Musculoskeletal System - Limb Abnormalities
| Embryology - 10 Mar 2026 |
|---|
| Google Translate - select your language from the list shown below (this will open a new external page) |
|
العربية | català | 中文 | 中國傳統的 | français | Deutsche | עִברִית | हिंदी | bahasa Indonesia | italiano | 日本語 | 한국어 | မြန်မာ | Pilipino | Polskie | português | ਪੰਜਾਬੀ ਦੇ | Română | русский | Español | Swahili | Svensk | ไทย | Türkçe | اردو | ייִדיש | Tiếng Việt These external translations are automated and may not be accurate. (More? About Translations) |
| ICD-11 Limb Abnormalities |
|---|
|
Structural LB74.1 Developmental dysplasia of hip - LB74.2 Congenital subluxation of hip | LB74.3 Unstable hip | LB74.4 Congenital coxa vara | LB74.5 Congenital coxa valga | LB74.6 Wide symphysis pubis LB75 Brachydactyly - LB75.0 Brachydactyly of fingers | LB75.1 Brachydactyly of toes | LB75.2 Symbrachydactyly of hands or feet | LB76 Triphalangeal thumb | LB77 Hyperphalangy | LB78 Polydactyly - LB78.0 Polydactyly of the thumb | LB78.1 Polysyndactyly | LB78.2 Postaxial polydactyly of fingers | LB78.3 Polydactyly of toes | LB79 Syndactyly - LB79.0 Fused fingers | LB79.1 Webbed fingers | LB79.2 Fused toes | LB79.3 Webbed toes | Congenital deformities of fingers or toes | LB80 Congenital deformities of fingers - LB80.0 Clinodactyly of fingers | LB80.1 Congenital club finger | LB80.2 Radial deviation of fingers | LB81 Congenital deformities of toes - LB81.0 Clinodactyly of toes | LB90 Joint formation defects | LB91 Congenital shoulder dislocation | LB92 Congenital elbow dislocation | LB93 Congenital knee dislocation | LB94 Congenital patella dislocation | LB95 Patella aplasia or hypoplasia | LB96 Congenital bowing of long bones | LB97 Limb overgrowth | LB98 Congenital deformities of feet | LB99 Reduction defects of upper limb | LB9A Reduction defects of lower limb | LB9B Reduction defects of upper or lower limbs |
| limb abnormalities |
Introduction
Musculoskeletal and limb abnormalities are one of the largest groups of congenital abnormalities. The upper and lower limbs have a large number of different genetic and environment derived abnormalities, some of which can be surgically repaired, while others may indicate other syndromes or karyotype anomalies (trisomy etc) by association. Congenital limb agenesis and deficiencies prevalence is about 7.9/10,000 live births.
A key historic area of limb abnormalities were those associated with limb reduction (and other defects) with the "morning sickness" prescription drug Thalidomide and its significant teratogenic effects (More? Thalidomide).
A 1994 review of data from Hungary (1975-1984)[1] showed in this population an overall 1 in 1,816 prevalence of limb deficiency at birth.
| System Abnormalities | ||||
|---|---|---|---|---|
|
Some Recent Findings
|
| More recent papers |
|---|
|
This table allows an automated computer search of the external PubMed database using the listed "Search term" text link.
More? References | Discussion Page | Journal Searches | 2019 References | 2020 References Search term: Abnormal Limb Development | limb reduction defect |
| Older papers |
|---|
| These papers originally appeared in the Some Recent Findings table, but as that list grew in length have now been shuffled down to this collapsible table.
See also the Discussion Page for other references listed by year and References on this current page.
|
Textbooks
- The Developing Human: Clinically Oriented Embryology (8th Edition) by Keith L. Moore and T.V.N Persaud - Moore & Persaud Chapter 15 the skeletal system
- Larsen’s Human Embryology by GC. Schoenwolf, SB. Bleyl, PR. Brauer and PH. Francis-West - Chapter 11 Limb Dev (bone not well covered in this textbook)
- Before we Are Born (5th ed.) Moore and Persaud Chapter 16,17: p379-397, 399-405
- Essentials of Human Embryology Larson Chapter 11 p207-228
Developmental Dysplasia of the Hip
For more details see Developmental Hip Dysplasia.
| ICD-11 LB74 Structural developmental anomalies of pelvic girdle |
|---|
|
Structural LB74.1 Developmental dysplasia of hip - A condition caused by failure of the hip to correctly develop during the antenatal period. This condition is characterized by slippage of the hip from the socket. This condition may present with outward turning of the leg, reduced movement on one side of the body, shortness of one leg, uneven skin folds on thigh or buttocks, walking difficulties, or inward rounding of the lower back. LB74.2 Congenital subluxation of hip | LB74.3 Unstable hip | LB74.4 Congenital coxa vara | LB74.5 Congenital coxa valga | LB74.6 Wide symphysis pubis LB74.Y Other specified structural developmental anomalies of pelvic girdle | LB74.Z Structural developmental anomalies of pelvic girdle, unspecified |
| limb abnormalities |

|

|
| X-Ray Hip Dysplasia | X-Ray Hip Dysplasia and renal agenesis[11] |
Also called Congenital Hip Dislocation.
- Instability: 1:60 at birth; 1:240 at 1 wk: Dislocation untreated; 1:700
- congenital instability of hip, later dislocates by muscle pulls or gravity
- familial predisposition female predominance
- Growth of femoral head, acetabulum and innominate bone are delayed until the femoral head fits firmly into the acetabulum
Barlow test
(Barlow maneuver) A clinical term to describe a physical examination of the newborn for developmental dysplasia of the hip (DDH). The examiner adducts the hip (bringing the thigh towards the midline) while applying light pressure on the knee, directing the force posteriorly. A positive sign is the hip being dislocatable, if the hip can be popped out of socket with this test. This test is then combined with the Ortolani test (maneuver).
The test is named after Thomas Barlow (1845 – 1945) a British royal physician.
Ortolani test
(Ortolani maneuver) A clinical term to describe a physical examination of the newborn for developmental dysplasia of the hip (DDH). This is a test for posterior dislocation of the hip. Using the examiner's thumb, abduct the infant's leg, while using the examiner's index finger to place anterior pressure on the greater trochanter. A positive sign is a distinctive 'clunk' which can be heard and felt as the femoral head relocates anteriorly into the acetabulum, usually becomes negative after 2 months of age. This test is combined with the Barlow test (maneuver).
The test is named after Marino Ortolani, the test developer in 1976.
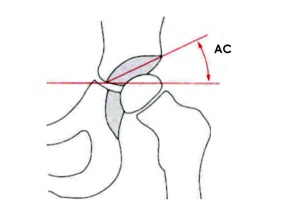
Acetabular index
This clinical measurement is based upon radiograph analysis of the acetabular inclination before ossification of the triradiate cartilage. The index is defined as the angle between Hilgenreiner's line and a line from the inferior margin of the iliac bone through the acetabular bony rim.
Triradiate cartilage is the Y-shaped growth plate region within the hip that does not complete ossification postnatally in humans until 14 - 16 years of age.
X-ray landmarks
- Hilgenreiner's line - a horizontal line drawn between the two triradiate cartilage centers of the hips, defines a horizontal plane and an approximation to flexion axis of the hips.
- Perkin's line - a perpendicular line to the horizontal line drawn at the edge of the boney part of the acetabular socket.
- Shenton's line - an oval that traces the lower pubis contour, that should smoothly continue on to trace the lower edge of the neck of the femur.
Abduction Splints
There is variable evidence for the use of abduction splinting during onset of walking in children on the maturation of mild dysplastic hips.[12]
- Links: Developmental Hip Dysplasia Screening for developmental dysplasia of the hip: recommendation statement.[13]
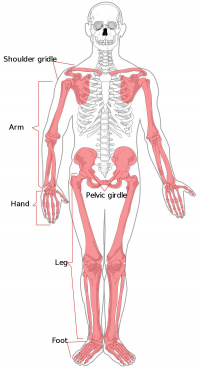
Developing Limb Regions
The developing limb can be described along the proximodistal axis as having three main regions , with abnormalities along this axis characterised by the changes to these specific skeletal components.
Stylopod
Limb development term describing the proximal region the limb, the skeletal component of the upper limb (forelimb) is the humerus, and for the lower limb (hindlimb) is the femur.
Zeugopod
Limb development term describing the mid-section of the limb , the skeletal components of the upper limb (forelimb) are the radius and ulna, and for the lower limb (hindlimb) are the tibia and fibula.
Autopod
Limb development term describing the distal region the limb, the musculoskeletal component of the upper limb (forelimb) is the hand, and for the lower limb (hindlimb) is the foot.
Limb Abnormality Classification
There have been a number of different classifications applied to limb abnormalities (Classic Classification, Frantz Classification, International Society for Prosthetics and Orthotics (ISPO) Classification System).
The current preferred classification system is the ISPO Classification,[14] which divides all limb deformities into either transverse (no distal remaining portions) or longitudinal (has distal portions).
The original classical classification of limb deficiencies was:
- Amelia - complete absence of a limb.
- Meromelia - the partial absence of a limb.
- Hemimelia - the absence of half a limb.
- Phocomelia - a flipper-like appendage attached to the trunk. (limbs with a stylopod, a truncated or absent zeugopod, and a nearly intact autopod)
- Acheiria a missing hand or foot.
- Adactyly - the absence of metacarpal or metatarsal.
- Aphalangia - an absent digit, finger or toe.
Hand Abnormality Classification
There is now a international classification for congenital hand anomalies based on an extension of an earlier classification system.[15] Some of these abnormalities can be initially detected prenatally by ultrasound and may be associated with other syndromes or karyotype anomalies.
Groups
- I. Failure of formation; transverse (A), or longitudinal (B) (radial and ulnar deficiencies, symbrachydactyly)
- II. Failure of differentiation
- III. Polydactyly (513 anomalies, Madelung deformity, the Kirner deformity and congenital trigger fingers and trigger thumbs, Triphalangeal thumbs)
- IV. Overgrowth
- V. Undergrowth
- VI. Amniotic band syndrome (amniotic bands)
- VII. Generalized skeletal syndromes.
- Failure of finger ray induction (cleft hand (IC), central polydactyly (III) and (bony) syndactyly (II)
- Unclassifiable
Alignment abnormalities (clenched hand, camptodactyly, clinodactyly, hypokinesia, clubhand, phocomelia), thumb anomalies, abnormal size (macrodactyly, trident hand), abnormal echogenicity (abnormal calcifications), abnormal number (polydactyly, syndactyly, ectrodactyly), and constriction band sequence.
Syndactyly
| ICD-11 LB79 Syndactyly - LB79.0 Fused fingers | LB79.1 Webbed fingers | LB79.2 Fused toes | LB79.3 Webbed toes |
Fusion of fingers or toes (Greek, syn = together, dactyly = digit) which may be single or multiple and may affect: skin only, skin and soft tissues or skin, soft tissues and bone. The condition is unimportant in toes but disabling in fingers and requires operative separation and is frequently inherited as an autosomal dominant. The presence of this additional "webbing" reflects preservation of the developmental tissues that in normal development are removed by programmed cell death (apotosis).
Syndactyly occuring in cattle is known as "mulefoot" an autosomal recessive trait and has been associated with mutations in the low density lipoprotein receptor-related protein 4 gene (LRP4). When shortening of the syndactyal digits also occurs it is then described as brachysyndactyly (Greek, brachys = short, syn = together, dactyly = digit). (More? Brachydactyly).
See also an article on molecular control of skeletal size with digit separation.[16]
Links: OMIM - Syndactyly I | Syndactyly II | Syndactyly III | Syndactyly IV | Syndactyly V
Search PubMed Now: Syndactyly | Syndactylia |
Polydactyly
| ICD-11 Limb AbnormalitiesLB78 Polydactyly - LB78.0 Polydactyly of the thumb | LB78.1 Polysyndactyly | LB78.2 Postaxial polydactyly of fingers | LB78.3 Polydactyly of toes |
Presence of additional toes or fingers (Greek, poly = many, dactyly = digit) also called polydactylia or polydactylism. The condition is often treated surgically in the infant. Polydactyly can also be associated with a number of different syndromes including Greig cephalopolysyndactyly syndrome (GCPS).
There are also several forms of polydactyly including: preaxial polydactyly type-IV (PPD-IV) and postaxial polydactyly.
Preaxial polydactyly (PPD) has been shown as a defect in Sonic Hedgehog (Shh) expression. SHH is normally expressed specifically in the zone of polarizing activity (ZPA) located posteriorly in the limb bud and is expressed in an additional ectopic site (at the anterior margin) in a mouse model of this disorder.
This expression appears to be due to point mutations in the limb-specific regulatory element of the SHH gene.
The author Ernest Hemmingway in the 1930's had a six-toed cat (Snowball) showing a form of polydactyly and cats with a similar condition today (image) are now called "Hemmingway cats".
Search PubMed Now: Polydactyly | Polydactylia |
Polysyndactyly
Developmental abnormality where there is a combination of additional digits (polydactyly) that are fused together (syndactyly) and is known as polysyndactyly. See also article on treatment of congenital upper extremity problems.[17]
Search PubMed Now: Polysyndactyly
Brachydactyly
| ICD-11 LB75 Brachydactyly - LB75.0 Brachydactyly of fingers | LB75.1 Brachydactyly of toes | LB75.2 Symbrachydactyly of hands or feet |
Middle phalanges of both hands and feet are very short (Greek, brachys = short, dactyly = digit) in length or absent. Condition can also be associated with endocrine abnormality, pseudohypoparathyroidism (end-organ unresponsiveness to parathyroid hormone) leading to short stature, round facies, brachydactyly, and short fourth or fifth metacarpals.
A chromosomal translocation (t(4;6)(q12;p23) has also been shown to disrupt a membrane-associated O-acetyl transferase gene (MBOAT1) in a patient with a novel brachydactyly-syndactyly syndrome.[9] "One of the genes on chromosome 6, the membrane-associated O-acetyl transferase gene 1 (MBOAT1), was disrupted by the breakpoint. ...Identification of the transferred acyl group and the target may reveal the signaling pathways altered in this novel brachydactyly-syndactyly syndrome."
Search PubMed Now: Brachydactyly
Symbrachydactyly
Symbrachydactyly describes a combination of syndactyly accompanied by brachydactyly. See clinical article on surgical reconstruction in symbrachydactyly using the reverse radial forearm flap.[18]
Search PubMed Now: Symbrachydactyly
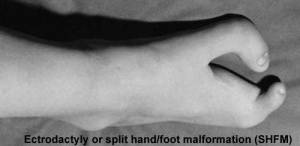
Ectrodactyly
Ectrodactyly or split hand/foot malformation (SHFM) or cleft hand, central ray deficiency (previously called "lobster-claw malformation"). Abnormality is a deep median cleft of either the hand and/or foot due to the embryonic absence of the central rays.
Highly variable malformation (genetic heterogeneous, 5+ loci mapped) occuring in isolation or in association with other systematic anomalies including congenital heart defects.
During limb development at the time of had or foot formation, the median apical ectodermal ridge (AER) fails to be maintained leading to an absence of its developmental regional signaling. Can have isolated vascular supply related cases and occur as part of a syndrome.
|

|
Search PubMed Now: Ectrodactyly | Split hand/foot malformation |
Triphalangeal Thumb
| The developmental abnormality triphalangeal thumb (TPT) has three phalanges instead of two, forming a long, finger-like thumb.
The isolated triphalangeal thumb anomaly has also been mapped to chromosome region 7q36 and has been identified as caused by point mutations in the ZPA regulatory sequence (ZRS) which is a long-range cis-regulator for the SHH gene.[8][19] See also the recent reviews.[4]PubmedParser error: The PubmedParser extension received invalid XML data. ()
Links: OMIM - Sall4 | OMIM - Tbx5 | Indian Pediatrics - Indian Pediatrics 2005;42:1246-1247 |

|
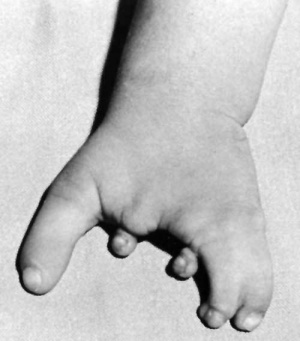
Talipes Equinovarus

(Latin, talipes = ankle bone, pes = foot, equinus = horse) Abnormality of the lower limb which begins in the embryonic period (first trimester of pregnancy) resulting in the foot is then turned inward and downward at birth, described as "club foot". Occurs in approximately 1 in 1,000 births, postnatally it affects how children walk on their toes with the foot pointed downward like a horse.
Can also occur in asociation with other syndromes. For example, camptomelic dysplasia, an extremely rare (2 per million live births) lethal congenital bony dysplasia which can be detected by ultrasound (25 weeks) visible as anterior bowing of long bones.
Search PubMed Now: talipes equinovarus
Links: Medline Plus - Clubfoot | The Clubfoot Club |
Amniotic band syndrome (amniotic bands)
Amniotic constriction bands are relatively rare and is caused by damage to the amnion, producing fiber-like bands that trap periperal structures (arms, legs, fingers, or toes) reducing local blood supply leading to abnormal development.
Abnormalities range from a permanent band or indentation around the structure (arm, leg, finger, or toe), digital webbing, too all or part of the limb missing.
Search PubMed Now: Amniotic band syndrome | amniotic bands |
Sirenomelia

Sirenomelia (mermaid syndrome) is named after the mythical Greek sirens. A rare developmental abnormality (incidence of 0.8-1 case /100000 births), male to female ratio 3:1. While demonstrating limb developmental abnormalities, including a single fused lower limb, there are also associated multiple urogenital, anorectal and vascular malformations. The condition has also been associated with maternal diabetes.
Classified into type I to type VII according mainly to the presence of skeletal elements in the thigh and leg.[22] Two existing mouse models;[23] 1. lacking Cyp26a1, an enzyme that degrades retinoic acid (RA), 2. reduced bone morphogenetic protein (Bmp) signaling in the caudal embryonic region.
A recent mouse model has used a bmp7;shh mutant model to look at signaling processes involved with this developmental abnormality.[7]
- Links: Image - Sirenomelia infant | Image - Sirenomelia x-ray | Developmental Signals - Retinoic acid | Limb Abnormalities | Maternal Diabetes
Limb Reduction
Genetic
There are many different genetic abnormalities and syndromes that have an associated limb reduction.
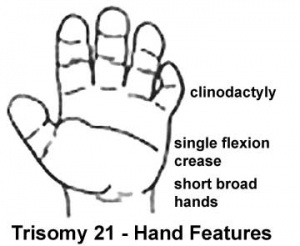
Trisomy 21 - (Down Syndrome) features short and broad hands, clinodactyly (curving of the fifth finger, little finger) with a single flexion crease (20%), hyperextensible finger joints, space between the great toe (big) and the second toe is increased, and acquired hip dislocation (6%).
Diastrophic dysplasia - an autosomal recessive disorder, due to mutations in the DTD sulphate transporter gene (chromosome 5q32–q33). Leads to severe short-limbed dwarfism, progressive spinal and joint problems and can be detected by ultrasound (16 and 19 weeks of gestation).
Environment
Thalidomide was the most well known example limb reducing insult (teratogen) in humans, which also produced a range of other deformities depending on developmental time and concentration of the drug exposure.
- Thalidomide effects
Many additional substances (teratogens) have been found capable of producing limb reduction defects in experimental animals but few have been related to humans.
Limb reduction defects may also be either direct or indirect, for example with loss of blood supply to part of the limb or abnormal innervation at the spinal or cerebral level. There are a number of as yet undefined mechanisms involved.
Limb reduction defects may be apical (congenital amputation) or pre- or post-axial (absence of radius and lateral digits; ulnar and medial digits).
Links: Abnormal Development - Thalidomide
Search PubMed Now: Congenital Limb Reduction
Nail Abnormalities
Covered in developmental notes on Integumentary Development Abnormalities, Nail Development.
Congenital hyponychia
Anonychia
Nail-patella syndrome
Ectodermal dysplasias
Brachydactylies
Search PubMed Now: Congenital hyponychia | Anonychia
References
- ↑ Evans JA, Vitez M & Czeizel A. (1994). Congenital abnormalities associated with limb deficiency defects: a population study based on cases from the Hungarian Congenital Malformation Registry (1975-1984). Am. J. Med. Genet. , 49, 52-66. PMID: 8172251 DOI.
- ↑ Al-Qattan MM. (2019). A Review of the Genetics and Pathogenesis of Syndactyly in Humans and Experimental Animals: A 3-Step Pathway of Pathogenesis. Biomed Res Int , 2019, 9652649. PMID: 31637260 DOI.
- ↑ Klungsøyr K, Nordtveit TI, Kaastad TS, Solberg S, Sletten IN & Vik AK. (2019). Epidemiology of limb reduction defects as registered in the Medical Birth Registry of Norway, 1970-2016: Population based study. PLoS ONE , 14, e0219930. PMID: 31314783 DOI.
- ↑ 4.0 4.1 Potuijt JWP, Galjaard RH, van der Spek PJ, van Nieuwenhoven CA, Ahituv N, Oberg KC & Hovius SER. (2018). A multidisciplinary review of triphalangeal thumb. J Hand Surg Eur Vol , , 1753193418803521. PMID: 30318985 DOI.
- ↑ Alexander PG, Clark KL & Tuan RS. (2016). Prenatal exposure to environmental factors and congenital limb defects. Birth Defects Res. C Embryo Today , 108, 243-273. PMID: 27768243 DOI.
- ↑ Elmakky A, Stanghellini I, Landi A & Percesepe A. (2015). Role of Genetic Factors in the Pathogenesis of Radial Deficiencies in Humans. Curr. Genomics , 16, 264-78. PMID: 26962299 DOI.
- ↑ 7.0 7.1 Garrido-Allepuz C, González-Lamuño D & Ros MA. (2012). Sirenomelia phenotype in bmp7;shh compound mutants: a novel experimental model for studies of caudal body malformations. PLoS ONE , 7, e44962. PMID: 23028704 DOI.
- ↑ 8.0 8.1 Sun M, Ma F, Zeng X, Liu Q, Zhao XL, Wu FX, Wu GP, Zhang ZF, Gu B, Zhao YF, Tian SH, Lin B, Kong XY, Zhang XL, Yang W, Lo WH & Zhang X. (2008). Triphalangeal thumb-polysyndactyly syndrome and syndactyly type IV are caused by genomic duplications involving the long range, limb-specific SHH enhancer. J. Med. Genet. , 45, 589-95. PMID: 18417549 DOI.
- ↑ 9.0 9.1 Dauwerse JG, de Vries BB, Wouters CH, Bakker E, Rappold G, Mortier GR, Breuning MH & Peters DJ. (2007). A t(4;6)(q12;p23) translocation disrupts a membrane-associated O-acetyl transferase gene (MBOAT1) in a patient with a novel brachydactyly-syndactyly syndrome. Eur. J. Hum. Genet. , 15, 743-51. PMID: 17440500 DOI.
- ↑ Nissim S, Allard P, Bandyopadhyay A, Harfe BD & Tabin CJ. (2007). Characterization of a novel ectodermal signaling center regulating Tbx2 and Shh in the vertebrate limb. Dev. Biol. , 304, 9-21. PMID: 17300775 DOI.
- ↑ Acién P, Galán F, Manchón I, Ruiz E, Acién M & Alcaraz LA. (2010). Hereditary renal adysplasia, pulmonary hypoplasia and Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome: a case report. Orphanet J Rare Dis , 5, 6. PMID: 20388228 DOI.
- ↑ 12.0 12.1 Windhagen H, Thorey F, Kronewid H, Pressel T, Herold D & Stukenborg-Colsman C. (2005). The effect of functional splinting on mild dysplastic hips after walking onset. BMC Pediatr , 5, 17. PMID: 15958160 DOI.
- ↑ US Preventive Services Task Force. (2006). Screening for developmental dysplasia of the hip: recommendation statement. Pediatrics , 117, 898-902. PMID: 16510673 DOI.
- ↑ Day HJ. (1991). The ISO/ISPO classification of congenital limb deficiency. Prosthet Orthot Int , 15, 67-9. PMID: 1923724 DOI.
- ↑ De Smet L. (2002). Classification for congenital anomalies of the hand: the IFSSH classification and the JSSH modification. Genet. Couns. , 13, 331-8. PMID: 12416642
- ↑ Ota S, Zhou ZQ, Keene DR, Knoepfler P & Hurlin PJ. (2007). Activities of N-Myc in the developing limb link control of skeletal size with digit separation. Development , 134, 1583-92. PMID: 17360777 DOI.
- ↑ Netscher DT & Baumholtz MA. (2007). Treatment of congenital upper extremity problems. Plast. Reconstr. Surg. , 119, 101e-129e. PMID: 17415231 DOI.
- ↑ Gülgönen A & Güdemez E. (2007). Reconstruction of the first web space in symbrachydactyly using the reverse radial forearm flap. J Hand Surg Am , 32, 162-7. PMID: 17275589 DOI.
- ↑ Potuijt JWP, Baas M, Sukenik-Halevy R, Douben H, Nguyen P, Venter DJ, Gallagher R, Swagemakers SM, Hovius SER, van Nieuwenhoven CA, Galjaard RH, van der Spek PJ, Ahituv N & de Klein A. (2018). A point mutation in the pre-ZRS disrupts sonic hedgehog expression in the limb bud and results in triphalangeal thumb-polysyndactyly syndrome. Genet. Med. , , . PMID: 29543231 DOI.
- ↑ ten Broek CM, Bots J, Varela-Lasheras I, Bugiani M, Galis F & Van Dongen S. (2013). Amniotic fluid deficiency and congenital abnormalities both influence fluctuating asymmetry in developing limbs of human deceased fetuses. PLoS ONE , 8, e81824. PMID: 24312362 DOI.
- ↑ Kshirsagar VY, Ahmed M & Colaco SM. (2012). Sirenomelia apus: a rare deformity. J Clin Neonatol , 1, 146-8. PMID: 24027712 DOI.
- ↑ Stocker JT & Heifetz SA. (1987). Sirenomelia. A morphological study of 33 cases and review of the literature. Perspect Pediatr Pathol , 10, 7-50. PMID: 3588246
- ↑ Garrido-Allepuz C, Haro E, González-Lamuño D, Martínez-Frías ML, Bertocchini F & Ros MA. (2011). A clinical and experimental overview of sirenomelia: insight into the mechanisms of congenital limb malformations. Dis Model Mech , 4, 289-99. PMID: 21504909 DOI.
Reviews
Rogers BH, Schmieg SL, Pehnke ME & Shah AS. (2020). Evaluation and Management of Preaxial Polydactyly. Curr Rev Musculoskelet Med , , . PMID: 32472371 DOI.
Al-Qattan MM. (2019). A Review of the Genetics and Pathogenesis of Syndactyly in Humans and Experimental Animals: A 3-Step Pathway of Pathogenesis. Biomed Res Int , 2019, 9652649. PMID: 31637260 DOI.
Tonkin MA. (2012). Thumb duplication: concepts and techniques. Clin Orthop Surg , 4, 1-17. PMID: 22379552 DOI.
Hill RE. (2007). How to make a zone of polarizing activity: insights into limb development via the abnormality preaxial polydactyly. Dev. Growth Differ. , 49, 439-48. PMID: 17661738 DOI.
Articles
Dauwerse JG, de Vries BB, Wouters CH, Bakker E, Rappold G, Mortier GR, Breuning MH & Peters DJ. (2007). A t(4;6)(q12;p23) translocation disrupts a membrane-associated O-acetyl transferase gene (MBOAT1) in a patient with a novel brachydactyly-syndactyly syndrome. Eur. J. Hum. Genet. , 15, 743-51. PMID: 17440500 DOI.
Gülgönen A & Güdemez E. (2007). Reconstruction of the first web space in symbrachydactyly using the reverse radial forearm flap. J Hand Surg Am , 32, 162-7. PMID: 17275589 DOI.
Nissim S, Allard P, Bandyopadhyay A, Harfe BD & Tabin CJ. (2007). Characterization of a novel ectodermal signaling center regulating Tbx2 and Shh in the vertebrate limb. Dev. Biol. , 304, 9-21. PMID: 17300775 DOI.
Guven MA, Batukan C, Ceylaner S, Ceylaner G & Uzel M. (2006). A case of fetal anticonvulsant syndrome with severe bilateral upper limb defect. J. Matern. Fetal. Neonatal. Med. , 19, 115-7. PMID: 16676441
Day HJ. (1991). The ISO/ISPO classification of congenital limb deficiency. Prosthet Orthot Int , 15, 67-9. PMID: 1923724 DOI.
McKee PR & Bagnall KM. (1987). Skeletal relationships in the human embryonic foot based on three-dimensional reconstructions. Acta Anat (Basel) , 129, 34-42. PMID: 3618097
Evans JA, Vitez M & Czeizel A. (1994). Congenital abnormalities associated with limb deficiency defects: a population study based on cases from the Hungarian Congenital Malformation Registry (1975-1984). Am. J. Med. Genet. , 49, 52-66. PMID: 8172251 DOI.
Search PubMed
Search Pubmed: limb developmental abnormalities
Additional Images
- Fetal limb abnormalities X-ray-01.jpg
bowing of the radius and ulna, bowing of the digits, bowing and hypoplasia of the femur, tibia and fibula.
Terms
- preaxial - referring to the lateral (radial) aspect of the upper limb, and the medial (tibial) aspect of the lower limb.
- postaxial - referring to the medial ( ulnar) aspect of the upper limb, and the lateral (fibular) aspect of the lower limb.
Glossary Links
- Glossary: A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | Numbers | Symbols | Term Link
Cite this page: Hill, M.A. (2026, March 10) Embryology Musculoskeletal System - Limb Abnormalities. Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/Musculoskeletal_System_-_Limb_Abnormalities
- © Dr Mark Hill 2026, UNSW Embryology ISBN: 978 0 7334 2609 4 - UNSW CRICOS Provider Code No. 00098G