Genital System - Abnormalities
Introduction
How and why do things go wrong in development? Human genital abnormalities are currently described as "Disorders of Sex Development" (DSD) and includes: chromosomal, gonadal dysfunction, tract abnormalities, external genitalia and gonadal descent. The genital system is closely associated developmentally and anatomically with the renal system, often called the "urogenital system", therefore abnormalities of renal development should also be considered when studying this topic.
Note, the earlier term "intersex" and a variety of other previously applied terms related to genetic abnormalities have been replaced by the term "disorders of sex development" (DSD).
Some Recent Findings
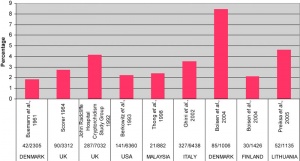
|
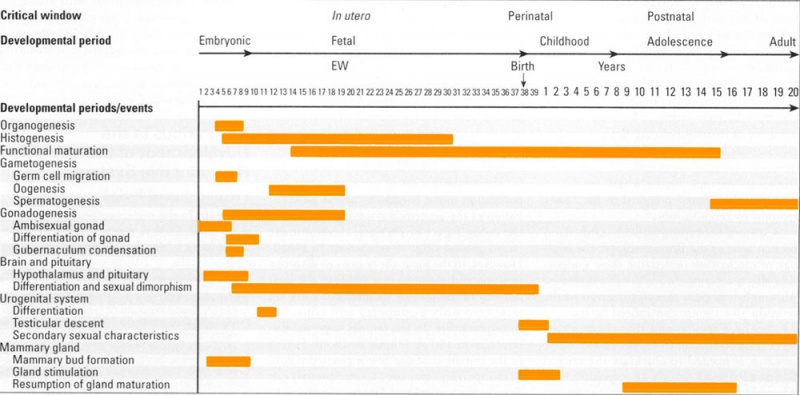
Human Genital Development Critical Periods
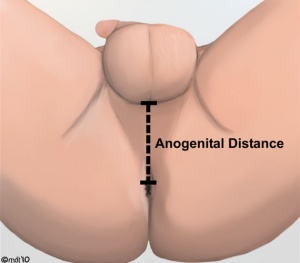
Anogenital Distance
Anogenital Distance (AGD) is a clinical measurement of a parameter that is sexually dimorphic for genital development. This distance, from the posterior aspect of the scrotum to the anal verge, has been used as a marker for endocrine disruption in animal studies and may also be shorter in infant males with genital anomalies (More? see related references)
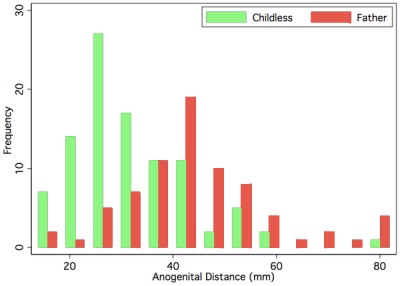
|
A recent study in humans has shown that infertile men possessed significantly shorter mean AGD than fertile men.[1]
|
Disorders of Sex Development
The previous human sex development terminology (true hermaphrodites, male pseudohermaphrodites and female pseudohermaphrodites) are considered outdated and stigmatising and have been replaced with the general term Disorders of Sex Development (DSD) established by the Consensus statement on management of intersex disorders.[4] See also the Medical Journal of Australia 2009 editorial article.[5]
| Previous Terminology | New Proposed Terminology |
| Intersex | DSD |
| Male pseudohermaphrodite, undervirilization of an XY male, and undermasculinization of an XY male | 46,XY DSD |
| Female pseudohermaphrodite, overvirilization of an XX female, and masculinization of an XX female | 46,XX DSD |
| True hermaphrodite | Ovotesticular DSD |
| XX male or XX sex reversal | 46,XX testicular DSD |
| XY sex reversal | 46,XY complete gonadal dysgenesis |
Congenital Adrenal Hyperplasia
- impairment of cortisol production by the adrenal cortex, is one of the most common causes of intersex genitalia at birth
- genetically male (XY) infants born with undervirilized genitalia (androgen insensitivity syndrome, cloacal exstrophy) are generally assigned and reared as girls.
Congenital adrenal hyperplasia due to 21-hydroxylase deficiency can be prenatally diagnosed in utero through molecular genetic analysis of fetal DNA. Prenatal treatment by dexamethasone administration to the at-risk pregnant mother has been shown to be effective in reducing genital virilization in the fetus, avoiding unnecessary postnatal genitoplasty in affected females.[6]
There has been recorded a prevalence of reduced fecundity in men with congenital adrenal hyperplasia, related to testicular adrenal rest tumours and poor semen parameters.[7]
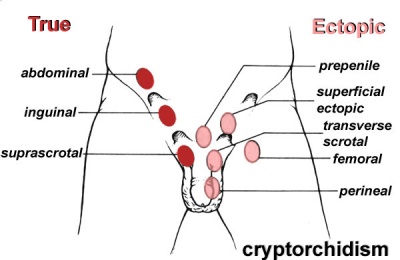
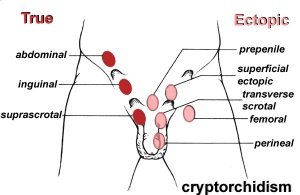
Cryptorchidism
- abnormality of either unilateral or bilateral testicular descent, occurring in up to 30% premature and 3-4% term males.
- Descent may complete postnatally in the first year, failure to descend can result in sterility.
Testis descent is thought to have 2 phases:
- transabdominal descent - dependent on insulin-like hormone 3 (INSL3).
- inguinoscrotal descent - dependent on androgens.
Management of cryptorchidism in children: guidelines.[9] "Cryptorchidism is best diagnosed clinically, and treated by surgical orchiopexy at age 6-12 months, without a routine biopsy. If no testis is palpable, or if other signs of hypovirilisation such as hypospadias are present, the chromosomal sex and hormonal status must be assessed. Laparoscopy is the best way of diagnosing and managing intra-abdominal testes."
Undescended Ovaries
- reasonably rare gonad abnormality, often detected following clinical assessment of fertility problems and may also be associated with other uterine malformations (unicornuate uterus).
- Due to the relative positions of the male (external) and female (internal) gonads and the pathways for their movement, failure of gonad descent is more apparent and common in male cryptorchidism than female undescended ovaries.
Hydrocele
- Male Hydrocele is a fluid-filled cavity of either testis or spermatic cord, where peritoneal fluid passes into a patent processus vaginalis.
- Female Hydrocele is a similar, but rarer, fluid-filled cavity occuring in the female as a pouch of peritoneum extending into the labium majorum (canal of Nuck).
Tract Abnormalities
Many different forms
- Uterine: associated with other anomolies, unicornuate uterus
- Vagina: agenesis, atresia
- Ductus Deferens: Unilateral or bilateral absence, failure of mesonephric duct to differentiate
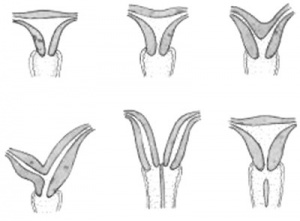
Uterine Duplication (uterus didelphys, double uterus, uterus didelphis) A rare uterine developmental abnormality where the paramesonephric ducts (Mullerian ducts) completely fail to fuse generating two separate uterus parts each connected to the cervix and having an ovary each.
Septate Uterus
Cervical: cervical agenesis, cervical duplication
Vaginal: Mayer-Rokitansky syndrome (MRK anomaly, Rokitansky-Küster-Hauser syndrome, RKH syndrome, RKH) congenital absence of the vagina, dyspareunia, vaginal agenesis.
Polycystic Ovary Syndrome
(PCOS) or Stein–Leventhal syndrome (1930s researchers) a metabolic syndrome with many other symptoms, ovarian cysts arise through incomplete follicular development or failure of ovulation. For review see [10]
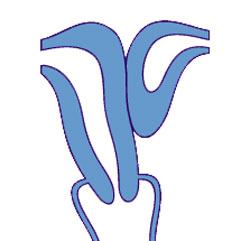
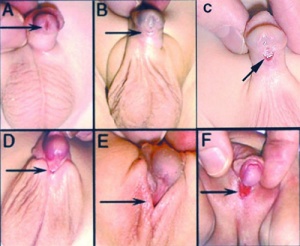
Hypospadia
Hypospadias are the most common penis abnormality (1 in 300) and result from a failure of male urogenital folds to fuse in various regions. This in turn leads to resulting in a proximally displaced urethral meatus. The cause is unknown, but suggested to involve many factors either indivdually or in combination including: familial inheritance, low birth weight, assisted reproductive technology, advanced maternal age, paternal subfertility and endocrine-disrupting chemicals.[11] Maternal hypertension during pregnancy has also been shown to double the risk and a pregnancy diet lacking meat and fish also show an increase in hypospadias.[12] Infants with hypospadias should not undergo circumcision.
| Hypospadia Classification | Meatus Opening |
| Anterior | on inferior surface of glans penis |
| Coronal | in balanopenile furrow |
| Distal | on distal third of shaft |
| Penoscrotal | at base of shaft in front of scrotum |
| Scrotal | on scrotum or between the genital swellings |
| Perineal | behind scrotum or genital swellings |
Surgical Repair
Depending on the class of hypospadias there are a number of different surgical repair techniques including: orthoplasty or penile straightening, urethroplasty, meatoplasty and glanuloplasty, scrotoplasty (oscheoplasty) and skin coverage.
Related Genetic Conditions
- Johanson-Blizzard syndrome[13] - hypospadias, failure to thrive, exocrine pancreatic deficiency, short stature and developmental delay, cutis aplasia on the scalp, aplasia of alae nasi, hypothyroidism, myxomatous mitral valve, and patent ductus arteriosus.
Splenogonadal Fusion
Rare abnormality resulting from fusion of the splenic and gonadal primordia during prenatal development.[14] On the left side and more common in male and adhesion to the gonad, epididymis or ductus deferens and then follows the caudal descent with the gonad. Failure of complete descent can also result in associated intraabdominal cryptorchism.
Two classifications:
- continuous - orthotopic spleen connects to the gonad with a cord of fibrous or splenic tissue.
- discontinuous - no connection between the orthotopic spleen and gonad.
- Links: Spleen Development
References
- ↑ 1.0 1.1 [Eisenberg ML, Hsieh MH, Walters RC, Krasnow R, Lipshultz LI. The Relationship between Anogenital Distance, Fatherhood, and Fertility in Adult Men. PLoS One. 2011 May 11;6(5):e18973. PMID:21589916 | PMC3092750 | PLoS One.
- ↑ <pubmed>20501980</pubmed>
- ↑ <pubmed>20503482</pubmed>
- ↑ <pubmed>16882788</pubmed>| Pediatrics.
- ↑ <pubmed>19485836</pubmed>| Med J Aust.
- ↑ <pubmed>19101608</pubmed>
- ↑ <pubmed>19258407</pubmed>| J Clin Endocrinol Metab.
- ↑ <pubmed>18032558</pubmed>| Hum Reprod Update.
- ↑ <pubmed>18726735</pubmed>
- ↑ <pubmed>14748678</pubmed>
- ↑ <pubmed>11713004</pubmed>
- ↑ <pubmed>18709149</pubmed>| PMC2516569
- ↑ <pubmed>20556423</pubmed>
- ↑ <pubmed>2191479</pubmed>
Reviews
Ostrer, H. GeneReviews Pagon RA, Bird TD, Dolan CR, et al., editors. Seattle (WA): University of Washington, Seattle; 1993-46,XY Disorder of Sex Development and 46,XY Complete Gonadal Dysgenesis
Articles
<pubmed>21525798</pubmed>
Search Pubmed
Search Pubmed: Genital System Abnormalities | Disorders of Sex Development | Hypospadia
External Links
External Links Notice - The dynamic nature of the internet may mean that some of these listed links may no longer function. If the link no longer works search the web with the link text or name. Links to any external commercial sites are provided for information purposes only and should never be considered an endorsement. UNSW Embryology is provided as an educational resource with no clinical information or commercial affiliation.
- DSD Consortium Guidelines | Handbook for Parents
- EuroDSD EuroDSD programme is a collaboration of doctors and scientists from all over Europe. Long-term outcome studies on the various DSD entities are desperately needed in order to establish a basis for evidence-based medicine regarding sex assignment and conservative and surgical treatment options.
- German DSD network
- Italian registry for DSD
- UK
- Intersex Society of North America
- Turner Syndrome Society of the U.S.
| Abnormality Links: abnormal development | abnormal genetic | abnormal environmental | Unknown | teratogens | ectopic pregnancy | cardiovascular abnormalities | coelom abnormalities | endocrine abnormalities | gastrointestinal abnormalities | genital abnormalities | head abnormalities | integumentary abnormalities | musculoskeletal abnormalities | limb abnormalities | neural abnormalities | neural crest abnormalities | placenta abnormalities | renal abnormalities | respiratory abnormalities | hearing abnormalities | vision abnormalities | twinning | Developmental Origins of Health and Disease | ICD-11 | ||
|
Glossary Links
- Glossary: A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | Numbers | Symbols | Term Link
Cite this page: Hill, M.A. (2024, April 28) Embryology Genital System - Abnormalities. Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/Genital_System_-_Abnormalities
- © Dr Mark Hill 2024, UNSW Embryology ISBN: 978 0 7334 2609 4 - UNSW CRICOS Provider Code No. 00098G