Introduction
Lecture Objectives
Lecture Resources
| Movies | |||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
| |||||||||||||||
|
|
| 2016 Lecture Video Recording |
|---|
| This 2016 lecture video recording is similar in content to the current 2017 online lecture.
<html5media height="600" width="800">File:2016Lecture-Musculoskeletal.mp4</html5media> Click to play new window - 2016 Lecture Video (48 MB) |
Patterning and differentiation of the somitic mesoderm

|
|
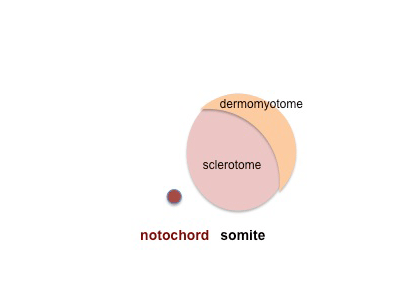
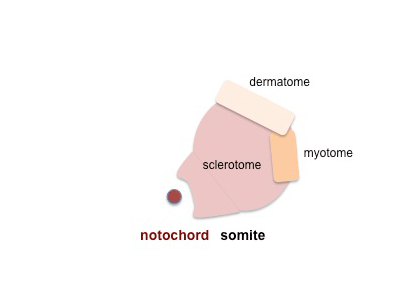
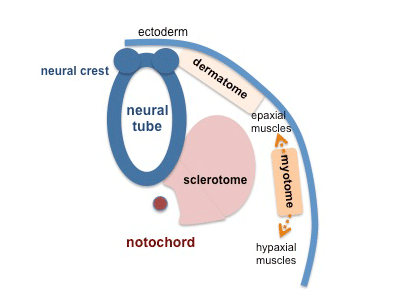
Somite Patterning
Each somite pair is initially patterned into the same verntro-dorsal components - sclerotome and dermomyotome
|
Dermomyotome is then divided into a dorsal dermatome and a ventral myotome
|
|
|
| |
Myotome is then divided into a dorsal epaxial and a ventral hypaxial muscle group
|
|
Neural Crest Derived Cells
(see Neural Crest and Head Lectures)
- Neural crest-derived cells are essential to form the bones and cartilage of the face and neck
- Also forms the cranial nerves and pigment cells, dorsal root ganglia and the sympathetic neurons.
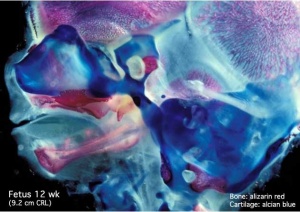
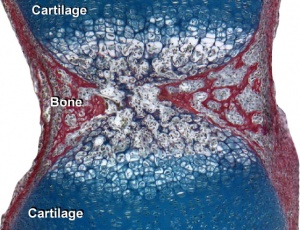
Cartilage Development
Most of the skeleton is formed initially by cartilage that is then replaced by bone
|
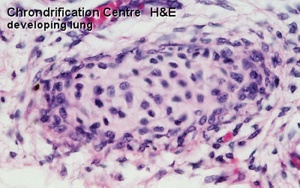
chondrification centre |
Cartilage 3 stages:
Cartilage replacement
|
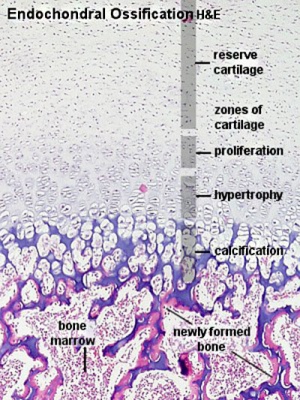
Endochondral ossification |
Cartilage Growth
- Interstitial growth - occurs mainly in immature cartilage. Chondroblasts in existing cartilage divide and form small groups of cells (isogenous groups) which produce matrix to become separated from each other by a thin partition of matrix.
- Appositional growth - occurs also in mature cartilage. Mesenchymal cells surrounding the cartilage in the deep part of the perichondrium (or the chondrogenic layer) differentiate into chondroblasts.
(review your Histology materials)
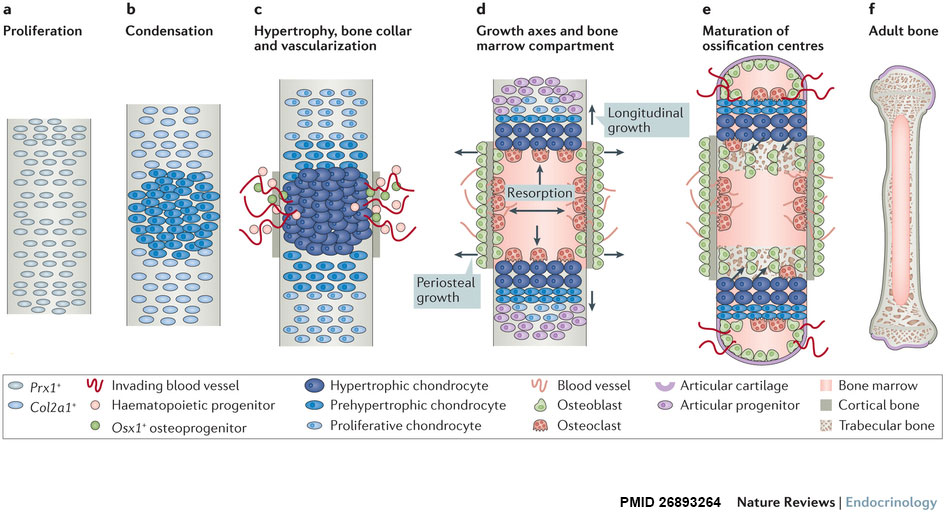
Hypertrophic Chondrocytes
- secrete VEGF, promoting vascular invasion
- hypertrophic calcified cartilage becomes resorbed, by recruited chondroclasts/osteoclasts via MMP9
Formation of Bone
|
|
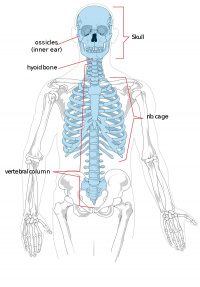
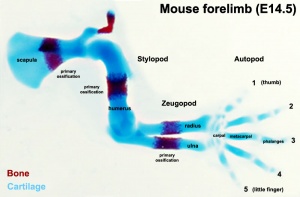
| Endochondral primary ossification centres | Intramembranous ossification centres |
- Two main forms of bone formation: Endochondral and Intramembranous.
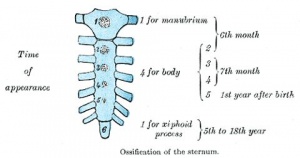
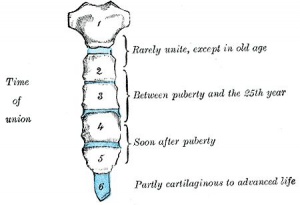
- Ossification process continues postnatally through puberty until mid 20s.
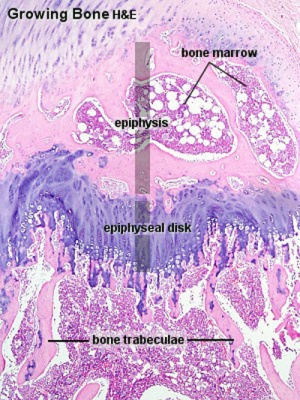
Endochondral initial primary and later secondary ossification centres (sites cartoon |

Periosteum is the source of osteoprogeitors for later bone growth |
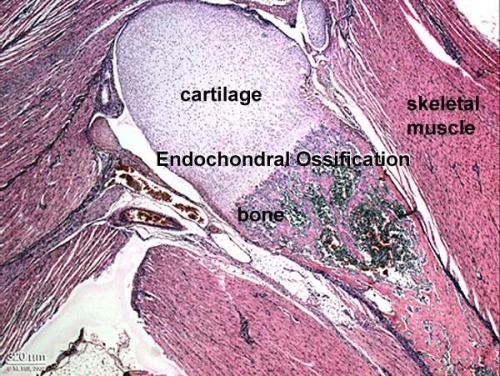
Endochondral Ossification
Endochondral Ossification[1]
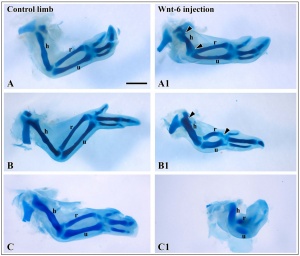
- Majority of skeleton formed by this process (vertebra, limb long bones)
- Osteoblasts derived from the bone collar replace cartilage matrix with a matrix rich in type I collagen leading to bone formation
- Ossification centres (primary and secondary)
- Early ossification occurs at ends of long bone
- Diagram of ossification in long bone University of Bristol - ossification
Endochondral bone development - Role of VEGF
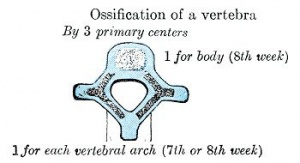
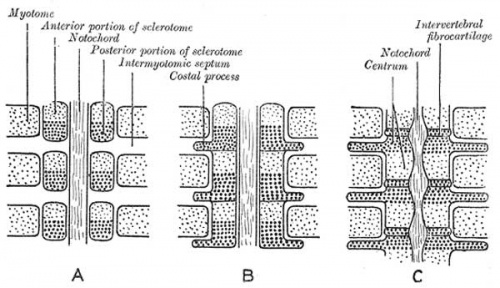
Development of Vertebrae
Week 4 - somite sclerotome surrounds notochord.
|
Initial formation of vertebral body |
|
|
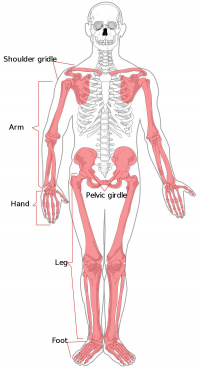
| Limb Bone Timeline |
|---|
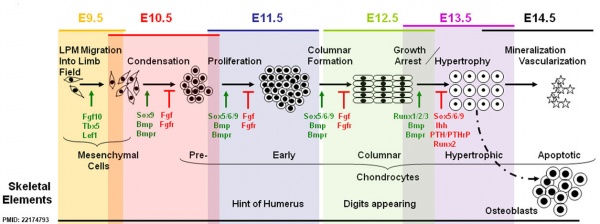
Mouse limb bone development timeline[2] (Note - this is shown as a general example of developmental bone changes you do not need to know the details) |
- Links: Bone Development Timeline | primary and secondary sites | Mice lacking Cbfa1 (Runx2) don't form bone
Vertebral segmentation
Adult vertebral column
|
|
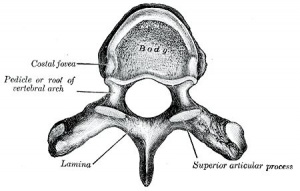
| Vertebra |
| Page | Play |
Axial Elements
| Intervertebral Disc | Ribs | Sternum |
|---|---|---|
Structure - annulus and nucleus pulposus
|
vertebra origin: body, arch, and costal process
|
|
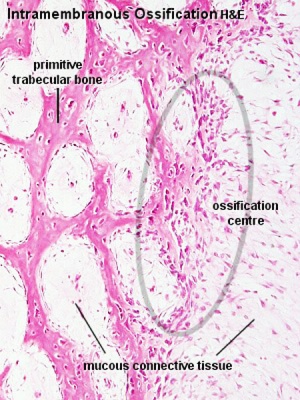
Intramembranous Ossification
- Specialized form of ossification from a mesenchymal membrane. (skull and clavicle)
- Neural crest-derived mesenchymal cells proliferate - some cells differentiate to form blood vessels, others become osteoblasts and begin secreting collagen-proteoglycan matrix that can bind calcium salts.
- Initial mesenchyme condensation is avascular.
- Angiogenesis is then required for intramembranous osteogenesis (vessels provide circulating factors)
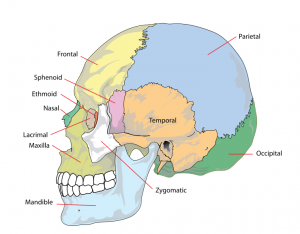
Skull
The Skull is a unique skeletal structure in several ways: embryonic cellular origin (neural crest), form of ossification (intramembranous and endochondrial) and flexibility (fibrous sutures). Musculoskeletal Development - Skull Development
The bones enclosing the brain have large flexible fibrous joints (sutures) which allow firstly the head to compress and pass through the birth canal and secondly to postnatally expand for brain growth.
These sutures gradually fuse at different times postnatally, firstly the metopic suture in infancy and the others much later. Abnormal fusion (synostosis) of any of the sutures will lead to a number of different skull defects.
Osteogenesis
- Osteoprogenitor cell - periosteum and endosteum
- Osteoblast - Secrete bone matrix, differentiate into osteocytes
- Osteocyte - Mature bone cell, Embedded in matrix, matrix calcifies soon after deposition
| Blood and Stromal Stem Cells |
|---|
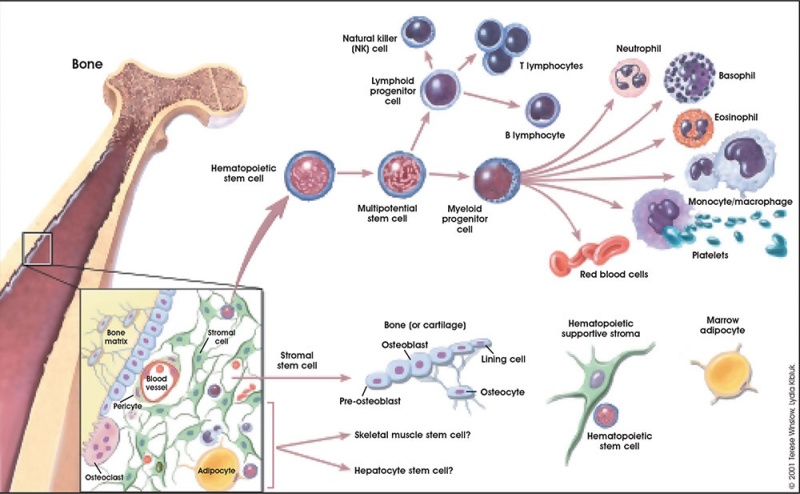
|
Osteoclastogenesis
- Formation of mature osteoclasts involved in bone resorption - the osteoblasts regulate this process through the production of RANKL (Receptor Activator for Nuclear Factor κ B Ligand) which is found on the cell surface of osteoblasts.
- RANKL is a key player in rheumatoid arthritis.
- Osteoclast origin - fusion of monocytes or macrophages, Blood macrophage precursor
- Attach to bone matrix - very large cells containing 15-20 nucleii.
- Lysosomes - released into space between ruffled border and bone matrix, enzymes break down collagen fibres, resorption bays or Howship's lacunae
Muscle
Myogenesis
(This lecture is about skeletal muscle)
- Skeletal muscle - cells originate from the paraxial mesoderm. Myoblasts undergo frequent divisions and coalesce with the formation of a multinucleated, syncytial muscle fibre or myotube. The nuclei of the myotube are still located centrally in the muscle fibre. In the course of the synthesis of the myofilaments/myofibrils, the nuclei are gradually displaced to the periphery of the cell.
- Cardiac muscle - cells originate from the prechordal splanchnic mesoderm.
- Smooth muscle - cells originate from undifferentiated mesenchymal cells. These cells differentiate first into mitotically active cells, myoblasts, which contain a few myofilaments. Myoblasts give rise to the cells which will differentiate into mature smooth muscle cells.
Skeletal Muscle Stages
| specified cells | myoblasts | primary myotube | secondary myotube | myofibre |
|---|---|---|---|---|
| somite myotome | migration to muscle location and proliferation | initial myoblast fusion | later myoblast proliferation and fusion | innervation and expression of contractile proteins |
- Myoblast - individual progenitor cells (from myotome)
- Myotube - multinucleated, but undifferentiated contractile apparatus (sarcomere)
- Myofibre (myofiber, muscle cell) - multinucleated and differentiated sarcomeres
- primary myofibres - first-formed myofibres, act as a structural framework upon which myoblasts proliferate, fuse in linear sequence
- secondary myofibers - second later population of myofibres that form surrounding the primary fibres.
| Mouse muscle development |
|---|

|
Muscle Fibre Types
- Motor neuron will regulate the contractile properties of all associated myofibres.
- A group of individual myofibres within a muscle will be innervated by a single motor neuron.
- myosin ATPase activity determines - type IIB, IIA, IIX, and I fibres
- Type I fibres - appear red, due to the presence of myoglobin (main type in fetal life)
- Type II fibres - appear white, due to the absence of myoglobin and their glycolytic nature.
| Muscle fibre type table | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
You do not need to know the detailed table below, it is provided for information purposes only.
|
Myotome
This term is used to describe the region of the somite that contributes skeletal muscle to the embryo body. Each somite pair level gives rise to a group of skeletal muscles supplied by a specific segmental spinal nerve. The muscle arises from a specific somite and the spinal nerve arises from a specific level of the spinal cord (identified by vertebral column).
| Spinal Nerve Table |
|---|
| You do not need to know the detailed table below, it is provided for information purposes only.
Humans spinal nerves (from top to bottom) and muscular functions:
|
Satellite Cells
|
Muscle stem cells located under the basal lamina around each skeletal muscle fibre.
|
|
Puberty
- Musculoskeletal mass doubles by the end of puberty
- regulated growth by - sex steroid hormones, growth hormone, insulin-like growth factors
- accumulation of (peak) bone mass during puberty relates to future osteoporosis in old age
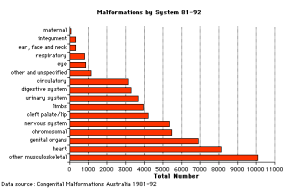
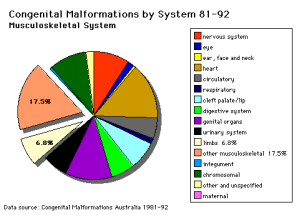
Abnormalities
Additional abnormalities will be covered in the limb development lecture.
- "Arthritis and musculoskeletal conditions affect more than 6 million Australians. In 2004-05, direct health expenditure on these conditions amounted to $4.0 billion or 7.5% of total allocated health expenditure in Australia." Health expenditure for arthritis and musculoskeletal conditions, 2004-05
Bone
Vertebra
- Spina Bifida - neural tube failure to close, disrupts neural arch formation
- Block vertebra - failure of vertebra separation, lumbar region, chrondrification abnormality
- Klippel-Feil Syndrome - non-segmented cervical vertebra, more female
- see also scoliosis
Rib
- Accessory rib (extra rib cervical or lumbar uni- or bilateral), short-rib polydactyly syndrome (lethal, chondroplasia), pigeon chest (rib overgrowth), funnel chest (sternum depression and lower costal cartilages)
Osteogenesis Imperfecta
- brittle-bone syndrome
- abnormal collagen type I, fail to assemble triple helix, degrade imperfect collagen, leads to fragile bones
Scoliosis
- assymetric growth impairment of vertebral bodies
- lateral deviation of spine (Lateral flexion, Forward flexion, Rotation of vertebral column on long axis)
- compensated by movement of vertebral column above and below affected region (producing a primary and two secondary curves)
- progresses rapidly in adolescence and becomes fixed once bone growth is completed.
Congenital Hip Dislocation
- Instability: 1:60 at birth; 1:240 at 1 wk: Dislocation untreated; 1:700
- congenital instability of hip, later dislocates by muscle pulls or gravity
- familial predisposition female predominance
- Growth of femoral head, acetabulum and innominate bone are delayed until the femoral head fits firmly into the acetabulum
Muscle
MH - Covered in next lecture and lab.
- Congenital Myopathies
- Muscular Dystrophy
References
- ↑ <pubmed>26893264</pubmed>
- ↑ <pubmed>22174793</pubmed>| PMC3235105 | PLoS One.
Online Textbooks
- Developmental Biology by Gilbert, Scott F. Sunderland (MA): Sinauer Associates, Inc.; c2000 Paraxial and intermediate mesoderm | Myogenesis: The Development of Muscle | Osteogenesis: The Development of Bones | Figure 14.10. Conversion of myoblasts into muscles in culture
- Molecular Biology of the Cell Alberts, Bruce; Johnson, Alexander; Lewis, Julian; Raff, Martin; Roberts, Keith; Walter, Peter New York and London: Garland Science; c2002 Search Molecular Biology of the CellBone Is Continually Remodeled by the Cells Within ItImage: Figure 22-52. Deposition of bone matrix by osteoblasts.Image: Figure 22-56. The development of a long bone.
Search
- Bookshelf mesoderm | somite | myogenesis | chondrogenesis | osteogenesis
- Pubmed mesoderm | somite | myogenesis | chondrogenesis | osteogenesis
External Links
External Links Notice - The dynamic nature of the internet may mean that some of these listed links may no longer function. If the link no longer works search the web with the link text or name. Links to any external commercial sites are provided for information purposes only and should never be considered an endorsement. UNSW Embryology is provided as an educational resource with no clinical information or commercial affiliation.
- UWA Blue Histology Skeletal Tissues - Muscle | Skeletal Tissues -Cartilage | Skeletal Tissues - Bone
- University of Kansas Histoweb Bone
- Loyola University Medical Education Network Part 9: Specialized Connective Tissue: Cartilage and Bone | Part 10: Endochondral Ossification
- University of Bristol ossification
Terms
| Bone Terms | ||
|---|---|---|
Bone Development
| ||
|
Images
| 2018 ANAT2341 - Timetable | Course Outline | Moodle | Tutorial 1 | Tutorial 2 | Tutorial 3 |
Labs: 1 Preimplantation and Implantation | 2 Reproductive Technology Revolution | 3 Group Projects | 4 GM manipulation mouse embryos | 5 Early chicken eggs | 6 Female reproductive tract | 7 Skin regeneration | 8 Vertebral development | 9 Organogenesis Lab | 10 Cardiac development | 11 Group projects | 12 Stem Cell Journal Club |
|
Lectures: 1 Introduction | 2 Fertilization | 3 Week 1/2 | 4 Week 3 | 5 Ectoderm | 6 Placenta | 7 Mesoderm | 8 Endoderm | 9 Research Technology | 10 Cardiovascular | 11 Respiratory | 12 Neural crest | 13 Head | 14 Musculoskeletal | 15 Limb | 16 Renal | 17 Genital | 18 Endocrine | 19 Sensory | 20 Fetal | 21 Integumentary | 22 Birth | 23 Stem cells | 24 Revision |
| Student Projects: Group Projects Information Project 1 | Project 3 | Project 4 | Project 5 | 2018 Test Student | Copyright |