Canada Statistics
| Embryology - 30 Apr 2024 |
|---|
| Google Translate - select your language from the list shown below (this will open a new external page) |
|
العربية | català | 中文 | 中國傳統的 | français | Deutsche | עִברִית | हिंदी | bahasa Indonesia | italiano | 日本語 | 한국어 | မြန်မာ | Pilipino | Polskie | português | ਪੰਜਾਬੀ ਦੇ | Română | русский | Español | Swahili | Svensk | ไทย | Türkçe | اردو | ייִדיש | Tiếng Việt These external translations are automated and may not be accurate. (More? About Translations) |
Introduction
This page links to the current online resources available to explore Canadian population and birth data. See also the recent report on ART in Canada.
| Statistics Links: Introduction | Reports | World Population | World Fertility | World Infant Mortality | Maternal Mortality | Australia | Brazil | Canada | China | Germany | India | Indonesia | Europe | Myanmar | Netherlands | Spain | United Kingdom | Romania | Uganda | United States | BGD Tutorial - Applied Embryology and Teratology | National Perinatal Statistics Unit | AIHW | Category:Statistics | |
|
Some Recent Findings
|
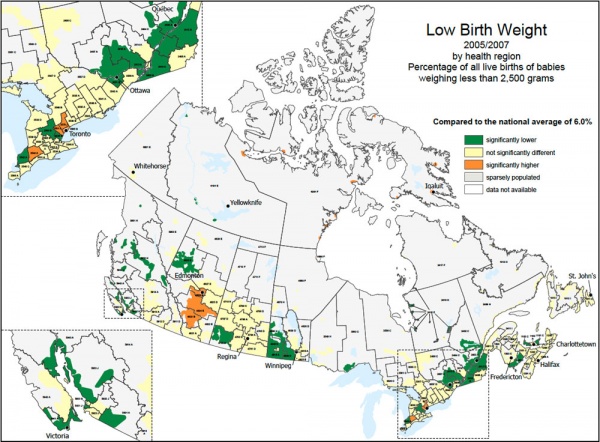
Low Birth Weight by Region
Source: Health Indicator Maps, catalogue no. 82-583-XIE, Vol. 2010, No.1. (CANSIM Table 102-4303). Produced by the Geography Division for the Health Statistics Division, Statistics Canada, 2010.
Canadian Growth Charts
- New standards: WHO growth charts measure up for Canada PDF
- Promoting optimal monitoring of child growth in Canada: Using the new who growth charts PDF
General Statistics
Population: 34,030,589 (July 2011 est.) country comparison to the world: 37
Age structure
- 0-14 years: 15.7% (male 2,736,737/female 2,602,342)
- 15-64 years: 68.5% (male 11,776,611/female 11,517,972)
- 65 years and over: 15.9% (male 2,372,356/female 3,024,571) (2011 est.)
Median age
- total: 41 years
- male: 39.8 years
- female: 42.1 years (2011 est.)
Population growth rate
- 0.794% (2011 est.)
- country comparison to the world: 136
Birth rate
- 10.28 births/1,000 population (2011 est.)
- country comparison to the world: 187
Death rate
- 7.98 deaths/1,000 population (July 2011 est.)
- country comparison to the world: 105
Sex ratio
- at birth: 1.056 male(s)/female
- under 15 years: 1.05 male(s)/female
- 15-64 years: 1.02 male(s)/female
- 65 years and over: 0.78 male(s)/female
- total population: 0.98 male(s)/female (2011 est.)
Infant mortality rate
- total: 4.92 deaths/1,000 live births
- country comparison to the world: 183
- male: 5.26 deaths/1,000 live births
- female: 4.56 deaths/1,000 live births (2011 est.)
Life expectancy at birth
- total population: 81.38 years
- country comparison to the world: 12
- male: 78.81 years
- female: 84.1 years (2011 est.)
Total fertility rate
- 1.58 children born/woman (2011 est.)
- country comparison to the world: 178
Age structure
- 0-14 years: 20.1% (male 32,107,900/female 30,781,823)
- 15-64 years: 66.8% (male 104,411,352/female 104,808,064)
- 65 years and over: 13.1% (male 17,745,363/female 23,377,542) (2011 est.)
Median age
- total: 36.9 years
- male: 35.6 years
- female: 38.2 years (2011 est.)
Population growth rate
- 0.963% (2011 est.)
- country comparison to the world: 119
Birth rate
- 13.83 births/1,000 population (2011 est.)
- country comparison to the world: 149
Death rate
- 8.38 deaths/1,000 population (July 2011 est.)
- country comparison to the world: 89
Sex ratio
- at birth: 1.047 male(s)/female
- under 15 years: 1.04 male(s)/female
- 15-64 years: 1 male(s)/female
- 65 years and over: 0.75 male(s)/female
- total population: 0.97 male(s)/female (2011 est.)
Infant mortality rate
- total: 6.06 deaths/1,000 live births
- country comparison to the world: 176
- male: 6.72 deaths/1,000 live births
- female: 5.37 deaths/1,000 live births (2011 est.)
Life expectancy at birth
- total population: 78.37 years
- country comparison to the world: 50
- male: 75.92 years
- female: 80.93 years (2011 est.)
Total fertility rate
- 2.06 children born/woman (2011 est.)
- country comparison to the world: 123
HIV/AIDS
adult prevalence rate
- 0.3% (2009 est.)
- country comparison to the world: 91
people living with HIV/AIDS
- 68,000 (2009 est.)
- country comparison to the world: 50
deaths
- fewer than 1,000 (2009 est.)
- country comparison to the world: 69
Ethnic groups
British Isles origin 28%, French origin 23%, other European 15%, Amerindian 2%, other, mostly Asian, African, Arab 6%, mixed background 26%
Data: The World Factbook Canada
Assisted Reproductive Technology
Society of Obstetricians and Gynaecologists of Canada - Pregnancy outcomes after assisted human reproduction[3]
Summary Statements (for January 2005 to December 2012)
- There is increasing evidence that infertility or subfertility is an independent risk factor for obstetrical complications and adverse perinatal outcomes, even without the addition of assisted human reproduction.
- The relative risk for an imprinting phenotype such as Silver-Russell syndrome, Beckwith-Wiedemann syndrome, or Angelman syndrome is increased in the assisted reproduction population, but the actual risk for one of these phenotypes to occur in an assisted pregnancy is estimated to be low, at less than 1 in 5000. The exact biological etiology for this increased imprinting risk is likely heterogeneous and requires more research. (II-2) Recommendations 1. All men with severe oligozoospermia or azoospermia (sperm count < 5 million/hpf) should be offered genetic/clinical counselling, karyotype assessment for chromosomal abnormalities, and Y-chromosome microdeletion testing prior to in vitro fertilization with intracytoplasmic sperm injection. (II-2A) 2. All men with unexplained obstructive azoospermia should be offered genetic/clinical counselling and genetic testing for cystic fibrosis prior to in vitro fertilization with intracytoplasmic sperm injection.
- Multiple pregnancy is the most powerful predictive factor for adverse maternal, obstetrical, and perinatal outcomes. Couples should be thoroughly counselled about the significant risks of multiple pregnancies associated with all assisted human reproductive treatments.
- The benefits and cumulative pregnancy rates of elective single embryo transfer support a policy of using this protocol in couples with good prognosis for success, and elective single embryo transfer should be strongly encouraged in this population.
- To reduce the incidence of multiple pregnancy, health care policies that support public funding for assisted human reproduction, with regulations promoting best practice regarding elective single embryo transfer, should be strongly encouraged.
- Among singleton pregnancies, assisted reproductive technology is associated with increased risks of preterm birth and low birth weight infants, and ovulation induction is associated with an increased risk of low birth weight infants. Until sufficient research has clarified the independent roles of infertility and treatment for infertility, couples should be counselled about the risks associated with treatment. (II-2B) There is a role for closer obstetric surveillance of women who conceive with assisted human reproduction.
- There is growing evidence that pregnancy outcomes are better for cryopreserved embryos fertilized in vitro than for fresh embryo transfers. This finding supports a policy of elective single embryo transfer for women with a good prognosis (with subsequent use of cryopreserved embryos as necessary), and may reassure women who are considering in vitro fertilization. (II-2A)
- Women and couples considering assisted human reproduction and concerned about perinatal outcomes in singleton pregnancies should be advised that (1) intracytoplasmic sperm injection does not appear to confer increased adverse perinatal or maternal risk over standard in vitro fertilization, and (2) the use of donor oocytes increases successful pregnancy rates in selected women, but even when accounting for maternal age, can increase the risks of low birth weight and preeclampsia.
- Any assisted reproductive technology procedure should be prefaced by a discussion of fetal outcomes and the slight increase in the risk of congenital structural abnormalities, with emphasis on known confounding factors such as infertility and body mass index.
- In pregnancies achieved by artificial reproductive technology, routine anatomic ultrasound for congenital structural abnormalities is recommended between 18 and 22 weeks. (II-2A)
- Pregnancies conceived by intracytoplasmic sperm injection may be at increased risk of chromosomal aberrations, including sex chromosome abnormalities. Diagnostic testing should be offered after appropriate counselling.
- The possible increased risk for late onset cancer due to gene dysregulation for tumour suppression requires more long-term follow-up before the true risk can be determined.
- The clinical application of preimplantation genetic testing in fertile couples must balance the benefits of avoiding disease transmission with the medical risks and financial burden of in vitro fertilization.
- Preimplantation screening for aneuploidy is associated with inconsistent findings for improving pregnancy outcomes. Any discussion of preimplantation genetic screening with patients should clarify that there is no adequate information on the long-term effect of embryo single cell biopsy.
References
External Links
External Links Notice - The dynamic nature of the internet may mean that some of these listed links may no longer function. If the link no longer works search the web with the link text or name. Links to any external commercial sites are provided for information purposes only and should never be considered an endorsement. UNSW Embryology is provided as an educational resource with no clinical information or commercial affiliation.
- Statistics Canada - Pregnancy and births
- The World Factbook Canada
Glossary Links
- Glossary: A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | Numbers | Symbols | Term Link
Cite this page: Hill, M.A. (2024, April 30) Embryology Canada Statistics. Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/Canada_Statistics
- © Dr Mark Hill 2024, UNSW Embryology ISBN: 978 0 7334 2609 4 - UNSW CRICOS Provider Code No. 00098G