| ICD-11
|
JA01 Ectopic pregnancy
- Any condition characterized by implantation of the embryo outside the endometrium and endometrial cavity during pregnancy.
|
Introduction
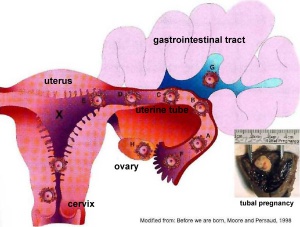
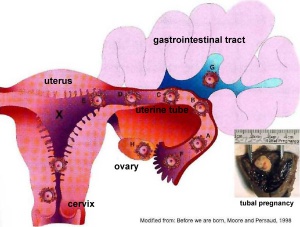
Ectopic implantation or ectopic pregnancy (Greek, ektopos = "out of place") refers to the abnormal implantation of the blastocyst. Implantation of the blastocyst normally occurs within the body of the uterus, also called eutopic implantation. Ectopic implantation can occur at number of sites outside the uterine body. The most common form of human ectopic pregnancy is when implantation occurs within the uterine tube, described as a tubal pregnancy. Note that the endocrine signals blocking the menstrual cycle and indicating a pregnancy will still be released following this ectopic implantation. Ectopic pregnancies are therefore often identified by early ultrasound scans.
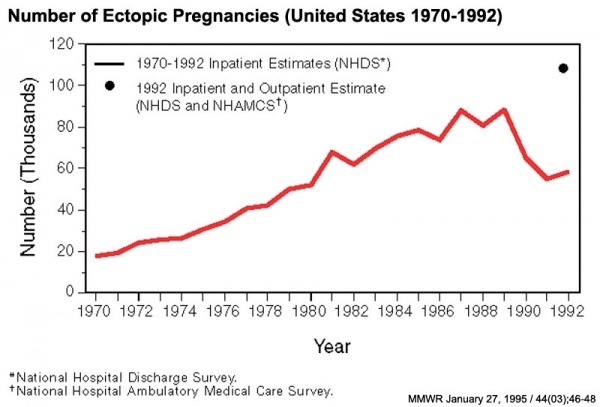
Ectopic pregnancy is also a high-risk maternal medical condition with an approximate incidence of 1.5 to 2 % in reported pregnancies. There is some indication that the incidence may be increasing (United States has increased from 4.5 per 1,000 pregnancies in 1970 to an estimated 19.7 per 1,000 pregnancies in 1992[1])
The risk factors for tubal ectopic pregnancy include: tubal damage by infection (particularly Chlamydia trachomatis) or surgery, smoking and in vitro fertilization therapy. Prolonged tubal damage is often described as pelvic inflammatory disease and "scarring" can affect the cilia-mediated transport of the blastocyst during the first week of development.
This is also the most common cause of pregnancy-related deaths in the first trimester. A recent United Kingdom enquiry into maternal deaths[2], identified ectopic pregnancy as the fourth most common cause of maternal death (73% of early pregnancy deaths).
Ectopic sites are named according to the anatomical location: Tubal (Ampullary, Isthmic, Cornual), Cervical and Ovarian. A study of 1800 surgically treated ectopics between 1992 and 2001 identified implantation sites by frequency: interstitial (2.4%), isthmic (12.0%), ampullary (70.0%), fimbrial (11.1%), ovarian (3.2%) or abdominal (1.3%).[3]
Some Recent Findings
Abnormal implantation sites
- Rates of pelvic inflammatory disease and ectopic pregnancy in Australia, 2009-2014[4] "To analyse yearly rates of pelvic inflammatory disease (PID) and ectopic pregnancy (EP) diagnosed in hospital settings in Australia from 2009 to 2014. METHODS: We calculated yearly PID and EP diagnosis rates in three states (Victoria, New South Wales, Queensland) for women aged 15-44 years using hospital admissions and emergency department (ED) attendance data, with population and live birth denominators. ...For EP, in 2014 the rate of all admissions was 17.4 (95% CI 16.9 to 17.9) per 1000 live births and of all ED presentations was 15.6 (95% CI 15.1 to 16.1). Comparing 2014 with 2009, the rates of all EP admissions (aIRR 1.06, 95% CI 1.04 to 1.08) and rates in EDs (aIRR 1.24, 95% CI 1.18 to 1.31) were higher. PID and EP remain important causes of hospital admissions for female STI-associated complications. Hospital EDs care for more PID cases than inpatient departments, particularly for young women." Australian statistics | bacterial infection
|
| More recent papers
|
|
This table allows an automated computer search of the external PubMed database using the listed "Search term" text link.
- This search now requires a manual link as the original PubMed extension has been disabled.
- The displayed list of references do not reflect any editorial selection of material based on content or relevance.
- References also appear on this list based upon the date of the actual page viewing.
References listed on the rest of the content page and the associated discussion page (listed under the publication year sub-headings) do include some editorial selection based upon both relevance and availability.
More? References | Discussion Page | Journal Searches | 2019 References | 2020 References
Search term: Ectopic Pregnancy | Tubal Pregnancy
|
| Older papers
|
| These papers originally appeared in the Some Recent Findings table, but as that list grew in length have now been shuffled down to this collapsible table.
See also the Discussion Page for other references listed by year and References on this current page.
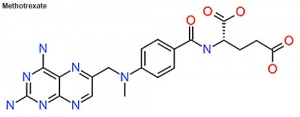
- Comparison of double- and single-dose methotrexate protocols for treatment of ectopic pregnancy (EP)[5] "For treatment of EP, double-dose methotrexate had efficacy and safety comparable to that of single-dose methotrexate; it had better success among patients with moderately high β-hCG and led to a shorter follow up."
- Misdiagnosis of cervical ectopic pregnancy (CEP)[6] "Misdiagnosis of CEP upon initial presentation is a common occurrence. Transvaginal ultrasound performed by a qualified practitioner may increase detection and prevent treatment delay."
- Human tubal ectopic pregnancy and knockout mouse models.[7] "Tubal abnormalities and dysfunction, such as altered contractility or abnormal ciliary activity, have been speculated to lead to tubal ectopic pregnancy. To elucidate the cellular and molecular mechanisms of the tubal transport process, several knockout (KO) mouse models have been developed. This review summarizes what has been learned from studies of the Fallopian tube in caspase-1, cannabinoid receptor and Dicer1 KO mice."
|
About Uterine Tube Anatomy
Anatomy - there are 3 main parts (regions) to the uterine tube:
- isthmus - closest to the uterus (body)
- ampulla - middle region, more dilated in diameter and most common site for fertilization.
- infundibulum - furthest from the uterus ending in the fimbriae and open to the peritoneum
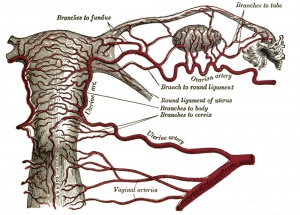
Blood Supply - arterial supply is from branches of the uterine and ovarian arteries, these small vessels are located within the mesosalpinx (part of the lining of the abdominal cavity).
Lymphatic drainage - through the iliac and lateral aortic nodes.
Innervation - has both sympathetic and parasympathetic fibers. Sensory fibres from thoracic segments (T11-T12) and the first lumbar segment (L1).
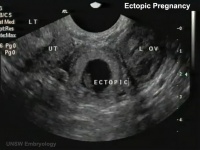
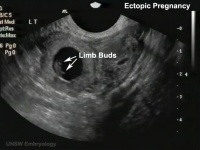
Ultrasound Ectopic Implantation
| Tubal Ectopic
|
Bicornuate Uterus Ectopic
|
|
|
|
- Links: Ectopic Implantation | Ultrasound
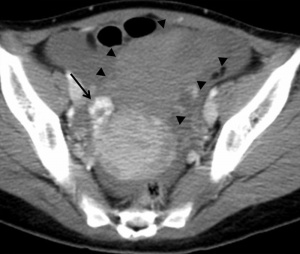
Computed Tomography Ectopic Implantation
Computed Tomography imaging findings of a 37-year-old woman with interstitial pregnancy.[8] Showing initial CT detection and a subsequent scan following rupture causing a hematoma around uterus and a massive hemoperitoneum.

Initial CT - gestational sac
|
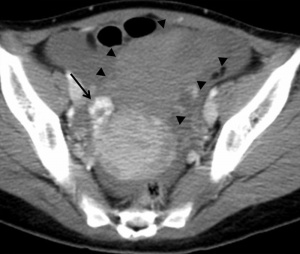
Follow-up CT - massive hemoperitoneum
|

CT - hematoma around uterus
|
- Links: Computed Tomography
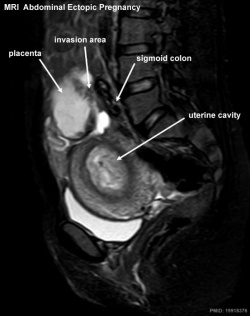
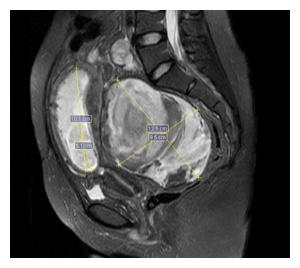
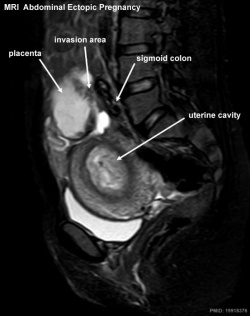
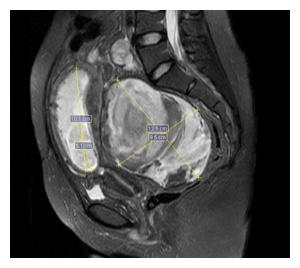
Magnetic Resonance Imaging Abdominal Ectopic Implantation
2W SPAIR sagittal MRI of lower abdomen demonstrating the placental invasion.[9]
- Placenta was attached tightly to the mesentery of sigmoid colon and was loosely adhered to the left abdominal sidewall.
- The fetus was localized at the right of the abdomen and was related to the placenta by a cord.
See also Heterotopic Pregnancy
|
|
- Links: Magnetic Resonance Imaging
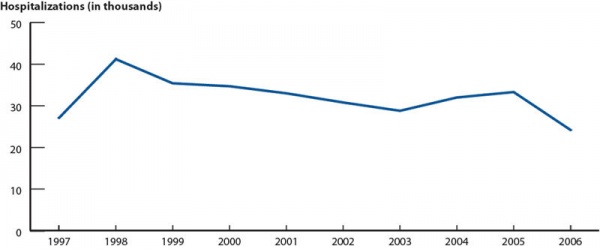
Statistics
Australia
Rates of pelvic inflammatory disease and ectopic pregnancy in Australia, 2009-2014[4]
- "To analyse yearly rates of pelvic inflammatory disease (PID) and ectopic pregnancy (EP) diagnosed in hospital settings in Australia from 2009 to 2014. METHODS: We calculated yearly PID and EP diagnosis rates in three states (Victoria, New South Wales, Queensland) for women aged 15-44 years using hospital admissions and emergency department (ED) attendance data, with population and live birth denominators. ...For EP, in 2014 the rate of all admissions was 17.4 (95% CI 16.9 to 17.9) per 1000 live births and of all ED presentations was 15.6 (95% CI 15.1 to 16.1). Comparing 2014 with 2009, the rates of all EP admissions (aIRR 1.06, 95% CI 1.04 to 1.08) and rates in EDs (aIRR 1.24, 95% CI 1.18 to 1.31) were higher. PID and EP remain important causes of hospital admissions for female STI-associated complications. Hospital EDs care for more PID cases than inpatient departments, particularly for young women."
- Links: Australian statistics | bacterial infection
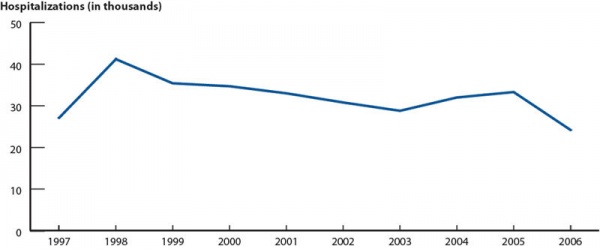
USA
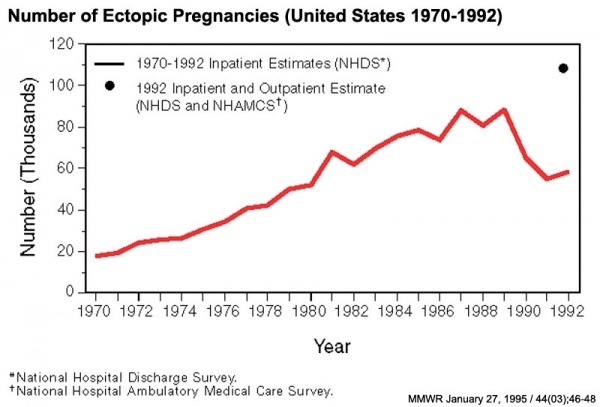
Ectopic Pregnancies- United-States 1970-1992[1]
- Links: USA
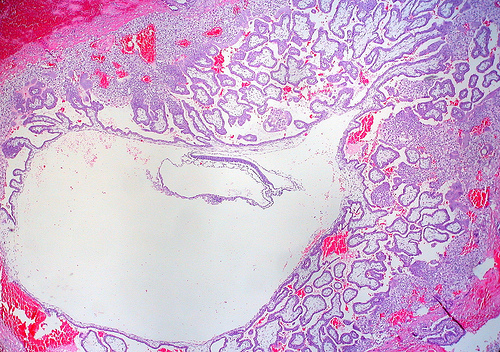
Ectopic Pregnancy Histology
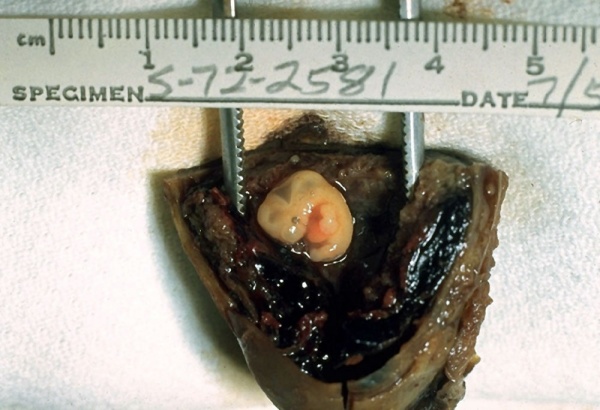
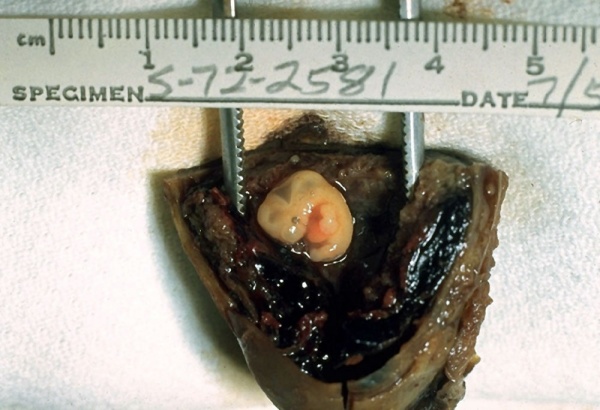
CDC Image by Dr. Edwin P. Ewing, Jr., 1972
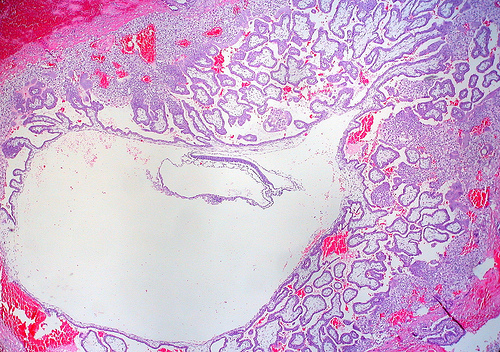
Ed Uthman Image (pathologist in Houston, Texas) section of ectopic (tubal) pregnancy about Carnegie stage 7 in Week 3.
Image version links: ExtraLarge 1712x1206px | Large 1024x721px | Medium 500x352px
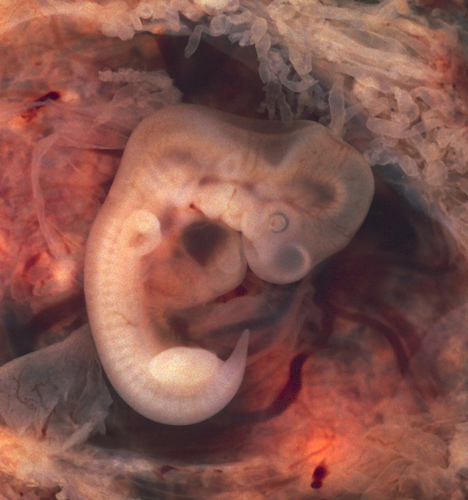
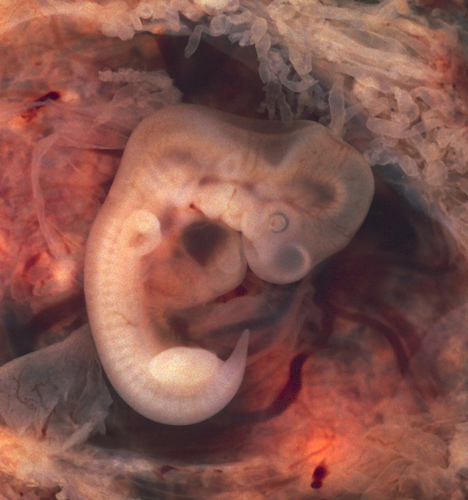
Ed Uthman Image (pathologist in Houston, Texas) image of of ectopic (tubal) pregnancy about Carnegie stage 15 in Week 5.
Image version links: ExtraLarge 1874 x 2000px | Large 959 x 1024px | Medium 468 x 500px
Tubal Ectopic Pregnancy
| Chlamydia infections (Chlamydia trachomatis) are the most common bacterial sexually transmitted infection, often undiagnosed and asymptomatic. The infections can ascend the female genital tract, colonizing the endometrial mucosa, then the uterine tubes. This type of infection is described as pelvic inflammatory disease (PID).
|
 Tubal pregnancy shown after hysterectomy |
Interstitial Pregnancy
| (cornual pregnancy) A less common type 2 to 4% of ectopic pregnancies. The gestation develops in the uterine portion of the fallopian tube lateral to the round ligament.
|
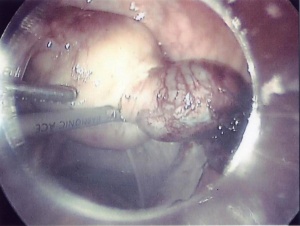 Interstitial ectopic pregnancy [10] |
Ovarian Ectopic Pregnancy
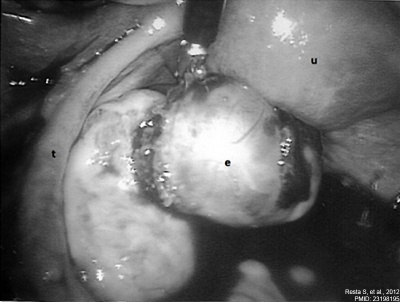
| Clinical operative photograph at the beginning of the procedure of the laparoscopic treatment of the ovarian pregnancy.
Legend
- u - normal aspect of the uterus.
- t - left fallopian tube.
- e - ruptured ectopic pregnancy in the left ovary.
|
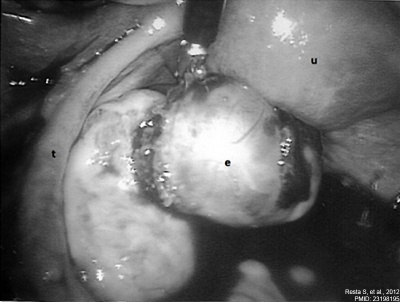
Ovarian Ectopic Pregnancy[11]
|
Cervical Ectopic Pregnancy

Cervical Ectopic Pregnancy Ultrasound
[12]This form of ectopic pregnancy is a rare high-risk condition and represents less than 1% of all ectopic pregnancies. The reported incidence varies between 1:1,000 to 1:18,000.
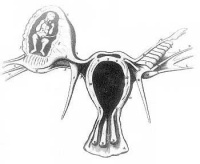
Rudimentary Horn Pregnancy
A rare types of ectopic pregnancy (about 1 in 76,000 pregnancies) in most cases the horn is non-communicating. Therefore fertilisation probably occurs by transperitoneal migration. This form untreated can also lead to uterine rupture.
Caesarean Scar Pregnancy
Caesarean scar pregnancy (CSP) is a rare types of ectopic pregnancy (about 1 in 2000 pregnancies), but probably increasing as caesarean rates rise. The gestation is completely surrounded by both myometrium and fibrous tissue of the caesarean section scar and separated from the endometrial cavity and endocervical canal.
A recent review of 17 studies (69 cases of CSP managed expectantly, 52 with and 17 without embryonic/fetal heart beat)[13]
| Caesarean scar pregnancy (CSP)
|
| with embryonic/fetal heart activity
|
without embryonic/fetal cardiac activity
|
- 13.0% experienced an uncomplicated miscarriage
- 20.0% required medical intervention
- 9.9% uterine rupture during the first or second trimester
- 15.2% required hysterectomy
- 76.9% women progressed to third trimester
- 39.2% experienced severe bleeding
- 74.8% had abnormally invasive placenta at delivery
- 69.7% had placenta percreta
|
- 69.1% experienced an uncomplicated miscarriage
- 30.9% required medical intervention
- 13.4% uterine rupture during the first trimester
- hysterectomy was not required in any case
|
Heterotopic Pregnancy
Heterotopic pregnancy MRI
[14](Greek, heteros = other) Clinical term for a very rare pregnancy of two or more embryos, consisting of both a uterine cavity embryo implantation and an ectopic implantation. The ectopic implantation usually identified by prenatal scanning as occurring within the uterine tube (tubal pregnancy) though has also been identified as abdominal pregnancies.[14][15]
Ectopic Molar Pregnancy

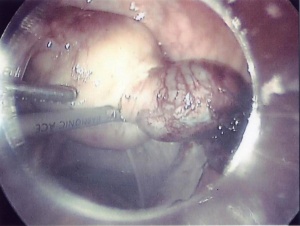
Left-sided unruptured ampullary ectopic pregnancy at laparoscopy.[16]
- Links: Hydatidiform Mole
Ruptured Ectopic

|
Ruptured ectopic pregnancy[17]
Ruptured ectopic pregnancy (black arrow) in remnant of left tube (blue arrow).
|
Methotrexate
(MTX, amethopterin) Drug with several different uses including the treatment of ectopic pregnancy[18] and for the induction of medical abortions. Acts as a antimetabolite and antifolate (folic acid antagonist) drug that inhibits DNA synthesis in actively dividing cells, including trophoblasts, and therefore has other medical uses include cancer and autoimmune disease treatment. Treatment success in ectopic pregnancy relates to serum β human chorionic gonadotropin (β-hCG) concentration.
- Links: Medline Plus
References
- ↑ 1.0 1.1 Centers for Disease Control and Prevention (CDC). (1995). Ectopic pregnancy--United States, 1990-1992. MMWR Morb. Mortal. Wkly. Rep. , 44, 46-8. PMID: 7823895
- ↑ Confidential Enquiry into Maternal Deaths (CEMD) Why Mothers Die 2000–2002 PDFPDF2
- ↑ Bouyer J, Coste J, Fernandez H, Pouly JL & Job-Spira N. (2002). Sites of ectopic pregnancy: a 10 year population-based study of 1800 cases. Hum. Reprod. , 17, 3224-30. PMID: 12456628
- ↑ 4.0 4.1 Goller JL, De Livera AM, Guy RJ, Low N, Donovan B, Law M, Kaldor JM, Fairley CK & Hocking JS. (2018). Rates of pelvic inflammatory disease and ectopic pregnancy in Australia, 2009-2014: ecological analysis of hospital data. Sex Transm Infect , , . PMID: 29720385 DOI.
- ↑ Hamed HO, Ahmed SR & Alghasham AA. (2012). Comparison of double- and single-dose methotrexate protocols for treatment of ectopic pregnancy. Int J Gynaecol Obstet , 116, 67-71. PMID: 22035883 DOI.
- ↑ Shavell VI, Abdallah ME, Zakaria MA, Berman JM, Diamond MP & Puscheck EE. (2012). Misdiagnosis of cervical ectopic pregnancy. Arch. Gynecol. Obstet. , 285, 423-6. PMID: 21748311 DOI.
- ↑ Shao R. (2010). Understanding the mechanisms of human tubal ectopic pregnancies: new evidence from knockout mouse models. Hum. Reprod. , 25, 584-7. PMID: 20023297 DOI.
- ↑ Shin BS & Park MH. (2010). Incidental detection of interstitial pregnancy on CT imaging. Korean J Radiol , 11, 123-5. PMID: 20046504 DOI.
- ↑ Yildizhan R, Kolusari A, Adali F, Adali E, Kurdoglu M, Ozgokce C & Cim N. (2009). Primary abdominal ectopic pregnancy: a case report. Cases J , 2, 8485. PMID: 19918376 DOI.
- ↑ Walid MS & Heaton RL. (2010). Diagnosis and laparoscopic treatment of cornual ectopic pregnancy. Ger Med Sci , 8, . PMID: 20725587 DOI.
- ↑ Resta S, Fuggetta E, D'Itri F, Evangelista S, Ticino A & Porpora MG. (2012). Rupture of Ovarian Pregnancy in a Woman with Low Beta-hCG Levels. Case Rep Obstet Gynecol , 2012, 213169. PMID: 23198195 DOI.
- ↑ Mohebbi MR, Rosenkrans KA, Luebbert EE, Hunt TT & Jung MJ. (2011). Ectopic pregnancy in the cervix: a case report. Case Rep Med , 2011, 858241. PMID: 22110520 DOI.
- ↑ Calì G, Timor-Tritsch IE, Palacios-Jaraquemada J, Monteaugudo A, Buca D, Forlani F, Familiari A, Scambia G, Acharya G & D'Antonio F. (2018). Outcome of Cesarean scar pregnancy managed expectantly: systematic review and meta-analysis. Ultrasound Obstet Gynecol , 51, 169-175. PMID: 28661021 DOI.
- ↑ 14.0 14.1 Sun SY, Araujo Júnior E, Elito Júnior J, Rolo LC, Campanharo FF, Sarmento SG, Nardozza LM & Moron AF. (2012). Diagnosis of heterotopic pregnancy using ultrasound and magnetic resonance imaging in the first trimester of pregnancy: a case report. Case Rep Radiol , 2012, 317592. PMID: 23259128 DOI.
- ↑ Gayer G. (2012). Images in clinical medicine. Abdominal ectopic pregnancy. N. Engl. J. Med. , 367, 2334. PMID: 23234516 DOI.
- ↑ Bousfiha N, Erarhay S, Louba A, Saadi H, Bouchikhi C, Banani A, El Fatemi H, Sekkal M & Laamarti A. (2012). Ectopic molar pregnancy: a case report. Pan Afr Med J , 11, 63. PMID: 22655097
- ↑ Samiei-Sarir B & Diehm C. (2013). Recurrent ectopic pregnancy in the tubal remnant after salpingectomy. Case Rep Obstet Gynecol , 2013, 753269. PMID: 24151570 DOI.
- ↑ Stovall TG & Ling FW. (1993). Single-dose methotrexate: an expanded clinical trial. Am. J. Obstet. Gynecol. , 168, 1759-62; discussion 1762-5. PMID: 8317518
Reviews
Shaw JL, Dey SK, Critchley HO & Horne AW. (2010). Current knowledge of the aetiology of human tubal ectopic pregnancy. Hum. Reprod. Update , 16, 432-44. PMID: 20071358 DOI.
Shao R. (2010). Understanding the mechanisms of human tubal ectopic pregnancies: new evidence from knockout mouse models. Hum. Reprod. , 25, 584-7. PMID: 20023297 DOI.
Corpa JM. (2006). Ectopic pregnancy in animals and humans. Reproduction , 131, 631-40. PMID: 16595714 DOI.
Articles
Exalto N, Vooys GP, Meyer JW & Lange WP. (1980). Ovarian pregnancy: a morphologic description. Eur. J. Obstet. Gynecol. Reprod. Biol. , 11, 179-87. PMID: 7194809
Purslow CE. (1915). Tubal Pregnancy showing Foetus undergoing Dissolution. Proc. R. Soc. Med. , 8, 68. PMID: 19978839
Matsunaga E & Shiota K. (1980). Ectopic pregnancy and myoma uteri: teratogenic effects and maternal characteristics. Teratology , 21, 61-9. PMID: 7385056 DOI.
Search Pubmed
June 2010
- "ectopic pregnancy" All (14958) Review (1350) Free Full Text (1196)
- "tubal pregnancy" All (8010) Review (683) Free Full Text (630)
Search Pubmed: ectopic pregnancy | ectopic implantation | tubal pregnancy | tubal implantation
External Links
External Links Notice - The dynamic nature of the internet may mean that some of these listed links may no longer function. If the link no longer works search the web with the link text or name. Links to any external commercial sites are provided for information purposes only and should never be considered an endorsement. UNSW Embryology is provided as an educational resource with no clinical information or commercial affiliation.
| Placenta Terms (expand to view)
|
- after-birth - term used to describe the delivery of placenta and placental membranes following birth of the child.
- allantois - An extraembryonic membrane, endoderm in origin extension from the early hindgut, then cloaca into the connecting stalk of placental animals, connected to the superior end of developing bladder. In reptiles and birds, acts as a reservoir for wastes and mediates gas exchange. In mammals is associated/incorporated with connecting stalk/placental cord fetal-maternal interface.
- amniocentesis - Clinical term for a prenatal diagnostic test where an ultrasound guided needle is used to extract a sample of the amniotic fluid. Amniocentesis
- anastomosis - Term used to describe the connection between two tubes. Applied to describe the connection between peripheral blood vessels without an intervening capillary bed.
- anchoring villi - (stem villi) describes the placental villi (embryonic) that attach to the decidua (maternal) tissue. The tip of the villi consists of a column of trophoblast cells attached to an epithelial plaque.
- angioblasts form clusters or blood islands on surface of yolk sac.
- angiogenesis - Term describing the development of new vessels from already existing vessels, this process is secondary to vasculogenesis which is the initial formation of first blood vessels by differentiation of pluripotent mesenchymal cells (extraembryonic mesoderm).
- capsularis - portion of maternal decidua that covers the conceptus facing towards the uterine cavity.
- cerebroplacental ratio - (CPR) a doppler ultrasound measurement calculated as the simple ratio between the middle cerebral artery pulsatility index (MCA‐PI) and the umbilical artery pulsatility index (UA‐PI). Fetuses with an abnormal ratio are thought to be a predictor of adverse pregnancy outcome.
- chorioamnionitis - (CA) An intraamniotic puerperal infection described as having 3 forms: histologic, clinical (clinical chorioamnionitis, IAI), and subclinical. Intraamniotic infection is a common (2-4%) event in labor and the systemic inflammatory response can also lead to preterm birth and neonatal complications.
- chorion - The extraembryonic membrane generated from trophoblast and extraembryonic mesoderm that forms placenta. chorion and amnion are made by the somatopleure. The chorion becomes incorporated into placental development. The avian and reptilian chorion lies beside the egg shell and allows gas exchange.
- chorionic cavity - The fluid-filled extraembryonic coelom (cavity) formed initially from trophoblast and extraembryonic mesoderm that forms placenta. chorion and amnion are made by the somatopleure. The chorion becomes incorporated into placental development. The avian and reptilian chorion lies beside the egg shell and allows gas exchange. In humans, this cavity is lost during week 8 when the amniotic cavity expands and fuses with the chorion.
- chorion frondosum - (frondosum = leafy) The chorion found on conceptus oriented towards maternal blood supply where the majority of villi form and proliferate, will contribute the fetal component of the future placenta.
- chorion laeve - (laeve = smooth) The smooth chorion found on conceptus away from maternal blood supply (towards uterine epithelium and cavity) with very few villi present.
- chorionic somatomammotropin - (CSH, human lactogen) A hormone synthesized within the placenta by syncytiotrophoblast cells. This protein hormone (190 amino acid) has a structure is similar to pituitary growth hormone.
- chorionic villus sampling - (CVS) The taking a biopsy of the placenta, usually at the end of the second month of pregnancy, to test the fetus for genetic abnormalities.
- coelocentesis - A sampling of extracoelomic fluid usually for an early prenatal diagnostic technique.
- connecting stalk - the original extra-embryonic mesoderm structure attaching the embryonic disc to the chorion. The placental blood vessels form within this structure.
- cord blood - (human umbilical cord blood, HUCB) A term used to describe blood collected from the placenta usually after birth. Has been identified as a source of stem cells with potential therapeutic uses and is stored in Cord Blood Banks throughout the world.
- cord knotting Term describing umbilical or placental cord knotting. This occurs in about 1% prevents the passage of placental blood, pseudoknots also occur usually with no effect.
- cord presentation - A term used to describe at birth the presence of the umbilical cord between the fetal presenting part and the cervix, with or without membrane rupture.
- cord prolapse - A term used to describe at birth the descent of the umbilical cord through the cervix alongside (occult) or past (overt) the presenting part in the presence of ruptured membranes (incidence of 0.1% to 0.6%).
- cotyledon - (Greek, kotyle = a deep cup) In the embryos of seed plants, the "seed leaves," in which nutrients are stored for use after germination. In placental animals, the term is also to describe the leaf-like structure of the placenta surface.
- cytotrophoblast - The "cellular" trophoblast layer surrounding (forming a "shell") the early implanting conceptus. Beginning at uterine adplantation, proliferation and fusion of these cells is thought to form a second outer trophoblast layer, the syncytiotrophoblast. The cytotrophoblast layer contributes to formation of the placental villi, the functional component of the fetal placenta.
- decidua basalis - The term given to the uterine endometrium at the site of implantation where signaling transforms the uterine stromal cells (fibroblast-like) into decidual cells. This forms the maternal component of the placenta, the decidualization process gradually spreads through the remainder of the uterus, forming the decidua parietalis.
- decidua basalis reaction - Term describing the maternal endometrial changes that occur initially at the site of, and following, blastocyst implantation. Seen as a deposition of glycogen, fibrin and proliferation of blood vessels. See also decidualization.
- decidua capsularis - The term given to the uterine endometrium which has been converted to decidua surrounding the conceptus on the smooth chorion side.
- decidua parietalis - The term given to the remainder of the uterine endometrium, away from the site of implantation, that gradually becomes comverted to decidua.
- decidual cell - The uterine stromal cells (fibroblast-like) that differentiate in response to both steroid hormones (progesterone) and embryonic signals. These cells then alter uterine environment to support further embryonic development as well as producing cytokines related to prolactin (PRL) and have an innate immune function.
- decidual reaction - maternal endometrial reaction invoked in order to block the rapid extension of the implanting syncytium.
- decidualization - (decidualisation, decidual reaction) The process by which uterine stromal cells differentiate in response to both steroid hormones and embryonic signals into large epitheliod decidual cells. This process is essential for the progress of implantation and establishing fetal-maternal communication.
- DHEA - (dehydroepiandrosterone, androstenolone) precursor of sex steroid hormones and is converted to testosterone and estradiol. Postnatally, an abundant circulating steroid produced in the adrenal gland. The fetal adrenal cortex produces dehydroepiandrosterone sulfate (DHEA-S) used by the placenta to produce estrogens. DHEA, androstenedione, and testosterone can be metabolized to epiandrosterone, and etiocholanolone. PMID 15635500
- fetal drug addiction - occurs when drugs used maternally cross the placental barrier and can establish neural/physiological addiction in the unborn fetus. drugs
- fetal erythroblastosis - (Haemolytic Disease of the Newborn) A clinical term describing an immune response between fetal and maternal blood groups; from fetus Rh+ / maternal Rh-. The leakage of blood from fetus, particularly at birth, causes maternal anti-Rh antibodies, which is then dangerous for a 2nd or future pregnancies.
- fetal intra-abdominal umbilical vein varix - (FIUV, umbilical vein varix) focal dilatation of the umbilical venous diameter at the level of cord insertion, the dilatation diameter increases linearly with gestational age. Represent about 4% of umbilical cord abnormalities
with an incidence of about 2.8 per 1,000 pregnancies, there is also a rarer form of extra-abdominal varices.PMID 24883288
- fibrinoid layer - (Nitabuch's layer) A layer formed at maternal/fetal interface during placentation and is thought to act to prevent excessively deep conceptus implantation. Fibrin-type fibrinoid (maternal blood-clot product) and matrix-type fibrinoid (secreted by invasive extravillous trophoblast cells).
- floating chorionic villi - Term used to describe the placental microanatomy structure of chorionic villi that are not attached to the maternal decidua and float in the maternal blood-filled space (lacunae). Structurally the same as anchoring chorionic villi conceptus side that are attached to the maternal decidua.These villi go through the same stages of development: primary villi - secondary villi - tertiary villi
- hemotrophic nutrition - Term used to describe in late placenta development the transfer of blood-borne nutrition from maternal to embryo/fetuscompared to early histiotrophic nutrition.
- heterotopic pregnancy - (Greek, heteros = other) Clinical term for a very rare pregnancy of two or more embryos, consisting of both a uterine cavity embryo implantation and an ectopic implantation.
- histiotrophic nutrition - Term used to describe in early placenta development the intital transfer of nutrition from maternal to embryo (histiotrophic nutrition) compared to later blood-borne nutrition (hemotrophic nutrition). Histotroph is the nutritional material accumulated in spaces between the maternal and fetal tissues, derived from the maternal endometrium and the uterine glands. This nutritional material is absorbed by phagocytosis initially by blastocyst trophectoderm and then by trophoblast of the placenta. in later placental development nutrition is by the exchange of blood-borne materials between the maternal and fetal circulations, hemotrophic nutrition.
- Hofbauer cells - Cells found within placental villi connective tissue. Have a role as macrophages of mesenchymal origin with potentially additional functions (remodeling, vasculogenesis, regulation of stromal water content).
- Human chorionic corticotropin - (hCACTH) placental derived hormone equivilant to corticotropin (ACTH) from the pituitary.
- Human chorionic gonadotrophin - (hCG) like leutenizing hormone, supports corpus luteum, originally secreted by trophoblast cells.
- Human chorionic somatommotropin - (hCS, placental lactogen) hormone level increases in maternal blood through pregnancy, decreases maternal insulin sensitivity (raising maternal blood glucose levels and decreasing maternal glucose utilization) aiding fetal nutrition.
- Template:Hydatiform mole - A uterine tumour with "grape-like" placenta appearance without enclosed embryo formation, arises mainly from a haploid sperm fertilizing an egg without a female pronucleus. It is one form of gestational trophoblastic disease(GTD), a number of abnormalities including hydatiform mole, invasive mole, choriocarcinoma and placental site trophoblastic tumor (PSTT).
- hysterectomy – clinical term for the surgical removal of the uterus.
- Langhans layer - cytotrophoblast cell layer.
- maternal antibodies - antibodies from the mother's immune system that are capable of crossing placental barrier. They can provide immune protection to the embryo, but may also participate in immune disease (fetal erythroblastosis).
- maternal sinusoids - placental spaces around chorionic villi that are filled with maternal blood. This is the closest maternal/fetal exchange site.
- Nitabuch's layer - (fibrinoid layer) The layer formed at maternal/fetal interface during placentation and is thought to act to prevent excessively deep conceptus implantation. Fibrin-type fibrinoid (maternal blood-clot product) and matrix-type fibrinoid (secreted by invasive extravillous trophoblast cells).
- Morbidly adherent placenta (MAP) A general clinical term used to describe the different forms of abnormal placental implantation (Accreta, Increta and Percreta).
- oligohydramnios - Clinical term for the accumulation a deficiency of amniotic fluid during pregnancy. See also polyhydramnios, an excess of amniotic fluid.
- persistent right umbilical vein - (PRUV) A placental cord abnormality associated with fetal abnormalities and poor neonatal prognosis. The estimated incidence of persistent right umbilical vein in a low-risk population is 1 : 526. PMID 12047534
- polyhydramnios - Clinical term for the accumulation of excess amniotic fluid during pregnancy. See also oligohydramnios, a deficiency of amniotic fluid.
- placenta - (Greek, plakuos = flat cake) The developmental organ formed from maternal and fetal contributions in animals with placental development. In human, the placenta at term is a discoid shape "flat cake" shape; 20 cm diameter, 3 cm thick and weighs 500-600 gm. Placenta are classified by the number of layers between maternal and fetal blood (Haemochorial, Endotheliochorial and Epitheliochorial) and shape (Discoid, Zonary, Cotyledenary and Diffuse). The placenta has many different functions including metabolism, transport and endocrine.
- placenta accreta - The abnormal placental adherence, either in whole or in part of the placenta with absence of decidua basalis, leading to retention as an after-birth to the underlying uterine wall. The incidence of placenta accreta also significantly increases in women with previous cesarean section compared to those without a prior surgical delivery.
- placental arteries - (umbilical arteries) In placental animals, the blood vessels which develop within the placental cord carrying relatively deoxygenated blood from the embryo/fetus to the placenta. In humans, there are two placental arteries continuous with the paired internal iliac arteries (hypogastric arteries) arising off the dorsal aortas. At birth this vessel regresses and form the remnant medial umbilical ligament.
- placental cord - (umbilical cord) The placental cord is the structure connecting the embryo/fetus to the placenta. It is initially extra-embryonic mesoderm forming the connecting stalk within which the placental blood vessels (arteries and veins) form. In human placental cords the placental blood vessels are initially paired, later in development only a single placental vein remains with a pair of placental arteries. This structure also contains the allantois, an extension from the hindgut cloaca then urogenital sinus. Blood collected from the placental cord following delivery is a source of cord blood stem cells.)
- placental diameter - is measured in the transverse section by calculating the maximum dimensions of the chorionic surface.
- placental growth factor - (PlGF) A growth factor of the vascular endothelial growth factor (VEGF) family, released from the placental trophoblast cells and other sources that stimulates blood vessel growth.
- placental malaria - The malarial infection of the placenta by sequestration of the infected red blood cells. This condition can be common in regions where malaria is endemic with women carrying their first pregnancy (primigravida).
- placenta membranacea - rare placental abnormality characterized by the presence of chorionic villi directly attached to and covering the fetal membranes. Placenta Membranacea
- placenta previa - placenta overlies internal os of uterus, abnormal bleeding, may require cesarian delivery.
- placental thickness - is measured at its mid-portion from the chorionic plate to the basilar plate, on a longitudinal plane (less than 4 cm at term). Excludes any abnormalities (fibroids, myometrial contractions, or venous lakes). The placental thickness approximates in millimeters to the weeks of gestation.
- placental vein - (umbilical vein) In placental animals, the blood vessels which develop within the placental cord carrying relatively oxygenated blood from the placenta to the embryo/fetus. In humans, there are initially two placental veins which fuse to form a single vein. The resence of paired veins in the placental cord can be indicative of developmental abnormalities.
- placentophagia - Term used to descrbe the maternal ingestion of afterbirth materials (placental membranes and amniotic fluid) that can occur following mammalian parturition (birth).
- primary villi - (primary chorionic villi) Term describing the earliest stage of embryonic placenta development. In humans, the conceptus during week 2 this first stage of chorionic villi development consists of only the trophoblastic shell cells (syncitiotrophoblasts and cytotrophoblasts) forming finger-like extensions into maternal decidua. Initially these finger-like projections cover the entire surface of chorionic sac and later become restricted to the placental surface. The villi stages are ongoing as the placenta continues to grow through both the embryonic and fetal development.
- pre-eclampsia - During pregnancy a combination of high blood pressure, protein in urine and fluid retention resulting in maternal sudden excessive swelling of the face, hands and feet. Eclampsia is the subsequent development of convulsions, kidney failure, liver failure, clotting problems or mortality.
- Rh alloimmunization - feto-maternal haemorrhage generally in late pregnancy results in an Rh-negative woman becoming sensitised to Rh-positive fetal cells that enter her circulation. Clinically treated with anti-D immune globulin prophylaxis, alloimmunization occurs in 9–10% of at-risk pregnancies. immune
- secondary villi - (secondary chorionic villi) Term describing the second stage of embryonic placenta development. In humans, the conceptus during week 3 onward this stage of chorionic villi development consists of the trophoblastic shell cells (syncytiotrophoblast and cytotrophoblasts) filled with extraembryonic mesoderm forming finger-like extensions into maternal decidua. Initially these finger-like projections cover the entire surface of chorionic sac and later become restricted to the placental surface. The villi stages are ongoing as the placenta continues to grow through both the embryonic and fetal development. Placental villi stages: primary villi - secondary villi - tertiary villi
- syncytiotrophoblast - A multinucleated cell currently thought to form by the fusion of another trophoblast cell the cytotrophoblasts, within the trophoblast layer (shell) of the implanting conceptus. In early development, these cells mediate implantation of the conceptus into the uterine wall and secrete the hormone (Template:Human Chorionic Gonadotrophin, hCG) responsible for feedback maintainance of the corpus luteum (in maternal ovary) and therefore maintaining early pregnancy.
- trophoblast - (trophectoderm, Greek, trophe = "nutrition" and blast = a primordial cell) cells that firstly support adplantation, implantation and endocrine support of pregnancy. Contribute to the extraembryonic tissues, fetal placenta and membranes. Initially form 2 populations individual cytotrophoblast cells and their fused multinucleate syncytiotrophoblast cells.
- Twin-twin transfusion syndrome - (TTTS) in monozygotic twins with monochorionic and diamniotic placenta, with intrauterine blood transfusion from one twin (donor) to another twin (recipient) where there is an imbalance of blood flow from the donor twin to the recipient twin. Clinically diagnosed by the alternate presence of polyhydramnios in one fetus and oligohydramnios in the co-twin, occurs in about 10% of monochorionic twins.
- umbilical cord (placental cord) fetal attachment cord 1-2 cm diameter, 30-90cm long, covered with amniotic attached to chorionic plate, umbilical vessels (artery, vein) branch into chorionic vessels. Vessels anastomose within the placenta.
- umbilical vein varix - (fetal intra-abdominal umbilical vein varix, FIUV) focal dilatation of the umbilical venous diameter at the level of cord insertion, the dilatation diameter increases linearly with gestational age. Represent about 4% of umbilical cord abnormalities
with an incidence of about 2.8 per 1,000 pregnancies, there is also a rarer form of extra-abdominal varices. PMID 24883288
- vasculogenesis - formation of first blood vessels by differentiation of pluripotent mesenchymal cells (extraembryonic mesoderm) followed by angiogenesis which is the development of new vessels from already existing vessels.
- vasculosyncytial membranes - localised areas of the placental villous membrane where the barrier thickness separating maternal and fetal circulations is reduced to as little as 1-2 microns. PMID 1287078
- villi - Plural of villus, which is a thin projection from a surface. The term in development is used to describe the individual functional units together of the fetal placenta.
- virus - small infectious agents that may cross the placental barrier. Can infect embryo and/or placenta and cause developmental abnormalities. (e.g. cytomegalovirus, rubella, measles).
- Wharton's jelly - placental cord (umbilical cord) gelatinous connective tissue composed of myofibroblast-like stromal cells, collagen fibers, and proteoglycans. Increases in volume (myxomatous, connective tissue embedded in mucus) at parturition (birth) to assist closure of placental blood vessels. Matrix cells from Wharton's jelly have recently been identified as a potential source of mesenchymal stem cells (MSC), also called mesenchymal stromal cell. This placental cord substance is named after Thomas Wharton (1614-1673) an English physician and anatomist who first described this placental tissue.
|
Glossary Links
- Glossary: A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | Numbers | Symbols | Term Link
Cite this page: Hill, M.A. (2026, February 27) Embryology Abnormal Development - Ectopic Implantation. Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/Abnormal_Development_-_Ectopic_Implantation
- What Links Here?
- © Dr Mark Hill 2026, UNSW Embryology ISBN: 978 0 7334 2609 4 - UNSW CRICOS Provider Code No. 00098G