubmed: Toxoplasmosis | Maternal Toxoplasmosis
External Links
External Links Notice - The dynamic nature of the internet may mean that some of these listed links may no longer function. If the link no longer works search the web with the link text or name. Links to any external commercial sites are provided for information purposes only and should never be considered an endorsement. UNSW Embryology is provided as an educational resource with no clinical information or commercial affiliation.
- NIH PubMed Health Toxoplasmosis | TORCH screen
- ABC Radio The Health Report - Toxoplasmosis Broadcast Monday 30 April 2001
- Queensland Health Topic - Toxoplasmosis
- Cat World toxoplasmosis in cats
Glossary Links
- Glossary: A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | Numbers | Symbols | Term Link
Cite this page: Hill, M.A. (2024, April 27) Embryology Abnormal Development - Toxoplasmosis. Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/Abnormal_Development_-_Toxoplasmosis
- © Dr Mark Hill 2024, UNSW Embryology ISBN: 978 0 7334 2609 4 - UNSW CRICOS Provider Code No. 00098G