Cardiovascular System - Patent Ductus Arteriosus
| Embryology - 9 Mar 2026 |
|---|
| Google Translate - select your language from the list shown below (this will open a new external page) |
|
العربية | català | 中文 | 中國傳統的 | français | Deutsche | עִברִית | हिंदी | bahasa Indonesia | italiano | 日本語 | 한국어 | မြန်မာ | Pilipino | Polskie | português | ਪੰਜਾਬੀ ਦੇ | Română | русский | Español | Swahili | Svensk | ไทย | Türkçe | اردو | ייִדיש | Tiếng Việt These external translations are automated and may not be accurate. (More? About Translations) |
LA8B.4 Patent Arterial Duct
| ICD-11 |
|---|
| LA8B.4 Patent arterial duct |
| ICD-11 Structural developmental anomalies of the circulatory system (draft) |
|---|
| ICD-11 Beta Draft - NOT FINAL, updated on a daily basis, It is not approved by WHO, NOT TO BE USED for CODING except for agreed FIELD TRIALS.
20 Developmental Anomalies - Structural Developmental Anomalies Beta coding and tree structure for "structural developmental anomalies" within this section are shown in the table below. |
| Structural developmental anomalies of the circulatory system |
|
| CD-11 Beta Draft - NOT FINAL, updated on a daily basis, It is not approved by WHO, NOT TO BE USED for CODING except for agreed FIELD TRIALS.
|
Introduction
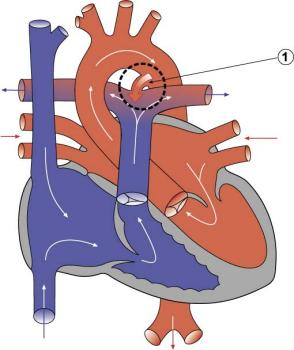
Patent ductus arteriosus (PDA), or Patent arterial duct (PAD), or common truncus, occurs commonly in preterm infants, and at approximately 1 in 2000 full term infants and more common in females (to male ratio is 2:1). Can also be associated with specific genetic defects, Trisomy 21 and Trisomy 18, and the Rubinstein-Taybi and CHARGE syndromes.
The opening is asymptomatic when the duct is small and can close spontaneously (by day three in 60% of normal term neonates), the remainder are ligated simply and with little risk, with transcatheter closure of the duct generally indicated in older children. The operation is always recommended even in the absence of cardiac failure and can often be deferred until early childhood.
- The ductus arteriosus, and its corresponding ligament, historically were described as the ductus Botallo, but should this have really been the ductus Aranzio?[1]
Some Recent Findings
|
| More recent papers |
|---|
|
This table allows an automated computer search of the external PubMed database using the listed "Search term" text link.
More? References | Discussion Page | Journal Searches | 2019 References | 2020 References Search term: Patent Ductus Arteriosus |
| Older papers |
|---|
| These papers originally appeared in the Some Recent Findings table, but as that list grew in length have now been shuffled down to this collapsible table.
See also the Discussion Page for other references listed by year and References on this current page.
|
Diagnostic Images
Cardiovascular Abnormalities
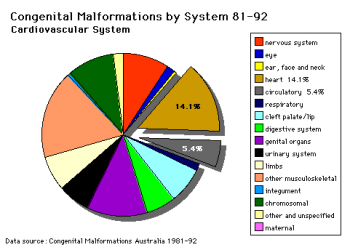
Heart defects and preterm birth are the most common causes of neonatal and infant death. The long-term development of the heart combined with extensive remodelling and post-natal changes in circulation lead to an abundance of abnormalities associated with this system.
A UK study literature showed that preterm infants have more than twice as many cardiovascular malformations (5.1 / 1000 term infants and 12.5 / 1000 preterm infants) as do infants born at term and that 16% of all infants with cardiovascular malformations are preterm. (0.4% of live births occur at greater than 28 weeks of gestation, 0.9% at 28 to 31 weeks, and 6% at 32 to 36 weeks. Overall, 7.3% of live-born infants are preterm)[8]
"Baltimore-Washington Infant Study data on live-born cases and controls (1981-1989) was reanalyzed for potential environmental and genetic risk-factor associations in complete atrioventricular septal defects AVSD (n = 213), with separate comparisons to the atrial (n = 75) and the ventricular (n = 32) forms of partial AVSD. ...Maternal diabetes constituted a potentially preventable risk factor for the most severe, complete form of AVSD." [9]
In addition, there are in several congenital abnormalities that exist in adults (bicuspid aortic valve, mitral valve prolapse, and partial anomalous pulmonary venous connection) which may not be clinically recognized.
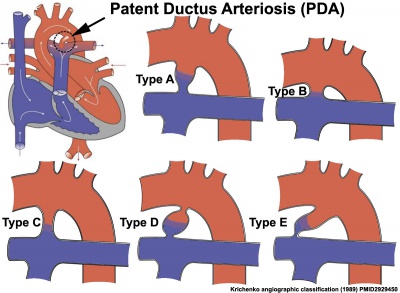
Clinical Classifications
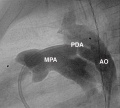
Patent Ductus Arteriosus (PDA) classification system on the basis of angiogram appearance by Krichenko (1989).[10]
|
|
A recent publication suggests a classification based on angiographic size and haemodynamic sound significance.[11]
| Type | Size | Haemodynamics |
|---|---|---|
| Silent PDA | usually less than 1.5 mm | PDA murmur not present |
| Very small PDA | less than 1.5 mm | PDA murmur present |
| Small PDA | 1.5 to 3.0 mm | PDA murmur present |
| Moderate PDA | 3 to 5 mm | PDA murmur present |
| Large PDA | greater than 5 mm | PDA murmur present |
The Aristotle Comprehensive Complexity (ACC) score has been suggested as a clinical tool for complexity adjustment in the analysis of outcome after reparative congenital heart surgery.[12][13]
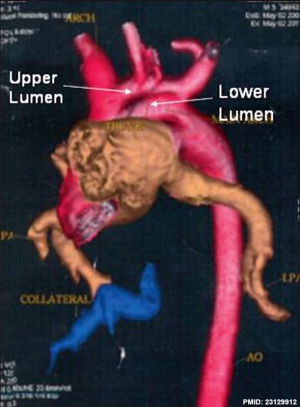
Patent Ductus Arteriosus with Persistent Fifth Aortic Arch
| Three-dimensional reconstructed computed tomography image showing left-sided patent ductus arteriosus with double-lumen aortic arch.[14]
|
|
References
- ↑ Fransson SG. (1999). The Botallo mystery. Clin Cardiol , 22, 434-6. PMID: 10376187
- ↑ Liebowitz M, Kaempf J, Erdeve O, Bulbul A, Håkansson S, Lindqvist J, Farooqi A, Katheria A, Sauberan J, Singh J, Nelson K, Wickremasinghe A, Dong L, Hassinger DC, Aucott SW, Hayashi M, Heuchan AM, Carey WA, Derrick M, Wolf IS, Kimball A, Sankar M, Leone T, Perez J, Serize A & Clyman RI. (2019). Comparative effectiveness of drugs used to constrict the patent ductus arteriosus: a secondary analysis of the PDA-TOLERATE trial (NCT01958320). J Perinatol , , . PMID: 30850756 DOI.
- ↑ Hsu KH, Wong P, Subramanyan RK, Evans J & Noori S. (2018). Predictors of Respiratory Improvement 1 Week after Ligation of Patent Ductus Arteriosus in Preterm Infants. J. Pediatr. , , . PMID: 30348438 DOI.
- ↑ Evans N. (2015). Preterm patent ductus arteriosus: A continuing conundrum for the neonatologist?. Semin Fetal Neonatal Med , 20, 272-7. PMID: 25818393 DOI.
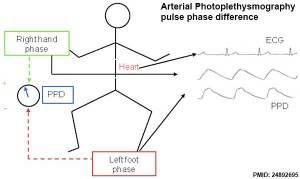
- ↑ Goudjil S, Imestouren F, Armougon A, Razafimanantsoa L, Mahmoudzadeh M, Wallois F, Leke A & Kongolo G. (2014). Noninvasive technique for the diagnosis of patent ductus arteriosus in premature infants by analyzing pulse wave phases on photoplethysmography signals measured in the right hand and the left foot. PLoS ONE , 9, e98763. PMID: 24892695 DOI.
- ↑ Ohlsson A, Walia R & Shah SS. (2013). Ibuprofen for the treatment of patent ductus arteriosus in preterm and/or low birth weight infants. Cochrane Database Syst Rev , , CD003481. PMID: 23633310 DOI.
- ↑ Ethington PN, Smith PB, Katakam L, Goldberg RN & Cotten CM. (2011). Treatment of patent ductus arteriosus with bidirectional flow in neonates. Early Hum. Dev. , 87, 381-4. PMID: 21402454 DOI.
- ↑ Tanner K, Sabrine N & Wren C. (2005). Cardiovascular malformations among preterm infants. Pediatrics , 116, e833-8. PMID: 16322141 DOI.
- ↑ Loffredo CA, Hirata J, Wilson PD, Ferencz C & Lurie IW. (2001). Atrioventricular septal defects: possible etiologic differences between complete and partial defects. Teratology , 63, 87-93. PMID: 11241431 <87::AID-TERA1014>3.0.CO;2-5 DOI.
- ↑ <pubmed>2929450</pubmed>
- ↑ Fernando R, Koranne K, Loyalka P, Kar B & Gregoric I. (2013). Patent ductus arteriosus closure using an Amplatzer(™) ventricular septal defect closure device. Exp Clin Cardiol , 18, e50-4. PMID: 24294051
- ↑ Bojan M, Gerelli S, Gioanni S, Pouard P & Vouhé P. (2011). Evaluation of a new tool for morbidity assessment in congenital cardiac surgery. Ann. Thorac. Surg. , 92, 2200-4. PMID: 22115230 DOI.
- ↑ Chang YH, Lee JY, Kim JE, Kim JY, Youn Y, Lee EJ, Moon S, Lee JY & Sung IK. (2013). The Aristotle score predicts mortality after surgery of patent ductus arteriosus in preterm infants. Ann. Thorac. Surg. , 96, 879-84. PMID: 23895892 DOI.
- ↑ Warrier D, Shah S, John C & Dayananda L. (2012). A rare association with patent ductus arteriosus. Ann Pediatr Cardiol , 5, 191-3. PMID: 23129912 DOI.
Reviews
Isayama T, Kusuda S, Reichman B, Lee SK, Lehtonen L, Norman M, Adams M, Bassler D, Helenius K, Hakansson S, Yang J, Jain A & Shah PS. (2020). Neonatal Intensive Care Unit-Level Patent Ductus Arteriosus Treatment Rates and Outcomes in Infants Born Extremely Preterm. J. Pediatr. , , . PMID: 32145968 DOI.
Sasi A & Deorari A. (2011). Patent ductus arteriosus in preterm infants. Indian Pediatr , 48, 301-8. PMID: 21532100
Articles
Yun SW. (2011). Congenital heart disease in the newborn requiring early intervention. Korean J Pediatr , 54, 183-91. PMID: 21829408 DOI.
Thébaud B & Lacaze-Mazmonteil T. (2010). Patent ductus arteriosus in premature infants: A never-closing act. Paediatr Child Health , 15, 267-70. PMID: 21532789
Search Pubmed
Search Pubmed: Patent Ductus Arteriosus
Search OMIM: Patent Ductus Arteriosus
External Links
External Links Notice - The dynamic nature of the internet may mean that some of these listed links may no longer function. If the link no longer works search the web with the link text or name. Links to any external commercial sites are provided for information purposes only and should never be considered an endorsement. UNSW Embryology is provided as an educational resource with no clinical information or commercial affiliation.
- MedlinePlus Patent Ductus Arteriosus
- OMIM 607411 Patent Ductus Arteriosus
Glossary Links
- Glossary: A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | Numbers | Symbols | Term Link
Cite this page: Hill, M.A. (2026, March 9) Embryology Cardiovascular System - Patent Ductus Arteriosus. Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/Cardiovascular_System_-_Patent_Ductus_Arteriosus
- © Dr Mark Hill 2026, UNSW Embryology ISBN: 978 0 7334 2609 4 - UNSW CRICOS Provider Code No. 00098G