| ICD-11 LA00-LA0Z Structural developmental anomalies of the nervous system
|
- LA00.0 Anencephaly - LA00.1 Iniencephaly, LA00.2 Acephaly, LA00.3 Amyelencephaly
- LA01 Cephalocele
- LA02 Spina bifida - LA02.0 Spina bifida cystica, LA02.00 Myelomeningocele with hydrocephalus, LA02.01 Myelomeningocele without hydrocephalus, LA02.02 Myelocystocele, LA02.1 Spina bifida aperta
- LA03 Arnold-Chiari malformation type II
- LA04 Congenital hydrocephalus
- LA05 Cerebral structural developmental anomalies - LA05.0 Microcephaly, LA05.1 Megalencephaly, LA05.2 Holoprosencephaly, LA05.3 Corpus callosum agenesis, LA05.4 Arhinencephaly, LA05.5 Abnormal neuronal migration, LA05.6 Encephaloclastic disorders, LA05.7 Brain cystic malformations
- LA06 Cerebellar structural developmental anomalies - LA06.0 Dandy-Walker malformation, LA06.1 Hypoplasia or agenesis of cerebellar hemispheres, LA06.2 Focal cerebellar dysplasia
- LA07 Structural developmental anomalies of the neurenteric canal, spinal cord or vertebral column
|
| View full table
|
Introduction
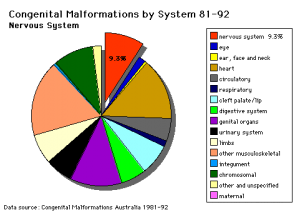
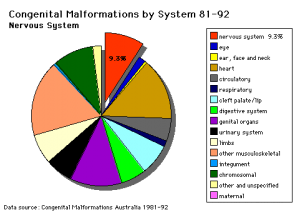
Australian abnormalities (1981-92)
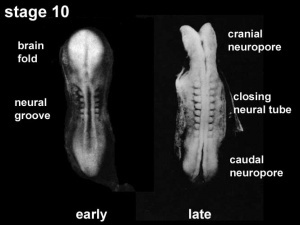
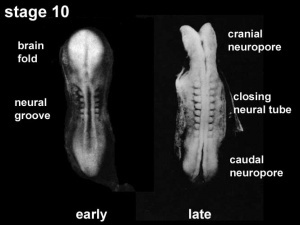
Neural groove closing to neural tube, early week 4
(
Stage 10)
There are many different congenital and environmentally derived abnormalities associated with the nervous system. There are potentially 1000's of neurological abnormalities that could be listed on this page, therefore this current page is only a very brief introduction to some of these neural abnormalities. For additional information see links at the bottom of each sub-heading. The latest ICD-11 coding now also includes a new category "LD90 Disorders of intellectual development" and also lists LA05.3 Corpus callosum agenesis as "the most common brain malformation and is characterized by total or partial absence of the main interhemispheric commissure, the corpus callosum."
As the nervous system continues to develop fetally and postnatally, environmental issues both before and after birth are relevant to neural development. Embryonic and fetal nutrition folate (required early for neural tube closure) and iodine (required later for neural growth and differentiation). The developmental environment can also impact upon neural growth; maternal drugs such as alcohol and heavy metals such as lead (mining, historically both petrol and paint). Finally, postnatally other sensory abnormalities (hearing) can also impact on achieving developmental milestones.

|
Huntington's disease (HD) is an adult onset inherited neurodegenerative disorder affecting both the striatum and cerebral cortex. A recent mouse model study of this disease[1] has demonstrated a developmental cortical hyperexcitability, suggesting that there may also be a developmental component to this disease. More? 2011 Student project
|
- Links: neural tube defect
Some Recent Findings
- Quantitative Folding Pattern Analysis of Early Primary Sulci in Human Fetuses with Brain Abnormalities[2] "Aberrant gyral folding is a key feature in the diagnosis of many cerebral malformations. However, in fetal life, it is particularly challenging to confidently diagnose aberrant folding because of the rapid spatiotemporal changes of gyral development. Currently, there is no resource to measure how an individual fetal brain compares with normal spatiotemporal variations. In this study, we assessed the potential for automatic analysis of early sulcal patterns to detect individual fetal brains with cerebral abnormalities. ... Automated analysis of interrelated patterning of early primary sulci could outperform the traditional gyrification index and has the potential to quantitatively detect individual fetuses with emerging abnormal sulcal patterns."
- The Lateral Temporal Lobe in Early Human Life[3] "Abnormalities of lateral temporal lobe development are associated with a spectrum of genetic and environmental pathologic processes, but more normative data are needed for a better understanding of gyrification in this brain region. Here, we begin to establish guidelines for the analysis of the lateral temporal lobe in humans in early life. We present quantitative methods for measuring gyrification at autopsy using photographs of the gross brain and simple computer-based quantitative tools in a cohort of 28 brains ranging in age from 27 to 70 postconceptional weeks (end of infancy). We provide normative ranges for different indices of gyrification and identify a constellation of qualitative features that should also be considered in these analyses. The ratio of the temporal area to the whole brain area increased dramatically in the second half of gestation, but then decelerated after birth before increasing linearly around 50 postconceptional weeks. Tertiary gyrification continued beyond birth in a linear process through infancy with considerable variation in patterns. Analysis of 2 brains with gyral disorders of the lateral temporal lobe demonstrated proof-of-principle that the proposed methods are of diagnostic value. These guidelines are proposed for assessments of temporal lobe pathology in pediatric brains in early life. "
|
| More recent papers
|
|
This table allows an automated computer search of the external PubMed database using the listed "Search term" text link.
- This search now requires a manual link as the original PubMed extension has been disabled.
- The displayed list of references do not reflect any editorial selection of material based on content or relevance.
- References also appear on this list based upon the date of the actual page viewing.
References listed on the rest of the content page and the associated discussion page (listed under the publication year sub-headings) do include some editorial selection based upon both relevance and availability.
More? References | Discussion Page | Journal Searches | 2019 References | 2020 References
Search term: Abnormal Neural Development
|
| Older papers
|
| These papers originally appeared in the Some Recent Findings table, but as that list grew in length have now been shuffled down to this collapsible table.
See also the Discussion Page for other references listed by year and References on this current page.
- Identification of PCSK9 as a novel serum biomarker for the prenatal diagnosis of neural tube defects using iTRAQ quantitative proteomics[4] "To identify candidate serum molecule biomarkers for the non-invasive early prenatal diagnosis of neural tube defects (NTDs), we employed an iTRAQ-based quantitative proteomic approach to analyze the proteomic changes in serum samples from embryonic day (E) 11 and E13 pregnant rats with spina bifida aperta (SBA) induced by all-trans retinoic acid. ...We observed the space-time expression changes of proprotein convertase subtilisin/kexin type 9 (PCSK9) at different stages of fetal development, including a marked decrease in the sera of NTD pregnancies and gradual increase in the sera of normal pregnancies with embryonic development."
- Mutations in genes encoding the glycine cleavage system predispose to neural tube defects in mice and humans[4] "Function of folate one-carbon metabolism (FOCM) has been implicated as a key determinant of susceptibility to NTDs. The glycine cleavage system (GCS) is a multi-enzyme component of mitochondrial folate metabolism, and GCS-encoding genes therefore represent candidates for involvement in NTDs. To investigate this possibility, we sequenced the coding regions of the GCS genes: AMT, GCSH and GLDC in NTD patients and controls. ... Overall, our findings suggest that loss-of-function mutations in GCS genes predispose to NTDs in mice and humans. These data highlight the importance of adequate function of mitochondrial folate metabolism in neural tube closure." Prenatal Diagnosis
- A randomized trial of prenatal versus postnatal repair of myelomeningoce[5] "Prenatal repair of myelomeningocele, the most common form of spina bifida, may result in better neurologic function than repair deferred until after delivery. We compared outcomes of in utero repair with standard postnatal repair. ....Prenatal surgery for myelomeningocele reduced the need for shunting and improved motor outcomes at 30 months but was associated with maternal and fetal risks. (Funded by the National Institutes of Health; ClinicalTrials.gov number, NCT00060606.)." (see also paper comments)
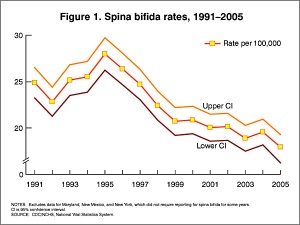
- Australia 1998–2005[6] "944 births over this period affected by NTD. Of these births, 523 were live births and 421 were fetal deaths (still births and terminations after 20 weeks gestation). This equates to a prevalence of neural tube defects (NTD) among births of 4.6 per 10,000."
|
Neural Tube Closure
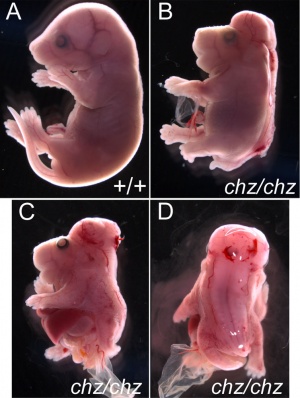
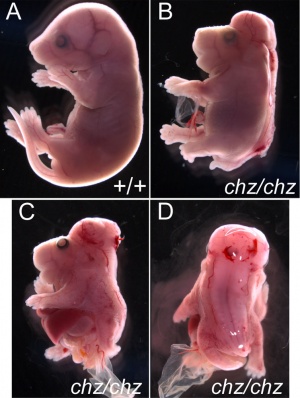
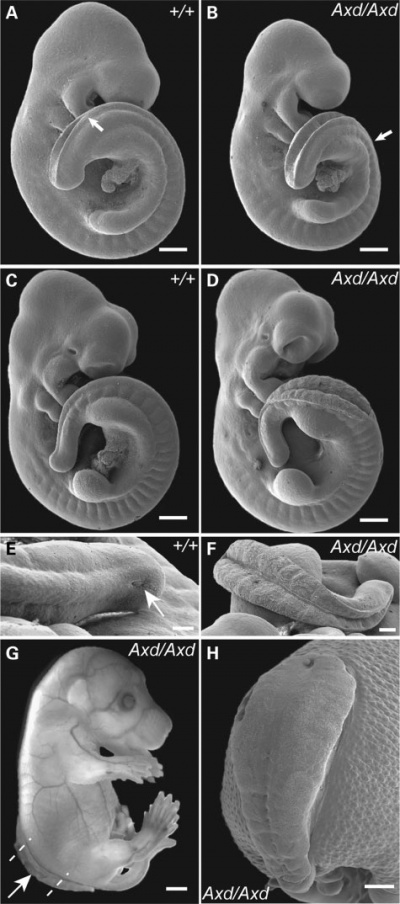
Mouse mutant showing neural tube closure defect
Dysraphism is the term often used to describe the defective fusion of the neural folds. The position and degree of failure of fusion will result in either embryonic death or a range of different neural defects. The way (mode) in which the human neural tube fuses has been a source of contention. In humans, fusion appears to initiate at multiple sites along the neural groove[7][8], this mode of closure may differ from that found in many animal species used in developmental studies.
Human Embryonic Death:
- 5 weeks with total failure of fusion.
- 6.5 weeks with opening over the rhombencephalon.
- survive beyond 7 weeks with a defect at the frontal and parietal regions.
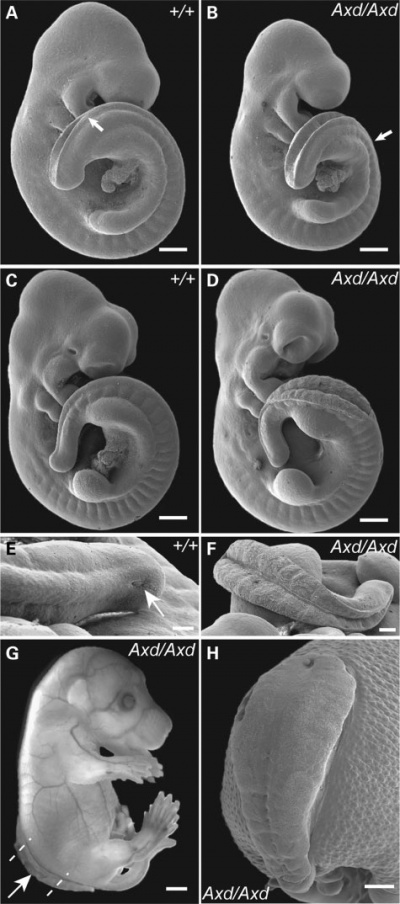
Mouse posterior neuropore Axd mutant[9]
- Links: Folic Acid and Neural Tube Defects
Spina Bifida

Spina Bifida and Anencephaly (dorsal view)
| ICD-11 LA02 Spina bifida
|
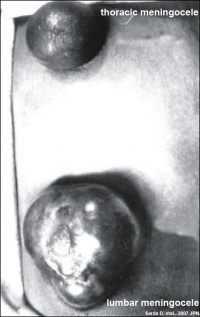
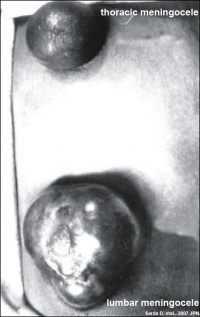
- LA02.0 Spina bifida cystica - failure of the neural tube to correctly develop during the antenatal period. This condition is characterized by nerve damage and the presence of meningoceles on the back. This condition may present with physical or mental impairment.
- LA02.00 Myelomeningocele with hydrocephalus - failure of the neural tube to correctly develop during the antenatal period. This condition is characterized by nerve damage and hydrocephalus. This condition may also present with syringomyelia, hip dislocation, headache, nausea, vomiting, blurry vision, balance problems, bladder control problems, meningitis, or mental impairment.
- LA02.01 Myelomeningocele without hydrocephalus - failure of the neural tube to close completely during fetal development. This condition is characterized by nerve damage. This condition may also present with syringomyelia, hip dislocation, headache, nausea, vomiting, blurry vision, balance problems, bladder control problems, meningitis, or mental impairment.
- LA02.02 Myelocystocele - failure of the neural tube to close completely during fetal development. The condition is characterized by skin covered lumbosacral masses, an arachnoid lined meningocele that is directly continuous with the spinal subarachnoid space, and a low lying hydromyelic spinal cord that traverses the meningocele and expands into a large terminal cyst. This condition can present with neural damage and consequent impairment of function below the site of the myelocystocele.
- LA02.1 Spina bifida aperta - failure of the neural tube to correctly develop during the antenatal period. This condition is characterized by nerve damage originating from a known location in the spine, signified by the presence of a meningocele or myelomeningocele. This condition may present with physical or mental impairment.
|
| spina bifida | neural abnormalities | ICD-11
|
(Meningomyelocele)
|
Double meningomyelocele[10]
|

|
|
| Meningomyelocele
|
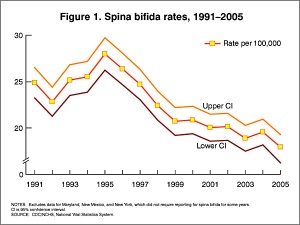
Spina Bifida Rates (USA Data)
|
There are potentially many different causes of spina bifida and neural tube defects. The basis of the abnormality is a failure of the neural tube to close caudally. At least one known cause is a low maternal diet of folic acid (folate) containing foods. (see Neural Tube Defects and Low Folic Acid or Folic Acid below)
Neural tube defects from failure to close can be screened by amniocentesis or ultrasound.
Alpha-fetoproetin normally present in the CSF, leaks and can be detected in amniotic fluid.
Neural Tube Defects - Potential risk factors
| Maternal nutrition
|
Alcohol use, Caffeine use, low folic acid, Low dietary quality, Elevated glycaemic load or index, Low methionine intake, Low serum choline level, Low serum vitamin B12 level, Low vitamin C level, Low zinc intake
|
| Other maternal factors
|
smoking, maternal hyperthermia, Low socio-economic status, Maternal infections and illnesses (TORCH, viral infection, bacterial infection, fungal infection), maternal diabetes, Pregestational obesity, Psychosocial stress, Valproic acid use
|
| Environmental factors
|
Ambient air pollution, Disinfectant by-products in drinking water, Indoor air pollution, Nitrate-related compounds, Organic solvents, Pesticides, Polycyclic aromatic hydrocarbons
|
| Table data from review[11] (see original review for references)
|
- Links: neural tube defect
Cephalic Disorders
Cephalic (Greek, kephale = head) are a large group of abnormalities that relate to both skeletal (skull) and neural (brain) associated defects including: anencephaly, hydrocephalus, encephalocele, colpocephaly (occipital horn enlargement), lissencephaly (smooth brain), porencephaly (cyst or cavity in cerebral hemisphere), acephaly (absence of head), exencephaly (brain outside skull), macrocephaly (large head), micrencephaly (small brain), otocephaly (absence of lower jaw), brachycephaly (premature fusion of coronal suture), oxycephaly (premature fusion of coronal suture + other), plagiocephaly (premature unilateral fusion of coronal or lambdoid sutures), scaphocephaly (premature fusion of sagittal suture), trigonocephaly.
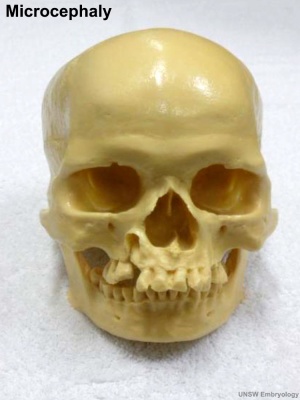
Microcephaly
|
Template:ICD11 LA05.0 Microcephaly - A condition caused by failure of the head to correctly develop during the antenatal period. This condition is characterized by a head size that is significantly smaller than normal for their age and sex. This condition may also present with developmental delays, difficulties with balance and coordination, short stature, hyperactivity, mental retardation, seizures, or other neurological abnormalities.
|
A recent Spanish study[12] has shown a concordance between a head circumference growth function and intellectual disability in relation with the cause of microcephaly.
- "3,269 head circumference (HC) charts of patients from a tertiary neuropediatric unit were reviewed and 136 microcephalic participants selected. Using the Z-scores of registered HC measurements we defined the variables: HC Minimum, HC Drop and HC Catch-up. We classified patients according to the presence or absence of intellectual disability (IQ below 71) and according to the cause of microcephaly (idiopathic, familial, syndromic, symptomatic and mixed). Using Discriminant Analysis a C-function was defined as C=HC Minimum + HC Drop with a cut-off level of C=-4.32 Z-score. In our sample 95% of patients scoring below this level, severe microcephaly, were classified in the disabled group while the overall concordance was 66%. In the symptomatic-mixed group the concordance between HC function and outcome reached 82% in contrast to only 54% in the idiopathic-syndromic group (P-value=0.0002)."
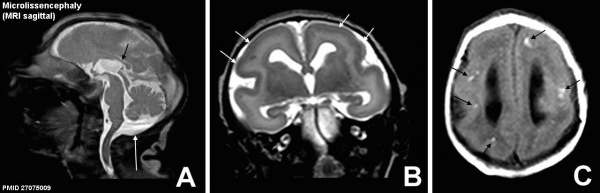
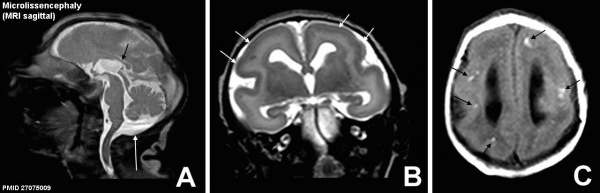
Microlissencephaly (MRI)[13] - Zika virus associated lishencephaly (smooth brain) in combination with severe congenital microcephaly (small head).
Anencephaly
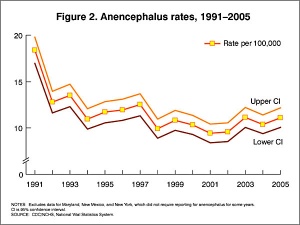
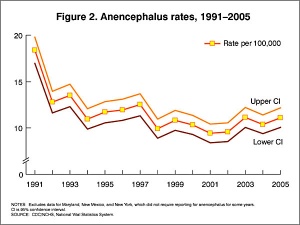
Anencephaly Rates (USA Data)
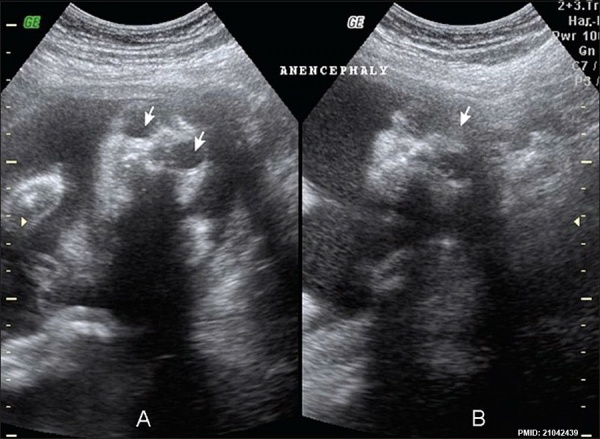
[14]A neural tube defect, anencephaly is a failure of the neural tube to close cranially. Also called exencephaly or craniorachischisis. (More? anencephaly)
| ICD-11 LA00.0 Anencephaly
|
a neural tube defect, characterized by the total or partial absence of the cranial vault and the covering skin, the brain being missing or reduced to a small mass. Most cases are stillborn, although some infants have been reported to survive for a few hours. In most cases autopsy findings reveal absence of adrenal glands. Anencephaly is likely to be multifactorial, the result of gene-environment interactions. Familial cases with a seemingly autosomal recessive mode of inheritance have been described but most cases are sporadic. Folic acid and zinc deficiencies, as well as maternal obesity, have been shown to be risk factors.
- LA00.1 Iniencephaly - a rare form of neural tube defect in which a malformation of the cervico-occipital junction is associated with a malformation of the central nervous system. The cardinal features are occipital bone defect, partial or total absence of cervicothoracic vertebrae, fetal retroflexion of the head and characteristic absence of the neck. It is associated with malformations of the central nervous (spina bifida and/or anencephaly), gastrointestinal (omphalocele) and cardiovascular systems.
- LA00.2 Acephaly
- LA00.3 Amyelencephaly - Amyelencephaly is the absence of both the brain and spinal cord.
LA01 Cephalocele - failure of the skull to correctly close during the antenatal period. This condition is characterized by herniation of the meninges. This condition may present with herniation of brain, or developmental delay. Confirmation is through observation of herniated meninges by imaging.
|
| anencephaly | neural abnormalities | ICD-11
|
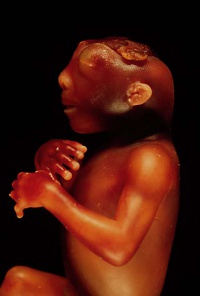
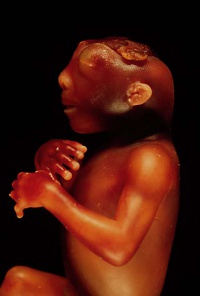
| Fetal Anencephaly
|

|
|
| ventral view
|
lateral view
|
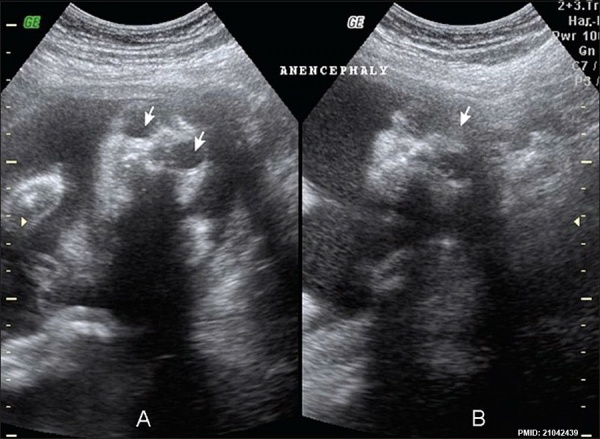
Anencephaly in a fetus (GA week 18) from a diabetic mother. Ultrasound images (coronal) show a complete absence of the cranial vault and brain and enlarged orbits.[15]
- Links: anencephaly | maternal diabetes
Cerebral Anomalies
| ICD-11 LA05 Cerebral structural developmental anomalies
|
- LA05.0 Microcephaly - failure of the head to correctly develop during the antenatal period. This condition is characterized by a head size that is significantly smaller than normal for their age and sex. This condition may also present with developmental delays, difficulties with balance and coordination, short stature, hyperactivity, mental retardation, seizures, or other neurological abnormalities.
- LA05.1 Megalencephaly - failure of the brain to correctly develop during the antenatal period. This condition is characterized by increased size or weight of an otherwise correctly formed brain. This condition may also present with seizures, motor deficits, mental retardation and mild cognitive impairment.
- LA05.2 Holoprosencephaly - brain malformation resulting from incomplete cleavage of the prosencephalon, occurring between the 18th and the 28th day of gestation and affecting both the forebrain and the face. In most of the cases, facial anomalies are observed: cyclopia, proboscis and median or bilateral cleft lip/palate in severe forms, and ocular hypotelorism or solitary median maxillary central incisor in minor forms. These latter midline defects can occur without the cerebral malformations (microforms). Children with HPE have many medical problems: developmental delay and feeding difficulties, epilepsy, and instability of temperature, heart rate and respiration. Endocrine disorders like diabetes insipidus, adrenal hypoplasia, hypogonadism, thyroid hypoplasia and growth hormone deficiency are frequent.
- LA05.3 Corpus callosum agenesis - the most common brain malformation and is characterized by total or partial absence of the main interhemispheric commissure, the corpus callosum.
- LA05.4 Arhinencephaly - failure of the olfactory organs to correctly develop during the antenatal period. This condition is characterized by absence of the olfactory bulbs and tracts.
- LA05.5 Abnormal neuronal migration - any condition caused by abnormal migration of neuronal cells during the antenatal period. These conditions may present with poor muscle tone and motor function, seizures, developmental delays, mental retardation, failure to grow and thrive, difficulties with feeding, swelling in the extremities or microcephaly.
- LA05.6 Encephaloclastic disorders
- LA05.7 Brain cystic malformations - A disease caused by expansion of the roof plate of the brain vesicle, or by extraaxial structures such as an arachnoid membrane or migrating ependymal cells. This disease is characterized by the presence of fluid filled cysts in the brain. This disease may present with asymmetry of the skull, brain compression, raised intracranial pressure, hydrocephalus, bleeding or seizures. This disease may also be asymptomatic. Confirmation is through observation of intracerebral cysts by imaging.
|
| cerebral anomalies | neural abnormalities | ICD-11
|
Holoprosencephaly
ICD-11 LA05 Cerebral structural developmental anomalies - LA05.2 Holoprosencephaly
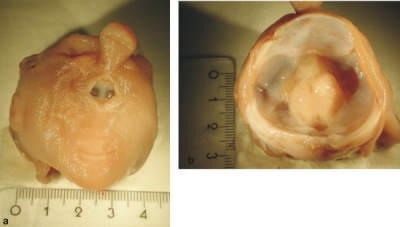
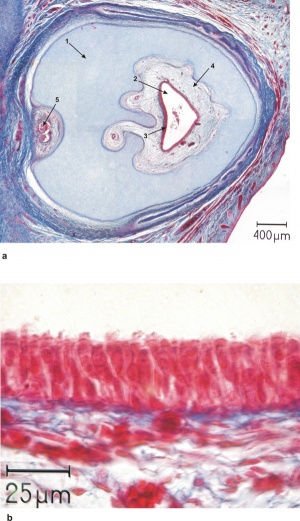
Below are shown images of fetal holoprosencephaly and associated cyclopia.[16]
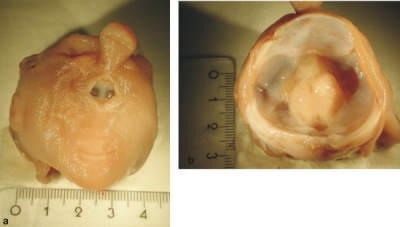
|
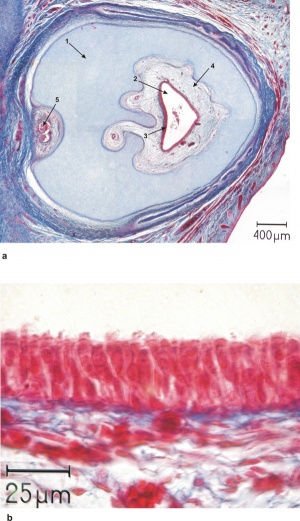
|
| Human holoprosencephaly cyclopean dissection
|
Proboscis histology
|
Hydrocephalus
Hydrocephalus (historic image from Hess, 1922)
This is a defect of cerebrospinal fliud (CSF) flow, excess fluid production or impaired fluid absorption and can be congenital or acquired. Estimated incidence of 1 in 1000 live births the condition leads to enlarged ventricles and head, separated skull cranial sutures and fontanelles. Obstruction of CSF flow can occur at any time (prenatally or postnatally) and leads to accumulation of within the ventricles. The time of onset will have different effects and should be compared to the equilivant neurological events that are occuring.
Ventricular obstruction usually occurs at the level of the cerebral aqueduct (narrowest site), but can occur elsewhere, and can be caused by viral infection or zoonotic disease.
- Links: Congenital Hydrocephalus
Dandy Walker malformation
| Dandy Walker malformation (MRI)[17] is another form of ventricular abnormality that affects cerebellar development.
The vermis of the cerebellum can be small or absent, the fourth ventricle enlarges due to cyst formation.
An ultrasound study[18] of fetuses with Dandy-Walker malformation 13 to 16 weeks (GA 15-18 weeks) identified the fourth ventricle widely open posteriorly, even in the standard transcerebellar view, and the brainstem-vermis (BV) angle was > 45°, significantly increased compared to that in normal fetuses (P < 0.0001). Note that at this age, an open fourth ventricle can also found in about 10% of normal fetuses.
Named after Walter Dandy (1886 – 1946) and Arthur Earl Walker (1907 – 1995), two USA neurosurgeons.
|

|
- Links: Congenital Hydrocephalus
Encephalocele
This defect is generally mesodermal in origin, leading to protrusion of brain and meninges outside the crainal cavity. The severity of the disorder can vary dependent upon the degree of mesodermal abnormality.
Encephalitis
Normally a postnatal clinical syndrome of the central nervous system resulting in inflammation of the brain parenchyma and caused by a range of pathogens (viral, bacterial and protozoal infections). This infectious disease is due mainly to viral pathogens: Herpes simplex encephalitis 10%–20% of cases, Murray Valley encephalitis virus, Japanese encephalitis virus, Australian bat lyssavirus, West Nile virus, Hendra virus and Nipah virus. The pathogen is generally included in the specific encephalitis naming; Varicella encephalitis and Toxoplasma meningoencephalitis.
- Links: neural abnormalities | TORCH | PMC2700670)
Fragile X Syndrome
Fragile X Syndrome (FXS) is the most common form of inherited mental retardation and autism. The condition is caused by a loss of the functional fragile X mental retardation protein (FMRP) an RNA-binding protein that can regulate the translation of specific mRNAs. There are several suggested additional roles for this protein including synaptic development and function[19] and in adult neurogenesis.[20]
- Links: Fragile X Syndrome
Autism
Autism (autism spectrum disorder, ASD) is a behaviourally defined brain disorder in children. Features include: impoverished verbal and non-verbal communication skills, reduced social interactions (bias their attention towards objects rather than the surrounding social situation), behavioural impairments in attention engagement/disengagement, poor emotional discrimination and facial recognition, and fail to response to their own names. There exist many different and unproven claims as to the origins of autism.
Developmentally associated with neural maturation changes in cortical thickness and organization, and particularly affecting pyramidal neurons. A rat model shows structural and behavioural features of autism as a result of altering the trajectory of early postnatal cortical development.[21]
- Links: Neural Exam Movies
Rett Syndrome
(RTT) A severe neurodevelopment disorder, with intellectual disability and abnormalities of movement, mainly caused by mutations in the X-linked (Xq28) Methyl-CpG-binding protein 2 (MECP2) gene and therefore almost exclusively in females. The congenital variant of Rett syndrome is caused by heterozygous mutation in the FOXG1 gene on chromosome 14q13.
- Links: OMIM - Congenital Rett syndrome | OMIM - Rett syndrome
Cerebral Palsy
| ICD-11 Cerebral palsy
|
8D20 Spastic cerebral palsy - characterized by increased muscle tone associated with hyperactive muscle stretch reflexes (deep tendon reflexes) and an increase in resistance to rapid muscle stretch. Extensor plantar responses are commonly present.
- 8D20.0 Spastic unilateral cerebral palsy - a form of cerebral palsy in which the spasticity is confined to one side; it is often accompanied by cortical sensory impairment and varying degrees of hemineglect, demonstrable by testing stereognosis and graphesthesia. Early hand preference is often the first sign of this disorder, and may be apparent in the first months of life.
- 8D20.1 Spastic bilateral cerebral palsy
- 8D21 Dyskinetic cerebral palsy - (extrapyramidal cerebral palsy) is characterized by impairment of voluntary movement because of the presence of interfering involuntary movements, and inappropriate co-contraction of agonist and antagonist muscles (dystonia). This group of disorders includes choreoathetotic cerebral palsy and dystonic cerebral palsy. The former is characterized by large amplitude, involuntary movements of mainly distal limbs(athetosis) with or without small amplitude, fleeting, asymmetric contractions of individual muscle groups (chorea). Dystonic cerebral palsy predominantly affects proximal trunk and limb muscles, which may show slow, persistent movements, leading to the adoption of unusual postures, such as torticollis.
- 8D22 Ataxic cerebral palsy - dominated by signs of cerebellar dysfunction, including hypotonia, ataxia, dysdiadochokinesis, dysmetria, dysarthria and nystagmus. Reflexes may be pendular, although there are often also signs of spasticity.
- 8D23 Worster-Drought syndrome - a form of cerebral palsy characterized by congenital pseudobulbar (suprabulbar) paresis manifesting as selective weakness of the lips, tongue and soft palate, dysphagia, dysphonia, drooling and jaw jerking.
|
| International Classification of Diseases - Cerebral palsy
|
| ICD-11 Cerebral palsy
|
8D20 Spastic cerebral palsy - characterized by increased muscle tone associated with hyperactive muscle stretch reflexes (deep tendon reflexes) and an increase in resistance to rapid muscle stretch. Extensor plantar responses are commonly present.
- 8D20.0 Spastic unilateral cerebral palsy - a form of cerebral palsy in which the spasticity is confined to one side; it is often accompanied by cortical sensory impairment and varying degrees of hemineglect, demonstrable by testing stereognosis and graphesthesia. Early hand preference is often the first sign of this disorder, and may be apparent in the first months of life.
- 8D20.1 Spastic bilateral cerebral palsy
- 8D21 Dyskinetic cerebral palsy - (extrapyramidal cerebral palsy) is characterized by impairment of voluntary movement because of the presence of interfering involuntary movements, and inappropriate co-contraction of agonist and antagonist muscles (dystonia). This group of disorders includes choreoathetotic cerebral palsy and dystonic cerebral palsy. The former is characterized by large amplitude, involuntary movements of mainly distal limbs(athetosis) with or without small amplitude, fleeting, asymmetric contractions of individual muscle groups (chorea). Dystonic cerebral palsy predominantly affects proximal trunk and limb muscles, which may show slow, persistent movements, leading to the adoption of unusual postures, such as torticollis.
- 8D22 Ataxic cerebral palsy - dominated by signs of cerebellar dysfunction, including hypotonia, ataxia, dysdiadochokinesis, dysmetria, dysarthria and nystagmus. Reflexes may be pendular, although there are often also signs of spasticity.
- 8D23 Worster-Drought syndrome - a form of cerebral palsy characterized by congenital pseudobulbar (suprabulbar) paresis manifesting as selective weakness of the lips, tongue and soft palate, dysphagia, dysphonia, drooling and jaw jerking.
|
|
Cerebral palsy is a group of disorders in motor impairment that limits activity, and is attributed to non-progressive disturbances during brain development in fetuses or infants (3-4 / 1,000).[22]
Represented by one or more of these features:
- impaired cognition
- impaired communication
- impaired sensory perception
- behavioural abnormalities
- seizure disorders
- Links: Neural Exam Movies | Medline Plus | NINDS - Info | CDC Screening and Diagnosis | Cerebral Palsy Alliance
Newborn Neural Exam
Neural - The collapsed tables below link to a number of short videos that demonstrate simple assessments of the postnatal developing nervous system.

- Links: Neural Exam Movies | Neural Exam Movies -Newborn Abnormal
International Classification of Disease
| International Classification of Diseases ICD-11 Neural developmental anomalies
|
| ICD-11 LA00-LA0Z Structural developmental anomalies of the nervous system
|
- LA00.0 Anencephaly - a neural tube defect, characterized by the total or partial absence of the cranial vault and the covering skin, the brain being missing or reduced to a small mass. Most cases are stillborn, although some infants have been reported to survive for a few hours. In most cases autopsy findings reveal absence of adrenal glands. Anencephaly is likely to be multifactorial, the result of gene-environment interactions. Familial cases with a seemingly autosomal recessive mode of inheritance have been described but most cases are sporadic. Folic acid and zinc deficiencies, as well as maternal obesity, have been shown to be risk factors.
- LA00.1 Iniencephaly - a rare form of neural tube defect in which a malformation of the cervico-occipital junction is associated with a malformation of the central nervous system. The cardinal features are occipital bone defect, partial or total absence of cervicothoracic vertebrae, fetal retroflexion of the head and characteristic absence of the neck. It is associated with malformations of the central nervous (spina bifida and/or anencephaly), gastrointestinal (omphalocele) and cardiovascular systems.
- LA00.2 Acephaly
- LA00.3 Amyelencephaly - Amyelencephaly is the absence of both the brain and spinal cord.
- LA01 Cephalocele - failure of the skull to correctly close during the antenatal period. This condition is characterized by herniation of the meninges. This condition may present with herniation of brain, or developmental delay. Confirmation is through observation of herniated meninges by imaging.
- LA02 Spina bifida -
- LA02.0 Spina bifida cystica - failure of the neural tube to correctly develop during the antenatal period. This condition is characterized by nerve damage and the presence of meningoceles on the back. This condition may present with physical or mental impairment.
- LA02.00 Myelomeningocele with hydrocephalus - failure of the neural tube to correctly develop during the antenatal period. This condition is characterized by nerve damage and hydrocephalus. This condition may also present with syringomyelia, hip dislocation, headache, nausea, vomiting, blurry vision, balance problems, bladder control problems, meningitis, or mental impairment.
- LA02.01 Myelomeningocele without hydrocephalus - failure of the neural tube to close completely during fetal development. This condition is characterized by nerve damage. This condition may also present with syringomyelia, hip dislocation, headache, nausea, vomiting, blurry vision, balance problems, bladder control problems, meningitis, or mental impairment.
- LA02.02 Myelocystocele - failure of the neural tube to close completely during fetal development. The condition is characterized by skin covered lumbosacral masses, an arachnoid lined meningocele that is directly continuous with the spinal subarachnoid space, and a low lying hydromyelic spinal cord that traverses the meningocele and expands into a large terminal cyst. This condition can present with neural damage and consequent impairment of function below the site of the myelocystocele.
- LA02.1 Spina bifida aperta - failure of the neural tube to correctly develop during the antenatal period. This condition is characterized by nerve damage originating from a known location in the spine, signified by the presence of a meningocele or myelomeningocele. This condition may present with physical or mental impairment.
- LA03 Arnold-Chiari malformation type II - failure of the brain and spinal cord to correctly develop during the antenatal period. This condition is characterized by extension of both cerebellar and brain stem tissue into the foramen magnum. This condition may present with partial or complete absence of the cerebellar vermis, myelomeningocele, neck pain, balance problems, muscle weakness, limb numbness, dizziness, vision problems, difficulty swallowing, ringing in the ears, hearing loss, vomiting, insomnia, depression, or impairment of motor skills.
- LA04 Congenital hydrocephalus - failure of the brain to correctly develop during the antenatal period. This condition is characterized by a rapid increase in head circumference or an unusually large head size due to excessive accumulation of cerebrospinal fluid in the brain. This condition may also present with vomiting, sleepiness, irritability, downward deviation of the eyes, or seizures. Confirmation is through observation of cerebrospinal fluid within cerebral ventricles by imaging.
- LA05 Cerebral structural developmental anomalies
- LA05.0 Microcephaly
- LA05.1 Megalencephaly
- LA05.2 Holoprosencephaly
- LA05.3 Corpus callosum agenesis
- LA05.4 Arhinencephaly
- LA05.5 Abnormal neuronal migration
- LA05.6 Encephaloclastic disorders
- LA05.7 Brain cystic malformations
- LA06 Cerebellar structural developmental anomalies
- LA06.0 Dandy-Walker malformation
- LA06.1 Hypoplasia or agenesis of cerebellar hemispheres
- LA06.2 Focal cerebellar dysplasia
- LA07 Structural developmental anomalies of the neurenteric canal, spinal cord or vertebral column
|
|
| International Classification of Diseases - Spina bifida
|
| ICD-11 LA02 Spina bifida
|
- LA02.0 Spina bifida cystica - failure of the neural tube to correctly develop during the antenatal period. This condition is characterized by nerve damage and the presence of meningoceles on the back. This condition may present with physical or mental impairment.
- LA02.00 Myelomeningocele with hydrocephalus - failure of the neural tube to correctly develop during the antenatal period. This condition is characterized by nerve damage and hydrocephalus. This condition may also present with syringomyelia, hip dislocation, headache, nausea, vomiting, blurry vision, balance problems, bladder control problems, meningitis, or mental impairment.
- LA02.01 Myelomeningocele without hydrocephalus - failure of the neural tube to close completely during fetal development. This condition is characterized by nerve damage. This condition may also present with syringomyelia, hip dislocation, headache, nausea, vomiting, blurry vision, balance problems, bladder control problems, meningitis, or mental impairment.
- LA02.02 Myelocystocele - failure of the neural tube to close completely during fetal development. The condition is characterized by skin covered lumbosacral masses, an arachnoid lined meningocele that is directly continuous with the spinal subarachnoid space, and a low lying hydromyelic spinal cord that traverses the meningocele and expands into a large terminal cyst. This condition can present with neural damage and consequent impairment of function below the site of the myelocystocele.
- LA02.1 Spina bifida aperta - failure of the neural tube to correctly develop during the antenatal period. This condition is characterized by nerve damage originating from a known location in the spine, signified by the presence of a meningocele or myelomeningocele. This condition may present with physical or mental impairment.
|
| spina bifida | neural abnormalities | ICD-11
|
|
| International Classification of Diseases - Anencephaly
|
| ICD-11 LA00.0 Anencephaly
|
a neural tube defect, characterized by the total or partial absence of the cranial vault and the covering skin, the brain being missing or reduced to a small mass. Most cases are stillborn, although some infants have been reported to survive for a few hours. In most cases autopsy findings reveal absence of adrenal glands. Anencephaly is likely to be multifactorial, the result of gene-environment interactions. Familial cases with a seemingly autosomal recessive mode of inheritance have been described but most cases are sporadic. Folic acid and zinc deficiencies, as well as maternal obesity, have been shown to be risk factors.
- LA00.1 Iniencephaly - a rare form of neural tube defect in which a malformation of the cervico-occipital junction is associated with a malformation of the central nervous system. The cardinal features are occipital bone defect, partial or total absence of cervicothoracic vertebrae, fetal retroflexion of the head and characteristic absence of the neck. It is associated with malformations of the central nervous (spina bifida and/or anencephaly), gastrointestinal (omphalocele) and cardiovascular systems.
- LA00.2 Acephaly
- LA00.3 Amyelencephaly - Amyelencephaly is the absence of both the brain and spinal cord.
LA01 Cephalocele - failure of the skull to correctly close during the antenatal period. This condition is characterized by herniation of the meninges. This condition may present with herniation of brain, or developmental delay. Confirmation is through observation of herniated meninges by imaging.
|
| anencephaly | neural abnormalities | ICD-11
|
|
| International Classification of Diseases - Cerebral structural developmental anomalies
|
| ICD-11 LA05 Cerebral structural developmental anomalies
|
- LA05.0 Microcephaly - failure of the head to correctly develop during the antenatal period. This condition is characterized by a head size that is significantly smaller than normal for their age and sex. This condition may also present with developmental delays, difficulties with balance and coordination, short stature, hyperactivity, mental retardation, seizures, or other neurological abnormalities.
- LA05.1 Megalencephaly - failure of the brain to correctly develop during the antenatal period. This condition is characterized by increased size or weight of an otherwise correctly formed brain. This condition may also present with seizures, motor deficits, mental retardation and mild cognitive impairment.
- LA05.2 Holoprosencephaly - brain malformation resulting from incomplete cleavage of the prosencephalon, occurring between the 18th and the 28th day of gestation and affecting both the forebrain and the face. In most of the cases, facial anomalies are observed: cyclopia, proboscis and median or bilateral cleft lip/palate in severe forms, and ocular hypotelorism or solitary median maxillary central incisor in minor forms. These latter midline defects can occur without the cerebral malformations (microforms). Children with HPE have many medical problems: developmental delay and feeding difficulties, epilepsy, and instability of temperature, heart rate and respiration. Endocrine disorders like diabetes insipidus, adrenal hypoplasia, hypogonadism, thyroid hypoplasia and growth hormone deficiency are frequent.
- LA05.3 Corpus callosum agenesis - the most common brain malformation and is characterized by total or partial absence of the main interhemispheric commissure, the corpus callosum.
- LA05.4 Arhinencephaly - failure of the olfactory organs to correctly develop during the antenatal period. This condition is characterized by absence of the olfactory bulbs and tracts.
- LA05.5 Abnormal neuronal migration - any condition caused by abnormal migration of neuronal cells during the antenatal period. These conditions may present with poor muscle tone and motor function, seizures, developmental delays, mental retardation, failure to grow and thrive, difficulties with feeding, swelling in the extremities or microcephaly.
- LA05.6 Encephaloclastic disorders
- LA05.7 Brain cystic malformations - A disease caused by expansion of the roof plate of the brain vesicle, or by extraaxial structures such as an arachnoid membrane or migrating ependymal cells. This disease is characterized by the presence of fluid filled cysts in the brain. This disease may present with asymmetry of the skull, brain compression, raised intracranial pressure, hydrocephalus, bleeding or seizures. This disease may also be asymptomatic. Confirmation is through observation of intracerebral cysts by imaging.
|
| cerebral anomalies | neural abnormalities | ICD-11
|
|
| International Classification of Diseases - Cerebral palsy
|
| ICD-11 Cerebral palsy
|
8D20 Spastic cerebral palsy - characterized by increased muscle tone associated with hyperactive muscle stretch reflexes (deep tendon reflexes) and an increase in resistance to rapid muscle stretch. Extensor plantar responses are commonly present.
- 8D20.0 Spastic unilateral cerebral palsy - a form of cerebral palsy in which the spasticity is confined to one side; it is often accompanied by cortical sensory impairment and varying degrees of hemineglect, demonstrable by testing stereognosis and graphesthesia. Early hand preference is often the first sign of this disorder, and may be apparent in the first months of life.
- 8D20.1 Spastic bilateral cerebral palsy
- 8D21 Dyskinetic cerebral palsy - (extrapyramidal cerebral palsy) is characterized by impairment of voluntary movement because of the presence of interfering involuntary movements, and inappropriate co-contraction of agonist and antagonist muscles (dystonia). This group of disorders includes choreoathetotic cerebral palsy and dystonic cerebral palsy. The former is characterized by large amplitude, involuntary movements of mainly distal limbs(athetosis) with or without small amplitude, fleeting, asymmetric contractions of individual muscle groups (chorea). Dystonic cerebral palsy predominantly affects proximal trunk and limb muscles, which may show slow, persistent movements, leading to the adoption of unusual postures, such as torticollis.
- 8D22 Ataxic cerebral palsy - dominated by signs of cerebellar dysfunction, including hypotonia, ataxia, dysdiadochokinesis, dysmetria, dysarthria and nystagmus. Reflexes may be pendular, although there are often also signs of spasticity.
- 8D23 Worster-Drought syndrome - a form of cerebral palsy characterized by congenital pseudobulbar (suprabulbar) paresis manifesting as selective weakness of the lips, tongue and soft palate, dysphagia, dysphonia, drooling and jaw jerking.
|
|
| ICD-11 Conditions with disorders of intellectual development as a relevant clinical feature
|
LD90 Conditions with disorders of intellectual development as a relevant clinical feature
- LD90.0 Angelman syndrome
- LD90.1 Early-onset parkinsonism - intellectual deficit
- LD90.2 Pelizaeus-Merzbacher-like disease
- LD90.3 Prader-Willi syndrome
- LD90.4 Rett syndrome
- 5C55.01 Lesch-Nyhan syndrome
- LA04.0 Hydrocephalus with stenosis of the aqueduct of Sylvius
- 8A44.0 Pelizaeus-Merzbacher disease
- 8C21.2 Hereditary sensory or autonomic neuropathy type IV
- LD20.00 Joubert syndrome
- 5C50.0 Phenylketonuria
- 5C50.12 Tyrosinaemia type 2
- 5C50.A1 Carbamoylphosphate synthetase deficiency
- 5C50.F1 Carnosinaemia
- 5C50.F2 Homocarnosinosis
- LD20.1 Syndromes with lissencephaly as a major feature
- 5C52.03 Sjögren-Larsson syndrome
- LA05.50 Polymicrogyria
- LA05.60 Porencephaly
- 5C53.02 Pyruvate dehydrogenase complex deficiency
- CB04.5 Brain-lung-thyroid syndrome
- 5C56.02 Metachromatic leukodystrophy
- 5C56.1 Neuronal ceroid lipofuscinosis
- 5C56.31 Mucopolysaccharidosis type 2
- 5C56.33 Mucopolysaccharidosis type 6
- 5C60.0 Oculocerebrorenal syndrome
- LD44.N0 CATCH 22 phenotype
- LD24.80 Langer-Giedion syndrome
- 5C58.00 Crigler-Najjar syndrome
- LD55 Fragile X chromosome
- LD27.00 Incontinentia pigmenti
- LD2D.2 Tuberous sclerosis
- LD2F.15 Noonan syndrome
- KA62.8 Congenital rubella syndrome
- KA62.3 Congenital cytomegalovirus infection
- LD40.0 Complete trisomy 21
- LD50.31 Klinefelter syndrome, male with more than two X chromosomes
|
- LD90.Y Other specified conditions with disorders of intellectual development as a relevant clinical feature
- LD90.Z Conditions with disorders of intellectual development as a relevant clinical feature, unspecified
|
| LD9Y Other specified developmental anomalies
LD9Z Developmental anomalies, unspecified
|
| neural abnormalities
|
| International Classification of Diseases ICD-11 20 Developmental anomalies (beta draft)
|
| ICD-11 Beta Draft - NOT FINAL, updated on a daily basis, It is not approved by WHO, NOT TO BE USED for CODING except for agreed FIELD TRIALS.
Chapter 20 Developmental anomalies, only a few examples of the draft ICD-11 Beta coding and tree structure for "structural developmental anomalies" within this section are shown in the table below.
|
| Mortality and Morbidity Statistics - 20 Developmental Anomalies
|
Structural Developmental Anomalies
- Structural developmental anomalies of the nervous system
- LA00 Anencephaly or similar anomalies
- LA01 Cephalocele
- LA02 Spina bifida
- LA03 Arnold-Chiari malformation type II
- LA04 Congenital hydrocephalus
- LA05 Cerebral structural developmental anomalies
- LA06 Cerebellar structural developmental anomalies
- LA07 Structural developmental anomalies of the neurenteric canal, spinal cord or vertebral column
- LA0Y Other specified structural developmental anomalies of the nervous system
- LA0Z Structural developmental anomalies of the nervous system, unspecified
- Structural developmental anomalies of the eye, eyelid or lacrimal apparatus
- LA10 Structural developmental anomalies of ocular globes
- LA11 Structural developmental anomalies of the anterior segment of eye
- LA30 Structural developmental anomalies of lens or zonula
- LA31 Structural developmental anomalies of the posterior segment of eye
- LA32 Structural developmental anomalies of eyelid, lacrimal apparatus or orbit
- LA3Y Other specified structural developmental anomalies of the eye, eyelid or lacrimal apparatus
- LA3Z Structural developmental anomalies of the eye, eyelid or lacrimal apparatus, unspecified
- Structural developmental anomalies of the ear
- LA40 Structural anomaly of eustachian apparatus
- LA41 Minor anomalies of pinnae
- LA42 Structural developmental anomalies of ear causing hearing impairment
- LA43 Otocephaly
- LA44 Accessory auricle
- LA4Y Other specified structural developmental anomalies of the ear
- LA4Z Structural developmental anomalies of the ear, unspecified
- Structural developmental anomalies of the face, mouth or teeth
- LA50 Structural developmental anomalies of teeth and periodontal tissues
- LA51 Structural developmental anomalies of mouth or tongue
- Clefts of lip, alveolus or palate
- LA70 Congenital velopharyngeal incompetence
- LA71 Facial clefts
- LA72 Facial asymmetry
- LA73 Macrocheilia
- LA74 Microcheilia
- LA75 Compression facies
- LA76 Pierre Robin syndrome
- LC20 Dermoid cyst
- LA7Y Other specified structural developmental anomalies of the face, mouth or teeth
- LA7Z Structural developmental anomalies of the face, mouth or teeth, unspecified
- Structural developmental anomalies of the neck
- Structural developmental anomalies of the respiratory system
- Structural developmental anomalies of the circulatory system
- Structural developmental anomaly of heart and great vessels
- LB00 Congenital heart or great vessel related acquired abnormality
- LB01 Congenital anomaly of atrioventricular or ventriculo-arterial connections
- LB02 Congenital anomaly of the mediastinal veins Congenital anomaly of atria or atrial septum
- LB20 Congenital anomaly of atrioventricular valves or septum
- LB21 Congenital anomaly of ventricles and ventricular septum
- LB22 Functionally univentricular heart
- LB23 Congenital anomaly of ventriculo-arterial valves and adjacent regions
- LB24 Congenital anomaly of great arteries including arterial duct
- LB25 Anomalous position-orientation of heart
- LB26 Total mirror imagery
- LB27 Left isomerism
- LB28 Congenital anomaly of coronary arteries
- LB29 Structural developmental anomalies of the pericardium
- LB2Y Other specified structural developmental anomaly of heart and great vessels
- LB2Z Structural developmental anomaly of heart and great vessels, unspecified
- LB30 Structural developmental anomalies of the peripheral vascular system
- LB30.1 Capillary malformations
- LB30.2 Lymphatic malformations
- LB30.21 Macrocystic lymphatic malformation
- LB30.22 Microcystic lymphatic malformation
- LB30.23 Cystic hygroma in fetus
- BD23.1 Primary lymphoedema
- EK91 Yellow nail syndrome
- LC5F.26 Noonan syndrome
- LB30.2Y Other specified lymphatic malformations
- LB30.2Z Lymphatic malformations, unspecified
- LB30.3 Peripheral venous malformations
- LB30.4 Peripheral arteriovenous malformations
- LB30.5 Peripheral arterial malformations
- LB30.6 Pulmonary arteriovenous fistula
- LB30.Y Other specified structural developmental anomalies of the peripheral vascular system
- LB30.Z Structural developmental anomalies of the peripheral vascular system, unspecified
- LB3Y Other specified structural developmental anomalies of the circulatory system
- LB3Z Structural developmental anomalies of the circulatory system, unspecified
- Structural developmental anomalies of the diaphragm, abdominal wall or umbilical cord
- Structural developmental anomalies of the digestive tract
- Structural developmental anomalies of the liver, biliary tract, pancreas or spleen
- Structural developmental anomalies of the urinary system
- Structural developmental anomalies of the female genital system
- Structural developmental anomalies of the male genital system
- Structural developmental anomalies of the breast
- Structural developmental anomalies of the skeleton
- Structural developmental anomalies of the skin
- Structural developmental anomalies of the adrenal glands
|
| Multiple developmental anomalies or syndromes
|
| Chromosomal anomalies, excluding gene mutations
|
| Conditions with disorders of intellectual development as a relevant clinical feature
|
| LD6Y Other specified developmental anomalies
LD6Z Developmental anomalies, unspecified
|
| CD-11 Beta Draft - NOT FINAL, updated on a daily basis, It is not approved by WHO, NOT TO BE USED for CODING except for agreed FIELD TRIALS.
See also International Classification of Diseases
ICD-10
|
References
- ↑ Cepeda C, Oikonomou KD, Cummings D, Barry J, Yazon VW, Chen DT, Asai J, Williams CK & Vinters HV. (2019). Developmental origins of cortical hyperexcitability in Huntington's disease: Review and new observations. J. Neurosci. Res. , 97, 1624-1635. PMID: 31353533 DOI.
- ↑ Im K, Guimaraes A, Kim Y, Cottrill E, Gagoski B, Rollins C, Ortinau C, Yang E & Grant PE. (2017). Quantitative Folding Pattern Analysis of Early Primary Sulci in Human Fetuses with Brain Abnormalities. AJNR Am J Neuroradiol , 38, 1449-1455. PMID: 28522661 DOI.
- ↑ Goldstein IS, Erickson DJ, Sleeper LA, Haynes RL & Kinney HC. (2017). The Lateral Temporal Lobe in Early Human Life. J. Neuropathol. Exp. Neurol. , 76, 424-438. PMID: 28498956 DOI.
- ↑ 4.0 4.1 Narisawa A, Komatsuzaki S, Kikuchi A, Niihori T, Aoki Y, Fujiwara K, Tanemura M, Hata A, Suzuki Y, Relton CL, Grinham J, Leung KY, Partridge D, Robinson A, Stone V, Gustavsson P, Stanier P, Copp AJ, Greene ND, Tominaga T, Matsubara Y & Kure S. (2012). Mutations in genes encoding the glycine cleavage system predispose to neural tube defects in mice and humans. Hum. Mol. Genet. , 21, 1496-503. PMID: 22171071 DOI.
- ↑ Adzick NS, Thom EA, Spong CY, Brock JW, Burrows PK, Johnson MP, Howell LJ, Farrell JA, Dabrowiak ME, Sutton LN, Gupta N, Tulipan NB, D'Alton ME & Farmer DL. (2011). A randomized trial of prenatal versus postnatal repair of myelomeningocele. N. Engl. J. Med. , 364, 993-1004. PMID: 21306277 DOI.
- ↑ Abeywardana S & Sullivan EA 2008. Neural tube defects in Australia. An epidemiological report. Cat. no. PER 45. Sydney: AIHW National Perinatal Statistics Unit | PDF.
- ↑ Van Allen MI, Kalousek DK, Chernoff GF, Juriloff D, Harris M, McGillivray BC, Yong SL, Langlois S, MacLeod PM & Chitayat D. (1993). Evidence for multi-site closure of the neural tube in humans. Am. J. Med. Genet. , 47, 723-43. PMID: 8267004 DOI.
- ↑ Nakatsu T, Uwabe C & Shiota K. (2000). Neural tube closure in humans initiates at multiple sites: evidence from human embryos and implications for the pathogenesis of neural tube defects. Anat. Embryol. , 201, 455-66. PMID: 10909899
- ↑ Brouns MR, De Castro SC, Terwindt-Rouwenhorst EA, Massa V, Hekking JW, Hirst CS, Savery D, Munts C, Partridge D, Lamers W, Köhler E, van Straaten HW, Copp AJ & Greene ND. (2011). Over-expression of Grhl2 causes spina bifida in the Axial defects mutant mouse. Hum. Mol. Genet. , 20, 1536-46. PMID: 21262862 DOI.
- ↑ Sarda D, Kothari P, Laddha A, Kulkarni B. Double meningomyelocele: Embryogenesis. J Pediatr Neurosci [serial online] 2007 [cited 2013 Mar 22];2:26-7. Available from: http://www.pediatricneurosciences.com/text.asp?2007/2/1/26/32004
- ↑ Copp AJ, Adzick NS, Chitty LS, Fletcher JM, Holmbeck GN & Shaw GM. (2015). Spina bifida. Nat Rev Dis Primers , 1, 15007. PMID: 27189655 DOI.
- ↑ Coronado R, Macaya Ruíz A, Giraldo Arjonilla J & Roig-Quilis M. (2015). [Concordance between a head circumference growth function and intellectual disability in relation with the cause of microcephaly]. An Pediatr (Barc) , 83, 109-16. PMID: 25534043 DOI.
- ↑ de Fatima Vasco Aragao M, van der Linden V, Brainer-Lima AM, Coeli RR, Rocha MA, Sobral da Silva P, Durce Costa Gomes de Carvalho M, van der Linden A, Cesario de Holanda A & Valenca MM. (2016). Clinical features and neuroimaging (CT and MRI) findings in presumed Zika virus related congenital infection and microcephaly: retrospective case series study. BMJ , 353, i1901. PMID: 27075009
- ↑ Mathews TJ. Trends in spina bifida and anencephalus in the United States, 1991-2005, National Vital Statistics System.
- ↑ Alorainy IA, Barlas NB & Al-Boukai AA. (2010). Pictorial Essay: Infants of diabetic mothers. Indian J Radiol Imaging , 20, 174-81. PMID: 21042439 DOI.
- ↑ Arnold WH & Meiselbach V. (2009). 3-D reconstruction of a human fetus with combined holoprosencephaly and cyclopia. Head Face Med , 5, 14. PMID: 19563629 DOI.
- ↑ Saleem SN. (2014). Fetal MRI: An approach to practice: A review. J Adv Res , 5, 507-23. PMID: 25685519 DOI.
- ↑ Contro E, Volpe P, De Musso F, Muto B, Ghi T, De Robertis V & Pilu G. (2014). Open fourth ventricle prior to 20 weeks' gestation: a benign finding?. Ultrasound Obstet Gynecol , 43, 154-8. PMID: 24151160 DOI.
- ↑ Bassell GJ & Warren ST. (2008). Fragile X syndrome: loss of local mRNA regulation alters synaptic development and function. Neuron , 60, 201-14. PMID: 18957214 DOI.
- ↑ Luo Y, Shan G, Guo W, Smrt RD, Johnson EB, Li X, Pfeiffer RL, Szulwach KE, Duan R, Barkho BZ, Li W, Liu C, Jin P & Zhao X. (2010). Fragile x mental retardation protein regulates proliferation and differentiation of adult neural stem/progenitor cells. PLoS Genet. , 6, e1000898. PMID: 20386739 DOI.
- ↑ Chomiak T, Karnik V, Block E & Hu B. (2010). Altering the trajectory of early postnatal cortical development can lead to structural and behavioural features of autism. BMC Neurosci , 11, 102. PMID: 20723245 DOI.
- ↑ Aisen ML, Kerkovich D, Mast J, Mulroy S, Wren TA, Kay RM & Rethlefsen SA. (2011). Cerebral palsy: clinical care and neurological rehabilitation. Lancet Neurol , 10, 844-52. PMID: 21849165 DOI.
Calloni SF, Caschera L & Triulzi FM. (2019). Disorders of Ventral Induction/Spectrum of Holoprosencephaly. Neuroimaging Clin. N. Am. , 29, 411-421. PMID: 31256862 DOI.
Journals
Journal of Pediatric Neurosciences - is official publication of the Indian Society for Pediatric Neurosurgery.
Search PubMed
Search term: Neural Development Abnormalities | Anencephaly | Hydrocephalus | Encephalocele | Holoprosencephaly | Autism
Glossary Links
- Glossary: A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | Numbers | Symbols | Term Link
Cite this page: Hill, M.A. (2026, March 8) Embryology Neural System - Abnormalities. Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/Neural_System_-_Abnormalities
- What Links Here?
- © Dr Mark Hill 2026, UNSW Embryology ISBN: 978 0 7334 2609 4 - UNSW CRICOS Provider Code No. 00098G