Abnormal Development - Fetal Alcohol Syndrome: Difference between revisions
mNo edit summary |
mNo edit summary |
||
| Line 43: | Line 43: | ||
|-bgcolor="F5FAFF" | |-bgcolor="F5FAFF" | ||
| | | | ||
* '''Proceedings of the 2019 Annual Meeting of the Fetal Alcohol Spectrum Disorders Study Group'''{{#pmid:32171771|PMID32171771}} "The 2019 Fetal Alcohol Spectrum Disorders Study Group (FASDSG) meeting was entitled "Computational Approaches to Studying Behavioral Control and Individual Change." The theme was reflected in the presentations of two keynote speakers: A. David Redish, Ph.D. who spoke about computational psychiatry and vulnerabilities in decision-making processes, and Kevin Grimm, Ph.D. who spoke about contemporary machine learning approaches to studying individual change. The conference presented updates from three government agencies, and short presentations by junior and senior investigators showcasing late-breaking FASD research. The conference was capped by H. Eugene Hoyme, M.D., FACMG, FAAP, the recipient of the 2019 Henry Rosett award for career-long contributions to the field." | |||
* '''Review - The Early Developmental Outcomes of Prenatal Alcohol Exposure'''{{#pmid:30619064|PMID30619064}} "This paper systematically reviews the literature on the effects of prenatal alcohol exposure on early child development from birth to 5 years with the aim to synthesize the developmental outcomes associated with prenatal alcohol exposure, and inform further research to improve our knowledge of the manifestations of prenatal alcohol exposure. Methods: Electronic databases (MEDLINE, Psych INFO, and Psych ARTICLES) were searched to find papers on the developmental outcomes of prenatal alcohol exposure in neonates, infants and toddlers and pre-school aged children. Studies were selected based on participants self-reporting alcohol consumption during pregnancy (either prospectively or retrospectively) and/or children being diagnosed with FASD based on a standardized assessment that includes a dysmorphology examination. Conclusion: The outcomes related to lower levels of prenatal alcohol exposure as well as outcomes in specific developmental domains, are poorly understood. Further research should aim to clarify the more subtle or less easily measurable manifestations of prenatal alcohol exposure on early development when the potential for greatest impact of interventions is highest." | * '''Review - The Early Developmental Outcomes of Prenatal Alcohol Exposure'''{{#pmid:30619064|PMID30619064}} "This paper systematically reviews the literature on the effects of prenatal alcohol exposure on early child development from birth to 5 years with the aim to synthesize the developmental outcomes associated with prenatal alcohol exposure, and inform further research to improve our knowledge of the manifestations of prenatal alcohol exposure. Methods: Electronic databases (MEDLINE, Psych INFO, and Psych ARTICLES) were searched to find papers on the developmental outcomes of prenatal alcohol exposure in neonates, infants and toddlers and pre-school aged children. Studies were selected based on participants self-reporting alcohol consumption during pregnancy (either prospectively or retrospectively) and/or children being diagnosed with FASD based on a standardized assessment that includes a dysmorphology examination. Conclusion: The outcomes related to lower levels of prenatal alcohol exposure as well as outcomes in specific developmental domains, are poorly understood. Further research should aim to clarify the more subtle or less easily measurable manifestations of prenatal alcohol exposure on early development when the potential for greatest impact of interventions is highest." | ||
Revision as of 23:05, 18 March 2020
| Embryology - 26 Apr 2024 |
|---|
| Google Translate - select your language from the list shown below (this will open a new external page) |
|
العربية | català | 中文 | 中國傳統的 | français | Deutsche | עִברִית | हिंदी | bahasa Indonesia | italiano | 日本語 | 한국어 | မြန်မာ | Pilipino | Polskie | português | ਪੰਜਾਬੀ ਦੇ | Română | русский | Español | Swahili | Svensk | ไทย | Türkçe | اردو | ייִדיש | Tiếng Việt These external translations are automated and may not be accurate. (More? About Translations) |
| ICD-11 |
|---|
LD2F.00 Foetal alcohol syndrome
|
Introduction

Fetal Alcohol Syndrome (FAS) disorder was clinically described (USA) in humans about 30 years ago (1973), while historically alcohol's teratogenic effects were identified in the early 20th century in a mix with the prohibition cause of the period.
Consuming alcohol during pregnancy is the cause of Fetal Alcohol Syndrome (FAS), consisting of a variable degree of birth defects and mental retardation, initially identified by a reduced head size and distinctive facial features.
Similar effects without the obvious alterations to appearance, but with nervous system effects, are sometimes typified as Fetal Alcohol Effects (FAE). Alcohol is able to cross the placenta from maternal circulation through the placenta into fetal circulation.
Alcohol exposure affects cranial neural crest cell migration and survival, that impacts upon frontonasal prominence and pharyngeal arch development. A second effect may be through alcohol exposure inducing retinoic acid deficiency in the embryo, affecting downstream pathways that are transcriptionally controlled retinoic acid target genes.[2]
Exposure of embryos in vitro to ethanol also simulates the premature differentiation of prechondrogenic mesenchyme of the facial primordia.[3] This result may explain some facial abnormalities associated with FAS, the mechanism of which is still unknown.
Alcohol intake is also one of several factor known to impact upon birthweight. In Australia (2005) 6.4% of all liveborn babies were of low birthweight (less than 2,500 grams).
- "Targeting or shaming women for drinking alcohol while they are pregnant is not effective in causing them to reduce their alcohol intake."
Cell death (apoptosis) induced by alcohol has also been suggested as relevant to craniofacial abnormalities and neurological development. The neurological effects (FAS limits IQ to around 70) may be due to cell death in the embryonic neuroepithelium (the outer layer of the developing neural tube) at an early developmental stage. Some additional evidence suggests that alcohol could also directly damage DNA.
These developmental abnormalities are maternal in origin and are not genetic, though there are probably genetic elements involved with alcoholism (More? OMIM alcoholism).
| Educational Use Only - Embryology is an educational resource for learning concepts in embryological development, no clinical information is provided and content should not be used for any other purpose. |
Some Recent Findings

|
| More recent papers |
|---|
|
This table allows an automated computer search of the external PubMed database using the listed "Search term" text link.
More? References | Discussion Page | Journal Searches | 2019 References | 2020 References Search term: Fetal Alcohol Syndrome | Fetal Alcohol Spectrum Disorder |
| Older papers |
|---|
| These papers originally appeared in the Some Recent Findings table, but as that list grew in length have now been shuffled down to this collapsible table.
See also the Discussion Page for other references listed by year and References on this current page.
|
Fetal Alcohol Spectrum Disorders
"Fetal Alcohol Spectrum Disorders (FASD) is an umbrella term describing the range of effects that can occur in an individual whose mother drank alcohol during pregnancy. These effects may include physical, mental, behavioral, and/or learning disabilities with possible lifelong implications. The term FASD is not intended for use as a clinical diagnosis." [11]
Fetal Alcohol Effect (FAE), Alcohol-related Birth Defect (ARBD), and Alcohol-Related Neurodevelopmental Disorder (ARND) are terms also used to describe a the spectrum of conditions related to prenatal alcohol exposure.
About Alcohol
The pure chemical, alcohol is generally available in alcoholic beverages at between 0.5 - 40% concentration. Metabolic rates for alcohol differ between men and women and is also dependent on body size. (SDS datasheet for alcohol)
The neurological euphoria induced by alcohol has been associated with the rapid release of dopamine in limbic areas of the brain.
Not all FAS babies are from alcoholics, but they do represent a significant population more at risk. The genetics of alcoholism are multifactorial, with several candidate genes identified as associated with the disease. (More? OMIM - Alcoholism)
Alcohol Statistics
Statistical information is often difficult to isolate directly, as alcohol is often combined with other drugs (tobacco, illicit drugs, etc).
There is an interesting "American paradox" that Americans have a relatively low rate of per capita alcohol consumption, yet the USA has the highest incidence of FAS (20 times all other countries) in the world.
USA studies by the CDC have reported FAS prevalence rates from 0.2 to 1.5 cases per 1,000 births across various populations. Disadvantaged groups, Native Americans and Australians, and other minorities have been documented to have rates as high as three to five FAS affected children per 1,000 children.[11]
Other studies reflecting a variety of ascertainment methodologies have produced estimates ranging from 0.5 to 2.0 cases per 1,000 live births. Using the CDC FAS estimates, among the approximately 4 million infants born each year, an estimated 1,000 to 6,000 will be born with FAS. Studies of particularly vulnerable populations yield prevalence estimates that far exceed those of other common disabilities.
Binge Drinking
Tracking binge drinking among U.S. childbearing-age women.[12] "The estimated binge drinking prevalence among childbearing-age women 18-44 years (USA) for the years 2001, 2002, and 2003 was 11.9%, 12.4%, and 13.0%, respectively. The estimated number of childbearing-age women who engaged in binge drinking rose from 6.2 million in 2001 to 7.1 million in 2003, an increase of 0.9 million."
FAS Diagnosis
There are a range of postnatal features which are used diagnostically including facial appearance and digit effects.
In addition, there are under development a number of different techniques which may be useful in the future for prenatal diagnosis.
Pregnancy characteristics of women giving birth to children with fetal alcohol syndrome in Far North Queensland.[13] "There is the potential to identify prospectively women presenting for antenatal care who are heavy drinkers and risk FAS in their infants, using the self-reported information about alcohol intake already being collected by our service; such women may then be offered specific interventions to try to reduce alcohol consumption in pregnancy."
Facial Appearance of FAS
Some, or all, of the following facial features are associated with FAS. There has also been a recent study to develop an automated facial analysis technique.[14]
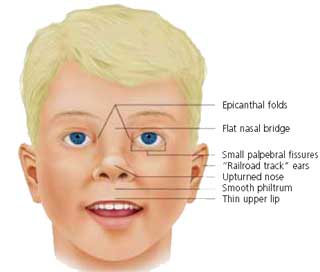
|
FAS facial features[1]
|
FAS Digital Effects
In addition to the distinct facial effects, there may also be abnormalities associated with the digits, fingers or toes.
- Camptodactyly - permanent flexion contracture of a finger or toe.
- Clinodactyly - permanent curving of the fifth finger (usually toward the other fingers) also seen for other fingers or toes.
- Palmar crease - transverse flexion crease of the palm close to the fingers, described as "Hockey stick", widens like the end of a hockey stick and ends between the second and third fingers.
Guidelines
2016 Australia Guidelines
Australian Guide to the diagnosis of Fetal Alcohol Spectrum Disorder (FASD)[15]
- "A diagnosis of FASD requires evidence of prenatal alcohol exposure and severe impairment in three or more domains of central nervous system structure or function."
A diagnosis of FASD can be divided into one of two sub-categories:
- FASD with three sentinel facial features
- FASD with less than three sentinel facial features
See also - Pregnancy characteristics of women giving birth to children with fetal alcohol syndrome in Far North Queensland.[13] "There is the potential to identify prospectively women presenting for antenatal care who are heavy drinkers and risk FAS in their infants, using the self-reported information about alcohol intake already being collected by our service; such women may then be offered specific interventions to try to reduce alcohol consumption in pregnancy."
Links: 2016 Australia Guidelines PDF | Draft Australian alcohol guidelines for low-risk drinking | National Alcohol Strategy Publications | National Alcohol Strategy 2001 to 2003-04 Occasional Paper
2013 German Guidelines
- Diagnosis of fetal alcohol syndrome (FAS): German guideline version 2013[10] "Fetal alcohol syndrome (FAS) belongs to the umbrella of fetal alcohol spectrum disorders (FASD) and affects 0.02-0.8% of all annual births with a high number of undetected cases. The aim of the German guideline version 2013 is to provide objectively evaluated, evidence-based, clinically relevant and easily applicable diagnostic criteria for the full picture FAS. The following diagnostic criteria for FAS resulted: at least one deficit of growth, three defined facial characteristics and one functional or structural anomaly of the central nervous system. Confirmation of intrauterine alcohol exposure is not considered as a prerequisite for FAS diagnosis. The German guideline presented here constitutes an unbiased evidence-based approach to the diagnosis of patients with fetal alcohol syndrome. It includes a practical pocket guide FAS for a quick overview of the diagnostic workup in everyday clinical work."
There were 6 key recommendations.
2005 USA Guidelines
2005 USA Guidelines Fetal Alcohol Syndrome Prevention Team, Division of Birth Defects and Developmental Disabilities, National Center on Birth Defects and Developmental Disabilities[16]
Publication by national task force (USA)[17]
2005 Canadian Guidelines
Fetal alcohol spectrum disorder: Canadian guidelines for diagnosis[18] "The guidelines are based on widespread consultation of expert practitioners and partners in the field. The guidelines have been organized into 7 categories: screening and referral; the physical examination and differential diagnosis; the neurobehavioural assessment; and treatment and follow-up; maternal alcohol history in pregnancy; diagnostic criteria for fetal alcohol syndrome (FAS), partial FAS and alcohol-related neurodevelopmental disorder; and harmonization of Institute of Medicine and 4-Digit Diagnostic Code approaches. The diagnosis requires a comprehensive history and physical and neurobehavioural assessments; a multidisciplinary approach is necessary."
Finland
Fetal alcohol spectrum disorders in Finland: clinical delineation of 77 older children and adolescents.[19] "We have recently completed dysmorphology examination and parent/guardian interviews of the 77 children in the Finnish cohort. ...Although 11% were born prematurely, 70% demonstrated prenatal growth deficiency, and 45% were microcephalic. Other than growth deficits and the cardinal facial features, the most common major and minor anomalies noted were: camptodactyly (55%), "hockey stick" or other altered palmar creases (51%), refractive errors (40%), strabismus (38%), dental crowding (43%), nail hypoplasia (38%), GU anomalies (22%), and congenital heart defects (18%), "Railroad track" ears were not observed in this population."
Brain Development
New brain imaging techniques have allowed greater insight into the effects of alcohol on the brain. In FAS children this includes qualitative and quantitative studies of the postnatal brain including changes include anatomical displacements (corpus callosum) and changes in the neural layer (gray matter) density of the brain.
Abnormal cortical thickness and brain-behavior correlation patterns in individuals with heavy prenatal alcohol exposure.[21] "Significant cortical thickness excesses of up to 1.2 mm were observed in the FASD subjects in large areas of bilateral temporal, bilateral inferior parietal, and right frontal regions."
Teratogenic effects of alcohol: a decade of brain imaging.[22] "Results indicated displacements in the corpus callosum, increased gray matter densities in both hemispheres in the perisylvian regions, and altered gray matter asymmetry in portions of the temporal lobes in the brains of alcohol-exposed subjects."
Sensory Development
Prenatal alcohol exposure delays the development of the cortical barrel field in neonatal rats.[23] "...our model system to examine the effect of prenatal alcohol exposure (PAE) on early somatosensory cortical development. ....These findings suggest that PAE delays the development of the somatosensory cortex (SI); such delays may interfere with timing and formation of cortical circuits."
Bone Development
Binge alcohol exposure during all three trimesters alters bone strength and growth in fetal sheep.[24] "Maternal bones were not different among groups. The higher alcohol dose resulted in reduced fetal femoral bone strength, whereas the tibial bone strength was lower when compared with the normal control subjects. In contrast, the lower alcohol dose increased fetal femoral strength compared to the normal control subjects. The alcohol-exposed fetal bones also tended to exhibit reduced lengths."
Animal Models
See this recent review of the different animal models for FAS.[25]
Mouse Model
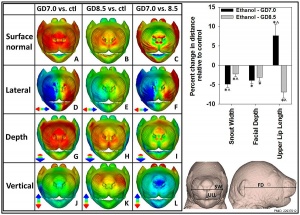
See also contributor Prof Kathy Sulik who works with the mouse model for FAS.
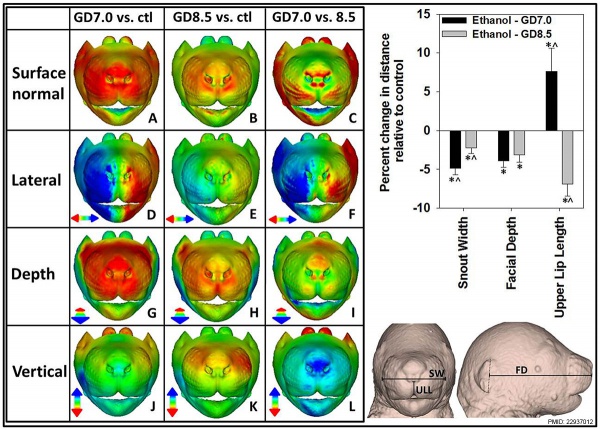
Mouse Face Phenotypes following Ethanol Exposure[20]
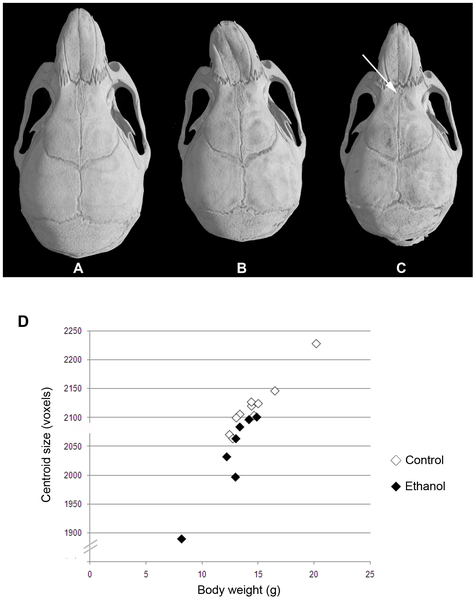
|
| Variable midfacial dysmorphism and microcephaly in a/a offspring of mothers that consumed ethanol during gestation.[26] |
- Links: FAS Mouse Model | FAS Sulik Lab | Mouse Development
Chicken Model
See this recent review of the chicken model of alcohol effects on craniofacial development.[27]
- Links: Chicken Development
Acamprosate
Acamprosate (Campral) is a medication used in conjunction with counselling to treat alcohol dependence. Statistics for acamprosate use in pregnancy are poor, though a study shows not clearly associated with poor maternal or neonatal health outcomes.[28]
References
- ↑ 1.0 1.1 Wattendorf DJ & Muenke M. (2005). Fetal alcohol spectrum disorders. Am Fam Physician , 72, 279-82, 285. PMID: 16050451
- ↑ Petrelli B, Bendelac L, Hicks GG & Fainsod A. (2019). Insights into retinoic acid deficiency and the induction of craniofacial malformations and microcephaly in Fetal Alcohol Spectrum Disorder. Genesis , , e23278. PMID: 30614633 DOI.
- ↑ Hoffman LM & Kulyk WM. (1999). Alcohol promotes in vitro chondrogenesis in embryonic facial mesenchyme. Int. J. Dev. Biol. , 43, 167-74. PMID: 10235393
- ↑ 4.0 4.1 Lecuyer M, Laquerrière A, Bekri S, Lesueur C, Ramdani Y, Jégou S, Uguen A, Marcorelles P, Marret S & Gonzalez BJ. (2017). PLGF, a placental marker of fetal brain defects after in utero alcohol exposure. Acta Neuropathol Commun , 5, 44. PMID: 28587682 DOI.
- ↑ Hamilton DA, Mooney SM, Petrenko CLM & Hamre KM. (2020). Proceedings of the 2019 Annual Meeting of the Fetal Alcohol Spectrum Disorders Study Group. Alcohol , , . PMID: 32171771 DOI.
- ↑ Subramoney S, Eastman E, Adnams C, Stein DJ & Donald KA. (2018). The Early Developmental Outcomes of Prenatal Alcohol Exposure: A Review. Front Neurol , 9, 1108. PMID: 30619064 DOI.
- ↑ McCormack C, Hutchinson D, Burns L, Youssef G, Wilson J, Elliott E, Allsop S, Najman J, Jacobs S, Rossen L, Olsson C & Mattick R. (2018). Maternal and partner prenatal alcohol use and infant cognitive development. Drug Alcohol Depend , 185, 330-338. PMID: 29499553 DOI.
- ↑ Jamuar SS, Picker JD & Stoler JM. (2018). Utility of Genetic Testing in Fetal Alcohol Spectrum Disorder. J. Pediatr. , , . PMID: 29398060 DOI.
- ↑ Harrar V, Elkrief L, Bouskila J, Kucera R, Fink-Jensen A, Bouchard JF, Palmour R & Ptito M. (2017). Effects of Prenatal Alcohol Exposure on the Visual System of Monkeys Measured at Different Stages of Development. Invest. Ophthalmol. Vis. Sci. , 58, 6282-6291. PMID: 29242902 DOI.
- ↑ 10.0 10.1 Landgraf MN, Nothacker M & Heinen F. (2013). Diagnosis of fetal alcohol syndrome (FAS): German guideline version 2013. Eur. J. Paediatr. Neurol. , 17, 437-46. PMID: 23618613 DOI.
- ↑ 11.0 11.1 Bertrand J, Floyd RL, Weber MK, O'Connor M, Riley EP, Johnson KA, Cohen DE, National Task Force on FAS/FAE. Fetal Alcohol Syndrome: Guidelines for Referral and Diagnosis. Atlanta, GA: Centers for Disease Control and Prevention; 2004. PDF
- ↑ Tsai J, Floyd RL & Bertrand J. (2007). Tracking binge drinking among U.S. childbearing-age women. Prev Med , 44, 298-302. PMID: 17150249 DOI.
- ↑ 13.0 13.1 Coyne KL, de Costa CM, Heazlewood RJ & Newman HC. (2008). Pregnancy characteristics of women giving birth to children with fetal alcohol syndrome in Far North Queensland. Aust N Z J Obstet Gynaecol , 48, 240-7. PMID: 18532953 DOI.
- ↑ Fang S, McLaughlin J, Fang J, Huang J, Autti-Rämö I, Fagerlund A, Jacobson SW, Robinson LK, Hoyme HE, Mattson SN, Riley E, Zhou F, Ward R, Moore ES & Foroud T. (2008). Automated diagnosis of fetal alcohol syndrome using 3D facial image analysis. Orthod Craniofac Res , 11, 162-71. PMID: 18713153 DOI.
- ↑ Bower C, Elliott EJ 2016, on behalf of the Steering Group. Report to the Australian Government Department of Health: “Australian Guide to the diagnosis of Fetal Alcohol Spectrum Disorder (FASD)”
- ↑ Bertrand J, Floyd LL & Weber MK. (2005). Guidelines for identifying and referring persons with fetal alcohol syndrome. MMWR Recomm Rep , 54, 1-14. PMID: 16251866
- ↑ FAS Fetal Alcohol Syndrome: Guidelines for Referral and Diagnosis." Atlanta, GA: Centers for Disease Control and Prevention; 2004. Bertrand J, Floyd RL, Weber MK, O'Connor M, Riley EP, Johnson KA, Cohen DE, National Task Force on FAS/FAE.
- ↑ Chudley AE, Conry J, Cook JL, Loock C, Rosales T & LeBlanc N. (2005). Fetal alcohol spectrum disorder: Canadian guidelines for diagnosis. CMAJ , 172, S1-S21. PMID: 15738468 DOI.
- ↑ Autti-Rämö I, Fagerlund A, Ervalahti N, Loimu L, Korkman M & Hoyme HE. (2006). Fetal alcohol spectrum disorders in Finland: clinical delineation of 77 older children and adolescents. Am. J. Med. Genet. A , 140, 137-43. PMID: 16353236 DOI.
- ↑ 20.0 20.1 Lipinski RJ, Hammond P, O'Leary-Moore SK, Ament JJ, Pecevich SJ, Jiang Y, Budin F, Parnell SE, Suttie M, Godin EA, Everson JL, Dehart DB, Oguz I, Holloway HT, Styner MA, Johnson GA & Sulik KK. (2012). Ethanol-induced face-brain dysmorphology patterns are correlative and exposure-stage dependent. PLoS ONE , 7, e43067. PMID: 22937012 DOI.
- ↑ Sowell ER, Mattson SN, Kan E, Thompson PM, Riley EP & Toga AW. (2008). Abnormal cortical thickness and brain-behavior correlation patterns in individuals with heavy prenatal alcohol exposure. Cereb. Cortex , 18, 136-44. PMID: 17443018 DOI.
- ↑ Riley EP, McGee CL & Sowell ER. (2004). Teratogenic effects of alcohol: a decade of brain imaging. Am J Med Genet C Semin Med Genet , 127C, 35-41. PMID: 15095470 DOI.
- ↑ Margret CP, Li CX, Chappell TD, Elberger AJ, Matta SG & Waters RS. (2006). Prenatal alcohol exposure delays the development of the cortical barrel field in neonatal rats. Exp Brain Res , 172, 1-13. PMID: 16506013 DOI.
- ↑ Ramadoss J, Hogan HA, Given JC, West JR & Cudd TA. (2006). Binge alcohol exposure during all three trimesters alters bone strength and growth in fetal sheep. Alcohol , 38, 185-92. PMID: 16905445 DOI.
- ↑ Patten AR, Fontaine CJ & Christie BR. (2014). A comparison of the different animal models of fetal alcohol spectrum disorders and their use in studying complex behaviors. Front Pediatr , 2, 93. PMID: 25232537 DOI.
- ↑ Kaminen-Ahola N, Ahola A, Maga M, Mallitt KA, Fahey P, Cox TC, Whitelaw E & Chong S. (2010). Maternal ethanol consumption alters the epigenotype and the phenotype of offspring in a mouse model. PLoS Genet. , 6, e1000811. PMID: 20084100 DOI.
- ↑ Kiecker C. (2016). The chick embryo as a model for the effects of prenatal exposure to alcohol on craniofacial development. Dev. Biol. , 415, 314-325. PMID: 26777098 DOI.
- ↑ Kelty E, Tran D, Lavin T, Preen DB, Hulse G & Havard A. (2019). Prevalence and safety of acamprosate use in pregnant alcohol-dependent women in New South Wales, Australia. Addiction , 114, 206-215. PMID: 30152012 DOI.
Reviews
Reviews Fetal Alcohol Syndrome
Ghazi Sherbaf F, Aarabi MH, Hosein Yazdi M & Haghshomar M. (2019). White matter microstructure in fetal alcohol spectrum disorders: A systematic review of diffusion tensor imaging studies. Hum Brain Mapp , 40, 1017-1036. PMID: 30289588 DOI.
Petrelli B, Bendelac L, Hicks GG & Fainsod A. (2019). Insights into retinoic acid deficiency and the induction of craniofacial malformations and microcephaly in Fetal Alcohol Spectrum Disorder. Genesis , , e23278. PMID: 30614633 DOI.
Subramoney S, Eastman E, Adnams C, Stein DJ & Donald KA. (2018). The Early Developmental Outcomes of Prenatal Alcohol Exposure: A Review. Front Neurol , 9, 1108. PMID: 30619064 DOI.
Riley EP & McGee CL. (2005). Fetal alcohol spectrum disorders: an overview with emphasis on changes in brain and behavior. Exp. Biol. Med. (Maywood) , 230, 357-65. PMID: 15956765
Stokowski LA. (2004). Fetal alcohol syndrome: new guidelines for referral and diagnosis. Adv Neonatal Care , 4, 324. PMID: 15609253
Sulik KK. (2005). Genesis of alcohol-induced craniofacial dysmorphism. Exp. Biol. Med. (Maywood) , 230, 366-75. PMID: 15956766
Caley LM, Kramer C & Robinson LK. (2005). Fetal alcohol spectrum disorder. J Sch Nurs , 21, 139-46. PMID: 15898848 DOI.
Hoyme HE, May PA, Kalberg WO, Kodituwakku P, Gossage JP, Trujillo PM, Buckley DG, Miller JH, Aragon AS, Khaole N, Viljoen DL, Jones KL & Robinson LK. (2005). A practical clinical approach to diagnosis of fetal alcohol spectrum disorders: clarification of the 1996 institute of medicine criteria. Pediatrics , 115, 39-47. PMID: 15629980 DOI.
O'Leary CM. (2004). Fetal alcohol syndrome: diagnosis, epidemiology, and developmental outcomes. J Paediatr Child Health , 40, 2-7. PMID: 14717994
Eustace LW, Kang DH & Coombs D. (2003). Fetal alcohol syndrome: a growing concern for health care professionals. J Obstet Gynecol Neonatal Nurs , 32, 215-21. PMID: 12685673
May PA & Gossage JP. (2001). Estimating the prevalence of fetal alcohol syndrome. A summary. Alcohol Res Health , 25, 159-67. PMID: 11810953
Bertrand J, Floyd RL, Weber MK, O'Connor M, Riley EP, Johnson KA, Cohen DE. National Task Force on FAS/FAE. Fetal Alcohol Syndrome: Guidelines for Referral and Diagnosis. Atlanta, GA: Centers for Disease Control and Prevention; 2004.
Reviews Alcohol Tissue Damage
Medina AE & Ramoa AS. (2005). Early alcohol exposure impairs ocular dominance plasticity throughout the critical period. Brain Res. Dev. Brain Res. , 157, 107-11. PMID: 15939092 DOI.
Medina AE, Krahe TE, Coppola DM & Ramoa AS. (2003). Neonatal alcohol exposure induces long-lasting impairment of visual cortical plasticity in ferrets. J. Neurosci. , 23, 10002-12. PMID: 14602814
Patel VB, Why HJ, Richardson PJ & Preedy VR. (1997). The effects of alcohol on the heart. Adverse Drug React Toxicol Rev , 16, 15-43. PMID: 9192055
Apte MV, Norton ID & Wilson JS. (1994). Ethanol induced acinar cell injury. Alcohol Alcohol Suppl , 2, 365-8. PMID: 8974357
Reviews Fatty Acid Ethyl Esters
Chan D, Caprara D, Blanchette P, Klein J & Koren G. (2004). Recent developments in meconium and hair testing methods for the confirmation of gestational exposures to alcohol and tobacco smoke. Clin. Biochem. , 37, 429-38. PMID: 15183290 DOI.
Swift R. (2003). Direct measurement of alcohol and its metabolites. Addiction , 98 Suppl 2, 73-80. PMID: 14984244
Soderberg BL, Salem RO, Best CA, Cluette-Brown JE & Laposata M. (2003). Fatty acid ethyl esters. Ethanol metabolites that reflect ethanol intake. Am. J. Clin. Pathol. , 119 Suppl, S94-9. PMID: 12951847
Best CA & Laposata M. (2003). Fatty acid ethyl esters: toxic non-oxidative metabolites of ethanol and markers of ethanol intake. Front. Biosci. , 8, e202-17. PMID: 12456329
Musshoff F. (2002). Chromatographic methods for the determination of markers of chronic and acute alcohol consumption. J. Chromatogr. B Analyt. Technol. Biomed. Life Sci. , 781, 457-80. PMID: 12450674
Sirtori CR & Galli C. (2002). N-3 fatty acids and diabetes. Biomed. Pharmacother. , 56, 397-406. PMID: 12442912
Laposata M, Hasaba A, Best CA, Yoerger DM, McQuillan BM, Salem RO, Refaai MA & Soderberg BL. (2002). Fatty acid ethyl esters: recent observations. Prostaglandins Leukot. Essent. Fatty Acids , 67, 193-6. PMID: 12324241
Koren G, Chan D, Klein J & Karaskov T. (2002). Estimation of fetal exposure to drugs of abuse, environmental tobacco smoke, and ethanol. Ther Drug Monit , 24, 23-5. PMID: 11805717
Agarwal DP. (2001). Genetic polymorphisms of alcohol metabolizing enzymes. Pathol. Biol. , 49, 703-9. PMID: 11762132
Soderberg BL & Laposata M. (2001). Fatty acid ethyl esters: markers of ethanol intake. Am Clin Lab , 20, 18-20. PMID: 11586934
Laposata M. (1999). Fatty acid ethyl esters: current facts and speculations. Prostaglandins Leukot. Essent. Fatty Acids , 60, 313-5. PMID: 10471114
Beckemeier ME & Bora PS. (1998). Fatty acid ethyl esters: potentially toxic products of myocardial ethanol metabolism. J. Mol. Cell. Cardiol. , 30, 2487-94. PMID: 9925383 DOI.
Laposata M. (1998). Fatty acid ethyl esters: ethanol metabolites which mediate ethanol-induced organ damage and serve as markers of ethanol intake. Prog. Lipid Res. , 37, 307-16. PMID: 10209651
De Jersey J & Treloar T. (1994). Biosynthesis and possible pathological significance of fatty acid ethyl esters. Alcohol Alcohol Suppl , 2, 171-6. PMID: 8974332
Bora PS & Lange LG. (1993). Molecular mechanism of ethanol metabolism by human brain to fatty acid ethyl esters. Alcohol. Clin. Exp. Res. , 17, 28-30. PMID: 8452205
Articles
Serrano M, Han M, Brinez P & Linask KK. (2010). Fetal alcohol syndrome: cardiac birth defects in mice and prevention with folate. Am. J. Obstet. Gynecol. , 203, 75.e7-75.e15. PMID: 20451895 DOI. (More? Folic Acid and Neural Tube Defects)
Parnell SE, O'Leary-Moore SK, Godin EA, Dehart DB, Johnson BW, Allan Johnson G, Styner MA & Sulik KK. (2009). Magnetic resonance microscopy defines ethanol-induced brain abnormalities in prenatal mice: effects of acute insult on gestational day 8. Alcohol. Clin. Exp. Res. , 33, 1001-11. PMID: 19302087 DOI.
Meintjes EM, Jacobson JL, Molteno CD, Gatenby JC, Warton C, Cannistraci CJ, Hoyme HE, Robinson LK, Khaole N, Gore JC & Jacobson SW. (2010). An FMRI study of number processing in children with fetal alcohol syndrome. Alcohol. Clin. Exp. Res. , 34, 1450-64. PMID: 20528824 DOI. (More? Molecular Development - Epigenetics)
Thomas JD, Zhou FC & Kane CJ. (2009). Proceedings of the 2008 annual meeting of the Fetal Alcohol Spectrum Disorders Study Group. Alcohol , 43, 333-9. PMID: 19560631 DOI.
Fang S, McLaughlin J, Fang J, Huang J, Autti-Rämö I, Fagerlund A, Jacobson SW, Robinson LK, Hoyme HE, Mattson SN, Riley E, Zhou F, Ward R, Moore ES & Foroud T. (2008). Automated diagnosis of fetal alcohol syndrome using 3D facial image analysis. Orthod Craniofac Res , 11, 162-71. PMID: 18713153 DOI.
Coyne KL, de Costa CM, Heazlewood RJ & Newman HC. (2008). Pregnancy characteristics of women giving birth to children with fetal alcohol syndrome in Far North Queensland. Aust N Z J Obstet Gynaecol , 48, 240-7. PMID: 18532953 DOI.
Jacobson SW, Stanton ME, Molteno CD, Burden MJ, Fuller DS, Hoyme HE, Robinson LK, Khaole N & Jacobson JL. (2008). Impaired eyeblink conditioning in children with fetal alcohol syndrome. Alcohol. Clin. Exp. Res. , 32, 365-72. PMID: 18162064 DOI.
Rothstein J, Heazlewood R & Fraser M. (2007). Health of Aboriginal and Torres Strait Islander children in remote Far North Queensland: findings of the Paediatric Outreach Service. Med. J. Aust. , 186, 519-21. PMID: 17516899
Stoller KP. (2005). Quantification of neurocognitive changes before, during, and after hyperbaric oxygen therapy in a case of fetal alcohol syndrome. Pediatrics , 116, e586-91. PMID: 16166387 DOI.
Endres M, Toso L, Roberson R, Park J, Abebe D, Poggi S & Spong CY. (2005). Prevention of alcohol-induced developmental delays and learning abnormalities in a model of fetal alcohol syndrome. Am. J. Obstet. Gynecol. , 193, 1028-34. PMID: 16157106 DOI.
Hoyme HE, May PA, Kalberg WO, Kodituwakku P, Gossage JP, Trujillo PM, Buckley DG, Miller JH, Aragon AS, Khaole N, Viljoen DL, Jones KL & Robinson LK. (2005). A practical clinical approach to diagnosis of fetal alcohol spectrum disorders: clarification of the 1996 institute of medicine criteria. Pediatrics , 115, 39-47. PMID: 15629980 DOI.
Search Pubmed
June 2010 "fetal alcohol syndrome" All (3475) Review (611) Free Full Text (396) "fetal alcohol spectrum disorders" All (306) Review (65) Free Full Text (84)
Search Pubmed: fetal alcohol syndrome | fetal alcohol effects | fetal alcohol spectrum disorders
Search OMIM: Alcoholism
Results - Alcohol Dependence
Books on Fetal Alcohol Syndrome
A selection of recent general public information books on FAS and children with FAS, available from various internet commercial suppliers (search using the book title). Please note that this listing does not reflect an endorsement of the book or its content and is provided for educational purposes only.
- The Challenge of Fetal Alcohol Syndrome, by Ann Streissguth (editor) and Jonathan Kanter (editor)
- Recognizing and Managing Children With Fetal Alcohol Syndrome-Fetal Alcohol Effects, by Brenda McCreight
- Fetal Alcohol Syndrome, Fetal Alcohol Effects: Strategies for Professionals, by Diane Malbin
- Fetal Alcohol Syndrome: A Guide for Families and Communities, by Ann Pytkowicz Streissguth
- The Best I Can Be: Living with Fetal Alcohol Syndrome-Effects, by Liz Kulp and Jodee Kulp
- The Broken Cord, by Michael Dorris
- Our FAScinating Journey: Keys to Brain Potential Along the Path of Prental Brain Injury, by Jodee Kulp
- Fantastic Antone Grows Up: Adolescents and Adults With Fetal Alcohol Syndrome, by Judith Kleinfeld (editor), Barbara Morse (editor) and Siobhan Wescott (editor)
Internet supplier link: Amazon
External Links
External Links Notice - The dynamic nature of the internet may mean that some of these listed links may no longer function. If the link no longer works search the web with the link text or name. Links to any external commercial sites are provided for information purposes only and should never be considered an endorsement. UNSW Embryology is provided as an educational resource with no clinical information or commercial affiliation.
- Medline Plus Fetal Alcohol Syndrome
- Australia
- Fetal alcohol spectrum disorders: a review of interventions for prevention and management in Indigenous communities AIHW resource sheet Feb2015
- The Medical Journal of Australia Health of Aboriginal and Torres Strait Islander children in remote Far North Queensland: findings of the Paediatric Outreach Service (Australia)
- Australian guidelines to reduce health risks from drinking alcohol | Brochure - If you are pregnant ... the safest option is not to drink alcohol PDF
- Fetal Alcohol Syndrome: National Workshop, 2002 Report (Australia) (PDF document)
- Telethon Institute for Child Health Research - FAS (Australia)
- National Organisation for Foetal Alcohol Syndrome and Related Disorders (Australia)
- USA
- University of Washington FAS Diagnostic and Prevention Network
- USA CDC - FASD
- spectrum-disorders-toolkit/Pages/default.aspx American Academy of Pediatrics – FASD toolkit[
- AMERICAN ACADEMY OF PEDIATRICS Policy Statement Fetal Alcohol Syndrome and Fetal Alcohol Effects (RE9310) Pediatrics Volume 91, Number 5 May, 1993, p1004-1006
- National Organization on FAS (USA)
- National Institute on Alcohol Abuse and Alcoholism (NIAAA, USA) Alcohol-Related Birth Defects,The Past, Present and Future
- Fetal Alcohol Spectrum Disorders Study Group (FASDSG)
- Research Monographs on Drug Exposed Women and their Children. (NIDA, USA)
- American Academy of Family Physicians Fetal Alcohol Spectrum Disorders Article (2005)
- Addiction Resources, Information, Utilization & Mission (ARIUM, USA)
- UK
- Substance Abuse and Mental Health Services Administration
- The Asante Centre
Glossary Links
- Glossary: A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | Numbers | Symbols | Term Link
Cite this page: Hill, M.A. (2024, April 26) Embryology Abnormal Development - Fetal Alcohol Syndrome. Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/Abnormal_Development_-_Fetal_Alcohol_Syndrome
- © Dr Mark Hill 2024, UNSW Embryology ISBN: 978 0 7334 2609 4 - UNSW CRICOS Provider Code No. 00098G