Abnormal Development - Iodine Deficiency
| Embryology - 27 Apr 2024 |
|---|
| Google Translate - select your language from the list shown below (this will open a new external page) |
|
العربية | català | 中文 | 中國傳統的 | français | Deutsche | עִברִית | हिंदी | bahasa Indonesia | italiano | 日本語 | 한국어 | မြန်မာ | Pilipino | Polskie | português | ਪੰਜਾਬੀ ਦੇ | Română | русский | Español | Swahili | Svensk | ไทย | Türkçe | اردو | ייִדיש | Tiếng Việt These external translations are automated and may not be accurate. (More? About Translations) |
| Educational Use Only - Embryology is an educational resource for learning concepts in embryological development, no clinical information is provided and content should not be used for any other purpose. |
| ICD-11 |
|---|
|
5B5K.3 Iodine deficiency - Iodine deficiency disorders (IDD), caused mainly by a low dietary supply of iodine, refer to all of the consequences of iodine deficiency in a population that can be prevented by ensuring that the population has an adequate intake of iodine. Iodine deficiency is the most frequent cause of preventable brain damage in childhood. 5A00.04 Congenital hypothyroidism due to iodine deficiency - Hypothyroidism is a condition which arises at birth where the thyroid gland produces too little or no thyroid hormone and it can be induced by iodine-deficiency. |
Introduction
Iodine deficiency disorders (IDD) is the single most common cause of preventable mental retardation and brain damage in the world. Iodine (Greek, ioeides = violet) is required for the synthesis of thyroid hormone, a key regulator of neurological development. IDD causes goiters and decreases the production of hormones vital to growth and development.
- 1.6 billion people are at risk
- IDD affects 50 million children
- 100,000 cretins are born every year
Children with IDD can grow up stunted, apathetic, mentally retarded and incapable of normal movement, speech or hearing. IDD in pregnant women cause miscarriage, stillbirth and mentally retarded children. A teaspoon of iodine is all a person requires in a lifetime, but because iodine cannot be stored for long periods by the body, tiny amounts are needed regularly. In areas of endemic iodine deficiency, where soil and therefore crops and grazing animals do not provide sufficient dietary iodine to the populace, food fortification and supplementation have proven highly successful and sustainable interventions. Iodized salt programs and iodized oil supplements are the most common tools in the fight against IDD.
In Australia, salt (where identified) and most breads (except organic varieties) are fortified with iodine. Before mandatory iodine fortification was introduced large proportions of the Australian and New Zealand population had inadequate iodine intakes based upon national surveys measuring median urinary iodine concentration (MUIC) in schoolchildren, an indicator of overall population status, confirmed mild iodine deficiency in both countries. The concentration was 96 μg per litre in Australia, and 66 μg per litre in New Zealand, less than the 100–200 μg per litre considered optimal.
Australia 2018 - Iodine requirements increase during pregnancy and a supplement of 150 micrograms a day is recommended.[1]
- Iodine Links: thyroid | neural | neural abnormalities
| Nutrition Links: nutrition | Vitamin A | Vitamin B | Vitamin C | Vitamin D | Vitamin E | Vitamin K | folate | iodine deficiency | neural abnormalities | Axial Skeleton Abnormalities |
Some Recent Findings
|
| More recent papers |
|---|
|
This table allows an automated computer search of the external PubMed database using the listed "Search term" text link.
More? References | Discussion Page | Journal Searches | 2019 References | 2020 References Search term: Fetal Iodine Deficiency |
| Older papers |
|---|
Template:Lder papers
|
WHO Statistics
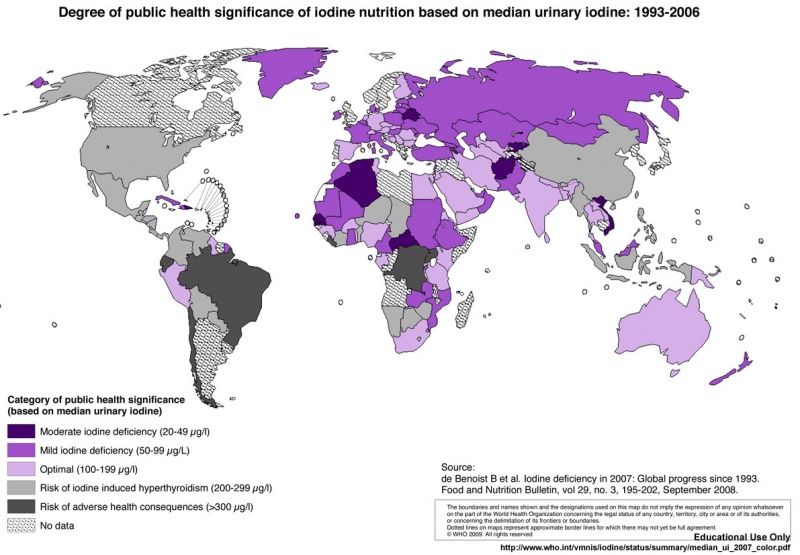
World map iodine status (2007)[9]
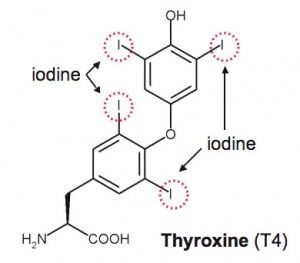
Iodine and Thyroid Hormone
Iodine incorporated into thyroid horomone, Thyroxine (T4)
Salt
Where salt iodization has been in place for over five years, improvement in iodine status has been overwhelming.Over the last decade, the number of countries with salt iodization programmes doubled, rising from 46 to 93. As a result, today 68% of the 5 billion people living in countries with IDD have access to iodized salt and the global rates of goitre, mental retardation and cretinism are falling fast.
(some text information from WHO page)
Iodine Requirements
The current WHO recommended daily iodine intakes are:
- 50 micrograms for infants (first 12 months of age)
- 90 micrograms for children (2-6 years of age)
- 120 micrograms for school children (7-12 years of age)
- 150 micrograms for adults (beyond 12 years of age)
- 200 micrograms for pregnant and lactating women
- Links: WHO - Micronutrient deficiencies Eliminating iodine deficiency disorders | WHO - Iodine data by country
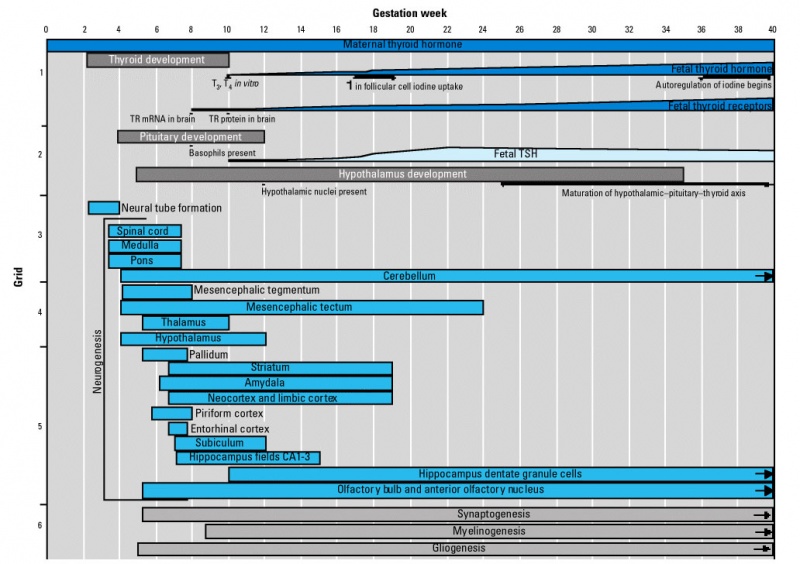
Thyroid System and Neural Development
- Links: Neural System Development
I - Iodine
This information is about Iodine the element, dietry intake is in the form of iodine as a salt. The solid halogen was discovered in 1811 by Bernard Courtois (1777-1838) in seaweed. Iodine (Greek, ioeides = violet) was named for the color of its vapour.
- Atomic number 53
- Density g/mL 4.92
- Atomic weight u 126.9045
- Melting point K 386.7
- Bonding radius A 1.33
- Boiling point K 458.4
- Atomic radius A 1.32
- Heat of vaporization kJ/mol 20.752
- Ionization Potential V 10.451
- Heat of fusion kJ/mol 7.824
- Electronegativity - 2.66
- Specific heat J/gK 0.214
- The oxide is a strong acid.
- Crystal are orthorhombic.
- Iodine has been used for its antibacterial qualities.
Congenital Hypothyroidism (CH)
This condition is not caused by iodine defficiency. Defined as thyroid hormone deficiency present at birth and occurs in approximately 1:2,000 to 1:4,000 newborns.[10] The condition is classified into permanent and transient forms that can be divided into primary, secondary, or peripheral etiologies.
- thyroid dysgenesis accounts for 85% of permanent primary
- inborn errors of thyroid hormone biosynthesis (dyshormonogeneses) account for 10-15% of cases
Australian Data
Mandatory iodine fortification of bread, through the replacement of salt with iodised salt in the making of bread, was implemented in October 2009 in Australia and in November 2009 in New Zealand.
Food Standards Australia New Zealand
Report June 2016: [http://www.foodstandards.gov.au/publications/Pages/Iodine-in-bread-report-.aspx
Monitoring the Australian population’s intake of dietary iodine before and after mandatory fortification]
IDD Prevalence and Control Program
IDD Prevalence and Control Program Data
(For other countries see also IDD Regional Data Page)
IDD Prevalence and Control Program Data
Last Modified: 6/98
Australia
I. IDD Prevalence
Goitre:
No national IDD data. Goiter historically limited to mountains of east and Tasmania. Before prophylaxis was introduced in 1950, IDD was greater than 50%. Presently, IDD not likely.
Cretinism:
Not present
TSH:
Neonatal TSH in screening shows levels compatible with iodine sufficiency, including Tasmania.
Urinary Iodine:
Current values: Tasmania 229-356 mcg/L, Sydney 180 mcg/L.
II. Salt Legislation
- Legislation:
- Legislation for Animals: No legislation, but widely used.
- Level Salt Iodization Required (ppm): 50
- Compound: KI
- Year Enacted: NA
- Latest Revision: NA
III. IDD Coordination
IDD Responsible Parties:
No national surveillance program
IV. Salt Supply
- Is Iodized Salt Available: Yes
- Percent Iodized Salt Available: No Data Available
- Percent of Salt Which is Imported:Australia is salt exporter
- Salt Imported from: NA
- Salt Production:
Iodized table salt has been available for over 50 years. However, noniodized salt is preferred and data indicate that less than a third of the consumed salt is iodized.
- Iodine (ppm): 50
- Compound: KI
- Method of Iodization: No Data Available
- Package Method: No Data Available
- Estimated daily per capita salt consumption: No Data Available
- Estimated % of all salt consumed by people which is adequately iodized (household level): No Data Available
- Cost of Iodized Salt (kg): No Data Available
- Cost of Uniodized Salt (kg): No Data Available
- Year: No Data Available
- Price differential between city and rural areas: No Data Available
- Estimated difference (urban/rural, %): No Data Available
- Time between production and consumption of iodized salt in remote areas (weeks): No Data Available
V. Supplementation:
- Total Number Supplemented:None
- % administered orally: NA
- % administered by injection: None
- Target Population: None.
- Other Supplementation Activities:
Iodized bread was introduced in 1963 in Canberra and in 1966 in Tasmania. It continues to be a source of iodine.
VI. Monitoring Activities
The following indicators are available to monitor IDD:
- Goitre:
- Urinary Iodine:
- Salt:
VII. Comments
Dietary diversification and use of iodine in farm animals has contributed to iodine sufficiency, and iodine deficiency does not appear a current problem. However, no national surveillance system exists. Recent informal reports raise questions of return of iodine deficiency to Tasmania and assessment is underway (1998).
VIII. Sources
IDD NL 9(1):11, 1993
- Links: Australia New Zealand Food Standards Code STANDARD 2.10.2 SALT AND SALT PRODUCTS
References
- ↑ Department of Health (2018) Clinical Practice Guidelines: Pregnancy Care. Canberra: Australian Government Department of Health. (5 June 2019)
- ↑ Levie D, Korevaar TIM, Bath SC, Murcia M, Dineva M, Llop S, Espada M, van Herwaarden AE, de Rijke YB, Ibarluzea JM, Sunyer J, Tiemeier H, Rayman MP, Guxens M & Peeters RP. (2019). Association of Maternal Iodine Status With Child IQ: A Meta-Analysis of Individual Participant Data. J. Clin. Endocrinol. Metab. , 104, 5957-5967. PMID: 30920622 DOI.
- ↑ Levie D, Derakhshan A, Shu H, Broeren MAC, de Poortere RA, Peeters RP, Bornehag CG, Demeneix B & Korevaar TIM. (2019). The Association of Maternal Iodine Status in Early Pregnancy with Thyroid Function in the Swedish Environmental Longitudinal, Mother and Child, Asthma and Allergy Study. Thyroid , , . PMID: 31524090 DOI.
- ↑ Nattero-Chávez L, Luque-Ramírez M & Escobar-Morreale HF. (2019). Systemic endocrinopathies (thyroid conditions and diabetes): impact on postnatal life of the offspring. Fertil. Steril. , 111, 1076-1091. PMID: 31155115 DOI.
- ↑ Taylor PN & Vaidya B. (2016). Iodine supplementation in pregnancy - is it time?. Clin. Endocrinol. (Oxf) , 85, 10-4. PMID: 26998765 DOI.
- ↑ NHMRC Iodine supplementation for Pregnant and Breastfeeding Women (2010) Online | PDF
- ↑ Azizi F, Hosseini MS, Amouzegar A, Tohidi M & Ainy E. (2011). Neonatal thyroid status in an area of iodine sufficiency. J. Endocrinol. Invest. , 34, 197-200. PMID: 20959719 DOI.
- ↑ Goodman JH & Gilbert ME. (2007). Modest thyroid hormone insufficiency during development induces a cellular malformation in the corpus callosum: a model of cortical dysplasia. Endocrinology , 148, 2593-7. PMID: 17317780 DOI.
- ↑ Bruno de Benoist, B Erin McLean, Maria Andersson, and Lisa Rogers Iodine deficiency in 2007: Global progress since 1993. Food and Nutrition Bulletin, vol. 29, no. 3 © 2008, The United Nations University. PDF
- ↑ Rastogi MV & LaFranchi SH. (2010). Congenital hypothyroidism. Orphanet J Rare Dis , 5, 17. PMID: 20537182 DOI.
Reviews
Zimmermann MB & Crill CM. (2010). Iodine in enteral and parenteral nutrition. Best Pract. Res. Clin. Endocrinol. Metab. , 24, 143-58. PMID: 20172478 DOI.
Hess SY. (2010). The impact of common micronutrient deficiencies on iodine and thyroid metabolism: the evidence from human studies. Best Pract. Res. Clin. Endocrinol. Metab. , 24, 117-32. PMID: 20172476 DOI.
Bürgi H. (2010). Iodine excess. Best Pract. Res. Clin. Endocrinol. Metab. , 24, 107-15. PMID: 20172475 DOI.
Articles
Andersson M, Aeberli I, Wüst N, Piacenza AM, Bucher T, Henschen I, Haldimann M & Zimmermann MB. (2010). The Swiss iodized salt program provides adequate iodine for school children and pregnant women, but weaning infants not receiving iodine-containing complementary foods as well as their mothers are iodine deficient. J. Clin. Endocrinol. Metab. , 95, 5217-24. PMID: 20810570 DOI.
Mackerras D, Powers J, Boorman J, Loxton D & Giles GG. (2011). Estimating the impact of mandatory fortification of bread with iodine on pregnant and post-partum women. J Epidemiol Community Health , 65, 1118-22. PMID: 20709857 DOI.
Search Pubmed
Search Pubmed: Iodine Deficiency | Iodine Deficiency Disorder
External Links
External Links Notice - The dynamic nature of the internet may mean that some of these listed links may no longer function. If the link no longer works search the web with the link text or name. Links to any external commercial sites are provided for information purposes only and should never be considered an endorsement. UNSW Embryology is provided as an educational resource with no clinical information or commercial affiliation.
- World Health Organization - Micronutrient deficiencies Eliminating iodine deficiency disorders
- World Health Organization - Iodine data by country
- Endocrinology: An Integrated Approach. Nussey, S.S. and Whitehead, S.A. Oxford, UK: BIOS Scientific Publishers, Ltd; 2001.Iodine intake
- Australian Journal of Nutrition and Dietetics
- Australian Nutrition Foundation
- CSIRO Human Nutrition
- Food, Nutrition & Health Information - Centre for Advanced Food Research
- Foodwatch
- Healthy Eating, Healthy Living
- AIS Sport Nutrition - information from the Australian Institute of Sport. Supplies nutrition research, a question-and-answer section, publications, and other resources.
- America's Eating Habits - a report from the U.S. Department of Agriculture's economic research service. Covers dietary recommendations, health claims in food advertising, reality about cholesterol, and various other topics.
- British Nutrition Foundation - an organization that works with academic, private, and public groups on nutrition. Includes nutrition education, facts, news, and publications.
- Center for Food Safety & Applied Nutrition - a repository of links relevant to all manner of food issues, including food safety. Emphasizes FDA regulations and related research programs.
- USA Office of Dietary Supplements Iodine
- Nutrition.gov - a collection of information and links to other sites on food safety, food programs, and federally funded research centers.
- Nutrition.org - site of the American Society for Nutritional Sciences. Features an encyclopedia that summarizes food sources, diet recommendations, and deficiencies for a number of macro- and micronutrients.
- Nutrition Navigator - a guide to nutrition websites reviewed and rated by Tufts University nutritionists. Supplies news and sections arranged by topic.
- U.S. Department of Agriculture
- Children's Nutrition Research Center
- Facts about the DASH Diet
- Healthfinder Kids
- Interactive Healthy Eating Index
- National Dairy Council
- Nutrition Explorations
Terms
- IDD - Iodine deficiency disorder
- WHO - World Health Organization
Glossary Links
- Glossary: A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | Numbers | Symbols | Term Link
Cite this page: Hill, M.A. (2024, April 27) Embryology Abnormal Development - Iodine Deficiency. Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/Abnormal_Development_-_Iodine_Deficiency
- © Dr Mark Hill 2024, UNSW Embryology ISBN: 978 0 7334 2609 4 - UNSW CRICOS Provider Code No. 00098G