Sandbox: Difference between revisions
mNo edit summary |
mNo edit summary |
||
| Line 1: | Line 1: | ||
''A draft page designed to be used only for testing.'' | ''A draft page designed to be used only for testing.'' | ||
[[File:SHsmall.jpg]] | |||
==Introduction== | |||
[[Image:Mark Hill.jpg|100px|left]] | |||
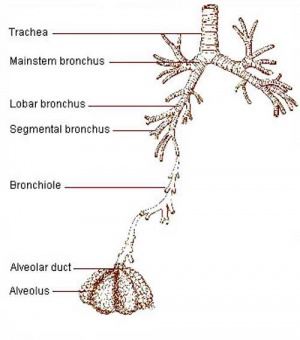
[[File:Respiratory tract.jpg|thumb|300px|Respiratory tract]] | |||
The lecture will introduce the development of the respiratory system and associated structures. The lecture '''will not cover''' adult anatomy, physiology of gas exchange, red blood cell function, cardiovascular development and will leave detailed histology to your associated practical class. | |||
:''Research suggests that in addition to genetic effects that the developmental environment (both fetal and postnatal) can influence the growth, differentiation and function of this system.'' | |||
'''Lecture currently being updated for 2014.''' | |||
[[ | Start Time/End Time: 10am to 11am Monday 10 March 2014 Clancy Auditorium [[Media:SH Lecture 2013 - Respiratory System Development.pdf|2013 Lecture Slides PDF]] | ||
:'''Lecture:''' [[Media:SH Lecture 2013 - Respiratory System Development.pdf|Lecture 2013 PDF]] | [http://embryology.med.unsw.edu.au/embryology/index.php?title=SH_Lecture_-_Respiratory_System_Development&oldid=119314 2013] | [http://php.med.unsw.edu.au/embryology/index.php?title=SH_Lecture_-_Respiratory_System_Development&oldid=98850 2012] | [[Media:SH Lecture - Respiratory System Development 2012.pdf|2012 PDF (10 pages)]] | [http://emed.med.unsw.edu.au/Map.nsf/0/6FF17DFEF645DABACA2573390006292A?OpenDocument&login eMed Link to Learning Activity - Respiratory System Development] | |||
{ | {{SH2011}} | ||
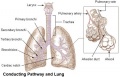
The respiratory system does not carry out its physiological function (of gas exchange) until after birth, though the respiratory tract, diaphragm and lungs do begin to form early in embryonic development and continue through fetal development, only functionally maturing just before birth. The lungs continue to grow postnatally through childhood and some research finding suggest that there remains potential for growth in the adult. | |||
The respiratory tract is divided anatomically into 2 main parts: | |||
# '''upper respiratory tract''' - consisting of the nose, nasal cavity and the pharynx. | |||
# '''lower respiratory tract''' - consisting of the larynx, trachea, bronchi and the lungs. | |||
The respiratory "system" usually includes descriptions of not only the functional development of the lungs, but also related musculoskeletal (diaphragm) and vascular (pulmonary) development. | |||
===Aims=== | |||
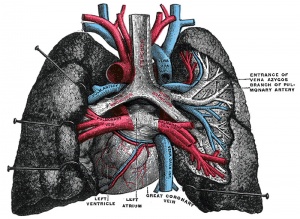
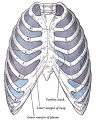
[[File:Gray0971.jpg|thumb|adult lungs]] | |||
To understand the prenatal and postnatal developmental anatomy of human respiratory organs. | |||
===Key Concepts=== | |||
# | # Embryonic origin of respiratory components (tract, lungs, diaphragm, muscles) | ||
# | # Key stages in respiratory development. | ||
# Time course of respiratory development. | |||
# Respiration at birth. | |||
# Postnatal development of respiration. | |||
# Developmental abnormalities. | |||
==Textbooks== | |||
{| | |||
|- | |||
| [[File:Logo.png|80px]] | |||
| {{Embryo citation}} | |||
{{Respiratory Links}} | |||
|- | |||
| [[File:Larsen's human embryology 4th edn.jpg|80px]] | |||
| Schoenwolf, G.C., Bleyl, S.B., Brauer, P.R. and Francis-West, P.H. (2009). <i>Larsen’s Human Embryology</i> (4<sup>th</sup> ed.). New York; Edinburgh: Churchill Livingstone. | |||
* [http://www.mdconsult.com/books/linkTo?type=bookPage&isbn=978-0-443-06811-9&eid=4-u1.0-B978-0-443-06811-9..10011-9 Chapter 11 - Development of the Respiratory System and Body Cavities] (chapter links only work with a UNSW connection). | |||
|- | |||
| [[File:The Developing Human, 8th edn.jpg|80px]] | |||
| Moore, K.L. & Persuad, T.V.N. (2008). <i>The Developing Human: clinically oriented embryology</i> (8<sup>th</sup> ed.). Philadelphia: Saunders. | |||
* [http://www.mdconsult.com/books/linkTo?type=bookPage&isbn=978-1-4160-3706-4&eid=4-u1.0-B978-1-4160-3706-4..50013-X Chapter 10 - The Respiratory System] (seem to no longer have UNSW connection?). | |||
|} | |||
{| class="wikitable collapsible collapsed" | {| class="wikitable collapsible collapsed" | ||
! | ! Additional Textbooks | ||
|- | |- | ||
| | | | ||
* Before We Are Born (5th ed.) Moore and Persaud Chapter 13 p255-287 | |||
* Essentials of Human Embryology Larson Chapter 9 p123-146 | |||
* Human Embryology Fitzgerald and Fitzgerald Chapter 19,20 p119-123 | |||
* Developmental Biology 8e Online[http://8e.devbio.com/article.php?ch=15&id=157 Lung Branching Morphogenesis] | |||
* [http://www.lab.anhb.uwa.edu.au/mb140/CorePages/Respiratory/respir.htm Blue Histology - Respiratory] | |||
|} | |||
{ | {| class="wikitable collapsible collapsed" | ||
! Audio | |||
|- | |||
| '''Lectopia Lecture Audio''' [[File:Podcast_icon.jpg|link=ANAT2341_Embryology_2011_Lecture_Recordings]] | [http://lectopia.telt.unsw.edu.au/lectopia/lectopia.lasso?ut=153&id=110475 Science Respiratory Lecture 2011] | |||
|} | |} | ||
== | ==Respiratory Functional Unit == | ||
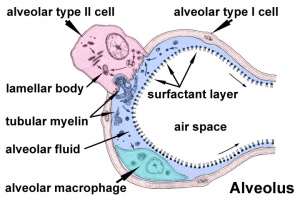
'''Alveolus''' (Latin ''alveolus'' = "little cavity", plural is alveoli) | |||
{| | {| | ||
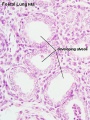
| [[File: | | [[File:Alveolar-sac-01.jpg|300px]] | ||
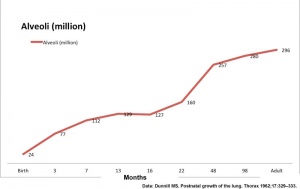
| [[File: | | [[File:Postnatal_alveoli_number.jpg|300px]] | ||
|- | |- | ||
| | | The alveoli cellular structure | ||
| Increase in human alveoli number | |||
| | |- | ||
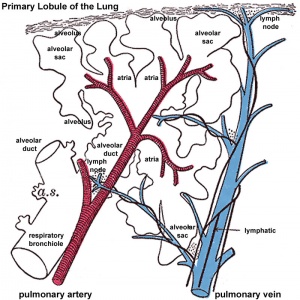
| [[File:Lung_primary_lobule_01.jpg|300px]] | |||
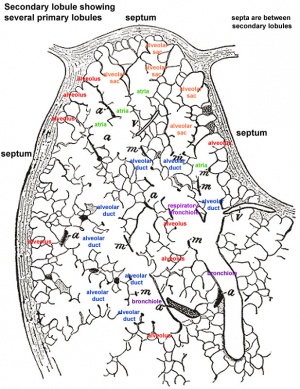
| [[File:Lung_secondary_lobule_01.jpg|300px]] | |||
|- | |||
| Alveoli and blood vessels | |||
| Lung structure | |||
|} | |} | ||
== | ==Developmental Overview== | ||
[[File:Stage14 respiratory tract.jpg|thumb|Week 5 Respiratory Development]] | |||
Germ Layers | |||
* Endoderm and splanchnic mesoderm form majority of conducting and alveoli. | |||
* Ectoderm will contribute the neural innervation. | |||
* Mesoderm also contributes the supporting musculoskeletal components. | |||
{| | {| | ||
| | | [[File:Bailey287.jpg|200px]] | ||
| | | [[File:Bailey288.jpg|200px]] | ||
| [[File:Bailey289.jpg|200px]] | |||
|- | |- | ||
| | | Week 4-5 (Stage [[Carnegie_stage_12|12]] to [[Carnegie_stage_13|13]]) | ||
| Week 5 (Stage [[Carnegie_stage_15|15]] to [[Carnegie_stage_16|16]]) | |||
| Week 6 (Stage [[Carnegie_stage_16|16]] to [[Carnegie_stage_17|17]]) | |||
| | |||
|} | |} | ||
'''Week 4''' - laryngotracheal groove forms on floor foregut. | |||
'''Week 5''' - left and right lung buds push into the pericardioperitoneal canals (primordia of pleural cavity) | |||
'''Week 6''' - descent of heart and lungs into thorax. Pleuroperitoneal foramen closes. | |||
'''Week 7''' - enlargement of liver stops descent of heart and lungs. | |||
'''Month 3-6''' - lungs appear glandular, end month 6 alveolar cells type 2 appear and begin to secrete surfactant. | |||
'''Month 7''' - respiratory bronchioles proliferate and end in alveolar ducts and sacs. | |||
==Development Stages== | |||
Note - the sequence is important rather than the actual timing, which is variable in the existing literature. | |||
{{lung stage table}} | |||
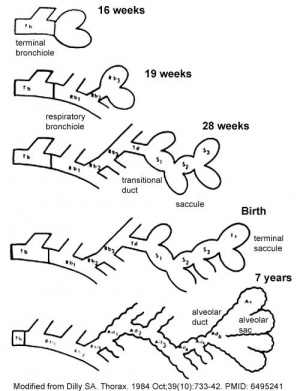
''' | [[File:Lung_alveoli_development_cartoon.jpg|thumb|300px]] | ||
===Embryonic=== | |||
* '''week 4 - 5''' | |||
* Endoderm - tubular ventral growth from foregut pharynx. | |||
* Mesoderm - mesenchyme of lung buds. | |||
* Intraembryonic coelom - pleural cavities elongated spaces connecting pericardial and peritoneal spaces. | |||
===Pseudoglandular stage=== | |||
* '''week 5 - 17''' | |||
* tubular branching of the human lung airways continues | |||
* by 2 months all segmental bronchi are present. | |||
* lungs have appearance of a glandlike structure. | |||
* stage is critical for the formation of all conducting airways. | |||
** lined with '''tall columnar epithelium''' | |||
** more distal structures are lined with '''cuboidal epithelium'''. | |||
===Canalicular stage=== | |||
* '''week 16 - 24''' | |||
* Lung morphology changes dramatically | |||
* differentiation of the pulmonary epithelium results in the formation of the future air-blood tissue barrier. | |||
* '''Surfactant''' synthesis and the canalization of the lung parenchyma by capillaries begin. | |||
* future gas exchange regions can be distinguished from the future conducting airways of the lungs. | |||
===Saccular stage=== | |||
[[File:Alveolar-sac-01.jpg|thumb|300px|Alveolar sac structure]] | |||
* '''week 24 to near term.''' | |||
* most peripheral airways form widened "airspaces", termed '''saccules'''. | |||
* saccules widen and lengthen the airspace (by the addition of new generations). | |||
* future gas exchange region expands significantly. | |||
* Fibroblastic cells also undergo differentiation, they produce extracellular matrix, collagen, and elastin. | |||
** May have a role in epithelial differentiation and control of '''surfactant secretion'''. | |||
* Alveolar Cells Type II (Type II pneumocytes) | |||
** begin to secrete '''surfactant''', levels of secretion gradually increase to term. | |||
** allows alveoli to remain inflated | |||
* Vascular tree - also grows in length and diameter during this time. | |||
* | ===Alveolar stage=== | ||
* late fetal to 8 years. | |||
* The postnatal lung, with '''alveoli''' forming. | |||
* Expansion of gas exchange alveoli, vascular beds (capillaries), lymphatics and innervation. | |||
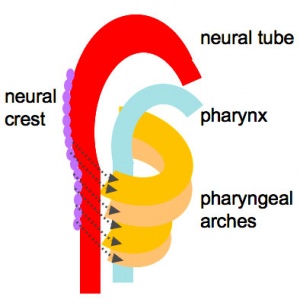
==Foregut Development== | |||
[[File:Head arches cartoon.jpg|thumb|Foregut cartoon]] | |||
From the oral cavity the next portion of the foregut is initially a single gastrointestinal (oesophagus) and respiratory (trachea) common tube, the pharynx which lies behind the heart. Note that the respiratory tract will form from a ventral bud arising at this level. | |||
* Oral cavity | |||
* Pharynx (esophagus, trachea) | |||
* Respiratory tract | |||
* Stomach | |||
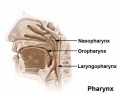
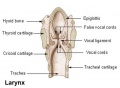
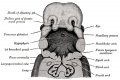
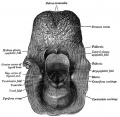
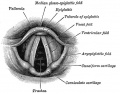
==Upper Respiratory Tract== | |||
[[File:Gray0961.jpg|thumb|Adult upper respiratory tract conducting system]] | |||
<gallery> | |||
File:Pharynx_cartoon.jpg|Pharynx | |||
File:Nasal cavities.jpg|Nasal cavities | |||
File:Pharynx.jpg|Pharynx | |||
File:Larynx.jpg|Larynx | |||
</gallery> | |||
* part of foregut development | |||
* anatomically the nose, nasal cavity and the pharynx | |||
* the pharynx forms a major arched cavity within the pharyngeal arches ('''MH''' - pharyngeal arches will be described in BGD head development lecture). | |||
{| class="wikitable collapsible collapsed" | |||
! Additional Information - Histology | |||
|- | |||
| This will be covered in detail in your associated SH Practical class. | |||
<gallery> | |||
File:Respiratory histology 13.jpg|Olfactory Epithelium | |||
File:Respiratory histology 14.jpg|Olfactory Epithelium | |||
File:Respiratory histology 11.jpg|Respiratory Epithelium | |||
File:Respiratory histology 12.jpg|Respiratory Epithelium | |||
</gallery> | |||
{| | |||
|- | |||
| valign=top width=380px|'''Olfactory epithelium''' | |||
* Olfactory cells | |||
* Sustentacular cells - located mainly in the superficial cell layer of the epithelium (difficult to distinguish from olfactory cells). | |||
* Basal cells - identified by their location in the epithelium. | |||
'''Epithelium''' | |||
* Cilia are not visible | |||
* goblet cells are absent from the olfactory epithelium. | |||
'''Lamina Propria''' | |||
* olfactory axon bundles (lightly stained, rounded areas) connected to olfactory cells. | |||
* Bowman's glands - (small mucous glands, olfactory glands) function to moisturise the epithelium. | |||
{{Nasal olfactory links}} | |||
{ | |||
| valign=top width=380px|'''Respiratory epithelium''' | |||
* goblet cells | |||
* ciliated cells | |||
* basal cells | |||
'''Lamina propria''' | |||
* connective tissue | |||
* cavernous sinusoids - large spaces (empty or filled with red blood cells) | |||
* glandular tissue - mucous glands (green) and muco-serous glands (brownish-green) | |||
'''Bone''' | |||
* Lamellae and osteocytes in lacunae. | |||
* Haversian systems are rare or absent. | |||
{{Nasal respiratory links}} | |||
|} | |||
{{Respiratory Histology}} | |||
|} | |} | ||
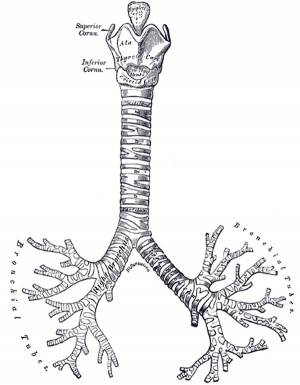
==Lower Respiratory Tract== | |||
<gallery> | |||
File:Gray0982a.jpg|week 4 early respiratory endodermal bud | |||
File:Gray0982b.jpg|week 4 later ventral endoderm growth | |||
File:Bronchi lungs.jpg|lower respiratory tract | |||
File:Respiratory tract.jpg|conducting system bronchi to lungs | |||
</gallery> | |||
{| | |||
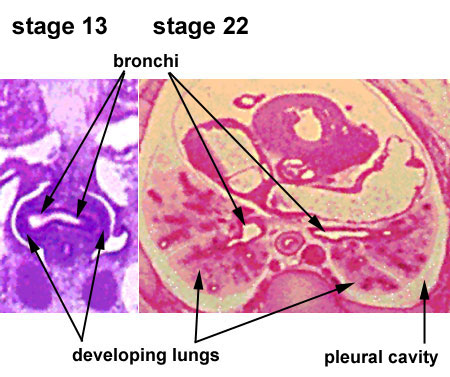
| [[File:Lung_development_stage13-22.jpg]] | |||
| [[File:Stage_22_image_171.jpg|300px]] | |||
|- | |||
| [[Respiratory_System_-_Carnegie_Stage_13|Stage 13 (Week 4-5)]] | |||
| [[Respiratory_System_-_Carnegie_Stage_22|Stage 22 (Week 8)]] | |||
|} | |||
[[File:Lung alveoli development cartoon.jpg|thumb|Lung alveoli development cartoon]] | |||
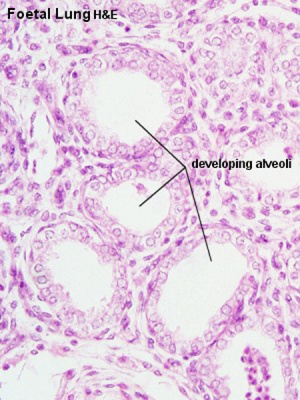
[[File: | [[File:Fetal lung histology.jpg|thumb|Fetal lung histology]] | ||
* | * lung buds ( endoderm epithelial tubes) grow/push into mesenchyme covered with pleural cells (lung border) | ||
* | * generates a tree-like network by repeated: | ||
# elongation | |||
# terminal bifurcation | |||
# lateral budding | |||
Growth initially of branched "conducting" system of bronchial tree, followed by later development of the "functional units" of the alveoli. | |||
{| class="wikitable collapsible collapsed" | |||
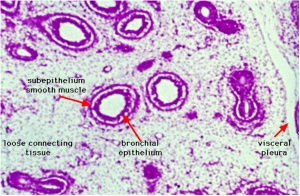
! Additional Information - Histology | |||
|- | |||
| This will be covered in detail in your associated SH Practical class. | |||
'''Respiratory Trachea''' | |||
'''Mucosa''' - formed by epithelium and underlying lamina propria. | |||
* | * respiratory epithelium - (pseudostratified columnar and ciliated) ciliated cells, goblet cells, brush cells, endocrine cells, surfactant-producing cells (Clara cells), serous cells, basal cells, basement membrane. | ||
* | * lamina propria - loose connective tissue, many elastic fibres | ||
'''Submucosa''' - connective tissue and submucosal glands | |||
* submucosal glands (both serous and mucous parts) | |||
* | |||
'''Cartilage''' | |||
* | * perichondrium | ||
* | * tracheal cartilage - hyaline cartilage, 16 to 20 C-shaped cartilages. | ||
* trachealis muscle - (smooth muscle) Not visible in this section, together with connective tissue fibres, join ends of the cartilages together. | |||
'''Hyaline Cartilage Development''' | |||
* forms from mesenchymal cells. | |||
* precursor cells become rounded and form densely packed cellular masses, chondrification centres. | |||
* chondroblasts - (cartilage-forming cells) begin secreting the extracellular matrix components of cartilage. | |||
** extracellular matrix - ground substance (hyaluronan, chondroitin sulfates and keratan sulfate) and tropocollagen (polymerises into fine collagen fibres, not visible). | |||
<gallery> | |||
File:Hyaline_cartilage_03.jpg|Trachea (overview HE) | |||
File:Hyaline_cartilage_04.jpg|Trachea (overview VG) | |||
File:Respiratory histology 05.jpg|Trachea (detail layers) | |||
File:Respiratory histology 06.jpg|Trachea (detail glands) | |||
</gallery> | |||
'''Bronchi Branching''' | |||
main bronchi -> lobar bronchi -> segmental bronchi (supply lung bronchopulmonary segments) -> bronchi -> bronchioles (smaller than 1 mm) -> '''respiratory bronchioles'''. | |||
* Trachea branches into 2 '''main bronchi''', with a histological structure similar to that of the trachea. | |||
* branches are accompanied by branches of the pulmonary artery, nerves and lymph vessels | |||
* surrounded by a layer of smooth muscle, which is located between the cartilage and epithelium. | |||
* the | '''Bronchioles''' | ||
* transition from bronchi to bronchioles the epithelium changes to a '''ciliated columnar epithelium'''. | |||
* | * Smooth muscle present, glands and cartilage are absent. | ||
'''Respiratory Bronchioles''' | |||
* first structures that belong to the respiratory portion of the respiratory system. | |||
* | * wall out-pouchings form alveoli (site of gas exchange) | ||
* | * end in alveolar ducts | ||
* alveoli - duct or sac. | |||
<gallery> | |||
File:Respiratory_histology_01.jpg|Bronchiole | |||
File:Respiratory histology 10.jpg|Lung Elastin | |||
File:Respiratory histology 08.jpg|labeled lung | |||
</gallery> | |||
{| | {| | ||
|- | |- | ||
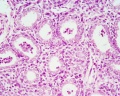
| | | valign=top width=350px|'''Alveolar type I cells''' | ||
* small alveolar cells or type I pneumocytes | |||
* are extremely flattened (the cell may be as thin as 0.05 µm) | |||
* form the bulk (95%) of the surface of the alveolar walls. | |||
* The shape of the cells is very complex, and they may actually form part of the epithelium on both faces of the alveolar wall. | |||
| valign=top width=350px|'''Alveolar type II cells''' | |||
* large alveolar cells or type II pneumocytes | |||
* | * about as many type II cells as type I cells (cell shape accounts for small contribution to alveolar area). | ||
* | * irregularly (sometimes cuboidal) shaped. | ||
* form small bulges on the alveolar walls. | |||
* contain are large number of granules called cytosomes (or multilamellar bodies) | |||
** consist of precursors to pulmonary surfactant (mixture of phospholipids that keep surface tension in the alveoli low). | |||
|} | |} | ||
<gallery> | <gallery> | ||
File: | File:Respiratory_histology_02.jpg|Alveolar Duct | ||
File: | File:Respiratory_histology_03.jpg|Alveoli | ||
File: | File:Respiratory histology 04.jpg|Alveoli Elastin | ||
</gallery> | </gallery> | ||
{{Respiratory Histology}} | |||
|} | |||
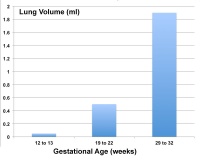
===Fetal Lung Volume=== | |||
Each human lung volume as determined by ultrasound and matched to gestational age <ref><pubmed>16388511</pubmed></ref> | |||
{| | {| | ||
| | | | ||
{| | |||
|-bgcolor="CEDFF2" | |||
| Weeks (gestational) | |||
| Volume (ml) | |||
|- | |||
| 12 to 13 | |||
| 0.05 | |||
|-bgcolor="F5FAFF" | |||
| 19 to 22 | |||
| 0.5 | |||
|- | |||
| 29 to 32 | |||
| 1.9 | |||
|} | |||
| [[File:Lung volume graph 01.jpg|200px]] | |||
|} | |||
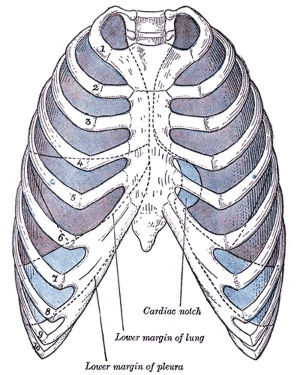
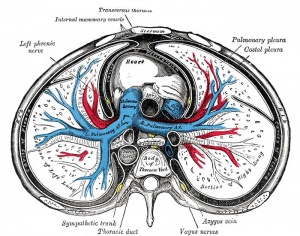
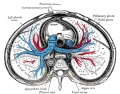
== Pleural Cavity == | |||
[[File:Gray0965.jpg|thumb|pleura]] | |||
[[File:Gray0968.jpg|thumb|pleura]] | |||
* anatomical body cavity in which the lungs develop and lie. | |||
* pleural cavity forms in the '''lateral plate mesoderm''' as part of the early single '''intraembryonic coelom'''. | |||
* This cavity is initially continuous with pericardial and peritoneal cavities and form initially as two narrow canals. | |||
** later becomes separated by folding (pleuropericardial fold, pleuroperitoneal membrane) and the later formation of the diaphragm. | |||
* '''pleuropericardial fold''' - (pleuropericardial membrane) An early embryonic fold which restricts the communication between pleural cavity and pericardiac cavity, contains both the cardinal vein and phrenic nerve. | |||
* '''pleuroperitoneal membrane''' - An early embryonic membrane that forms inferiorly at the septum transversum to separate peritoneal cavity from pleural cavity. | |||
===Pleura=== | |||
* '''serous membrane''' covers the surface of the lung and the spaces between the lobes. | |||
* arranged as a closed invaginated sac. | |||
* two layers ('''pulmonary''', '''parietal''') continuous with each other, the potential space between them is the '''pleural cavity'''. | |||
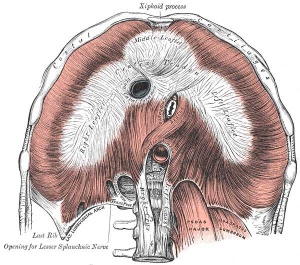
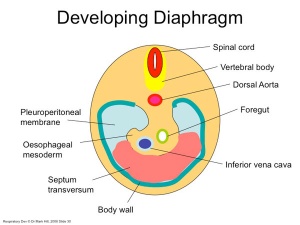
==Diaphragm== | |||
* Not respiratory tract but musculoskeletal development, there are '''5 embryonic elements''' that contribute to the diaphragm. | |||
{| | |||
| [[File:Diaphragm components.jpg|300px|Components of the diaphragm]] | |||
| | |||
# septum transversum- central tendon | |||
# 3rd to 5th somite- musculature of diaphragm | |||
# ventral pleural sac- connective tissue | |||
# mesentry of oesophagus- connective tissue around oesophasus and IVC | |||
# pleuroperitoneal membranes- connective tissue around central tendon | |||
|} | |} | ||
[[File:Gray804.gif|thumb|Adult Cervical Plexus (phrenic nerve shown lower right)]] | |||
[[File:Gray0391.jpg|300px|adult diaphragm]] | |||
''' | * Innervation of the human diaphragm is by the '''phrenic nerves''' | ||
** arising from the same segmental levels from which the diaphragm skeletal muscles arise, segmental levels C3 to C5. | |||
* The paired phrenic nerves are '''mixed nerves''' | |||
** motor neurons for the diaphragm | |||
** sensory nerves for other abdominal structures (mediastinum, pleura, liver, gall bladder). | |||
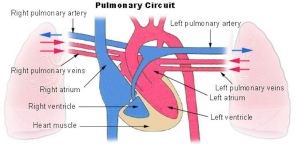
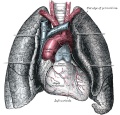
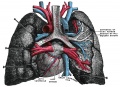
==Pulmonary Circulation== | |||
[[File:Pulmonary circulation cartoon.jpg|thumb|300px|Pulmonary circulation]] | |||
* the pulmonary system not "functional" until after birth | |||
* pulmonary arteries - 6th aortic arch arteries | |||
* pulmonary veins - are incorporated into the left atrium wall | |||
* bronchial arteries - branches from dorsal aorta | |||
== | ==Fetal== | ||
===Fetal Respiratory Movements=== | |||
* Fetal respiratory movements (FRM) or Fetal breathing movements (FBM) are regular muscular contrations occurring in the third trimester. | |||
* preparing the respiratory muscular system for neonatal function. | |||
* may also have a role in late lung development. | |||
[[File: | ==The First Breath== | ||
[[File:Alveolar-sac-01.jpg|thumb|Alveolar sac structure]] | |||
* | * The respiratory system does not carry out its physiological function (gas exchange) prenatally and remain entirely fluid-filled until birth. | ||
* At birth, fluid in the upper respiratory tract is expired and fluid in the lung aveoli is rapidly absorbed this event has also been called "dewatering of the lung". | |||
** The lung epithelia has to now rapidly change from its prenatal secretory function to that of fluid absorbtion. | |||
** | |||
The exchange of lung fluid for air leads to: | |||
* fall in pulmonary vascular resistance | |||
* increase in pulmonary blood flow | |||
* thinning of pulmonary arteries (stretching as lungs increase in size) | |||
* blood fills the alveolar capillaries | |||
In the heart - pressure in the right side of the heart decreases and pressure in the left side of the heart increases (more blood returning from pulmonary). | |||
==Postnatal== | |||
[[File:Postnatal alveoli number.jpg|thumb|300px|Postnatal alveoli number]] | |||
[[File:Neonatal rib orientation.jpg|thumb|Rib orientation]] | |||
===Alveoli=== | |||
* At birth about 15% of adult alveoli number have formed | |||
** 20 - 50 million to in the adult about 300 million. | |||
* remaining subdivisions develop in the first few postnatal years | |||
* | |||
** | |||
* | |||
[[:File:Postnatal_alveoli_number.jpg|Alveoli Number]] | |||
===Respiratory Rate=== | |||
* neonatal rate is higher (30-60 breaths/minute) than adult (12-20 breaths/minute). | |||
** tachypnea - (Greek, rapid breathing) an increased respiratory rate of greater than 60 breaths/minute in a quiet resting baby | |||
{| | {| | ||
| | |-bgcolor="CEDFF2" | ||
| width= "300px"|'''Age''' | |||
| width= "200px"|'''Rate''' (breaths/minute) | |||
|- | |||
| Infant (birth - 1 year) | |||
| 30 - 60 | |||
|- bgcolor="F5FAFF" | |||
| Toddler (1 - 3 years) | |||
| 24 - 40 | |||
|- | |||
| Preschool (3 - 6 years) | |||
| 22 - 34 | |||
|-bgcolor="F5FAFF" | |||
| School age (6 - 12 years) | |||
| 18 - 30 | |||
|- | |||
| Adolescent (12 - 18 years) | |||
| 12 - 16 | |||
|-bgcolor="F5FAFF" | |||
| | | | ||
|} | |||
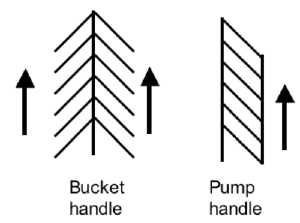
===Rib Orientation=== | |||
* Infant rib - is virtually '''horizontal''', allowing diaphragmatic breathing only. | |||
* Adult rib - is '''oblique''' (both anterior and lateral views), allows for pump-handle and bucket handle types of inspiration. | |||
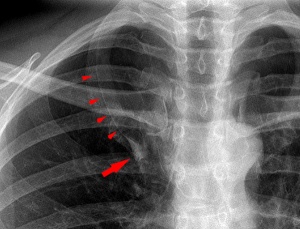
== Respiratory Tract Abnormalities == | |||
| | [[File:Lung_Azygos_Lobe_02.jpg|thumb|Lung Azygos Lobe]] | ||
[[Respiratory System - Abnormalities]] | |||
* '''Meconium Aspiration Syndrome''' - (MAS) Meconium is the gastrointestinal contents that accumulate in the intestines during the fetal period. Fetal stress in the third trimester, prior to/at/ or during parturition can lead to premature meconium discharge into the amniotic fluid and sunsequent ingestion by the fetus and damage to respiratory function. Damage to placental vessels meconium myonecrosis may also occur. | |||
* '''Newborn Respiratory Distress Syndrome''' - (Hyaline Membrane Disease) membrane-like substance from damaged pulmonary cells, absence of surfactant, if prolonged can be irreversible, intrauterine asphyxia, prematurity and maternal diabetes [http://www.nlm.nih.gov/MEDLINEPLUS/ency/article/001563.htm medline plus] | [http://www.medscape.com/article/976034-overview eMedicine] | |||
* '''Tracheoesophageal Fistula''' - Tracheo-Oesophageal Fistula, Oesophageal Atresia - Oesophageal Atresia with or without tracheo-oesophageal [[F#fistula|fistula]] '''Fistula''' - an abnormal communication between 2 structures (organs, vessels, cavities) that do not normally connect. | |||
# ''' | |||
* '''Lobar Emphysema''' (Overinflated Lung) - There is an overinflated left upper lobe There is a collapsed lower lobe The left lung is herniating across the mediastinum | |||
* | |||
* '''Congenital Diaphragmatic Hernia''' - (1 in 3,000 live births) Failure of the pleuroperitoneal foramen (foramen of Bochdalek) to close (left side), allows viscera into thorax -iIntestine, stomach or spleen can enter the pleural cavity, compressing the lung. rare (Morgagni hernia) -an opening in the front of the diaphragm. [http://www.ncbi.nlm.nih.gov/books/NBK1359 GeneReviews] | |||
''' | |||
* '''Azygos Lobe''' - Common condition (0.5% of population). The right lung upper lobe expands either side of the posterior cardinal. There is also some course variability of the phrenic nerve in the presence of an azygos lobe. | |||
* '''Congenital Laryngeal Webs''' - Laryngeal abnormality due to embryonic (week 10) incomplete recanalization of the laryngotracheal tube during the fetal period. Rare abnormality occuring mainly at the level of the vocal folds (glottis). | |||
* Hyaline Membrane Disease - (Newborn Respiratory Distress Syndrome) a membrane-like substance from damaged pulmonary cells. | |||
* '''Bronchopulmonary Dysplasia''' - A chronic lung disease which can occur following premature birth and related lung injury. Most infants who develop BPD are born more than 10 weeks before their due dates, weigh less than 1,000 grams (about 2 pounds) at birth, and have breathing problems. | |||
* '''Asthma''' - Flow limitation during tidal expiration in early life significantly associated with the development of physician-diagnosed asthma by the age of 2 years. Infants with abnormal lung function soon after birth may have a genetic predisposition to asthma or other airway abnormalities that predict the risk of subsequent lower respiratory tract illness. PMID 8176553 | |||
* '''Cystic Fibrosis''' - Inherited disease of the mucus and sweat glands, causes mucus to be thick and sticky. Clogging the lungs, causing breathing problems and encouraging bacterial grow. (Covered elsewhere in the course) | |||
* '''Environmental Factors''' see recent review below. <pubmed>20444669</pubmed> | |||
==Additional Information== | ==Additional Information== | ||
[[ | [[Respiratory Quiz]] | ||
{| class="wikitable collapsible collapsed" | {| class="wikitable collapsible collapsed" | ||
! | ! Grays - Respiratory Images | ||
|- | |- | ||
| | | | ||
<gallery> | <gallery> | ||
File: | File:Gray0947.jpg|947 The head and neck human embryo thirty-two days seen from the ventral surface. | ||
File: | File:Gray0948.jpg|948 Lung buds from a human embryo of about four weeks, showing commencing lobulations. | ||
File: | File:Gray0949.jpg|949 Lungs of a human embryo more advanced in development than week 4. | ||
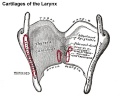
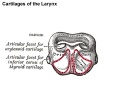
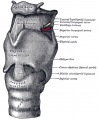
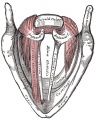
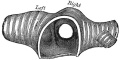
File:Gray0950.jpg|950 Cartilages of the larynx | |||
File:Gray0950 epiglottis cartilage.jpg|950 epiglottis cartilage | |||
File:Gray0950 thyroid cartilage.jpg|950 thyroid cartilage | |||
File:Gray0950 cricoid cartilage.jpg|950 cricoid cartilage | |||
File:Gray0950 arytenoid cartilage.jpg|950 arytenoid cartilage | |||
File:Gray0951.jpg|951 Ligaments of the larynx (anterior view) | |||
File:Gray0952.jpg|952 Ligaments of the larynx (posterior view) | |||
File:Gray0953.jpg|953 Larynx and upper part of the trachea | |||
File:Gray0954.jpg|954 | |||
File:Gray0955.jpg|955 Larynx entrance | |||
File:Gray0956.jpg|956 | |||
File:Gray0957.jpg|957 | |||
File:Gray0958.jpg|958 | |||
File:Gray0959.jpg|959 | |||
File:Gray0960.jpg|960 | |||
File:Gray0961.jpg|961 Cartilages of larynx, trachea, and bronchi (front view) | |||
File:Gray0962.jpg|962 Bronchi and bronchioles | |||
File:Gray0963.jpg|963 | |||
File:Gray0964.jpg|964 | |||
File:Gray0965.jpg|965 | |||
File:Gray0966.jpg|966 Lateral view of thorax, showing the relations of the pleuræ and lungs to the chest wall. Pleura in blue; lungs in purple. | |||
File:Gray0967.jpg|967 Transverse section through the upper margin of the second thoracic vertebra. | |||
File:Gray0968.jpg|968 | |||
File:Gray0969.jpg|969 | |||
File:Gray0970.jpg|970 Front view of heart and lungs | |||
File:Gray0971.jpg|971 Adult lungs | |||
File:Gray0974.jpg|974 Lung secondary lobule | |||
File:Lung_secondary_lobule_01.jpg|974 relabeled version | |||
File:Gray0975.jpg|975 Lung primary lobule | |||
File:Lung_primary_lobule_01.jpg|975 relabeled version | |||
File:Gray0976.jpg|976 Pig embryo lung | |||
</gallery> | </gallery> | ||
|} | |} | ||
{| class="wikitable collapsible collapsed" | {| class="wikitable collapsible collapsed" | ||
! | ! Respiratory Histology | ||
|- | |- | ||
| | | | ||
Histology will be covered in more detail in your associated practical class. | |||
===Fetal Histology=== | |||
<gallery> | |||
File:Fetal lung histology 02.jpg|Hyaline cartilage | |||
File:Fetal lung histology.jpg|late canalicular | |||
File:Fetal lung histology 01.jpg|unlabeled late canalicular | |||
</gallery> | |||
{{Fetal_Respiratory_Histology}} | |||
{{ | |||
===Adult Histology=== | |||
<gallery> | <gallery> | ||
File: | File:Respiratory histology 13.jpg|Olfactory Epithelium | ||
File:Respiratory histology 14.jpg|Olfactory Epithelium | |||
File:Respiratory histology 11.jpg|Respiratory Epithelium | |||
File:Respiratory histology 12.jpg|Respiratory Epithelium | |||
File:Respiratory histology 05.jpg|Trachea 1 | |||
File:Respiratory histology 06.jpg|Trachea 2 | |||
File:Respiratory_histology_01.jpg|Bronchiole | |||
File:Respiratory histology 10.jpg|Lung Elastin | |||
File:Respiratory histology 08.jpg|labeled lung | |||
File:Respiratory_histology_02.jpg|Alveolar Duct | |||
File:Respiratory_histology_03.jpg|Alveoli | |||
File:Respiratory histology 04.jpg|Alveoli Elastin | |||
File: | |||
File: | |||
File: | |||
File: | |||
File: | |||
File: | |||
File: | |||
File: | |||
File: | |||
File: | |||
File: | |||
</gallery> | </gallery> | ||
{{Respiratory_Histology}} | |||
|} | |} | ||
{{Glossary}} | {{Glossary}} | ||
{{Footer}} | {{Footer}} | ||
[[Category: | [[Category:Endoderm]] [[Category:Respiratory]] | ||
Revision as of 09:36, 8 March 2014
A draft page designed to be used only for testing.
Introduction
The lecture will introduce the development of the respiratory system and associated structures. The lecture will not cover adult anatomy, physiology of gas exchange, red blood cell function, cardiovascular development and will leave detailed histology to your associated practical class.
- Research suggests that in addition to genetic effects that the developmental environment (both fetal and postnatal) can influence the growth, differentiation and function of this system.
Lecture currently being updated for 2014.
Start Time/End Time: 10am to 11am Monday 10 March 2014 Clancy Auditorium 2013 Lecture Slides PDF
- Lecture: Lecture 2013 PDF | 2013 | 2012 | 2012 PDF (10 pages) | eMed Link to Learning Activity - Respiratory System Development
- SH Links: Lymphatic Lecture | Lymphatics Practical Support | Respiratory Lecture | Respiratory Practical Support | Medicine
The respiratory system does not carry out its physiological function (of gas exchange) until after birth, though the respiratory tract, diaphragm and lungs do begin to form early in embryonic development and continue through fetal development, only functionally maturing just before birth. The lungs continue to grow postnatally through childhood and some research finding suggest that there remains potential for growth in the adult.
The respiratory tract is divided anatomically into 2 main parts:
- upper respiratory tract - consisting of the nose, nasal cavity and the pharynx.
- lower respiratory tract - consisting of the larynx, trachea, bronchi and the lungs.
The respiratory "system" usually includes descriptions of not only the functional development of the lungs, but also related musculoskeletal (diaphragm) and vascular (pulmonary) development.
Aims
To understand the prenatal and postnatal developmental anatomy of human respiratory organs.
Key Concepts
- Embryonic origin of respiratory components (tract, lungs, diaphragm, muscles)
- Key stages in respiratory development.
- Time course of respiratory development.
- Respiration at birth.
- Postnatal development of respiration.
- Developmental abnormalities.
Textbooks
| Additional Textbooks |
|---|
|
| Audio |
|---|
| Lectopia Lecture Audio |
Respiratory Functional Unit
Alveolus (Latin alveolus = "little cavity", plural is alveoli)
|
|
| The alveoli cellular structure | Increase in human alveoli number |
|
|
| Alveoli and blood vessels | Lung structure |
Developmental Overview
Germ Layers
- Endoderm and splanchnic mesoderm form majority of conducting and alveoli.
- Ectoderm will contribute the neural innervation.
- Mesoderm also contributes the supporting musculoskeletal components.
|

|
|
| Week 4-5 (Stage 12 to 13) | Week 5 (Stage 15 to 16) | Week 6 (Stage 16 to 17) |
Week 4 - laryngotracheal groove forms on floor foregut.
Week 5 - left and right lung buds push into the pericardioperitoneal canals (primordia of pleural cavity)
Week 6 - descent of heart and lungs into thorax. Pleuroperitoneal foramen closes.
Week 7 - enlargement of liver stops descent of heart and lungs.
Month 3-6 - lungs appear glandular, end month 6 alveolar cells type 2 appear and begin to secrete surfactant.
Month 7 - respiratory bronchioles proliferate and end in alveolar ducts and sacs.
Development Stages
Note - the sequence is important rather than the actual timing, which is variable in the existing literature.
| Lung Stage | Human | Features | Vascular | |
|---|---|---|---|---|
| Embryonic | week 4 to 5 | lung buds originate as an outgrowth from the ventral wall of the foregut where lobar division occurs | extra pulmonary artery then lobular artery | |
| Pseudoglandular | week 5 to 17 | conducting epithelial tubes surrounded by thick mesenchyme are formed, extensive airway branching | Pre-acinar arteries | |
| Canalicular | week 16 to 25 | bronchioles are produced, increasing number of capillaries in close contact with cuboidal epithelium and the beginning of alveolar epithelium development | Intra-acinar arteries | |
| Saccular | week 24 to 40 | alveolar ducts and air sacs are developed | alveolar duct arteries | |
| Alveolar | late fetal to 8 years | secondary septation occurs, marked increase of the number and size of capillaries and alveoli | alveolar capillaries | |
| embryonic stage - pseudoglandular stage - canalicular stage - saccular stage - alveolar stage Links: Species Stage Comparison | respiratory | ||||
Embryonic
- week 4 - 5
- Endoderm - tubular ventral growth from foregut pharynx.
- Mesoderm - mesenchyme of lung buds.
- Intraembryonic coelom - pleural cavities elongated spaces connecting pericardial and peritoneal spaces.
Pseudoglandular stage
- week 5 - 17
- tubular branching of the human lung airways continues
- by 2 months all segmental bronchi are present.
- lungs have appearance of a glandlike structure.
- stage is critical for the formation of all conducting airways.
- lined with tall columnar epithelium
- more distal structures are lined with cuboidal epithelium.
Canalicular stage
- week 16 - 24
- Lung morphology changes dramatically
- differentiation of the pulmonary epithelium results in the formation of the future air-blood tissue barrier.
- Surfactant synthesis and the canalization of the lung parenchyma by capillaries begin.
- future gas exchange regions can be distinguished from the future conducting airways of the lungs.
Saccular stage
- week 24 to near term.
- most peripheral airways form widened "airspaces", termed saccules.
- saccules widen and lengthen the airspace (by the addition of new generations).
- future gas exchange region expands significantly.
- Fibroblastic cells also undergo differentiation, they produce extracellular matrix, collagen, and elastin.
- May have a role in epithelial differentiation and control of surfactant secretion.
- Alveolar Cells Type II (Type II pneumocytes)
- begin to secrete surfactant, levels of secretion gradually increase to term.
- allows alveoli to remain inflated
- Vascular tree - also grows in length and diameter during this time.
Alveolar stage
- late fetal to 8 years.
- The postnatal lung, with alveoli forming.
- Expansion of gas exchange alveoli, vascular beds (capillaries), lymphatics and innervation.
Foregut Development
From the oral cavity the next portion of the foregut is initially a single gastrointestinal (oesophagus) and respiratory (trachea) common tube, the pharynx which lies behind the heart. Note that the respiratory tract will form from a ventral bud arising at this level.
- Oral cavity
- Pharynx (esophagus, trachea)
- Respiratory tract
- Stomach
Upper Respiratory Tract
- part of foregut development
- anatomically the nose, nasal cavity and the pharynx
- the pharynx forms a major arched cavity within the pharyngeal arches (MH - pharyngeal arches will be described in BGD head development lecture).
| Additional Information - Histology | ||
|---|---|---|
This will be covered in detail in your associated SH Practical class.
|
Lower Respiratory Tract
|
|
| Stage 13 (Week 4-5) | Stage 22 (Week 8) |
- lung buds ( endoderm epithelial tubes) grow/push into mesenchyme covered with pleural cells (lung border)
- generates a tree-like network by repeated:
- elongation
- terminal bifurcation
- lateral budding
Growth initially of branched "conducting" system of bronchial tree, followed by later development of the "functional units" of the alveoli.
| Additional Information - Histology | ||
|---|---|---|
| This will be covered in detail in your associated SH Practical class.
Respiratory Trachea Mucosa - formed by epithelium and underlying lamina propria.
Submucosa - connective tissue and submucosal glands
Cartilage
Hyaline Cartilage Development
Bronchi Branching main bronchi -> lobar bronchi -> segmental bronchi (supply lung bronchopulmonary segments) -> bronchi -> bronchioles (smaller than 1 mm) -> respiratory bronchioles.
Bronchioles
Respiratory Bronchioles
|
Fetal Lung Volume
Each human lung volume as determined by ultrasound and matched to gestational age [1]
|
|
Pleural Cavity
- anatomical body cavity in which the lungs develop and lie.
- pleural cavity forms in the lateral plate mesoderm as part of the early single intraembryonic coelom.
- This cavity is initially continuous with pericardial and peritoneal cavities and form initially as two narrow canals.
- later becomes separated by folding (pleuropericardial fold, pleuroperitoneal membrane) and the later formation of the diaphragm.
- pleuropericardial fold - (pleuropericardial membrane) An early embryonic fold which restricts the communication between pleural cavity and pericardiac cavity, contains both the cardinal vein and phrenic nerve.
- pleuroperitoneal membrane - An early embryonic membrane that forms inferiorly at the septum transversum to separate peritoneal cavity from pleural cavity.
Pleura
- serous membrane covers the surface of the lung and the spaces between the lobes.
- arranged as a closed invaginated sac.
- two layers (pulmonary, parietal) continuous with each other, the potential space between them is the pleural cavity.
Diaphragm
- Not respiratory tract but musculoskeletal development, there are 5 embryonic elements that contribute to the diaphragm.
|
|
- Innervation of the human diaphragm is by the phrenic nerves
- arising from the same segmental levels from which the diaphragm skeletal muscles arise, segmental levels C3 to C5.
- The paired phrenic nerves are mixed nerves
- motor neurons for the diaphragm
- sensory nerves for other abdominal structures (mediastinum, pleura, liver, gall bladder).
Pulmonary Circulation
- the pulmonary system not "functional" until after birth
- pulmonary arteries - 6th aortic arch arteries
- pulmonary veins - are incorporated into the left atrium wall
- bronchial arteries - branches from dorsal aorta
Fetal
Fetal Respiratory Movements
- Fetal respiratory movements (FRM) or Fetal breathing movements (FBM) are regular muscular contrations occurring in the third trimester.
- preparing the respiratory muscular system for neonatal function.
- may also have a role in late lung development.
The First Breath
- The respiratory system does not carry out its physiological function (gas exchange) prenatally and remain entirely fluid-filled until birth.
- At birth, fluid in the upper respiratory tract is expired and fluid in the lung aveoli is rapidly absorbed this event has also been called "dewatering of the lung".
- The lung epithelia has to now rapidly change from its prenatal secretory function to that of fluid absorbtion.
The exchange of lung fluid for air leads to:
- fall in pulmonary vascular resistance
- increase in pulmonary blood flow
- thinning of pulmonary arteries (stretching as lungs increase in size)
- blood fills the alveolar capillaries
In the heart - pressure in the right side of the heart decreases and pressure in the left side of the heart increases (more blood returning from pulmonary).
Postnatal
Alveoli
- At birth about 15% of adult alveoli number have formed
- 20 - 50 million to in the adult about 300 million.
- remaining subdivisions develop in the first few postnatal years
Respiratory Rate
- neonatal rate is higher (30-60 breaths/minute) than adult (12-20 breaths/minute).
- tachypnea - (Greek, rapid breathing) an increased respiratory rate of greater than 60 breaths/minute in a quiet resting baby
| Age | Rate (breaths/minute) |
| Infant (birth - 1 year) | 30 - 60 |
| Toddler (1 - 3 years) | 24 - 40 |
| Preschool (3 - 6 years) | 22 - 34 |
| School age (6 - 12 years) | 18 - 30 |
| Adolescent (12 - 18 years) | 12 - 16 |
Rib Orientation
- Infant rib - is virtually horizontal, allowing diaphragmatic breathing only.
- Adult rib - is oblique (both anterior and lateral views), allows for pump-handle and bucket handle types of inspiration.
Respiratory Tract Abnormalities
Respiratory System - Abnormalities
- Meconium Aspiration Syndrome - (MAS) Meconium is the gastrointestinal contents that accumulate in the intestines during the fetal period. Fetal stress in the third trimester, prior to/at/ or during parturition can lead to premature meconium discharge into the amniotic fluid and sunsequent ingestion by the fetus and damage to respiratory function. Damage to placental vessels meconium myonecrosis may also occur.
- Newborn Respiratory Distress Syndrome - (Hyaline Membrane Disease) membrane-like substance from damaged pulmonary cells, absence of surfactant, if prolonged can be irreversible, intrauterine asphyxia, prematurity and maternal diabetes medline plus | eMedicine
- Tracheoesophageal Fistula - Tracheo-Oesophageal Fistula, Oesophageal Atresia - Oesophageal Atresia with or without tracheo-oesophageal fistula Fistula - an abnormal communication between 2 structures (organs, vessels, cavities) that do not normally connect.
- Lobar Emphysema (Overinflated Lung) - There is an overinflated left upper lobe There is a collapsed lower lobe The left lung is herniating across the mediastinum
- Congenital Diaphragmatic Hernia - (1 in 3,000 live births) Failure of the pleuroperitoneal foramen (foramen of Bochdalek) to close (left side), allows viscera into thorax -iIntestine, stomach or spleen can enter the pleural cavity, compressing the lung. rare (Morgagni hernia) -an opening in the front of the diaphragm. GeneReviews
- Azygos Lobe - Common condition (0.5% of population). The right lung upper lobe expands either side of the posterior cardinal. There is also some course variability of the phrenic nerve in the presence of an azygos lobe.
- Congenital Laryngeal Webs - Laryngeal abnormality due to embryonic (week 10) incomplete recanalization of the laryngotracheal tube during the fetal period. Rare abnormality occuring mainly at the level of the vocal folds (glottis).
- Hyaline Membrane Disease - (Newborn Respiratory Distress Syndrome) a membrane-like substance from damaged pulmonary cells.
- Bronchopulmonary Dysplasia - A chronic lung disease which can occur following premature birth and related lung injury. Most infants who develop BPD are born more than 10 weeks before their due dates, weigh less than 1,000 grams (about 2 pounds) at birth, and have breathing problems.
- Asthma - Flow limitation during tidal expiration in early life significantly associated with the development of physician-diagnosed asthma by the age of 2 years. Infants with abnormal lung function soon after birth may have a genetic predisposition to asthma or other airway abnormalities that predict the risk of subsequent lower respiratory tract illness. PMID 8176553
- Cystic Fibrosis - Inherited disease of the mucus and sweat glands, causes mucus to be thick and sticky. Clogging the lungs, causing breathing problems and encouraging bacterial grow. (Covered elsewhere in the course)
- Environmental Factors see recent review below. <pubmed>20444669</pubmed>
Additional Information
| Grays - Respiratory Images |
|---|
|
|
| Respiratory Histology |
|---|
|
Histology will be covered in more detail in your associated practical class. Fetal Histology
Adult Histology
|
Glossary Links
- Glossary: A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | Numbers | Symbols | Term Link
Cite this page: Hill, M.A. (2024, June 27) Embryology Sandbox. Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/Sandbox
- © Dr Mark Hill 2024, UNSW Embryology ISBN: 978 0 7334 2609 4 - UNSW CRICOS Provider Code No. 00098G
- ↑ <pubmed>16388511</pubmed>