SH Practical - Lymphatic Structure and Organs
| Embryology - 27 Apr 2024 |
|---|
| Google Translate - select your language from the list shown below (this will open a new external page) |
|
العربية | català | 中文 | 中國傳統的 | français | Deutsche | עִברִית | हिंदी | bahasa Indonesia | italiano | 日本語 | 한국어 | မြန်မာ | Pilipino | Polskie | português | ਪੰਜਾਬੀ ਦੇ | Română | русский | Español | Swahili | Svensk | ไทย | Türkçe | اردو | ייִדיש | Tiếng Việt These external translations are automated and may not be accurate. (More? About Translations) |
Objectives
- Understand the major cell types of blood as they appear in blood smears
- Understand the histology and organization of lymphoid organs (thymus, spleen, lymph node)
- Understand the histology and organization of lymphoid tissue, particularly that associated with the gastrointestinal tract.
Resources
| Moodle Lab Slides
Note - Moodle icon links appearing below on this page go directly to Lab Slide. |
- SH Lecture Lymphatic Structure and Organs | PDF Lecture 2019
- Practical Room - Health and Safety Information PDF
- Practical Manual Notes - 2018 Practical 1 PDF | 2017 Practical 1 PDF | 2016 page | 2015 page | 2013 Practical 1 PDF
- UNSW Embryology SH Lecture - Lymphatic Structure and Organs | SH Practical - Lymphatic Structure and Organs
- UNSW Library - Kierszenbaum, A. L., & Tres, L. L. (2012). Histology and cell biology: An introduction to pathology. Philadelphia, PA: Elsevier Saunders. UNSW Students have online access to the current 3rd edn. through the UNSW Library subscription.
Chapter 10. Immune-Lymphatic System
Virtual Slides - Moodle and BEST Links
| SH Practical - Lymphatic Structure and Organs - Virtual Slides | |||
|---|---|---|---|
| Moodle | BEST | MH Annotation | |
| Slide - Human Blood Smear | BEST - Human Blood Smear | annotation | |
| Slide - Bone Marrow Smear | BEST - Bone Marrow Smear | annotation | |
| Slide - Thymus (infant) | BEST - Thymus (infant) | annotation | |
| Slide - Thymus (adult 1) | BEST - Thymus (adult 1) | annotation | |
| Slide - Spleen | BEST - Spleen | annotation | |
| Slide - Spleen (silver stain) | BEST - Spleen (silver stain) | annotation | |
| Slide - Lymph Node | BEST - Lymph Node | annotation | |
| Slide - Lymph Node (silver stain) | BEST - Lymph Node (silver stain) | annotation | |
| Slide - Lingual tonsil (tongue} | BEST - Lingual tonsil (tongue} | annotation | |
| Slide - Pharyngeal tonsil | BEST - Pharyngeal tonsil | annotation | |
| Slide - Appendix | BEST - Appendix | annotation | |
| Note - My annotations available for revision purposes only and may contain errors. Always refer to your own labels. Lecture | Prac Support | Quiz | |||
Here is another appendix slide BEST - Appendix 2
Virtual Slides
- Slide - Human Blood Smear
- Slide - Bone Marrow Smear
- Slide - Thymus (infant)
- Slide - Thymus (adult 1)
- Slide - Thymus (adult 2)
- Slide - Spleen
- Slide - Spleen (silver stain)
- Slide - Lymph Node
- Slide - Lymph Node (silver stain)
- Slide - Lingual tonsil (tongue}
- Slide - Pharyngeal tonsil
- Slide - Appendix
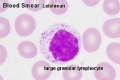
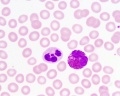
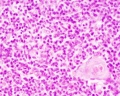
Blood Cells: Lymphocyte
Blood | Thymus | Spleen | Lymph Node | Tonsil | GIT | Lymphatic Quiz
Introduction
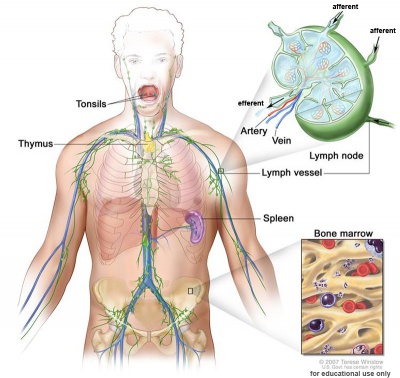
This practical class has 2 main parts. The first part will briefly revise the cellular components of blood and their development.
The second part will look in more detail at the organs and tissues associated with lymphoid (lymphatic) immune function.
The Practical involves studying selected slides from the Virtual Slide Box. Some text in these practical notes modified from Virtual Slidebox Histology. Additional online self-directed learning resources are available from UNSW Embryology page (address above) including external resource and glossary links.
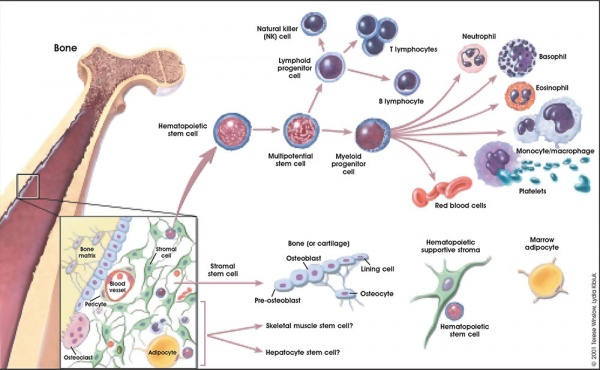
Blood
The circulating blood is a liquid connective tissue consisting of cells (red and white blood cells), fragments of cells (platelets) and liquid (plasma). The different cell types are all derived from haemopoietic stem cells located in the bone marrow. Red blood cells (RBCs) have a metabolic role, in carrying oxygen to tissues and carbon dioxide to the lungs. White blood cells (WBCs or leukocytes) have a role in the body’s defence, and are an important clinical indicator of disease.
| Slide - Human Blood Smear |
Find an area in the smear where the red blood cells are spread out and individual cells can be identified.
Identify:
- Red blood cells (7-8 um diameter anucleate biconcave disc)
- White blood cells: neutrophils, eosinophils, basophils, lymphocytes and monocytes (basophils are normally rare).
Note the presence or absence of granules, shape of the nucleus and relative cell sizes. Also identify platelets.
- 60% neutrophils (50% - 70%)
- 30% lymphocytes (20% - 40%)
- 3% eosinophils (>0% - 5%)
- 5% monocytes (1% - 9%)
- 0.5% basophils (>0% - 2%)
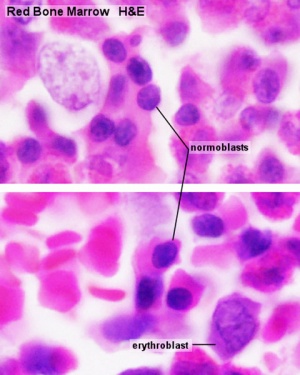
| Slide - Bone Marrow Smear |
- Do not attempt to identify all the cells in the bone marrow smear, but compare its appearance with that of the blood smear.
- Haematopoiesis (hematopoiesis) is the process of blood cell differentiation and occurs mainly in the bone marrow.
- This bone marrow smear will contain a large number of differentiating blood cells: band cells and normoblasts.
- band cell - (band neutrophil, band form or stab cell) WBC precursor. Previous stage metamyelocytes have a bent nucleus that becomes pronounced in this last immature form WBC, the band cells. All WBCs form band stage, as neutrophils are most abundant in blood, most will be neutrophilic band cells.
- normoblast - intense even nuclear stain, eosinophilic cytoplasm, RBC progenitor.
- The largest cells visible are megakaryocytes, which are responsible for platelet production.
- These cells are clearly visible even at low magnifications.
- Megakaryoblast - very dark and large
- Megakaryocytes - even larger but lighter in colour
Lymphocyte - differentiation begins in the bone marrow and continues in central lymphoid organs (bone marrow - B cells and thymus - T cells), then in the peripheral lymphoid organs (lymph nodes, spleen).
Neutrophils - are produced and stored in large reserves in the bone marrow. Allowing rapid deployment when required into the circulation. These cells are also the most abundant in circulation (50% - 70%) and possess a potent microbicidal activity.
- Bone Marrow Histology: Blood Development | Marrow overview | Megakaryocyte | Megakaryocyte detail | Myelocyte | Normoblast | Reticulocyte | Blood Histology | Bone Development | Category:Blood
- bone marrow cells
Blood Histology
|
Lymphocyte Electron Micrographs
- Blood Histology: Blood Development | Blood Cell Number Table | Lymphocyte 1 | Lymphocyte 2 | Lymphocyte 3 | Lymphocyte 4 | Monocyte 1 | Monocyte 2 | Monocyte 3 | Monocyte 4 | Neutrophils 1 | Neutrophil 2 | Neutrophil 3 | Neutrophil 4 | Eosinophil 1 | Eosinophil 2 | labeled Neutrophil and Eosinophil | unlabeled - Neutrophil and Eosinophil | Basophil 1 | Basophil 2 | Basophil 3 | Platelet 1 | Platelet 2 | Reticulocyte | Megakaryocyte | Movie | Bone Marrow Histology | Category:Blood
| Blood Cells |
|---|
Adult human blood cell numbers shown in the table below is for reference purposes.
Blood Cell NumbersThe adult ranges of cells / 1 litre (l), total blood volume is about 4.7 to 5 litres. Blood Development | Blood Histology Red Blood Cells
Leukocytes (white blood cells)
Granulocytes
Non-Granulocytes
Lymphocytes
Platelets
|
- Bone Marrow Histology: Blood Development | Marrow overview | Megakaryocyte | Megakaryocyte detail | Myelocyte | Normoblast | Reticulocyte | Blood Histology | Bone Development | Category:Blood
Blood Questions
- What is the normal blood haematocrit range?
- Does this haematocrit differ for male/female?
- What is the function of the various blood cells?
- Which tissues have very large numbers of white blood cells and why?
- In blood, can you identify the difference between T and B lymphocytes?
Lymphoid Tissue
Thymus
Main Cell Types
|
| FYI - T Cell Maturation |
|---|
| This is not part of the histology class, but it helps you understand the process of T cell maturation and cellular interactions.
This is the pathway of an immature T cell entering the thymus and undergoing maturation.
|
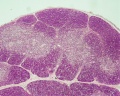
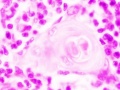
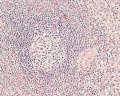
| Slide - Thymus (infant) |
Section of a thymus lobe of an infant.
The thymus changes its histological appearance from infant to puberty to adult, in a process called involution (replacement of cortical lymphoid tissue by adipose tissue) and there is also an increase in the size of thymic corpuscles.
At low magnification: note the surrounding connective tissue capsule along the surface. The thymus is divided into many smaller lobules by connective tissue septa extending inward from the capsule. These lobues have a cortex (dark staining) and a medulla (pale staining). The interlobular septa do not penetrate into the medulla, and lobules are joined together in the medulla. Some septa may carry blood vessels and efferent lymphatic vessels.
At high magnification: Cortex has a dense layer of closely packed cells (developing and maturing T lymphocytes, thymocytes). Medulla consist of an eosinophilic central mass surrounded by concentrically arranged epithelial cells (Hassalls corpuscles). Do not confuse them with blood vessels.
Compare the appearance of the infant with the adult thymus (below).
Blood-Thymic Barrier
- Blood vessels are separated from thymus cortex by epithelioreticular cells.
- impermeable to most macromolecules.
- Barrier layers: capillary endothelium - endothelial basal lamina- perivascular CT sheath - basal lamina of epithelioreticular cells - epithelioreticular cell sheath
Thymus Involution
A postnatal process defined as a decrease in the size, weight and activity of the gland with advancing age. In a recent review[1], thymic involution was described as a result of high levels of circulating sex hormones, in particular during puberty, and a lower population of precursor cells from the bone marrow and finally changes in the thymic microenvironment.
|
|
- Reticular cells - abundant and their cytoplasm is eosinophilic. Nucleus is large, ovoid and light nuclei may contain one or two nucleoli.
- Macrophages - also abundant and difficult to distinguish from reticular cells, may be larger and paler.
- Lymphocytes - in both cortex and medulla, but more numerous in the cortex. Sizes are variable (5 - 15 µm) in the cortex but usually small in the medulla, most will be developing T-lymphocytes.
T-lymphocyte pathway:
- stem cells enter the cortical regions of the thymus
- they divide in the cortex to form lymphocytes
- only a small fraction of generated cells (10-30%) will leave the thymus (the rest die and removed by cortical macrophages)
- lymphocytes migrate to the medulla
- from the medulla enter into the blood
Thymus Histology
- Thymus Histology: Fetal Thymus overview | Fetal Thymus Medulla | Fetal Thymus Cortex | Adult Thymus | unlabeled fetal overview | unlabeled fetal medulla |unlabeled fetal thymic corpuscle |unlabeled fetal cortex | unlabeled adult overview | Category:Thymus | Immune System Development
Spleen

| Spleen Overview | Red Pulp |
|---|---|
|
|
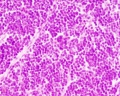
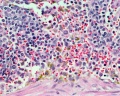
| Slide - Spleen |
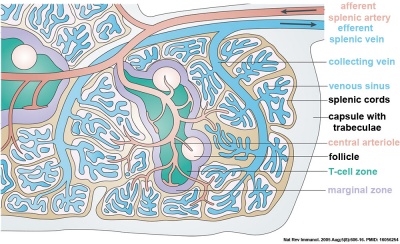
The spleen in fetal life is a site for blood formation (hematopoiesis). The adult spleen has 2 main functions: immune, as a major site of antigen presentation for the circulation system and removal of aged erythrocytes from the circulation. The spleen has a dense connective tissue capsule, which contains trabeculae running into the interior of the spleen forming incomplete compartments (as in the thymus). The stroma is mainly composed of reticular connective tissue and cells. There is a Hilum, which contains arteries and veins, but unlike a lymph node, there are no lymphatics. It should also be noted that the spleen cannot be divided into a medulla and cortex, which helps differentiate it from the thymus or a lymph node.
The spleen is a major site of antigen presentation for the circulation system, and in fetal life, it is a site for hematopoiesis. It also functions in removing senescent erythrocytes from the circulation. The spleen is surrounded by a dense connective tissue capsule, which contains trabeculae running into the interior of the spleen forming incomplete compartments. The stroma is mainly composed of reticular connective tissue and cells. There is a Hilum, which contains arteries and veins, but unlike a lymph node, there are no lymphatics. It should also be noted that the spleen cannot be divided into a medulla and cortex, which helps differentiate it from the thymus or a lymph node.
Identify connective tissue capsule, trabeculae, white pulp, red pulp, lymphatic nodules, and central arterioles.
The two main interior divisions of the spleen are white and red pulp. White pulp consists of a sheath of lymphoid cells surrounding an eccentrically located central arteriole. The T lymphocytes immediately surrounding the central arteriole are referred to as periarterial lymphatic sheaths (PALS). Surrounding that is a layer of peripheral white pulp (PWP), which is composed of B lymphocytes. Antigen enters the white pulp from the central arteriole, activates the PALS, which then activates the PWP. The marginal zone on the periphery of the white pulp is believed to be an important area for trapping antigens and initiation of immune responses. Both lymphocytes and macrophages are present in the marginal zone.
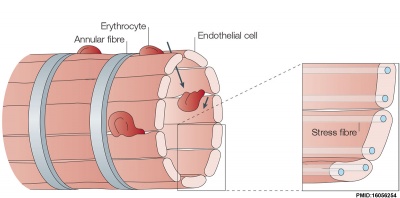
The red pulp consists of splenic cords of Billroth and splenic sinusoids. The splenic cords of Billroth contain reticular cells, macrophages, lymphocytes, plasma cells, and erythrocytes. The splenic sinusoids are modified capillaries with an exceptionally wide lumen and spaces in the wall to allow cells to squeeze in and out. Macrophages are also able to extend processes into the sinusoid, allowing them to identify senescent red blood cells.
| Mice and Men |
|---|
| This information is not examinable, but should be of interest to you as a medical researcher as the mouse is often used as a model in ham diseases.
|
Blood enters the spleen via the splenic artery at the hilum. The blood then travels through the trabecular arteries, central arterioles, penicillar arterioles, capillaries, splenic sinusoids, trabecular veins, and finally out the splenic vein at the hilum.
Spleen silver-stained to show connective tissue reticular fibers (black), compare this with the silver-stained lymph node.
| Slide - Spleen (silver stain) |
| Histology - Silver Stain |
|---|
| (Silver Impregnation)
There are a variety of specialised silver staining techniques. Most of the teaching slides use silver staining to show connective tissue (collagen) components. Silver deposits can be formed by 3 different reactions: argentaffin, argyrophil, and Ion-exchange.
|
Spleen Histology
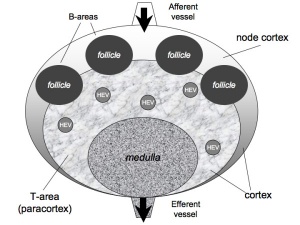
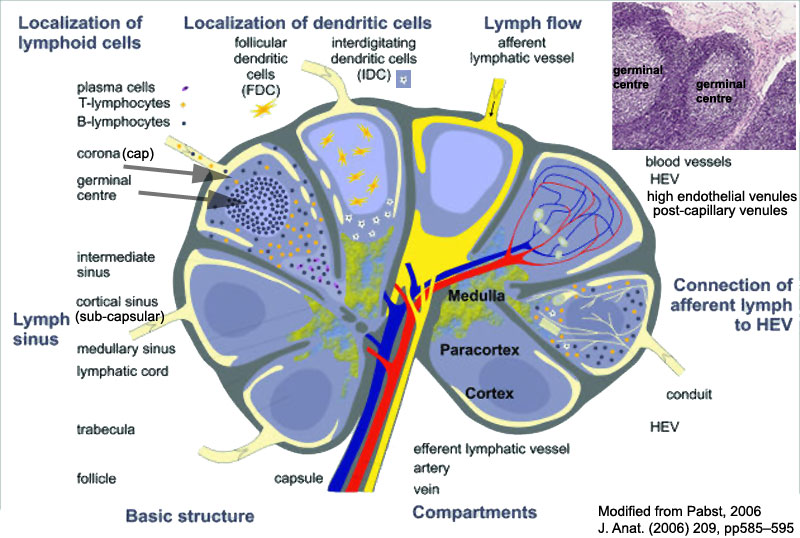
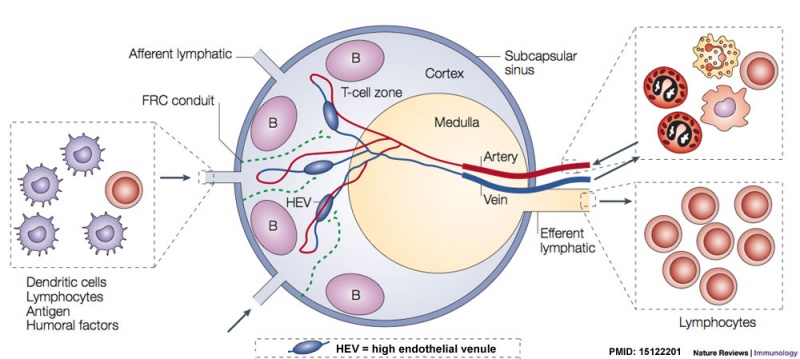
Lymph Node
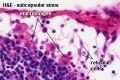
- Lymph Node Histology: Subcapsular Sinus | Follicle | Germinal Centre | Medullary Cords and Sinuses | High Endothelial Venules | Macrophages | Node cartoons
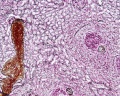
| Slide - Lymph Node |
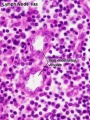
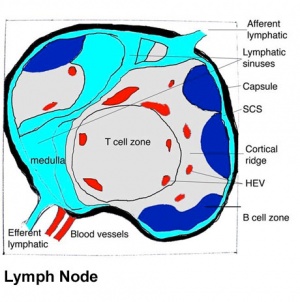
Lymph nodes are peripheral lymphoid organs involved in helping the body defend against foreign organisms. Lymph, which contains antigen and antigen presenting cells, flows from local tissue lymphatic vessels and enters the subcapsular sinus. The lymph then filters though the intermediate sinuses, into the medullary sinuses, and finally out the efferent lymphatic vessels at the hilum before it is returned to the circulation. B and T cells are numerous in the lymph node, and they enter through afferent arteries, enter the lymphoidal tissue across specialized vessels called high-endothelial venules, and return to the circulation via efferent veins.
Identify the following features: the connective tissue capsule, the trabeculae, the subcapsular sinus (lying immediately below the capsule), the intermediate sinus (lying next to a trabecula), outer cortex (composed of lymphatic nodules follicles), the inner cortex (non-nodular area between outer cortex and medulla) and the medulla (with medullary cords and medullary sinuses).
| Slide - Lymph Node (silver stain) |
Lymph node silver stained to show connective tissue reticular fibers (black).
Identify reticular fiber distribution in: capsule, trabeculae, subcapsular sinuses, intermediate sinuses, lymphoid nodules, the inner cortex, and the medulla.
Lymph Node Histology
- Lymph Node Histology: Subcapsular Sinus | Follicle | Germinal Centre | Medullary Cords and Sinuses | High Endothelial Venules | Macrophages | Node cartoons
| <html5media height="285" width="300">File:Mouse_adult_lymph_node_03.mp4</html5media>
Click Here to play on mobile device Adult Mouse Lymph Node - T cells within the medullary sinus.
ReferencesWei SH, Rosen H, Matheu MP, Sanna MG, Wang SK, Jo E, Wong CH, Parker I & Cahalan MD. (2005). Sphingosine 1-phosphate type 1 receptor agonism inhibits transendothelial migration of medullary T cells to lymphatic sinuses. Nat. Immunol. , 6, 1228-35. PMID: 16273098 DOI. Cahalan MD & Parker I. (2008). Choreography of cell motility and interaction dynamics imaged by two-photon microscopy in lymphoid organs. Annu. Rev. Immunol. , 26, 585-626. PMID: 18173372 DOI. Movie SourceMichael D. Cahalan, Professor and Chair, Department of Physiology and Biophysics, University of California, Irvine. Lab Two-photon imaging movies reproduced with permission of Prof. Cahalan. | ||||||||||||||||||||||||||||||||||||||||||||||||
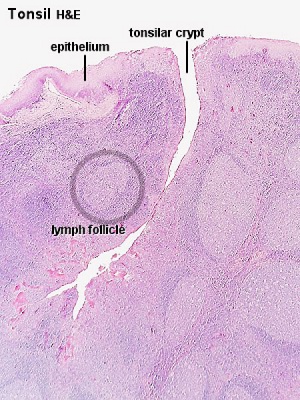
Tonsil
| Slide - Lingual tonsil (tongue} |
The lingual tonsils are numerous small tonsils located at the base of the tongue. They are covered by a stratified squamous epithelium, but are not enclosed by a capsule. Salivary glands and skeletal muscle are directly adjacent to the tonsil.
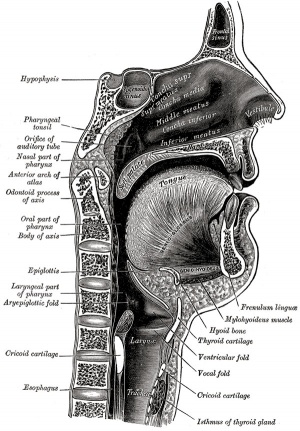
| Slide - Pharyngeal tonsil |
Closely packed lymph nodules comprise the outer portion of this organ. The pharyngeal tonsil is covered with a pseudostratified columnar epithelium with cilia (typical of respiratory tract).
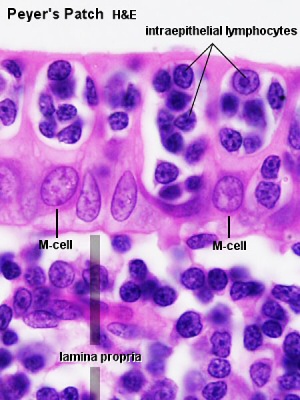
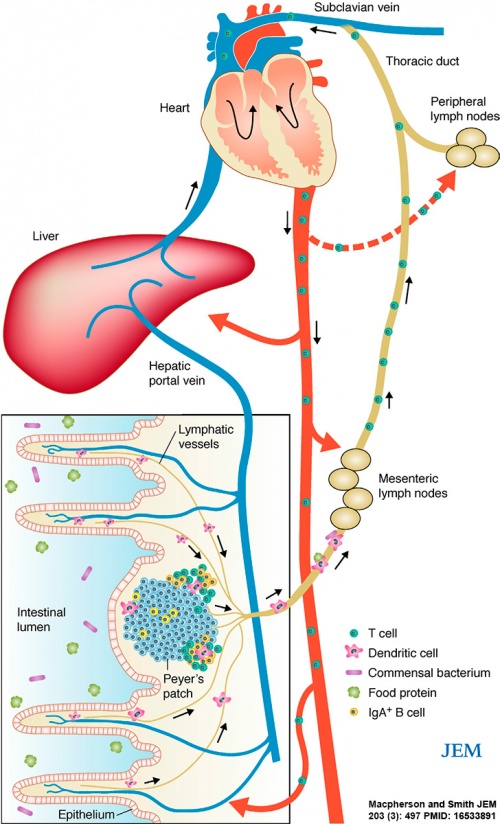
Gastrointestinal Tract
Gastrointestinal tract intestine immune overview[2]
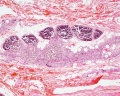
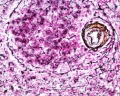
| Slide - Appendix |
The appendix (vermiform appendix) anatomy is as a finger-like structure that arises from the cecum. The length (2.5-13 cm) is longer in both infants and children and also has more abundant lymphatic tissue in early life. The wall structure is similar to the small intestine (though with no villi), nor plicae circularis.
Lymph nodules surround the lumen of the gastrointestinal tract and extend from the mucosa into the submucosa. Note in this section most of the muscularis mucosa has been obliterated by lymphatic invasion.
- Immune Images: Oesophagus MALT | Colon MALT | Peyer's patch overview | Peyer's patch detail | Cartoon - IEL development | Cartoon - IEL function | Cartoon - IEL differentiation | Mesenteric Lymph Nodes overview | Palatine Tonsil | Tonsil | Immune System Development
Lymphatic Questions
- What is the difference between stroma and parenchyma?
- Which cells make reticular fibers?
- Why are lymphoid tissues associated with the gastrointestinal tract and respiratory tissues?
- What is an antigen and what does it produce in the immune system?
- Where can tonsilar tissue be found in the gastrointestinal tract?
Terms
A few key terms associated with the Lymphoid system.
- adenoid - (Greek " +-oeides = in form of) in the form of a gland, glandular; the pharyngeal tonsil.
- afferent lymph - vessel carrying lymph towards a node containing antigen-presenting cells, antigen, effector and memory T cells, and regulatory T cells.
- acquired immune deficiency syndrome - (AIDS) note this is now better described as "advanced HIV disease", decrease in the number of CD4 T cells. (More? Immunobiology - AIDS)
- anastomose - joining of two tubes or structures together.
- Antibody mediated immunity - the immune function of plasma cells (active B lymphocytes) secreting antibody which binds antigen.
- antibodies - mammals have five classes (IgA, IgD, IgE, IgG, and IgM)
- antigen - any substance that is recognised by the immune system and stimulates antibody production.
- appendix - is a gut-associated lymphoid tissue (GALT) located at the beginning of the colon. The anatomy is as a finger-like structure that arises from the cecum. The length (2.5-13 cm) is longer in both infants and children and also has more abundant lymphatic tissue in early life. The wall structure is similar to the small intestine (though with no villi), nor plicae circularis. Lymph nodules surround the lumen of the gastrointestinal tract and extend from the mucosa into the submucosa.
- B cell - (B-cell, B lymphocyte) historically named after a structure called the bursa of Fabricius in birds, a source of antibody-producing lymphocytes. These immune cells develop in the bone marrow. (More? Electron micrographs of nonactivate and activated lymphocytes)
- blood - liquid connective tissue containing cells of the lymphatic system see Cardiovascular terms
- B lymphocyte - (B cell, B-cell)
- BALT - (Bronchus Associated Lymphoid Tissue) immune tissue associated with the respiratory tract.
- band cell - (band neutrophil or stab cell) immature neutrophil seen in bone marrow smear, a cell undergoing granulopoiesis, derived from a metamyelocyte, and leading to a mature granulocyte. Also occasionally seen in circulating blood.
- bone marrow sinusoid - endothelial cells and no supporting cells vascular space supplied by arteriole and capillary vessels, interconnected by inter-sinusoidal capillaries, spanning throughout the bone marrow. Radially distributed around the draining central sinus (about 100 µm in diameter). Bone marrow sinusoids are unique and are not comparable with regular veins.
- cecum - (caecum, Latin, caecus = "blind") within the gastrointestinal tract a pouch that connects the ileum with the ascending colon of the large intestine.
- cell - has a specific cell biology definition, but is often used instead of "lymphocyte" when describing B and T cells.
- cell-mediated immunity - the immune function of T lymphocytes. (More? Immunobiology - T Cell-Mediated Immunity)
- central tolerance - in thymus mediated by cortical epithelial cells, medullary epithelial cells and thymic dendritic cells, involves deletion of self reactive thymocytes (T cell) (see [https://www.ncbi.nlm.nih.gov/pubmed/30476234 PMID30476234).
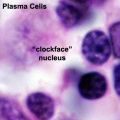
- "clockface" - a term used to describe the appearance of plasma cell nuclei due to the clumping of the chromatin at the nucleus periphery. More clearly seen in tissue plasma cells that the bone marrow smear, where they are sometimes confused with the basophilic erythroblasts. Image - plasma cell
- CD - (cluster of differentiation) identifies immunological surface markers on cells. Positive (+) generally means that the substance is expressed/identified, while negative (-) means that it is missing/not identified.
- CD4+ - (T helper cells) refers to T lymphocytes that express CD4 (cluster of differentiation 4, a glycoprotein of the immunoglobulin superfamily) on their surface, associated with helper/inducer function. These cells can be infected by human immunodeficiency virus (HIV).
- CD4/CD8 ratio - clinical measurement of different immune cell types (ratios between 1.5 to 2.5 are considered normal). Viral infections such as HIV, cytomegalovirus, Epstein-Barr virus, and influenza virus, associated with an inversion of the ratio.
- CD8+ - (cytotoxic T cells) refers to T lymphocytes that express CD8 (glycoprotein of the immunoglobulin superfamily) on their surface, associated with cytotoxic/suppressor activity.
- "clockface" - a term used to describe the appearance of plasma cell nuclei due to the clumping of the chromatin at the nucleus periphery. More clearly seen in tissue plasma cells that the bone marrow smear, where they are sometimes confused with the basophilic erythroblasts.
- cords of Billroth - spleen cellular columns located in red pulp. surrounded by splenic sinusoids. Cords contain reticular cells, macrophages, lymphocytes, plasma cells and erythrocytes.
- cortex - outer layer, used in association with medulla (innner layer or core) a general description that can be applied to describing an organ with a layered structure.
- cortical Thymic Epithelial Cell - (cTEC, types I - IV) support and antigen presenting cells located in the cortex regions of the thymus required for positive and negative selection of maturing T cells. See also medullary epithelial cell.
- crypt - (tonsil crypt) tonsil squamous epithelium infold, with intraepithelial passages containing non-epithelial cells. Functions include: intimate contact between immune response effector cells, facilitate transport of antigens, synthesise secretory components, and contain a pool of immunoglobulins. PMID 7559106
- dendritic cell - (DC, antigen-presenting cell, APC) cells that present antigens and induce a primary immune response in resting naïve T lymphocytes. Originate from the same common progenitor as monocytes (PMID 20193011). In 2011 Ralph M. Steinman received half the Nobel Prize half of the award to to Ralph M. Steinman for his discovery of the dendritic cell and its role in adaptive immunity.
- Effector cells - the immune functioning (active) B and T lymphocytes.
- Efferent lymph - vessel carrying lymph away from a node.
- fibroblastic reticular cell - (FRC) specialized myofibroblasts that form the structural mesenchymal network "sponge" within lymphoid tissue that regulate immune cell migration, activation, and survival. Immune T cells, B cells, dendritic cells (DCs), plasma cells and macrophages move and interact.
- follicular dendritic cell - (FDC) in B cell follicles of secondary lymphoid organs, cells interspersed within the stromal cell network function: Primary - help B cells to cluster. Secondary - in GC long-term retention of intact antigen and support B cell survival.
- GALT - Gut Associated Lymphatic Tissue consisting of Peyer’s patches, isolated lymphoid follicles and mesenteric lymph nodes.
- germinal centre - (GC) centre of B cell follicles of secondary lymphoid organs, where antigen-activated B-cell clones expand and undergo immunoglobulin gene hypermutation and selection.
- haemopoiesis (hemopoiesis) formation of blood cells.
- Hassall's corpuscles - (Hassall's body, thymic corpuscle) Epithelial reticular cells located in the thymic medulla. Named after Arthur Hill Hassall (1817-1894) a British physician and chemist.
- high endothelial venule - (HEV) the specialised post-capillary venous region that enables blood lymphocytes and pre-dendritic cells to enter a lymph node. The endothelial cells express ligands that bind lymphocytes, aiding their adhesion and subsequent transmigration into the lymph node. With inflammation, monocytes and NK cells can also enter here.
- humoral immune response - production of antibody by plasma cells derived from B lymphocytes (B cells).
- IEL - Intraepithelial Lymphocyte are T lymphocytes located in the gastrointestinal tract epithelium. Natural IELs (previously ‘type b’ IELs) acquire activated phenotype during development in the thymus in the presence of self antigens. Induced IELs (previously ‘type a’ IELs) progeny of conventional T cells activated post-thymically in response to peripheral antigens.
- IgA - the main class of antibody released at mucosal surfaces and in secretions (saliva, tears, milk, and respiratory and intestinal secretions) and the most abundantly produced antibody (70%). PMID 22566964
- IgD - the immunoglobulin B cell starts to produce as a cell-surface molecule after leaving the bone marrow.
- IgE - bind Fc receptors (surface of mast cells in tissues and basophils in the blood) release of potent pro inflammatory molecules mediators of allergic reactions.
- IgG - the major class of immunoglobulin in the blood.
- IgM - the first class of antibody made by a developing B cell, which may switch to making other classes of antibody.
- immunodeficiency - when one or more components of the immune system is defective. (More? Immunobiology - immunodeficiency)
- immunoglobulin - (antibody, Ab) protein produced by plasma cells.
- immunosenescence - in ageing and disease, refers to a weaker immune responses producing a progressive deterioration and increased susceptibility to infectious diseases, neoplasia, and autoimmune diseases.
- innate lymphoid cells - (ILCs) subset of lymphocytes that lack antigen-specific receptors, are located in peripheral tissues and abundant at barrier surfaces, decrease in number with age. PMID 29924974
- intraepithelial lymphocyte (IEL) immune cells residing in the gastrointestinal tract epithelium. image - Intraepithelial lymphocyte differentiation
- involution - in the thymus refers to the replacement, mainly in the cortex, of cells by adipose tissue. (More? PubMed- thymus involution) | Cancer Medicine - Thymomas and Thymic Tumors)
- Kupffer cells - stellate macrophage cells located in the liver sinusoids, named after Karl Wilhelm von Kupffer (1829 - 1902) a German anatomist who originally identified these cells. (More? Liver Development)
- lacteal - term used to describe the lymphatic vessels of the small intestine.
- lamina propria - a layer of loose connective tissue found underneath an epithelium, together with the epithelium described as mucosa.
- Langerhans cell - (LC, dendritic cell) Antigen-presenting immune cell found mainly in the basal/suprabasal layers of adult skin and mucosa. Cells lie in the basal/suprabasal layers of stratified epidermal and mucosal tissues. First in the innate antiviral immune defines and can migrate to lymph nodes and induce a T cell–mediated adaptive immune response. (More? Integumentary | Immune System Development)
- Leukocyte - (Greek, lukos = clear, white) white blood cell.
- lingual - related to the tongue, as in lingual tonsil, forms part of Waldeyer’s ring.
- lymph node - connective tissue encapsulated lymphoid organ (1mm - 2cm in size), positioned in the pathway of lymph vessels. (More? Lymph Node Development)
- lymphangion - the functional unit of a lymph vessel that lies between two semilunar (half moon-shaped) valves.
- lymphangiogenesis - formation of new lymph vessels from pre-existing lymphatic structures. During embryogenesis and in adult tissues as reaction to inflammation or injury.
- M cell - (microfold cell) found in the follicle-associated epithelium of the Peyer's patch. Function to transport gut lumen organisms and particles to immune cells across the epithelial barrier.
- macrophage - a large highly motile white blood cell which engulfs foreign material (bacteria etc) and both degenerating cells and cell fragments. Differentiates from a monocyte and found in many different tissues and locations. Current theory suggests tissue macrophage is also derived from resident stem cell population in many tissues. More? Immunobiology - Defects in phagocytic cells are associated with persistence of bacterial infection)
- MALT - Mucosa Associated Lymphoid Tissue.
- medulla - inner layer or core, used in association with cortex (outer layer) a general description that can be applied to describing an organ with a layered structure.
- medullary Thymic Epithelial Cell - (mTEC, types I-VII) support and antigen presenting cells located in the medullary regions of the thymus, required for central tolerance (negative selection) of maturing T cells (PMID 11375064). See also cortical thymic epithelial cell.
- Memory Cell - effector T cell (lymphocyte)
- mesenteric lymph nodes - Part of GALT as well as being involved in gut-draining. image - mesenteric lymph nodes
- Mononuclear Phagocytic System - (MPS, Lymphoreticular System, Reticuloendothelial System, RES) Consists of circulating monocytes in the peripheral blood and non-circulating (fixed) tissue macrophages (MΦ) located in tissues and organs.
- NAVL - (naval) mnemonic to remember the neurovascular bundle components Nerve Artery Vein Lymph found travelling together within organs and tissues.
- negative selection - T cells bearing autoreactive T cell antigen receptors (TCRs) are eliminated during their development in the thymus, protects against autoimmunity.
- normoblast - seen in bone marrow smear, a developing erythroblast (red blood cell) that still retains a nucleus.
- nude mice - (nu/nu) mice which are congenitally hairless and athymic, therefore they do not reject tissue and tumor grafts.
- PALS - acronym for PeriArterial Lymphoid Sheath in the spleen white pulp.
- parenchyma - (Greek = enkeim "to pour in") cells forming the functional cells of an organ or tissue. These cells carry out the function of the organ at a cellular level, and are not the structural cells, connective tissue, extracellular matrix (stromal).
- periarterial lymphoid sheath - (PALS) in the spleen the white pulp that surrounds the central arteries. (T-lymphocytes,macrophages and plasma cells)
- pharyngeal pouch III - origin of endodermal component of the thymus (also formed from neural crest). Pharyngeal arches
- Plasma Cell - active B cell (lymphocyte) which is secreting antibody. Located in either bone marrow or peripheral lymphoid tissues, these cells have and increased cytoplasmic volume (due to increase rough endoplasmic reticulum) in comparison to the inactive (non-secreting) lymphocyte.
- primary follicle - follicle that does not contain germinal centre, secondary follicles do germinal centre.
- red pulp - spleen region, organized as cell cords (splenic cords, cords of Billroth) and vascular sinuses.
- regulatory T cells - (Tregs) maintain self tolerance and suppress pathological immune responses by control of immune response to non-self antigens.
- reticular fibres - reticular cells secrete this extracellular matrix protein, composed of type III collagen.
- right lymphatic duct - drains most of the right upper quadrant. See also thoracic duct.
- secondary follicle - contain germinal centre, primary follicle does not contain germinal centre.
- sentinel lymph node - the hypothetical first lymph node or group of nodes reached by metastasizing cancer cells from a primary tumour.
- sinus - a larger vessel or space usually curved that may contain air, blood, or lymph. e.g. splenic medullary sinus, lymph node medullary sinus, sub-capsular sinus, trabecular sinus.
- sinusoid - a tiny vessel with a tortuous path and many connections to similar vessels. e.g. hepatic and bone marrow sinusoids.
- splenic capillary sheaths - in spleen around capillary endothelium and consist of three main cell types: CD271+ stromal capillary sheath cells, CD68+CD163− macrophages and recirculating B-lymphocytes. Sheaths may; 1. allow interaction among sheath macrophages and B-lymphocytes, 2. attract recirculating B-lymphocytes from the open circulation of the red pulp to start migration into white pulp follicles. 30356180
- splenic sinusoids - enlarged splenic spaces located in red pulp and surrounding cords of Billroth.
- sphingosine-1-phosphate - (S1P) sphingolipid secreted into the extracellular space establishing a gradient acting through G protein-coupled receptors to attract lymphocytes out of lymphoid organs (lymph node, thymus, spleen) into the circulation.
- stroma - (Greek = "a cover, table-cloth, bedding") tissue forming the framework/support of an organ or tissue. That is the structural cells which form connective tissue and secrete extracellular matrix, rather than the functional cells (parenchymal). All organs can therefore be functionally divided into these 2 components, stromal/parenchymal.
- Subcapsular sinus (=marginal sinus) space lying under the connective tissue capsule which receives lymph from afferent lymphatic vessels.
- T cell - (T-cell, T lymphocyte) named after thymus, where they develop, the active cell is responsible for cell-mediated immunity (killer T cells and helper T cells). Cells express T-cell receptor on surface and directly kill virally or bacterially infected cells. These cells can themselves be infected by HIV. (More? Electron micrographs of nonactivate and activated lymphocytes)
- TEC - (Thymic Epithelial Cell) thymus support and antigen presenting cells further divided anatomically and functionally into medullary TEC (mTEC, types I-VII, for central tolerance) and cortical epithelial cell (cTEC, types I-IV, positive and negative selection) populations (see PMID 28800929 PMID 30308217).
- T cell activation - (T lymphocyte activation)The activation process begins with T-cells searching for and encountering antigen-bearing dendritic cells within lymph nodes.
- thoracic duct - (TD) largest and main lymphatic vessel, drains the lower body including the extremities and abdomen. Intra-thoracic tributaries include: intercostal, mediastinal, and bronchomediastinal trunks.
- Thymic corpuscle - (Hassall's corpuscle) a mass of concentric epithelioreticular cells found in the thymus. The number present and size tend to increase with thymus age. (see classical description of Hammar, J. A. 1903 Zur Histogenese und Involution der Thymusdriise. Anat. Anz., 27: 1909 Fiinfzig Jahre Thymusforschung. Ergebn. Anat. Entwickl-gesch. 19: 1-274.)
- thymic epitheliocytes - reticular cells located in the thymus cortex that ensheathe the cortical capillaries, creating and maintain the microenvironment necessary for the development of T-lymphocytes in the cortex.
- T helper cells - (helper T-cells) (Th cells, CD4+) refers to T lymphocytes that when mature express CD4 (glycoprotein of the immunoglobulin superfamily) on their surface.
- T lymphocyte - (T cell, T-cell) regulate cell-mediated immunity.
- thymus - an immune/endocrine (thymic hormone, thymosins) organ involved in the maturation (differentiation) of T lymphocytes (T-cells).
- tonsils - lymph nodules embedded in the mucus membranes located at the back of the mouth and top of the throat. The overlying epithelium helps identify the location.
- tonsillitis - a common bacterial infection of the palatine tonsils, occurring mostly in children and young adults and can also become recurrent tonsillitis.
- vermiform appendix - see appendix, anatomical region containing gut-associated lymphoid tissue located within the gastrointestinal tract at the beginning of the colon. The anatomy is as a finger-like structure that arises from the cecum. The length (2.5-13 cm) is longer in both infants and children and also has more abundant lymphatic tissue in early life. The wall structure is similar to the small intestine (though with no villi), nor plicae circularis. Lymph nodules surround the lumen of the gastrointestinal tract and extend from the mucosa into the submucosa.
- VDJ recombination - (variable, diversity and joining gene segments) genetic recombination event that occurs in immune cell maturation in primary lymphoid organs, B cells ((bone marrow) and T cells (thymus).
- Waldeyer’s ring - ring of lymphoid tissue in the pharyngeal wall: palatine tonsils, nasopharyngeal tonsil (adenoid) and lingual tonsil. First described in 1884 by von Waldeyer-Hartz.
- white pulp - (Malpighian follicles, Malpighian bodies of the spleen, white nodules, splenic lymphoid nodules) spleen lymphoid region, organized as lymphoid sheaths with both T-cell and B-cell compartments, around the branching arterial vessels (resembles lymph node structure).
| Other Terms Lists |
|---|
| Terms Lists: ART | Birth | Bone | Cardiovascular | Cell Division | Endocrine | Gastrointestinal | Genital | Genetic | Head | Hearing | Heart | Immune | Integumentary | Neonatal | Neural | Oocyte | Palate | Placenta | Radiation | Renal | Respiratory | Spermatozoa | Statistics | Tooth | Ultrasound | Vision | Historic | Drugs | Glossary |
References
- ↑ Appay V, Sauce D & Prelog M. (2010). The role of the thymus in immunosenescence: lessons from the study of thymectomized individuals. Aging (Albany NY) , 2, 78-81. PMID: 20354268 DOI.
- ↑ Macpherson AJ & Smith K. (2006). Mesenteric lymph nodes at the center of immune anatomy. J. Exp. Med. , 203, 497-500. PMID: 16533891 DOI.
Additional Information
| Additional Information - Content shown under this heading is not part of the material covered in this class. It is provided for those students who would like to know about some concepts or current research in topics related to the current class page. |
MALT
Spencer J, Siu JHY & Montorsi L. (2019). Human intestinal lymphoid tissue in time and space. Mucosal Immunol , 12, 296-298. PMID: 30542110 DOI.
| Jejunum and Ileum | Colon | Mucosa |
|---|---|---|
|
|
|
| Data source: Senda T, Dogra P, Granot T, Furuhashi K, Snyder ME, Carpenter DJ, Szabo PA, Thapa P, Miron M & Farber DL. (2019). Microanatomical dissection of human intestinal T-cell immunity reveals site-specific changes in gut-associated lymphoid tissues over life. Mucosal Immunol , 12, 378-389. PMID: 30523311 DOI. |
Lymph Node
Petrovas C & Velu V. (2018). Editorial: Lymph Node T Cell Dynamics and Novel Strategies for HIV Cure. Front Immunol , 9, 2950. PMID: 30619310 DOI.
Dimopoulos Y, Moysi E & Petrovas C. (2017). The Lymph Node in HIV Pathogenesis. Curr HIV/AIDS Rep , 14, 133-140. PMID: 28685417 DOI.
Kuka M & Iannacone M. (2014). The role of lymph node sinus macrophages in host defense. Ann. N. Y. Acad. Sci. , 1319, 38-46. PMID: 24592818 DOI.
Thymus
Kondo K, Ohigashi I & Takahama Y. (2018). Thymus machinery for T-cell selection. Int. Immunol. , , . PMID: 30476234 DOI.
Kumar BV, Connors TJ & Farber DL. (2018). Human T Cell Development, Localization, and Function throughout Life. Immunity , 48, 202-213. PMID: 29466753 DOI.
Takaba H & Takayanagi H. (2017). The Mechanisms of T Cell Selection in the Thymus. Trends Immunol. , 38, 805-816. PMID: 28830733 DOI.
Spleen
Mouse and rat spleen structure is different. Mouse models have though shown that as the splenic white pulp ages it looses its structural organization, perhaps contributing to the impaired immune system function seen with age.[1]
| Feature | ||
|---|---|---|
| Carnegie stage 14 to 17
appears as a bulge in the dorsal mesogastrium. Mesothelium pseudostratified. | ||
| Mesothelium (pseudostratified} replaced with high columnar cells and then low columnar cells. | ||
| Basement membrane present after this stage. | ||
| Hematopoietic cells detected. | ||
| Spleen is now apparent. Mesenchymal cells differentiated from cells in dorsal mesogastrium. Sinus and hilus formation after this stage. | ||
| Arteries and veins parallel entries at this stage. | ||
| Feature | ||
| reticulum cells (alpha-smooth muscle actin-positive) scattered around the arterioles | ||
| reticulum cells increase in number and began to form a reticular framework. Accumulation of T and B lymphocytes within this framework, and a primitive white pulp was observed around the arterioles. | ||
| reticular framework antigenic diversity, and T and B lymphocytes were segregated in the framework. T lymphocytes were sorted into the alpha-SMA-positive reticular framework, and the periarteriolar lymphoid sheath (PALS) was formed around the arteriole. B lymphocytes aggregated in eccentric portions to the PALS and formed the lymph follicle (LF, reticular framework alpha-SMA-negative). | ||
| marginal zone appears in reticular framework around the white pulp. | ||
| Human embryonic data[2] and fetal data [3] Links: spleen | Kyoto Collection | human timeline | ||
Steiniger B, Bette M & Schwarzbach H. (2011). The open microcirculation in human spleens: a three-dimensional approach. J. Histochem. Cytochem. , 59, 639-48. PMID: 21525186 DOI.
Tan JKH & Watanabe T. (2018). Determinants of postnatal spleen tissue regeneration and organogenesis. NPJ Regen Med , 3, 1. PMID: 29367882 DOI.
Cesta MF. (2006). Normal structure, function, and histology of the spleen. Toxicol Pathol , 34, 455-65. PMID: 17067939 DOI.
Mebius RE & Kraal G. (2005). Structure and function of the spleen. Nat. Rev. Immunol. , 5, 606-16. PMID: 16056254 DOI.
Blood
Prame Kumar K, Nicholls AJ & Wong CHY. (2018). Partners in crime: neutrophils and monocytes/macrophages in inflammation and disease. Cell Tissue Res. , 371, 551-565. PMID: 29387942 DOI.
Glossary Links
- Glossary: A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | Numbers | Symbols | Term Link
Cite this page: Hill, M.A. (2024, April 27) Embryology SH Practical - Lymphatic Structure and Organs. Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/SH_Practical_-_Lymphatic_Structure_and_Organs
- © Dr Mark Hill 2024, UNSW Embryology ISBN: 978 0 7334 2609 4 - UNSW CRICOS Provider Code No. 00098G
- ↑ Masters AR, Jellison ER, Puddington L, Khanna KM & Haynes L. (2018). Attrition of T Cell Zone Fibroblastic Reticular Cell Number and Function in Aged Spleens. Immunohorizons , 2, 155-163. PMID: 30706058 DOI.
- ↑ Endo A, Ueno S, Yamada S, Uwabe C & Takakuwa T. (2015). Morphogenesis of the spleen during the human embryonic period. Anat Rec (Hoboken) , 298, 820-6. PMID: 25403423 DOI.
- ↑ Satoh T, Sakurai E, Tada H & Masuda T. (2009). Ontogeny of reticular framework of white pulp and marginal zone in human spleen: immunohistochemical studies of fetal spleens from the 17th to 40th week of gestation. Cell Tissue Res. , 336, 287-97. PMID: 19255788 DOI.