Cardiovascular System - Transposition of the Great Vessels
| Embryology - 28 Apr 2024 |
|---|
| Google Translate - select your language from the list shown below (this will open a new external page) |
|
العربية | català | 中文 | 中國傳統的 | français | Deutsche | עִברִית | हिंदी | bahasa Indonesia | italiano | 日本語 | 한국어 | မြန်မာ | Pilipino | Polskie | português | ਪੰਜਾਬੀ ਦੇ | Română | русский | Español | Swahili | Svensk | ไทย | Türkçe | اردو | ייִדיש | Tiếng Việt These external translations are automated and may not be accurate. (More? About Translations) |
LA85.1 Transposition of the Great Arteries
| ICD-11 |
|---|
| LA85.1 Transposition of the great arteries
LA85 Congenital anomaly of an atrioventricular or ventriculo-arterial connection A congenital cardiovascular malformation in which one or more of the following connections is abnormal 1) the morphologically right atrium to the morphologically right ventricle, 2) the morphologically left atrium to the morphologically left ventricle, 3) the morphologically right ventricle to the pulmonary trunk, 4) the morphologically left ventricle to the aorta. This excludes codes for hearts with a univentricular atrioventricular connection (mitral atresia, tricuspid atresia and double inlet ventricle), as these are listed under Functionally Univentricular Heart. |
Introduction
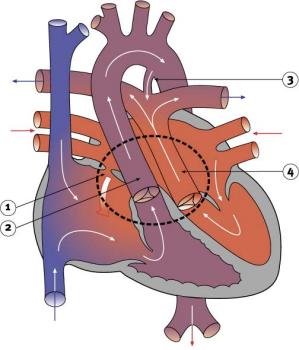
Characterized by aorta arising from right ventricle and pulmonary artery from the left ventricle and often associated with other cardiac abnormalities (e.g. ventricular septal defect).
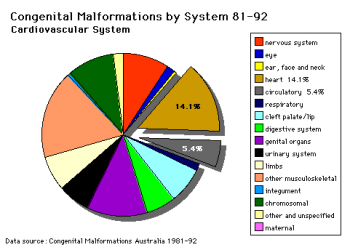
- International Classification of Diseases code 745.1
- Australian national rate (1982-1992) 3.6/10,000 births.
- Of 988 infants 4.1% were stillborn and 23.2% liveborn died during neonatal period.
- slightly more common in twin births than singleton.
- Congenital Malformations Australia 1981-1992 P. Lancaster and E. Pedisich ISSN 1321-8352
- Neonates with transposed great arteries die without an arterial switch operation, first carried out in 1975.
Some Recent Findings
|
| More recent papers |
|---|
|
This table allows an automated computer search of the external PubMed database using the listed "Search term" text link.
More? References | Discussion Page | Journal Searches | 2019 References | 2020 References Search term: Transposition of the Great Vessels | Transposition of the Great Arteries |
| Older papers |
|---|
| These papers originally appeared in the Some Recent Findings table, but as that list grew in length have now been shuffled down to this collapsible table.
See also the Discussion Page for other references listed by year and References on this current page.
|
Ultrasound
<html5media height="450" width="640">File:US Transposition Great Arteries GA36week.mp4</html5media>
Ultrasound showing Transposition Great Arteries (GA 36 weeks)
- Links: MP4 movie | Transposition of the Great Vessels | Ultrasound | International Classification of Diseases | Movies
History
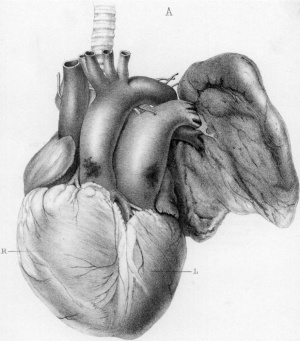
1833
The morbid anatomy of some of the most important parts of the human body (1833)[6]
- "A very singular Malformation of the Heart, in a child about two months old, came, some time ago, into my possession : the aorta arose out of the right ventricle, and the pulmonary artery out of the left. There was no communication between the one vessel and the other, except through the small remains of the ductus arteriosus, which was just large enough to admit a crow quill. The foramen ovale was a little more closed than in a child newly born. The heart was of the common size for a child of two months old, and, except for the circumstances which have been stated, it had nothing remarkable in its structure. In this child florid blood must have always been circulating between the lungs and the left side of the heart, except for the admixture of the dark blood which passed through the small communication of the foramen ovale ; and dark blood must have been always circulating between the right side of the heart and the general mass of the body, except for the very small quantity of florid blood which passed into the aorta by the remains of the ductus arteriosus. Life must, therefore, have been supported for a very considerable length of time with hardly any florid blood distributed over the body."
1863
- "The aorta arises from the fleshy part of the base of the right ventricle, at its left portion, where it presents itself in front, being quite uncovered by the pulmonary artery, and is situate between this vessel and the right auricle."[5]
Australian Statistics
Number of women who gave birth to babies with transposition of great vessels, Australia, 2002–2003
| Year | Number | Rate1 |
| 2002 | 105 | 4.3 |
| 2003 | 103 | 4.1 |
| 2002–2003 | 208 | 4.2 |
1The rate is per 10,000 women who gave birth.
Based upon Table 2.10.4 of Congenital anomalies in Australia 2002–2003.[7]
Cardiovascular Abnormalities
Heart defects and preterm birth are the most common causes of neonatal and infant death. The long-term development of the heart combined with extensive remodelling and post-natal changes in circulation lead to an abundance of abnormalities associated with this system.
A UK study literature showed that preterm infants have more than twice as many cardiovascular malformations (5.1 / 1000 term infants and 12.5 / 1000 preterm infants) as do infants born at term and that 16% of all infants with cardiovascular malformations are preterm. (0.4% of live births occur at greater than 28 weeks of gestation, 0.9% at 28 to 31 weeks, and 6% at 32 to 36 weeks. Overall, 7.3% of live-born infants are preterm)[8]
"Baltimore-Washington Infant Study data on live-born cases and controls (1981-1989) was reanalyzed for potential environmental and genetic risk-factor associations in complete atrioventricular septal defects AVSD (n = 213), with separate comparisons to the atrial (n = 75) and the ventricular (n = 32) forms of partial AVSD. ...Maternal diabetes constituted a potentially preventable risk factor for the most severe, complete form of AVSD."[9]
In addition, there are in several congenital abnormalities that exist in adults (bicuspid aortic valve, mitral valve prolapse, and partial anomalous pulmonary venous connection) which may not be clinically recognized.
References
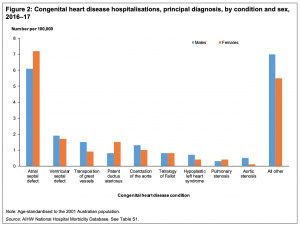
- ↑ Australian Institute of Health and Welfare 2019. Congenital heart disease in Australia. Cat. no. CDK 14. Canberra: AIHW.
- ↑ Sugiura T, Kurihara C, Kawabori M, Critsinelis AC, Civitello AB, Morgan JA & Frazier OH. (2018). Continuous-Flow Left Ventricular Assist Device Therapy in Adults with Transposition of the Great Vessels. Ann Thorac Cardiovasc Surg , , . PMID: 30101823 DOI.
- ↑ Kutty S, Danford DA, Diller GP & Tutarel O. (2018). Contemporary management and outcomes in congenitally corrected transposition of the great arteries. Heart , 104, 1148-1155. PMID: 29326110 DOI.
- ↑ Cohen MD, Johnson T & Ramrakhiani S. (2010). MRI of surgical repair of transposition of the great vessels. AJR Am J Roentgenol , 194, 250-60. PMID: 20028930 DOI.
- ↑ 5.0 5.1 Cockle J. (1863). A Case of Transposition of the Great Vessels of the Heart. Med Chir Trans , 46, 193-210.3. PMID: 20896216
- ↑ Matthew, Baillie The morbid anatomy of some of the most important parts of the human body (1833) Internet Archive
- ↑ Abeywardana S & Sullivan EA 2008. Congenital anomalies in Australia 2002–2003. Birth anomalies series no. 3 Cat. no. PER 41. Sydney: AIHW National Perinatal Statistics Unit. PDF
- ↑ Tanner K, Sabrine N & Wren C. (2005). Cardiovascular malformations among preterm infants. Pediatrics , 116, e833-8. PMID: 16322141 DOI.
- ↑ Loffredo CA, Hirata J, Wilson PD, Ferencz C & Lurie IW. (2001). Atrioventricular septal defects: possible etiologic differences between complete and partial defects. Teratology , 63, 87-93. PMID: 11241431 <87::AID-TERA1014>3.0.CO;2-5 DOI.
Reviews
Kutty S, Danford DA, Diller GP & Tutarel O. (2018). Contemporary management and outcomes in congenitally corrected transposition of the great arteries. Heart , 104, 1148-1155. PMID: 29326110 DOI.
Martins P & Castela E. (2008). Transposition of the great arteries. Orphanet J Rare Dis , 3, 27. PMID: 18851735 DOI.
Murphy DJ. (2005). Transposition of the great arteries: long-term outcome and current management. Curr Cardiol Rep , 7, 299-304. PMID: 15987628
Articles
Guven H, Billadello J & Beardslee M. (2004). An isolated single coronary artery supplying the entire myocardium in a patient with congenitally corrected transposition of the great vessels. Heart , 90, 1410. PMID: 15547014 DOI.
Formanek AG. (1990). MR imaging of congenitally corrected transposition of the great vessels in adults. AJR Am J Roentgenol , 154, 898-9. PMID: 2107695 DOI.
Hesz N & Clark EB. (1988). Cognitive development in transposition of the great vessels. Arch. Dis. Child. , 63, 198-200. PMID: 3348669
Search Pubmed
Search Pubmed: Transposition of the Great Vessels
Search OMIM: Transposition of the Great Vessels
External Links
External Links Notice - The dynamic nature of the internet may mean that some of these listed links may no longer function. If the link no longer works search the web with the link text or name. Links to any external commercial sites are provided for information purposes only and should never be considered an endorsement. UNSW Embryology is provided as an educational resource with no clinical information or commercial affiliation.
Glossary Links
- Glossary: A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | Numbers | Symbols | Term Link
Cite this page: Hill, M.A. (2024, April 28) Embryology Cardiovascular System - Transposition of the Great Vessels. Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/Cardiovascular_System_-_Transposition_of_the_Great_Vessels
- © Dr Mark Hill 2024, UNSW Embryology ISBN: 978 0 7334 2609 4 - UNSW CRICOS Provider Code No. 00098G