Abnormal Development - Syphilis
| Embryology - 28 Apr 2024 |
|---|
| Google Translate - select your language from the list shown below (this will open a new external page) |
|
العربية | català | 中文 | 中國傳統的 | français | Deutsche | עִברִית | हिंदी | bahasa Indonesia | italiano | 日本語 | 한국어 | မြန်မာ | Pilipino | Polskie | português | ਪੰਜਾਬੀ ਦੇ | Română | русский | Español | Swahili | Svensk | ไทย | Türkçe | اردو | ייִדיש | Tiếng Việt These external translations are automated and may not be accurate. (More? About Translations) |
| Educational Use Only - Embryology is an educational resource for learning concepts in embryological development, no clinical information is provided and content should not be used for any other purpose. |
Introduction
The variety of bacterial infections that can occur during pregnancy is as variable as the potential developmental effects, from virtually insignificant to major developmental, abortive or fatal in outcome. Some bacteria are common and are part of the normal genital tract flora (Lactobacillus sp), while other bacterial infections are less common or even rare and initially infect/transmit by air or fluids through the different epithelia (genital tract, lungs, gastrointestinal tract). The genitally transmitted common sexually transmitted diseases (STDs) are the bacterial infections described as syphilis and gonorrhoea.
In the USA before 1989, reported cases of congenital syphilis (CS) were defined and classified on the basis of a set of clinical and serologic features known as the "Kaufman criteria". In 1988, the CDC developed a new surveillance case definition "All infants born to mothers who have untreated or inadequately treated syphilis are considered potentially infected. (This criterion is based on the 70%-100% chance that during the first 4 years of infection, an untreated woman will transmit syphilis to her unborn baby)."[1]
| Bacterial Links: bacterial infection | syphilis | gonorrhea | tuberculosis | listeria | salmonella | TORCH | Environmental | Category:Bacteria |
Some Recent Findings
|
| More recent papers |
|---|
|
This table allows an automated computer search of the external PubMed database using the listed "Search term" text link.
More? References | Discussion Page | Journal Searches | 2019 References | 2020 References Search term: Abnormal Development Syphilis | Congenital Syphilis |
| Older papers |
|---|
| These papers originally appeared in the Some Recent Findings table, but as that list grew in length have now been shuffled down to this collapsible table.
See also the Discussion Page for other references listed by year and References on this current page.
|
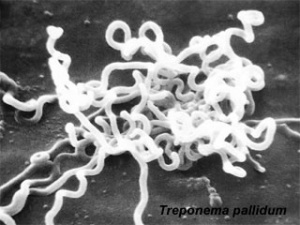
Treponema Pallidum
Lineage
- Bacteria; Spirochaetes; Spirochaetes (class); Spirochaetales; Spirochaetaceae; Treponema; Treponema pallidum; Treponema pallidum subsp. pallidum;
- Treponema pallidum subsp. pallidum SS14
- Treponema pallidum subsp. pallidum str. Nichols
Congenital Syphilis
The following information is based upon the 2003 CDC Surveillance Case Definition for Congenital Syphilis.[1]
Confirmed case
Congenital syphilis is an infant or child in whom Treponema pallidum is identified by darkfield microscopy, direct fluorescent antibody, or other specific stains in specimens from lesions, placenta, umbilical cord, or autopsy material.
Presumptive case
Congenital syphilis is either of the following:
- A. any infant whose mother had untreated or inadequately treated1 syphilis at the time of delivery, regardless of the findings in the infant or child
- B. any infant or child who has a reactive treponemal test for syphilis and any one of the following:
- evidence of congenital syphilis on physical examination
- evidence of congenital syphilis on long bone X-ray
- reactive cerebrospinal fluid CSF-VDRL
- elevated CSF cell count or protein (without other cause)
- reactive test for IgM antibody.
Syphilitic Stillbirth
Defined as a fetal death in which the mother had untreated or inadequately treated syphilis at the time of delivery of a fetus after a 20-week gestation or of a fetus weighing >500g.
Signs of Congenital Syphilis
| In an infant or a child younger than 2 years of age | In an older child |
|---|---|
|
|
Australian Data
The following data is based upon a table from a recent article by Jones and Jones (2010),[8] reminding physicians to be aware of maternal and congenital syphilis.
The following data is based upon a table from a recent article by Jones and Jones (2010)[9] reminding physicians to be aware of maternal and congenital syphilis.
| Year | Syphilis | Congenital syphilis | ||||||
|---|---|---|---|---|---|---|---|---|
| Male | Female | Total | Male | Female | Unknown | Total | ||
| 2007 | 1231 | 150 | 1381 | 5 | 2 | 1 | 8 | |
| 2006 | 689 | 182 | 871 | 6 | 7 | - | 13 | |
| 2005 | - | - | 653 | 8 | 6 | 1 | 15 | |
| 2004 | - | - | 636 | 11 | 2 | - | 13 | |
| Table data[9]
| ||||||||
Gram Stain
Bacterial staining procedure named after Hans Christian Gram (1853 - 1938). Generally divides bacteria into either:
- Gram-positive bacteria purple crystal violet stain is trapped by layer of peptidoglycan (forms outer layer of the cell).
- Gram-negative bacteria outer membrane prevents stain from reaching peptidoglycan layer in the periplasm, outer membrane then permeabilized and pink safranin counterstain is trapped by peptidoglycan layer.
Historic Embryology
There is a chapter in the 1921 Contributions to Embryology publication Studies on Abortuses: A Survey of Pathologic Ova in the Carnegie Embryological Collection specifically related to syphilis.
Chapter 17. Changes Suggestive of Lues By A. W. Meyer
- "Since Schaudin's discovery, attention naturally has been directed very largely from placental lesions of syphilis to the presence of spirochsetse. But unfortunately the hope that the presence of this organism would form not only a crucial but also an infallible criterion for the determination of fetal lues does not seem to have been realized. The search for spirochsetee seems to have been attended by such uncertain results that a routine examination of the placenta has not even been recommended by prominent obstetricians."
| Historic Disclaimer - information about historic embryology pages |
|---|
| Pages where the terms "Historic" (textbooks, papers, people, recommendations) appear on this site, and sections within pages where this disclaimer appears, indicate that the content and scientific understanding are specific to the time of publication. This means that while some scientific descriptions are still accurate, the terminology and interpretation of the developmental mechanisms reflect the understanding at the time of original publication and those of the preceding periods, these terms, interpretations and recommendations may not reflect our current scientific understanding. (More? Embryology History | Historic Embryology Papers) |
References
- ↑ 1.0 1.1 Congenital Syphilis Case Investigation and Reporting Form Instructions PDF
- ↑ Rowe CR, Newberry DM & Jnah AJ. (2018). Congenital Syphilis: A Discussion of Epidemiology, Diagnosis, Management, and Nurses' Role in Early Identification and Treatment. Adv Neonatal Care , 18, 438-445. PMID: 30020089 DOI.
- ↑ Kittipornpechdee N, Hanamornroongruang S, Lekmak D & Treetipsatit J. (2018). Fetal and Placental Pathology in Congenital Syphilis: A Comprehensive Study in Perinatal Autopsy. Fetal Pediatr Pathol , 37, 231-242. PMID: 30207805 DOI.
- ↑ Rac MW, Bryant SN, McIntire DD, Cantey JB, Twickler DM, Wendel GD & Sheffield JS. (2014). Progression of ultrasound findings of fetal syphilis after maternal treatment. Am. J. Obstet. Gynecol. , 211, 426.e1-6. PMID: 24907700 DOI.
- ↑ Shahrook S, Mori R, Ochirbat T & Gomi H. (2014). Strategies of testing for syphilis during pregnancy. Cochrane Database Syst Rev , , CD010385. PMID: 25352226 DOI.
- ↑ Blencowe H, Cousens S, Kamb M, Berman S & Lawn JE. (2011). Lives Saved Tool supplement detection and treatment of syphilis in pregnancy to reduce syphilis related stillbirths and neonatal mortality. BMC Public Health , 11 Suppl 3, S9. PMID: 21501460 DOI.
- ↑ Zhu L, Qin M, Du L, Xie RH, Wong T & Wen SW. (2010). Maternal and congenital syphilis in Shanghai, China, 2002 to 2006. Int. J. Infect. Dis. , 14 Suppl 3, e45-8. PMID: 20137991 DOI.
- ↑ <pubmed>20618256</pubmed>
- ↑ 9.0 9.1 Jones IS & Jones AI. (2010). We keep forgetting maternal and congenital syphilis. Aust N Z J Obstet Gynaecol , 50, 306-7. PMID: 20618256 DOI.
Reviews
Rac MW, Revell PA & Eppes CS. (2017). Syphilis during pregnancy: a preventable threat to maternal-fetal health. Am. J. Obstet. Gynecol. , 216, 352-363. PMID: 27956203 DOI.
Shahrook S, Mori R, Ochirbat T & Gomi H. (2014). Strategies of testing for syphilis during pregnancy. Cochrane Database Syst Rev , , CD010385. PMID: 25352226 DOI.
Berman SM. (2004). Maternal syphilis: pathophysiology and treatment. Bull. World Health Organ. , 82, 433-8. PMID: 15356936
Carey JC. (2003). Congenital syphilis in the 21st century. Curr Womens Health Rep , 3, 299-302. PMID: 12844452
Goldenberg RL, Hauth JC & Andrews WW. (2000). Intrauterine infection and preterm delivery. N. Engl. J. Med. , 342, 1500-7. PMID: 10816189 DOI.
Ross SM. (1982). Sexually transmitted diseases in pregnancy. Clin Obstet Gynaecol , 9, 565-92. PMID: 6293753
Articles
Nelson R. (2018). Congenital syphilis and other STIs rise in the USA. Lancet Infect Dis , 18, 1186-1187. PMID: 30507406 DOI.
Patel NU, Oussedik E, Landis ET & Strowd LC. (2018). Early Congenital Syphilis: Recognising Symptoms of an Increasingly Prevalent Disease. J Cutan Med Surg , 22, 97-99. PMID: 28821219 DOI.
Colombo DF, Lew JL, Pedersen CA, Johnson JR & Fan-Havard P. (2006). Optimal timing of ampicillin administration to pregnant women for establishing bactericidal levels in the prophylaxis of Group B Streptococcus. Am. J. Obstet. Gynecol. , 194, 466-70. PMID: 16458647 DOI.
Nowicki S, Selvarangan R & Anderson G. (1999). Experimental transmission of Neisseria gonorrhoeae from pregnant rat to fetus. Infect. Immun. , 67, 4974-6. PMID: 10456962
Search Pubmed
Search NCBI Bookshelf: Medical Microbiology - Syphilis Search
Search PubMed: Congenital Syphilis | Abnormal Embryology Syphilis | Abnormal Development Syphilis
External Links
External Links Notice - The dynamic nature of the internet may mean that some of these listed links may no longer function. If the link no longer works search the web with the link text or name. Links to any external commercial sites are provided for information purposes only and should never be considered an endorsement. UNSW Embryology is provided as an educational resource with no clinical information or commercial affiliation.
- CDC (USA)
- CDC Fact Sheet - STD and Pregnancy
- CDC Fact Sheet - Syphilis
- Congenital Syphilis Case Investigation and Reporting Form Instructions PDF
- Public Health Training Network Epidemiology and Prevention of Vaccine-Preventable Diseases (viewable Webcasts requires Media Player) | Advisory Committee on Immunization Practices (ACIP) Recommendations
- Medline Plus
- Office on Women's Health (USA) Fact Sheet - Syphilis
- Royal College of Obstetricians and Gynaecologists (UK) Infection and Pregnancy - study group recommendations (Jun 2001)
Glossary Links
- Glossary: A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | Numbers | Symbols | Term Link
Cite this page: Hill, M.A. (2024, April 28) Embryology Abnormal Development - Syphilis. Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/Abnormal_Development_-_Syphilis
- © Dr Mark Hill 2024, UNSW Embryology ISBN: 978 0 7334 2609 4 - UNSW CRICOS Provider Code No. 00098G