| Educational Use Only - Embryology is an educational resource for learning concepts in embryological development, no clinical information is provided and content should not be used for any other purpose.
|
| ICD-11
|
|
LD50.03 Mosaicism, 45, X, 46, XX or XY - A disease caused by embryonic fusion, or by the loss of one of the sex chromosomes from a cell early in embryonic development; Gonadal status: normal or variable abnormalities of sexual anatomy, maturation or function. Phenotype: normal, or abnormal sexual development.
LD52.1 Male with double or multiple Y - A condition affecting males, caused by the presence of supernumerary Y chromosomes. This condition is asymptomatic. Confirmation is through observation of supernumerary Y chromosomes by karyotyping.
LD50.2 Mosaicism, lines with various numbers of X chromosomes
LD43.1 Mosaic monosomy of autosome - Any disease caused by embryonic fusion or loss of an autosome early in embryonic development, resulting in a subset of cells in the body having only one of a pair of autosomes.
|
Introduction
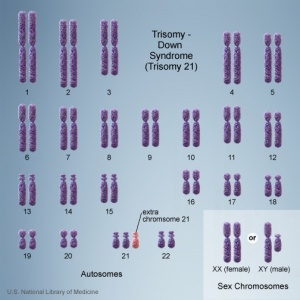
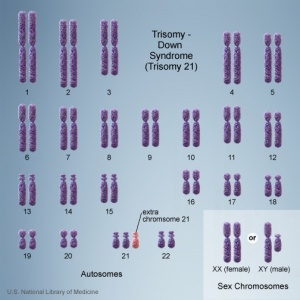
Chromosomes in trisomy 21
This page gives a general introduction to information about the genetic abnormality of trisomy mosaicism. The term "trisomy" refers to the abnormal copy number of a specific chromosome in all cells, that is 3 copies instead of 2. The abnormality is identified by the chromosome that is present as 3 copies within the cell. In humans, the most common trisomy is Trisomy 21 or Down syndrome. Other identified human trisomies include Trisomy 13, Trisomy 18 and Trisomy X.
In contrast, a "mosaicism" is a rare chromosome disorder characterized by having an extra copy of a chromosome in a proportion, but not all, of a person’s cells. These are examples of a class of very rare and not inherited genetic disorders. Mosaicism can arise initially meiotically, with a subsequent post-zygotic 'trisomy rescue' event, with adverse outcomes. Some mosaics could also be initially chromosomally normal, and arise purely post-zygotically.[1]
Some Recent Findings
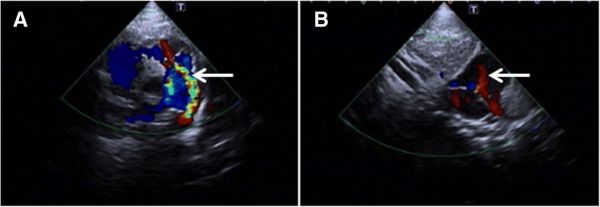
- Mosaic trisomy 22 in a 4-year-old boy with congenital heart disease and general hypotrophy: A case report[2] "Trisomy 22 mosaicism is a rare autosomal anomaly with survival compatibility. Recognition of the complete trisomy 22 which is incompatible with life from the mosaic form is critical for genetic counseling. Affected mosaic cases have prevalent clinical presentations such as webbed neck, developmental delay, abnormal ears, cardiac disorders, and microcephaly. Phenotype of these patients is milder than full chromosomal aneuploidy, and the severity of the phenotype depends on the count of trisomic cells. We describe a 4-year-old boy with mosaic trisomy 22 from healthy parents and no family history of any genetic disorders in the pedigree. METHOD AND RESULTS: The patient had determined dysmorphic clinical features including facial asymmetry, cleft palate, gastroenteritis, hydronephrosis, developmental delay, genital anomalies, dysplastic toenails, flattened nasal bridge, congenital heart defect, hearing loss, cryptorchidism, and hypotonic muscle. He is the first reported with hypothyroidism and larynx wall thickness in worldwide and the first with atrial septal defect (ASD) from Iran. Chromosomal analyses using G-banding indicated a de novo Mos 47,XY,+22(6)/46,XY(44) karyotype with no other chromosomal structural changes."
- Rare autosomal trisomies: Important and not so rare[3] "Noninvasive prenatal testing (NIPT) can assess chromosomes other than 13, 18, 21, X and Y. These rare autosomal trisomies (RATs) can adversely affect pregnancy outcome. METHODS: A prospective study of NIPT using the Illumina sequencing platform assessing all chromosomes were reported for further management. RESULTS: There were 28 RATs identified in 23 388 samples (one in 835), the most common being trisomy 7 (n = 6), followed by trisomy 16 (n = 4) and trisomy 22 (n = 3). Abnormal outcomes occurred in 16 cases: miscarriage (n = 6), true fetal mosaicism (n = 5), and fetal structural anomaly on ultrasound (n = 5). Growth restriction was seen in eight cases and correlated with very low-pregnancy-associated plasma protein-A levels. Two of the 17 live born babies had a structural anomaly, and one had a phenotype similar to mosaic trisomy 16 despite a normal microarray result. Rare autosomal trisomies are not rare and often associated with poor obstetric outcomes. They should be discussed with the clinician to guide management. Pregnancy outcomes varied by chromosome being generally favourable for some (eg, trisomy 7) and poor for others (eg, trisomy 22). In the presence of a RAT, pregnancy-associated plasma protein-A is predictive of placental dysfunction and fetal growth restriction."
- Unexpected finding of uniparental disomy mosaicism in term placentas: Is it a common feature in trisomic placentas?[4] "Non-invasive prenatal testing (NIPT) detects placental chromosome aberrations. When amniocentesis reveals a normal karyotype, confined placental mosaicism (CPM) may be assumed. In order to confirm this, placental cytogenetic studies were performed. METHOD: NIPT was conducted in the course of the Dutch TRIDENT study. Placentas of 10 cases with NIPT results indicating an autosomal trisomy and showing a normal (N = 9) or low mosaic karyotype (N = 1) in amniotic fluid (AF) were investigated. The cytotrophoblast as well as the mesenchymal core of two to four placental chorionic villi biopsies were studied with single nucleotide polymorphism (SNP) array. Clinical outcome data were collected. RESULTS: In 10/10 cases, CPM was proven. In 3/10 cases trisomy/uniparental disomy (UPD)/biparental disomy (BPD) mosaicism was discovered. In 2/3 cases, all three cell lines were present in the placenta, whereas BPD was found in AF. In 1/3 cases trisomy 22/UPD22 was present in AF while trisomy 22/BPD22 mosaicism was found in the placenta. Five of 10 pregnancies were affected with pre-eclampsia, low birth weight, preterm delivery, and/or congenital malformations. CONCLUSION: The presence of trisomy/UPD/BPD mosaicism in 3/10 cases that we investigated proves that trisomic zygote rescue may involve multiple rescue events during early embryogenesis. UPD mosaicism, when present in crucial fetal tissues, may explain the abnormal phenotype in undiagnosed cases."
|
| Older papers
|
| These papers originally appeared in the Some Recent Findings table, but as that list grew in length have now been shuffled down to this collapsible table.
See also the Discussion Page for other references listed by year and References on this current page.
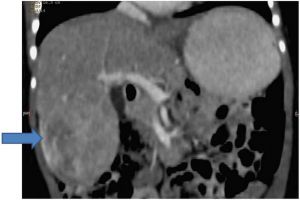
- Hepatoblastoma in a mosaic trisomy 18 child with hemihypertrophy[5] "To date, there are 12 reported cases of hepatoblastoma in trisomy 18 patients, three of whom had a mosaic chromosome pattern. We report on an 18-month-old child who had hemihypertrophy and developmental delay, was found to have hepatoblastoma on surveillance ultrasound scan, and was subsequently diagnosed with mosaic trisomy 18 on array comparative genomic hybridisation from a peripheral blood sample and molecular cytogenetic analysis of the tumour specimen. Although hemihypertrophy has been associated with mosaic trisomies, there are only a couple of published case reports of hemihypertrophy or asymmetry in mosaic trisomy 18 patients and none in the reported cases of hepatoblastoma in a mosaic trisomy 18 setting. We have reviewed the published case reports of hepatoblastoma in trisomy 18 patients and found that they seem to tolerate the intensive treatment very well if there are no significant comorbidities"
- The BabySeq Project "The BabySeq Project is a first-of-its-kind randomized clinical trial designed to examine how best to use genomics in clinical pediatric medicine by creating and safely testing methods for integrating sequencing into the care of newborns." Clinical Trials
|
Trisomy 22 Mosaicism
Rare Disease Database - The characteristic features of mosaic trisomy 22 typically include prenatal and postnatal growth failure or delay, asymmetrical development of the two sides of the body (hemidystrophy), congenital heart defects. While some patients with mosaic trisomy 22 have abnormal cognitive development, normal development has been documented for some children."
Trisomy 18 Mosaicism
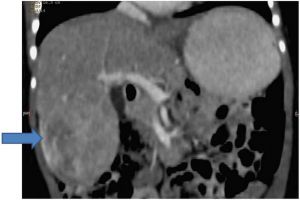
Mosaic Trisomy 18 hepatoblastoma CT
[5]Constellation of congenital abnormalities in an infant: a new syndrome or tissue-specific mosaicism for trisomy 18?[6] - "Blood lymphocyte and skin fibroblast karyotypes were normal. He died in the neonatal period of postoperative complications. On interphase fluorescence in-situ hybridization (FISH) using autopsy specimens, a significant number of cells in the liver (17%) were trisomic for chromosome 18, compared to normal control liver tissue. However, interphase FISH analyses of blood lymphocytes, skin fibroblasts, and kidney tissue were normal."
See also Trisomy 18
Trisomy 17 Mosaicism
NIH - rare diseases - "Some cases of trisomy 17 mosaicism detected during pregnancy have been confirmed in the baby after birth. The symptoms reported include: developmental delays, body asymmetry, slow growth, and cerebellar hypoplasia. Again, signs and symptoms may vary in these individuals depending on which cells and how many cells contain an extra chromosome 17."
Trisomy 14 Mosaicism
Rare Disease Database - "The disorder may be characterized by growth delays before birth (intrauterine growth retardation); failure to grow and gain weight at the expected rate (failure to thrive) during infancy; delays in the acquisition of skills requiring the coordination of mental and physical abilities (psychomotor delays); and mental retardation. Affected infants also have distinctive abnormalities of the head and facial (craniofacial) region, such as a prominent forehead; deeply set, widely spaced eyes; a broad nasal bridge; and low-set, malformed ears. Additional craniofacial abnormalities may include an unusually small lower jaw (micrognathia); a large mouth and thick lips; and incomplete closure or abnormally high arching of the roof of the mouth (palate). Many affected infants also have structural malformations of the heart (e.g., tetralogy of Fallot). In some cases, additional physical abnormalities may also be present."
Trisomy 12 Mosaicism
Trisomy 12 mosaicism confirmed in multiple organs from a liveborn child.[7] - "meiotic origin of the trisomy, maternal meiosis I, was determined. Mosaic aneuploidy was suspected because of pigmentary dysplasia, a frequent but non-specific finding in chromosomal mosaicism. The severe phenotype of this child, who died in infancy with a complex heart malformation, was probably a result of the high percentage of trisomic cells. Cytogenetic and interphase fluorescent in situ hybridization analyses showed a highly variable distribution of aneuploid cells in the nine tissues studied, from none in blood and ovary to 100% in spleen and liver."
Trisomy 10 Mosaicism

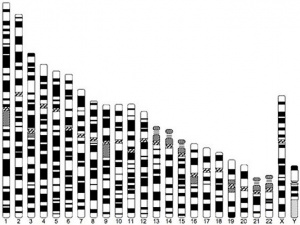
Trisomy 10 mosaicism karyotype
[8]Mosaicism trisomy 10 in a 14-month-old child with additional neurological abnormalities[8] - "Trisomy 10 is very rarely diagnosed, especially in living persons. Most reports of trisomy 10 pertain to prenatal diagnosis of trisomy 10 in the fetus. In addition, trisomy 10 has been reported as part of partial chromosomal abnormalities in some leukemic cells and tumor specimens. Only 6 cases of mosaicism trisomy 10 have been reported so far. None of these reports pertain to living children with neurological abnormalities."
Cardiovascular Abnormalities
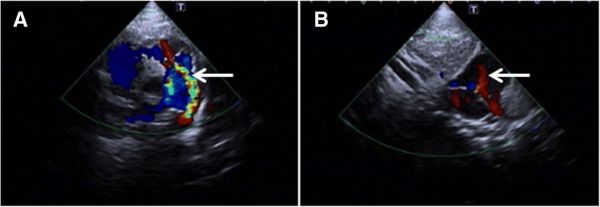
a - patent ductus arteriosus b - patent foramen ovale
Trisomy 9 Mosaicism
Rare Disease Database - "Associated symptoms and findings may vary greatly in range and severity, depending on the percentage of cells with the extra chromosome. However, common features include growth deficiency before birth (intrauterine growth restriction or IUGR); structural malformations of the heart that are present at birth (congenital heart defects); and/or distinctive differences in the shape of the skull and facial (craniofacial) region, such as a sloping forehead, a bulbous nose, short eyelid folds (palpebral fissures), deeply set eyes, and/or low-set ears. The syndrome may also be characterized by musculoskeletal, genital, kidney (renal), and/or additional physical anomalies. Intellectual disability is common and varies in severity."
Trisomy 8 Mosaicism
NIH - rare diseases - "The signs and symptoms vary, but may include distinctive facial features; intellectual disability; and joint, kidney, cardiac, and skeletal abnormalities. Males are more frequently affected than females."
Trisomy 2 Mosaicism
Prenatal diagnosis of trisomy 2 mosaicism[9] NIH - rare diseases - "Features of trisomy 2 mosaicism may include intrauterine growth restriction (IUGR), any of various birth defects, distinctive facial features, growth delay, developmental delays, and intellectual disabilities.[1][2] However, children with trisomy 2 mosaicism with no significant medical problems have been reported (although long-term follow-up was not available)."
Genetic Abnormality Topics
These statistics do not directly relate to trisomy mosaicism frequency, but that of genetic risk related to maternal age for all abnormalities.
Genetic Risk Maternal Age
Genetic Risk Maternal Age
| Age of Mother
|
Risk of Trisomy 21
|
Risk of Any Chromosomal Abnormality
|
| 20
|
1 in 1667
|
1 in 526
|
| 21
|
1 in 1667
|
1 in 526
|
| 22
|
1 in 1429
|
1 in 500
|
| 23
|
1 in 1429
|
1 in 500
|
| 24
|
1 in 1250
|
1 in 476
|
| 25
|
1 in 1250
|
1 in 476
|
| 26
|
1 in 1176
|
1 in 476
|
| 27
|
1 in 1111
|
1 in 455
|
| 28
|
1 in 1053
|
1 in 435
|
| 29
|
1 in 1000
|
1 in 417
|
| 30
|
1 in 952
|
1 in 384
|
| 31
|
1 in 909
|
1 in 384
|
| 32
|
1 in 769
|
1 in 323
|
| 33
|
1 in 625
|
1 in 286
|
| 34
|
1 in 500
|
1 in 238
|
| 35
|
1 in 385
|
1 in 192
|
| 36
|
1 in 294
|
1 in 156
|
| 37
|
1 in 227
|
1 in 127
|
| 38
|
1 in 175
|
1 in 102
|
| 39
|
1 in 137
|
1 in 83
|
| 40
|
1 in 106
|
1 in 66
|
| 41
|
1 in 82
|
1 in 53
|
| 42
|
1 in 64
|
1 in 42
|
| 43
|
1 in 50
|
1 in 33
|
| 44
|
1 in 38
|
1 in 26
|
| 45
|
1 in 30
|
1 in 21
|
| 46
|
1 in 23
|
1 in 16
|
| 47
|
1 in 18
|
1 in 13
|
| 48
|
1 in 14
|
1 in 10
|
| 49
|
1 in 11
|
1 in 8
|
| Table Data[10][11][12]
|
References
- ↑ Griffin DK & Ogur C. (2018). Chromosomal analysis in IVF: just how useful is it?. Reproduction , 156, F29-F50. PMID: 29945889 DOI.
- ↑ Kalayinia S, Shahani T, Biglari A, Maleki M, Rokni-Zadeh H, Razavi Z & Mahdieh N. (2019). Mosaic trisomy 22 in a 4-year-old boy with congenital heart disease and general hypotrophy: A case report. J. Clin. Lab. Anal. , 33, e22663. PMID: 30259573 DOI.
- ↑ Scott F, Bonifacio M, Sandow R, Ellis K, Smet ME & McLennan A. (2018). Rare autosomal trisomies: Important and not so rare. Prenat. Diagn. , 38, 765-771. PMID: 29956348 DOI.
- ↑ Van Opstal D, Diderich KEM, Joosten M, Govaerts LCP, Polak J, Boter M, Saris JJ, Cheung WY, van Veen S, van de Helm R, Go ATJI, Knapen MFCM, Papatsonis DNM, Dijkman A, de Vries F, Galjaard RH, Hoefsloot LH & Srebniak MI. (2018). Unexpected finding of uniparental disomy mosaicism in term placentas: Is it a common feature in trisomic placentas?. Prenat. Diagn. , 38, 911-919. PMID: 30187503 DOI.
- ↑ 5.0 5.1 Ahmad N, Wheeler K, Stewart H & Campbell C. (2016). Hepatoblastoma in a mosaic trisomy 18 child with hemihypertrophy. BMJ Case Rep , 2016, . PMID: 26795740 DOI.
- ↑ Shashi V, Golden WL, von Kap-Herr C & Wilson WG. (1996). Constellation of congenital abnormalities in an infant: a new syndrome or tissue-specific mosaicism for trisomy 18?. Am. J. Med. Genet. , 62, 38-41. PMID: 8779322 <38::AID-AJMG8>3.0.CO;2-S DOI.
- ↑ DeLozier-Blanchet CD, Roeder E, Denis-Arrue R, Blouin JL, Low J, Fisher J, Scharnhorst D & Curry CJ. (2000). Trisomy 12 mosaicism confirmed in multiple organs from a liveborn child. Am. J. Med. Genet. , 95, 444-9. PMID: 11146464
- ↑ 8.0 8.1 Gao Y, Ma YC, Ju YH & Li YN. (2018). Mosaicism trisomy 10 in a 14-month-old child with additional neurological abnormalities: case report and literature review. BMC Pediatr , 18, 266. PMID: 30081864 DOI.
- ↑ Sifakis S, Velissariou V, Papadopoulou E, Petersen MB & Koumantakis E. (2004). Prenatal diagnosis of trisomy 2 mosaicism: a case report. Fetal. Diagn. Ther. , 19, 488-90. PMID: 15539872 DOI.
- ↑ Hook EB. (1981). Rates of chromosome abnormalities at different maternal ages. Obstet Gynecol , 58, 282-5. PMID: 6455611
- ↑ Hook EB, Cross PK & Schreinemachers DM. (1983). Chromosomal abnormality rates at amniocentesis and in live-born infants. JAMA , 249, 2034-8. PMID: 6220164
- ↑ Schreinemachers DM, Cross PK & Hook EB. (1982). Rates of trisomies 21, 18, 13 and other chromosome abnormalities in about 20 000 prenatal studies compared with estimated rates in live births. Hum. Genet. , 61, 318-24. PMID: 6891368
Reviews
Mavridi A, Ntali G, Theodora M, Stamatelopoulos K & Michala L. (2018). A Spontaneous Pregnancy in a Patient with Turner Syndrome with 45,X/47,XXX Mosaicism: A Case Report and Review of the Literature. J Pediatr Adolesc Gynecol , 31, 651-654. PMID: 30012427 DOI.
Grati FR, Malvestiti F, Branca L, Agrati C, Maggi F & Simoni G. (2017). Chromosomal mosaicism in the fetoplacental unit. Best Pract Res Clin Obstet Gynaecol , 42, 39-52. PMID: 28284509 DOI.
Articles
Search Pubmed
Search Pubmed: genetic developmental abnormality
Terms
- anaphase - (Greek, ana = up, again) Cell division term referring to the fourth mitotic stage, where the paired chromatids now separate and migrate to spindle poles. This is followed by telophase.
- Mitosis Phases: prophase - prometaphase - metaphase - anaphase - telophase
- anaphase B - Cell division term referring to the part of anaphase during which the poles of the mitotic spindle move apart. (More? Cell Division - Mitosis)
- aneuploidy - Genetic term used to describe an abnormal number of chromosomes mainly (90%) due to chromosome malsegregation mechanisms in maternal meiosis I.
- disomy - Genetic term referring to the presence of two chromosomes of a homologous pair in a cell, as in diploid. See chromosomal number genetic disorders uniparental disomy and aneuploidy. Humans have pairs usually formed by one chromosome from each parent.
- meiosis I (MI) The first part of meiosis resulting in separation of homologous chromosomes, in humans producing two haploid cells (N chromosomes, 23), a reductional division.
- Meiosis I: Prophase I - Metaphase I - Anaphase I - Telophase I
- meiosis II - (MII) The second part of meiosis. In male human spermatogenesis, producing of four haploid cells (23 chromosomes, 1N) from the two haploid cells (23 chromosomes, 1N), each of the chromosomes consisting of two sister chromatids produced in meiosis I. In female human oogenesis, only a single haploid cell (23 chromosomes, 1N) is produced.
- Meiosis II: Prophase II - Metaphase II - Anaphase II - Telophase II
- prometaphase - (Greek, pro = before) Cell division term referring to the second mitotic stage, when the nuclear envelope breaks down into vesicles. Microtubules then extend from the centrosomes at the spindle poles (ends) and reach the chromosomes. This is followed by metaphase.
- Philadelphia chromosome - (Philadelphia translocation) Genetic term referring to a chromosomal abnormality resulting from a reciprocal translocation between chromosome 9 and 22 (t(9;22)(q34;q11)). This is associated with the disease chronic myelogenous leukemia (CML).
- prophase - (Greek, pro = before) Cell division term referring to the first mitotic stage, when the diffusely stained chromatin resolves into discrete chromosomes, each consisting of two chromatids joined together at the centromere.
- telophase - Cell division term referring to the fifth mitotic stage, where the vesicles of the nuclear envelope reform around the daughter cells, the nucleoli reappear and the chromosomes unfold to allow gene expression to begin. This phase overlaps with cytokinesis, the division of the cell cytoplasm.
- trisomy mosaicism - a rare chromosome disorder characterized by having an extra copy of a chromosome in a proportion, but not all, of a person’s cells.
- uniparental disomy - Genetic term referring to cells containing both copies of a homologous pair of chromosomes from one parent and none from the other parent.
| Cell Division Terms (expand to view)
|
meiosis | mitosis
- anaphase - (Greek, ana = up, again) Mitosis term referring to the fourth stage, where the paired chromatids now separate and migrate to spindle poles. This is followed by telophase.
- anaphase A - Mitosis term referring to the part of anaphase during which the chromosomes move.
- anaphase B - Mitosis term referring to the part of anaphase during which the poles of the mitotic spindle move apart.
- aneuploidy - (aneuploid) term used to describe an abnormal number of chromosomes mainly (90%) due to chromosome malsegregation mechanisms in maternal meiosis I.
- aster - (Latin, aster = star) star-like object visible in most dividing eukaryotic cells contains the microtubule organizing center.
- astral microtubule - spindle apparatus microtubule (MT) originating from the centrosome which does not connect to a kinetochore. These microtubules only exist during mitosis, the other spindle types are polar and kinetochore microtubules.
- autosomal inheritance - term used in hereditary diseases which means that the disease is due to a DNA error in one of the 22 chromosome pairs that are not sex chromosomes. Both boys and girls can then inherit this error. If the error is in a sex chromosome, the inheritance is said to be sex-linked.
- bivalent - (tetrad) a pair of homologous chromosomes physically held together by at least one DNA crossover.
- bouquet stage - meiosis term for when in prophase transition to the zygotene stage, the chromosome telomeres attachment to the inner nuclear envelope and form a cluster. This occurs before the onset of homologous pairing and synapsis. The name comes from the chromosomes resembling a "bouquet of flowers".
- diploid - (Greek, di = double + ploion = vessel) having two sets of chromosomes (2n), this is the normal euploidy state for all human cells, other than gametes that are haploid (n, a single set of chromosomes).
- diplotene stage- (diplotene phase, diplonema; Greek, diplonema = "two threads") meiotic stage seen during prophase I, the chromosomes separate from one another a small amount giving this appearance. In the developing human ovary, oocytes remain at the diplotene stage from fetal life through postnatal childhood, until puberty when the lutenizing hormone (LH) surges stimulate the resumption of meiosis. Prophase I, is divided into 5 stages (leptotene, zygotene, pachytene, diplotene, diakinesis) based upon changes associated with the synaptonemal complex structure that forms between two pairs of homologous chromosomes.
- euploidy - the normal genome chromosomal set (n, 2n, 3n) or complement for a species, in humans this is diploid (2n). The other classes of numerical chromosomal abnormalities include aneuploidy, polyploidy and mixoploidy.
- FUCCI - Acronym for Fluorescence Ubiquitination Cell Cycle Indicator a molecular tool for identifying the stage in the cell cycle. In G0/G1 cells express a red fluorescent protein and S/G2/M cells express a green fluorescent protein. (More? Tooth Development Movie)
- haploid - (Greek, haploos = single) Having a single set of chromosomes (n) as in mature germ/sex cells (oocyte, spermatozoa) following reductive cell division by meiosis. Normally cells are diploid, containing 2 sets of chromosomes. Ploidy refers to the number of sets of chromosomes in the nucleus of a cell.
- heteroplasmy - presence of more than one type of organellar genome. In humans this can refer to variations in the mitochondrial DNA (mtDNA). (More? PMID 26281784)
- homologous chromosomes - meiosis term for the two matching (maternal and one paternal) chromosomes that align during meiosis I.
- homologous recombination - meiosis term when DNA of homologous chromosomes is covalently exchanged to produce chromosomes with new allele combinations, and also links homologous chromosomes with each other to form a bivalent
- human genome - DNA within the 23 nucleus chromosome pairs and the cytoplasmic mitochondrial DNA.
- kinetochore - the protein structure formed on chromatids where the spindle kinetochore microtubules attach during cell division.
- kinetochore microtubule - spindle apparatus microtubule (MT) that attaches to the chromosome kinetochore by its plus end, the other spindle types are astral and polar microtubules.
- kinesin - a microtubule (MT) motor protein that exists in many isoforms and most move towards the MT positive end. Different isoforms have different functions within the spindle apparatus. PMID 20109570
- meiosis - reductive cell division required to produce germ cells (oocyte, spermatozoa) and for sexual reproduction. Note that only spermatozoa complete meiosis before fertilisation. Chromosome number is reduced from diploid to haploid, during this process maternal and paternal genetic material are exchanged. All other non-germ cells in the body divide by mitosis. (More? Meiosis | Spermatozoa Development | Oocyte Development | Week 1)
- meiosis I - (MI) the first part of meiosis resulting in separation of homologous chromosomes, in humans producing two haploid cells (N chromosomes, 23), a reductional division.
- meiosis II - (MII) the second part of meiosis. In male human spermatogenesis, producing of four haploid cells (23 chromosomes, 1N) from the two haploid cells (23 chromosomes, 1N), each of the chromosomes consisting of two sister chromatids produced in meiosis I. In female human oogenesis, only a single haploid cell (23 chromosomes, 1N) is produced. Meiosis II: Prophase II - Metaphase II - Anaphase II - Telophase II.
- meiotic silencing of unsynapsed chromatin - (MSUC) an aneuploidy protective mechanism for subsequent generations, during meiosis where chromosomes are silenced that fail to pair with their homologous partners.
- merotelic kinetochore - cell division abnormality in chromosomal attachment that occurs when a single kinetochore is attached to microtubules arising from both spindle poles. Normal chromosomal attachment in early mitosis, is by only one of the two sister kinetochores attached to spindle microtubules (monotelic attachment) later sister kinetochores attach to microtubules arising from opposite spindle poles (amphitelic attachment).
- metaphase - mitosis term referring to the third stage where mitotic spindle kinetochore microtubules align chromosomes in one midpoint plane. Metaphase ends when sister kinetochores separate. Originally based on light microscopy of living cells and electron microscopy of fixed and stained cells. A light microscope analysis called a "metaphase spread" was originally used to detect chromosomal abnormalities in cells. Mitosis Phases: prophase - prometaphase - metaphase - anaphase - telophase
- metaphase spread - In mitosis using light microscope analysis originally used to detect chromosomal abnormalities in cells, as chromosomes are only visible during cell division.
- microfilament - (MF) cytoskeleton filament normally required for cytoplasmic intracellular transport, motility and cell shape. Named by the actin monomers assembling into the smallest in cross-section of the three filament systems (microtubules and intermediate filaments). This system is disassembled and reassembled as the contractile ring for cytokinesis (cytoplasm division) following cell division mitosis and meiosis.
- microtubule - (MT) cytoskeleton filament normally required for cytoplasmic intracellular transport and motility. Named by the tubulin monomers assembling into "tubes", and are the largest in cross-section of the three filament systems (microfilaments and intermediate filaments). This system is disassembled and reassembled as the spindle apparatus during cell division.
- mitochondrial DNA - (mtDNA) multiple copies of a small circular DNA molecule located within the mitochondria matrix. In humans 16,568 bp in length containing 37 genes, originally inherited only from the oocyte (maternal inheritance).
- mitosis - (M phase) The normal division of all cells, except germ cells, where chromosome number is maintained (diploid). In germ cell division (oocyte, spermatozoa) meiosis is a modified form of this division resulting in reduction in genetic content (haploid). Mitosis, division of the nucleus, is followed by cytokinesis the division of the cell cytoplasm and the cytoplasmic contents. cytokinesis overlaps with telophase.
- p - chromosome short arm (possibly French, petit) and used along with chromosome and band number to indicate genes located on this arm of the chromosome. The chromosome long arm is identified as q (possibly French, tall) chosen as next letter in alphabet after p. These chromosomal arms are only seen when the chromosome is folded for cell division.
- polar microtubule - spindle apparatus microtubule (MT) that can arise from either pole and overlap at the spindle midzone. This interdigitating structure consisting of antiparallel microtubules is responsible for pushing the poles of the spindle apart. The other spindle types are astral and kinetochore microtubules.
- prometaphase - (Greek, pro = before) mitosis term referring to the second stage, when the nuclear envelope breaks down into vesicles. Microtubules then extend from the centrosomes at the spindle poles (ends) and reach the chromosomes. This is followed by metaphase.
- pronuclear fusion - (Greek, pro = before) the process of the fusion of the two haploid nuclear structures (pronuclei) contributed from the spermatazoa and oocyte to form the first diploid nucleus cell. Can also be called "fusion of pronuclei".
- pronucleus - (Greek, pro = before; plural, pronuclei) the two haploid nuclei or nuclear structures containing the genetic material from the spermatozoa and the oocyte. These two haploid nuclei will fuse together to form the first diploid nucleus cell, the zygote. Therefore the nuclear structures that exist "before the nucleus", the plural term is pronuclei.
- prophase - (Greek, pro = before) - mitosis term referring to the first stage, when the diffusely stained chromatin resolves into discrete chromosomes, each consisting of two chromatids joined together at the centromere.
- prophase I - meiosis term refers to the first phase of meiosis I, which together with meiosis II results in the reductive cell division only occurring gametes. Prophase can be further divided into a number of stages: leptotene zygotene, pachytene, diplotene, diakinesis.
- q - chromosome long arm (possibly French, tall), the next letter in alphabet after p, and used along with chromosome and band number to indicate genes located on this arm of the chromosome. The chromosome short arm is identified as p (possibly French, petit). These chromosomal arms are only seen when the chromosome is folded for cell division.
- S phase - during interphase of cell cycle where DNA is duplicated prior to second growth period (G2 phase) that is followed by mitosis (M phase).
- synapsis - (syndesis) meiosis term for the pairing of two homologous chromosomes that occurs during prophase I.
- synaptonemal complex - meiosis term for a protein structure essential for synapsis of homologous chromosomes. (proteins SCP3 and SCP1).
- telomere - region found at each end of the chromosome and involved in cellular ageing and the capacity for division. The regions consist of repeated sequences protecting the ends of chromosomes and harbour DNA repair proteins. In the absence of the enzyme telomerase, these regions shorten during each cell division and becoming critically short, cell senescence occurs.
- telophase - mitosis term referring to the fifth stage, where the vesicles of the nuclear envelope reform around the daughter cells, the nucleoli reappear and the chromosomes unfold to allow gene expression to begin. This phase overlaps with cytokinesis, the division of the cell cytoplasm.
- telomerase - the enzyme that maintains the chromosome end length, the telomeres, involved in cellular ageing and the capacity for division. Absence of telomerase activity leads to the chromosome ends shorten during each cell division, becoming critically short and cell senescence then occurs.
- tetrad - (bivalent) a pair of homologous chromosomes physically held together by at least one DNA crossover.
|
|
|
External Links
External Links Notice - The dynamic nature of the internet may mean that some of these listed links may no longer function. If the link no longer works search the web with the link text or name. Links to any external commercial sites are provided for information purposes only and should never be considered an endorsement. UNSW Embryology is provided as an educational resource with no clinical information or commercial affiliation.
Glossary Links
- Glossary: A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | Numbers | Symbols | Term Link
Cite this page: Hill, M.A. (2024, April 27) Embryology Trisomy Mosaicism. Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/Trisomy_Mosaicism
- What Links Here?
- © Dr Mark Hill 2024, UNSW Embryology ISBN: 978 0 7334 2609 4 - UNSW CRICOS Provider Code No. 00098G