Ultrasound
| Embryology - 27 Apr 2024 |
|---|
| Google Translate - select your language from the list shown below (this will open a new external page) |
|
العربية | català | 中文 | 中國傳統的 | français | Deutsche | עִברִית | हिंदी | bahasa Indonesia | italiano | 日本語 | 한국어 | မြန်မာ | Pilipino | Polskie | português | ਪੰਜਾਬੀ ਦੇ | Română | русский | Español | Swahili | Svensk | ไทย | Türkçe | اردو | ייִדיש | Tiếng Việt These external translations are automated and may not be accurate. (More? About Translations) |
Introduction
The generic term ultrasound refers to the non-invasive technique using sound waves in the ultrasonic (above our hearing range) frequency. The technique can visualise and allow prenatal diagnosis of several features of development of: follicles in the ovary, the gestational sac, fetus in the uterus, fetal parameters, and the placenta. Ultrasound imaging began in the 1950's but it was only with the application of computer analysis beginning in the 1980's that more detailed images could be generated. This current page links to all human and animal ultrasound movies, you can also use the Category:Ultrasound to find related content.
Parents now commonly see ultrasound movies or images in the first trimester and clinically this is a non-invasive prenatal diagnostic tool for detection of abnormalities as well as a method of staging (ageing) and checking growth. There are several different standards available[1] for calculating age based upon several measurements, including embryo or fetal crown rump length (CRL).[2]
Ultrasound can also be used in combination with other techniques to locate both embryo and placenta for other prenatal tests (More? prenatal diagnosis). Development of modern ultrasound techniques now allow the measurement of blood flow (doppler) as well as computer three-dimensional reconstruction of embryos or structures.
The ultrasound technique can be used at any stage during pregnancy for fetal and placenta monitoring (More? placenta | Placenta Abnormalities | Prenatal Diagnosis).
Some diagnostic measurements include:
- Trisomies - Nuchal translucency (NT), nasal bone visualization (NB)
- Cardiovascular - tricuspid valve regurgitation (TR), "a"-wave pattern, DV PIV, S-wave (peak systolic velocity), D-wave (peak diastolic velocity), a-wave (atrial contraction in late diastole), time-averaged maximum velocity (TAMXV)
| How to Play Ultrasound Movies | |
|---|---|
| <html5media height="300" width="400">File:Ultrasound_Fetus_02.mp4</html5media> | 
The ultrasound movies can be viewed in two ways:
Abnormal developmental ultrasound and features are listed on a separate page (More? abnormal ultrasound) all content is for educational use only. |
| Page | Play Movie shows a 12 week fetus in 3d in realtime (hence 4D). |
Special thanks to Dr Andrew McLennan, Foetal Medicine Unit, Royal North Shore Hospital and Dr Stanley Ng for many of the original video materials. |
Some Recent Findings
|
| More recent papers |
|---|
|
This table allows an automated computer search of the external PubMed database using the listed "Search term" text link.
More? References | Discussion Page | Journal Searches | 2019 References | 2020 References Search term: Fetal Ultrasound | First Trimester Ultrasound | Second Trimester Ultrasound | Fetal Doppler Ultrasound | |
| Older papers |
|---|
| These papers originally appeared in the Some Recent Findings table, but as that list grew in length have now been shuffled down to this collapsible table.
See also the Discussion Page for other references listed by year and References on this current page.
|
Ultrasound Movies
This table of images links to both normal and abnormal ultrasound movies. Page link will open a new window with the movie and additional information.
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Ultrasound Gestational Age
The following table is based upon Australian data from ultrasound measurements of Crown Rump Length (CRL).[1]
Note that Gestational Age GA differs from fertilisation age by about 2 weeks.
| Gestational Age and Crown-Rump Length (measured by ultrasound) | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Fertilization and Gestational Age - Crown-Rump Length (ultrasound) | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
First Trimester Ultrasound
First trimester screening refers to the ltrasound scan typically carried out between GA 11+ 0 – 13+ 6 weeks. The scan can determine the gestation age GA, embryo anatomical size measurements, placenta position and structure.[13][14]
The scan can also detect, with varying degrees of accuracy, some developmental abnormalities.
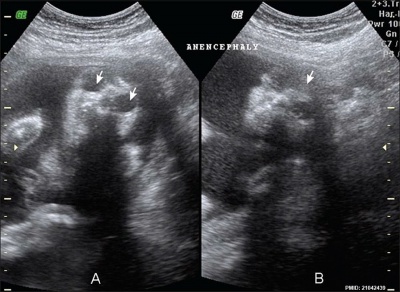
Detectable
- anencephaly/exencephaly
- holoprosencephaly
- omphalocele gastroschisis
- body stalk anomaly
- megacystis
Potentially Detectable
- hand and foot abnormalities
- diaphragmatic hernia
- lethal skeletal dysplasia
- severe heart defects
- spina bifida aperta
- facial clefts
Not Detectable
- microcephaly
- anomaly of the corpus callosum
- ventriculomegaly
- tumors
- ovarian cysts
- pulmonary lesions
- gastrointestinal obstructions
Second Trimester Ultrasound
Second trimester ultrasound provides information about: number of fetuses, gestational age, location of the placenta, fetal growth and maternal anatomy.[15]
Doppler Ultrasound
Doppler ultrasound is a noninvasive measure of blood flow and blood pressure by bouncing ultrasound off circulating red blood cells. Originally used for fetal heart beat detection, more recently used diagnostically in uterine, placental, ductus venosus and other fetal blood vessels.
Doppler effect is due to the movement of blood cells causing a change in pitch of the reflected sound waves.
| Velamentous Cord Insertion | Vasa Previa | |||
|---|---|---|---|---|
| <html5media>File:Velamentous cord insertion 02.mp4</html5media>
This colour doppler ultrasound movie shows blood flow in the umbilical cord inserted into the post uterine wall and then courses superiorly to enter the fundal edge of the anterior placenta. |
|
Dr Stanley Ng - Obstetrical and gynecological sonologist (Sydney) for providing fetal ultrasound images and movie clips.
4D Ultrasound
Fetal Face
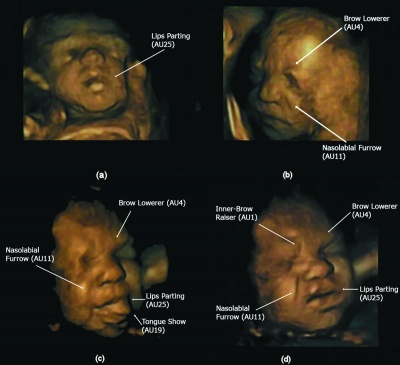
|
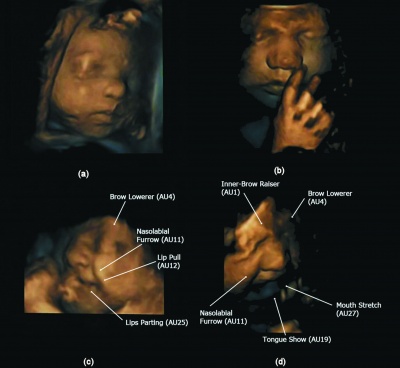
|
| (a) 24 weeks (b) 27.5 weeks (c - d) 32 weeks. [16] | (a) 28 weeks neutral face (b) 33 weeks (c) 32.5 weeks (d) 33 weeks.[16] |
3D Ultrasound
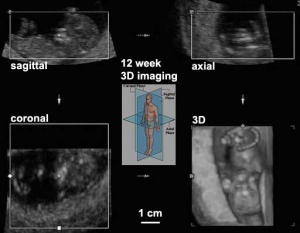
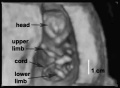
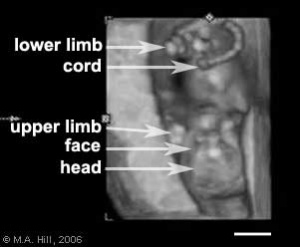
Three dimensional (3D) ultrasound scan images are generated from a series of images in 3 different planes. The image shows a 12 week fetal ultrasound images in the sagittal, axial and coronal planes that are used by the computer to generate the final 3D image in the lower right. Computers are able to generate these images in realtime, therefore in addition to static pictures, realtime 4D movies can be generated.
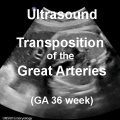
Cardiovascular
| Cardiac | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
| |||||||||
The heart is the first organ in the embryo that can be easily ultrasound visualised by its contractility. The absence of contractility also being a early diagnosis of embryo/fetal demise or trophoblastic disease.
The use of ultrasound at later stages of heart development in the mid-1980's began to be used as a diagnostic tool for congenital cardiac abnormalities.[17]
| Fetal ductus venosus ultrasound[18] | |
|---|---|

|
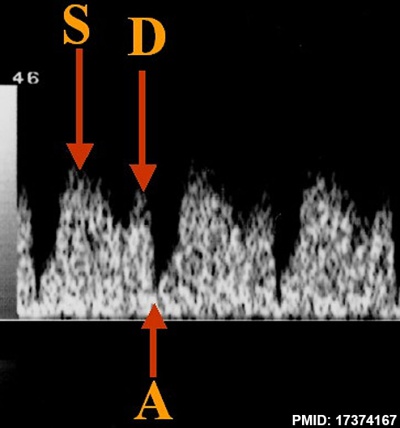
|
Soft Markers

The term "soft markers" refers to ultrasound measurements which may not be diagnostic by themselves, but can have an indicative role for further diagnostic analysis of the pregnancy.
The Diagnostic Imaging Committee of the Society of Obstetricians and Gynaecologists of Canada in 2005[20] made the following recommendations:
- The screening ultrasound at 16 to 20 weeks should evaluate 8 markers, 5 of which (thickened nuchal fold, echogenic bowel, mild ventriculomegaly, echogenic focus in the heart, and choroid plexus cyst) are associated with an increased risk of fetal aneuploidy, and in some cases with nonchromosomal problems, while 3 (single umbilical artery, enlarged cisterna magna, and pyelectasis) are only associated with an increased risk of nonchromosomal abnormalities when seen in isolation (II-2 B).
- Identification of soft markers for fetal aneuploidy requires correlation with other risk factors, including history, maternal age, and maternal serum testing results (II-1 A).
- Soft markers identify a significant increase in fetal risk for genetic disease. Timely referral for confirmation, counselling, and investigation is required to maximize management options (III-B).
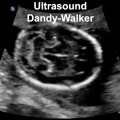
Neural
| Neural | |||||||
|---|---|---|---|---|---|---|---|
|
| ||||||
Anencephaly ultrasound[21]
Ultrasound Placenta
Ultrasound can be used to measure both normal and abnormal placentation. Morbidly adherent placenta (MAP) is the general clinical term used to describe the different forms of abnormal placental implantation (Accreta, Increta and Percreta). Clinical ultrasound indicators of MAP are the presence of an interruption of the bladder line, absence of a retroplacental clear zone, and the presence of placental lacunae.
| Placenta | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
| |||||||||
Placenta Previa
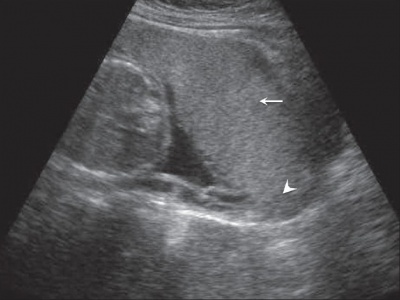
|

|
| Anterior placenta position (upper arrow) in relation to cervix os (lower arrow). | Posterior placenta position (arrow) in relation to cervix os (triangle). |
- Links: Placenta Abnormalities
Placental Cord
| Velamentous Cord |
| Page | Play |
A number of clinical and diagnostic measurements can be made from ultrasound scans of the placental cord, including its insertion site with the placenta. Key measures are blood vessel number, measured by cross-sectional scan, and blood flow, measured by colour doppler.
- Cord
- length (cm)
- cross-sectional area (mm2)
- coiling index
- Wharton’s jelly area (mm2)
- Artery
- cross-sectional area (mm2)
- pulsatility index
- Vein
- cross-sectional area (mm2)
- absolute blood flow (ml/min)
- blood flow for fetal weight (ml/kg/min)
- blood flow mean velocity (cm/second)
Genital
Sex Determination
The earliest accurate ultrasound marker for fetal sex by ultrasound is at end of first trimester scan (12-13 weeks GA). Based upon direction of the genital tubercle when scanned in the sagittal plane ("sagittal sign").[22]
- female - downward direction of the genital tubercle
- male - upward direction of the genital tubercle
Other sonographic landmarks can include:
- female - labial lines, uterus
- male - midline penis raphe, descended testis, micturition jet
Earlier embryonic sex determination can now be made by non-invasive genetic analysis techniques.
Twinning
| Placental Membranes | |
|---|---|

|

|
| Dichorionic diamniotic
GA 13 week = 11 week |
Monochorionic diamniotic
GA 12 week = 10 week |
| Thick dividing membrane and "lambda" or twin peak sign at the junction with the placenta. | Thin dividing membrane and "T" sign at the junction with the placenta. |
| Links: Placenta Membranes |

Dichorionic twins ultrasound[23] |
Transvaginal ultrasonography of dichorionic-diamniotic twins at 8 weeks and 5 days since co-incubation as part of IVF. The twin at left in the image is shown in the sagittal plane with the head pointing towards upper left. The twin at right in the image is shown in the coronal plane with the head pointing rightwards. |
Ultrasound Research
Ultrasound imaging began in the 1950's but it was only with the application of computer analysis beginning in the 1980's that more detailed images could be generated. The increasing quality of ultrasonic equipment and computing allows today realtime 3D scans and calculations of fetal measurements as well as doppler measurement of heart rates.
In medical research there have been recent developments that allow spatial high resolution down to 30 microns in real-time.
Other Imaging Techniques
There are a range of other imaging techniques to study development and used in developmental research.
Other developmental research imaging techniques include:
- Magnetic Resonance Imaging
- Computed Tomography
- high frequency ultrasound or High Intensity Focused Ultrasound (HIFU)
- positron emission tomography (PET)
- single photon emission computed tomography
- optical bioluminescence
- fluorescence
Additional Images
References
- ↑ 1.0 1.1 1.2 Westerway SC, Davison A & Cowell S. (2000). Ultrasonic fetal measurements: new Australian standards for the new millennium. Aust N Z J Obstet Gynaecol , 40, 297-302. PMID: 11065037
- ↑ Chalouhi GE, Bernard JP, Benoist G, Nasr B, Ville Y & Salomon LJ. (2011). A comparison of first trimester measurements for prediction of delivery date. J. Matern. Fetal. Neonatal. Med. , 24, 51-7. PMID: 20350241 DOI.
- ↑ Fatihoglu E & Aydin S. (2020). Diagnosing Small for Gestational Age during second trimester routine screening: Early sonographic clues. Taiwan J Obstet Gynecol , 59, 287-292. PMID: 32127152 DOI.
- ↑ Casati D, Pellegrino M, Cortinovis I, Spada E, Lanna M, Faiola S, Cetin I & Rustico MA. (2019). Longitudinal Doppler references for monochorionic twins and comparison with singletons. PLoS ONE , 14, e0226090. PMID: 31809530 DOI.
- ↑ Becker DA, Tang Y, Jacobs AP, Biggio JR, Edwards RK & Subramaniam A. (2019). Sensitivity of prenatal ultrasound for detection of trisomy 18. J. Matern. Fetal. Neonatal. Med. , 32, 3716-3722. PMID: 29712489 DOI.
- ↑ Ferreira C, Rouxinol-Dias AL, Loureiro T & Nicolaides K. (2019). Subarachnoid space diameter in chromosomally abnormal fetuses at 11-13 weeks' gestation. J. Matern. Fetal. Neonatal. Med. , 32, 2079-2083. PMID: 29338474 DOI.
- ↑ Vayna AM, Veduta A, Duta S, Panaitescu AM, Stoica S, Buinoiu N, Nedelea F & Peltecu G. (2018). Diagnosis of Fetal Structural Anomalies at 11 to 14 Weeks. J Ultrasound Med , , . PMID: 29476550 DOI.
- ↑ Näslund Thagaard I, Krebs L, Lausten-Thomsen U, Olesen Larsen S, Holm JC, Christiansen M & Larsen T. (2016). Dating of Pregnancy in First versus Second Trimester in Relation to Post-Term Birth Rate: A Cohort Study. PLoS ONE , 11, e0147109. PMID: 26760299 DOI.
- ↑ Afrakhteh M, Moeini A, Taheri MS, Haghighatkhah HR, Fakhri M & Masoom N. (2014). Uterine Doppler velocimetry of the uterine arteries in the second and third trimesters for the prediction of gestational outcome. Rev Bras Ginecol Obstet , 36, 35-9. PMID: 24554228 DOI.
- ↑ Ebrashy A, El Kateb A, Momtaz M, El Sheikhah A, Aboulghar MM, Ibrahim M & Saad M. (2010). 13-14-week fetal anatomy scan: a 5-year prospective study. Ultrasound Obstet Gynecol , 35, 292-6. PMID: 20205205 DOI.
- ↑ Picone O, Simon I, Benachi A, Brunelle F & Sonigo P. (2008). Comparison between ultrasound and magnetic resonance imaging in assessment of fetal cytomegalovirus infection. Prenat. Diagn. , 28, 753-8. PMID: 18551722 DOI.
- ↑ Araujo Júnior E, Filho HA, Pires CR, Zanforlin Filho SM & Moron AF. (2006). Prenatal diagnosis of vasa previa through color Doppler and three-dimensional power Doppler ultrasonography. A case report. Clin Exp Obstet Gynecol , 33, 122-4. PMID: 16903253
- ↑ Edwards L & Hui L. (2018). First and second trimester screening for fetal structural anomalies. Semin Fetal Neonatal Med , 23, 102-111. PMID: 29233624 DOI.
- ↑ Mei JY, Afshar Y & Platt LD. (2019). First-Trimester Ultrasound. Obstet. Gynecol. Clin. North Am. , 46, 829-852. PMID: 31677757 DOI.
- ↑ Cargill Y & Morin L. (2017). No. 223-Content of a Complete Routine Second Trimester Obstetrical Ultrasound Examination and Report. J Obstet Gynaecol Can , 39, e144-e149. PMID: 28729106 DOI.
- ↑ 16.0 16.1 Reissland N, Francis B, Mason J, Lincoln K (2011) Do Facial Expressions Develop before Birth? PLoS ONE 6(8): e24081. doi:10.1371/journal.pone.0024081 PLoS One
- ↑ DeVore GR. (1985). The prenatal diagnosis of congenital heart disease--a practical approach for the fetal sonographer. J Clin Ultrasound , 13, 229-45. PMID: 3923046
- ↑ da Silva FC, de Sá RA, de Carvalho PR & Lopes LM. (2007). Doppler and birth weight Z score: predictors for adverse neonatal outcome in severe fetal compromise. Cardiovasc Ultrasound , 5, 15. PMID: 17374167 DOI.
- ↑ Alphonse J, Cox J, Clarke J, Schluter P & McLennan A. (2013). The Effect of Ethnicity on 2D and 3D Frontomaxillary Facial Angle Measurement in the First Trimester. Obstet Gynecol Int , 2013, 847293. PMID: 24288543 DOI.
- ↑ Van den Hof MC & Wilson RD. (2005). Fetal soft markers in obstetric ultrasound. J Obstet Gynaecol Can , 27, 592-636. PMID: 16100637
- ↑ Alorainy IA, Barlas NB & Al-Boukai AA. (2010). Pictorial Essay: Infants of diabetic mothers. Indian J Radiol Imaging , 20, 174-81. PMID: 21042439 DOI.
- ↑ Odeh M, Granin V, Kais M, Ophir E & Bornstein J. (2009). Sonographic fetal sex determination. Obstet Gynecol Surv , 64, 50-7. PMID: 19099612 DOI.
- ↑ Häggström, M. "Medical gallery of Mikael Häggström 2014". Wikiversity Journal of Medicine 1 (2). DOI:10.15347/wjm/2014.008. ISSN 20018762.
Journals
- Journal of Ultrasound in Medicine published by the American Institute of Ultrasound in Medicine.
Books
Molecular Imaging and Contrast Agent Database (MICAD) NBK5330 | PMID:20641179
Articles
Butt K & Lim K. (2014). Determination of gestational age by ultrasound. J Obstet Gynaecol Can , 36, 171-181. PMID: 24518917 DOI.
Lubusky M, Studnickova M, Skrivanek A, Vomackova K & Prochazka M. (2012). Ultrasound evaluation of fetal gender at 12-14 weeks. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub , 156, 324-9. PMID: 22660228 DOI.
Search PubMed
Search PubMed: Ultrasound prenatal diagnosis | Ultrasound
- ART - Assisted Reproductive Technology a general term to describe all the clinical techniques used to aid fertility.
- blastomere biopsy - An ART preimplantation genetic diagnosis technique carried out at cleavage stage (day 3), excluding poor quality embryos, detects chromosomal abnormalities of both maternal and paternal origin. May not detect cellular mosaicism in the embryo.
- blastocyst biopsy - An ART preimplantation genetic diagnosis technique carried out at blastocyst stage (day 4-5), removes several trophoblast (trophoderm) cells, detects chromosomal abnormalities of both maternal and paternal origin and may detect cellular mosaicism.
- cell-free fetal deoxyribonucleic acid - (cfDNA) refers to fetal DNA circulating and isolated from the plasma portion of maternal blood. Can be performed from GA 10 weeks as a first-tier test or as a second-tier test, with women with increased probability on combined first trimester screening offered cfDNA or diagnostic testing.
- false negative rate - The proportion of pregnancies that will test negative given that the congenital anomaly is present.
- false positive rate - The proportion of pregnancies that will test positive given that the congenital anomaly is absent.
- free β human chorionic gonadotrophin - beta-hCG subunit of hCG used as a diagnostic marker for: early detection of pregnancy, Trisomy 21, spontaneous abortion, ectopic pregnancy, hydatidiform mole or choriocarcinoma.
- multiples of the median - (MoM) A multiple of the median is a measure of how far an individual test result deviates from the median and is used to report the results of medical screening tests, particularly where the results of the individual tests are highly variable.
- negative predictive value - The probability that a congenital anomaly is absent given that the prenatal screening test is negative.
- Non-Invasive Prenatal Testing - (NIPT) could refer to ultrasound or other imaging techniques, but more frequently used to describe analysis of cell-free fetal DNA circulating in maternal blood.
- polar body biopsy - (PB biopsy) An ART preimplantation genetic diagnosis technique that removes either the first or second polar body from the zygote. As these are generated by oocyte meiosis they detects chromosomal abnormalities only on the female genetics.
- positive predictive value - The probability that a congenital anomaly is present given that the prenatal screening test is positive.
- pre-implantation genetic diagnosis - (PGD, pre-implantation genetic screening) a diagnostic procedure for embryos produced through Assisted Reproductive Technology (ART, in vitro fertilisation, IVF) for genetic diseases that would generate developmental abnormalities or serious postnatal diseases.
- prenatal screening sensitivity - (detection rate) The probability of testing positive on a prenatal screening test if the congenital anomaly is present.
- prenatal screening specificity - The probability of testing negative on a prenatal screening test if the congenital anomaly is absent.
- quadruple test (maternal serum testing of a-fetoprotein Template:AFP, free B-hCG or total hCG, unconjugated estriol, and inhibin A) is a fetal chromosomal anomaly test usually carried out later in pregnancy (GA 14 to 20 weeks).
- single nucleotide polymorphisms - (SNPs) the variation in a single DNA nucleotide that occurs at a specific position in the genome.
- triple test - (maternal serum testing of a-fetoprotein Template:AFP, free B-hCG or total hCG, and unconjugated estriol) is a fetal chromosomal anomaly test usually carried out later in pregnancy (GA 14 to 20 weeks).
| Other Terms Lists |
|---|
| Terms Lists: ART | Birth | Bone | Cardiovascular | Cell Division | Endocrine | Gastrointestinal | Genital | Genetic | Head | Hearing | Heart | Immune | Integumentary | Neonatal | Neural | Oocyte | Palate | Placenta | Radiation | Renal | Respiratory | Spermatozoa | Statistics | Tooth | Ultrasound | Vision | Historic | Drugs | Glossary |
Terms
- Biparietal diameter - (BPD) used to determine fetal age and normal development (small/large/abnormal) parameters. Measured as the diameter between the 2 sides of the head, measurements after 13 weeks (2.4 cm) to term (9.5 cm).
- cerebroplacental ratio - (CPR) a doppler ultrasound measurement calculated as the simple ratio between the middle cerebral artery pulsatility index (MCA‐PI) and the {{placenta]]l artery pulsatility index (UA‐PI). Fetuses with an abnormal ratio are thought to be a predictor of adverse pregnancy outcome such as: small for gestational age, abnormal fetal heart rate pattern, meconium stained liquor, low Apgar score, and acidosis at birth. PMID 28216258
- Crown-Rump Length - (CRL) measurement used in embryology to more accurately stage the early embryo and fetus. Measured from the curvature at the top (crown) to the curvature at the bottom (rump) of the "C-shaped" early embryo. Used in clinical ultrasound as a measurement between the periods of 7 to 13 weeks as an accurate estimation of the gestational age GA.
- DICOM - (ISO standard 12052:2006) Acronym for Digital Imaging and Communications in Medicine, a clinical standard for handling, storing, printing, and transmitting imaging information.
- Femur length - (FL) is used to determine fetal age and normal development (small/large/abnormal) parameters. The femur is the longest bone in the body and measurements and reflects the longitudinal growth of the fetus (approximately 14 weeks 1.5 cm - term 7.8 cm). It is one of the four typical ultrasound assessments of fetal size and age: Biparietal Diameter (BPD), |Head Circumference (HC), Abdominal Circumference (AC), and Femur Length (FL).
- Fetal size and age - typically measured using 4 ultrasound assessments: Biparietal Diameter (BPD), Head Circumference (HC), Abdominal Circumference (AC), and Femur Length (FL).
- Functional linear discriminant analysis - (FLDA) new growth assessment technique using serial measurements to discriminate between normal and abnormal fetal growth during 2nd and 3rd trimester.
- Head Circumference - (HC) Measured as an ellipse in a horizontal section at the level of the thalamus and the cavum septi pellucidi. 2nd trimester Fetal head growth
- Gestational sac - (GS) size formed initially by the chorionic cavity, after the embryonic period (week 8, GA W10) the amniotic cavity expands and fuses with the chorion. Measured by mean gestation sac diameter.
- inversion mode - an ultrasound processing method of volume analysis for the visualization of fluid-filled fetal structures such as; heart chambers, vessel lumen, stomach, gallbladder, renal pelvis, and the bladder. Post-processing inverts the gray scale of the volume voxels showing the normally anechoic structures in 3D or 4D renderings. This technique has been used to identify cardiac anomalies.
- Linear discriminant analysis - (LDA) to longitudinal data (James and Hastie, 2001)
- Mean gestation sac diameter - (MSD) = (length + height + width)/3. At week 3 (GAweek 5) MSD measures 2-3 mm. Normal MSD (in mm) + 30 = days of pregnancy.
- Mean yolk sac diameter - (MYD) can be used as marker for subsequent embryonic death or abnormalities (PMID 22215774).
- Spatiotemporal image correlation (STIC) - an image acquisition method used mainly for fetal heart analysis. Requires two steps; an automatic volume sweep, then image data analysis according to spatial and temporal domain generating an online dynamic 3D image sequence.
- Transabdominal scan - the ultrasound probe is placed on the external abdomen wall to scan pelvic region structures, conceptus and placenta. Also used to guide prenatal diagnostic techniques of chorionic villus sampling and amniocentesis.
- Transvaginal scan - (TVS) the ultrasound probe is placed inside the vagina and scans for female genital (uterus, ovary) and ectopic pregnancy.
- Termination of pregnancy - (TOP)
| Other Terms Lists |
|---|
| Terms Lists: ART | Birth | Bone | Cardiovascular | Cell Division | Endocrine | Gastrointestinal | Genital | Genetic | Head | Hearing | Heart | Immune | Integumentary | Neonatal | Neural | Oocyte | Palate | Placenta | Radiation | Renal | Respiratory | Spermatozoa | Statistics | Tooth | Ultrasound | Vision | Historic | Drugs | Glossary |
External Links
External Links Notice - The dynamic nature of the internet may mean that some of these listed links may no longer function. If the link no longer works search the web with the link text or name. Links to any external commercial sites are provided for information purposes only and should never be considered an endorsement. UNSW Embryology is provided as an educational resource with no clinical information or commercial affiliation.
- Australian Society for Ultrasound Medicine - Guidelines For The Mid Trimester Obstetric Scan PDF (2005)
- American Registry for Diagnostic Medical Sonography - ARDMS Resources for Students and Educators
Glossary Links
- Glossary: A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | Numbers | Symbols | Term Link
Cite this page: Hill, M.A. (2024, April 27) Embryology Ultrasound. Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/Ultrasound
- © Dr Mark Hill 2024, UNSW Embryology ISBN: 978 0 7334 2609 4 - UNSW CRICOS Provider Code No. 00098G