BGDA Practical - Male Reproductive Tract Histology
From Embryology
Introduction
| This current page provides background support information for Medicine phase 1 BGD Histology Practical Virtual Slides. Page does not form part of the BGDA practical class virtual slides.
|
Objectives
- Gain an overview of the microanatomy of the male reproductive system.
- Undertake a microscopical examination of the testis, epididymis, vas deferens, seminal vesicle, prostate gland, penis, and sperm. The functional significance of the various histological structures identified will be discussed.
- Links: Testis Development | Prostate Development | Histology
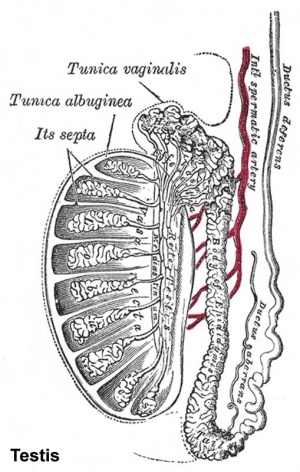
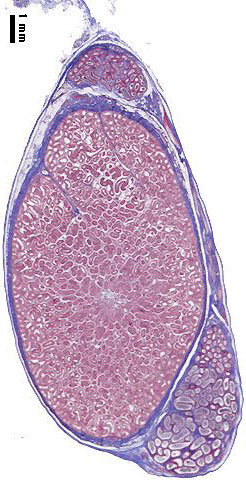
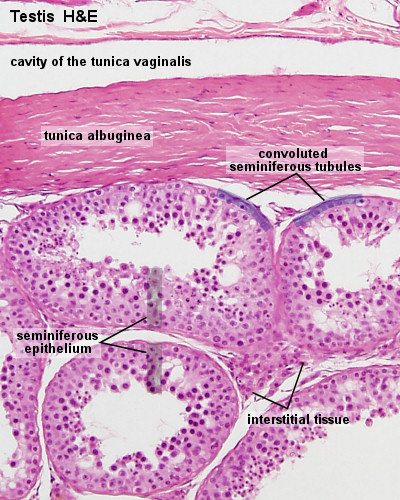
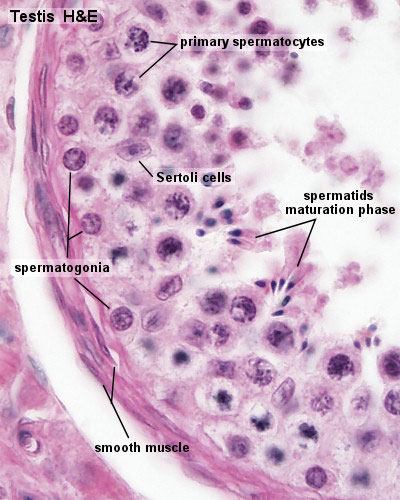
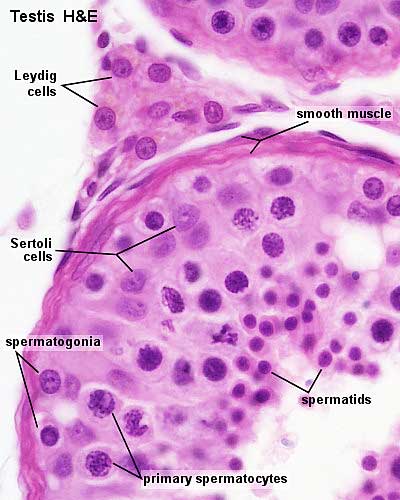
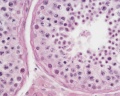
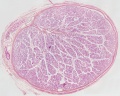
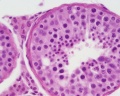
Testis Histology
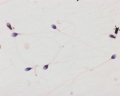
Spermatozoa
|
<html5media height="240" width="300">File:Spermatozoa_animation.mp4</html5media> |
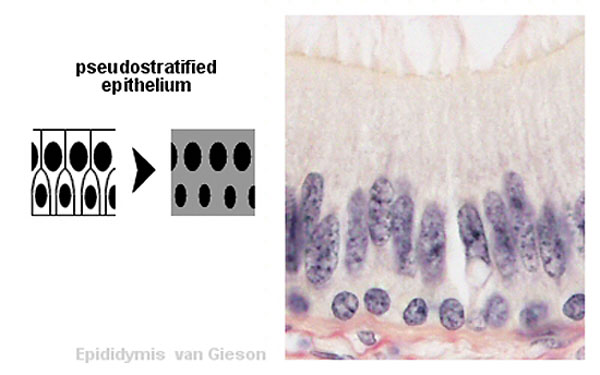
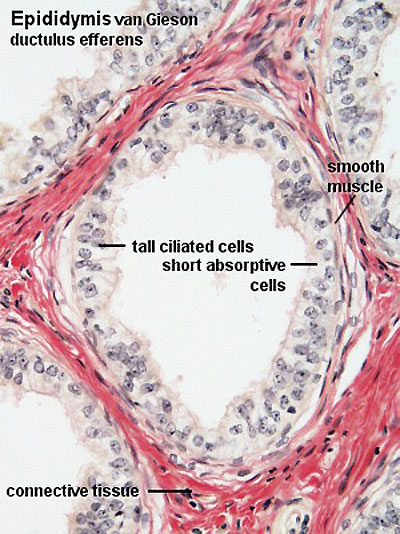
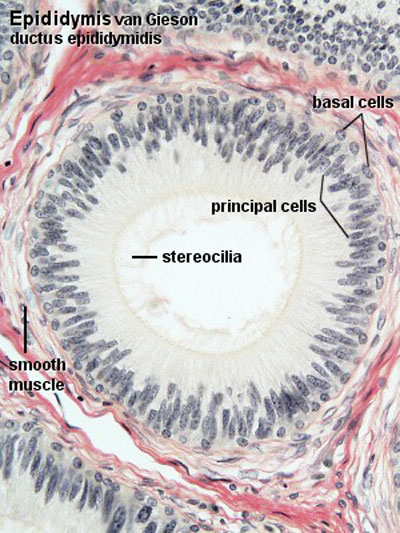
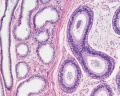
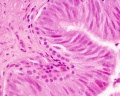
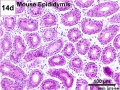
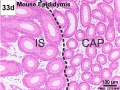
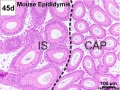
Epididymis Histology
Human Testis (adult)
Human Testis (young)
Other Species
Rabbit
Mouse
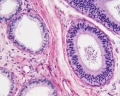
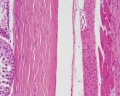
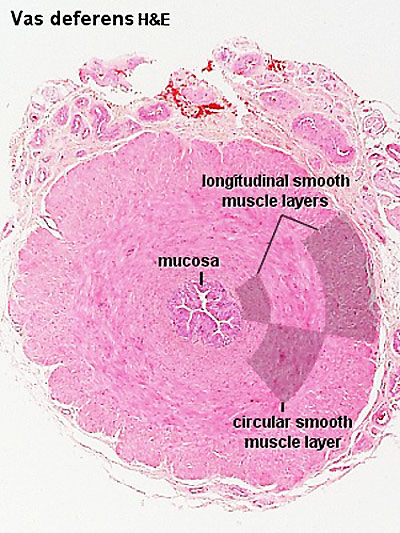
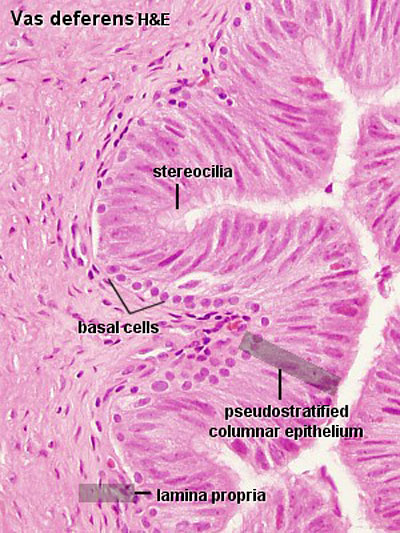
Ductus Deferens Histology
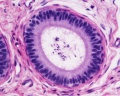
Prostate Histology

|
|
|
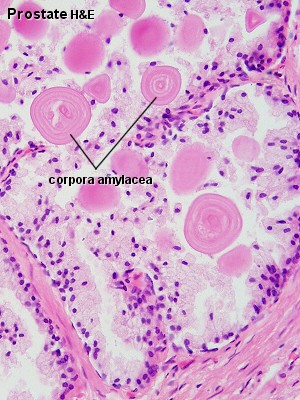
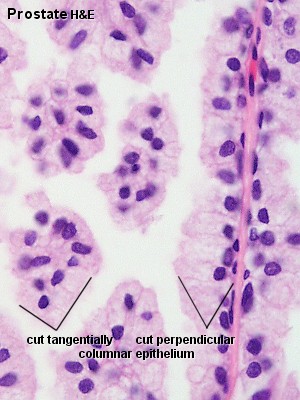
| Human prostate histology | Corpora Amylacea | Submucosal gland |
| (adult, low power overview) | (adult, detail) | (adult, high power detail) |
Penis Histology
Terms
- cortex - (Latin = rind, or bark) outer layer of an organ.
- hilum - or hilus (Latin,= a trifle; depression in a seed) a depression at vascular entrance/exit of a gland or organ.
- medulla - (Latin, medulla = pith, marrow) the inner portion of an organ, in contrast to cortex.
- mucosa - (Latin, = mucous membrane) thin layer which lines body cavities and passages formed by epithelium and lamina propria.
- parenchyma - (Greek," + enkeim = to pour in) the essential functional cells of an organ as opposed to its stroma.
- serosa - (Latin, serum = whey; a pale fluid) a serous membrane lining body cavities.
- stroma - (Greek, = a cover, table-cloth, bedding) term for the internal supporting frame-work of a tissue, or organ, as opposed to its parenchyma.
- tunica albuginea - a dense, white, fibrous sheath enclosing a part or organ.
- Histology Glossary: A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | ANAT2241 Support | Histology | Histology Stains | Embryology Glossary
BGDA: Lecture 1 | Lecture 2 | Practical 3 | Practical 6 | Practical 12 | Lecture Neural | Practical 14 | Histology Support - Female | Male | Tutorial
Glossary Links
- Glossary: A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | Numbers | Symbols | Term Link
Cite this page: Hill, M.A. (2026, March 2) Embryology BGDA Practical - Male Reproductive Tract Histology. Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/BGDA_Practical_-_Male_Reproductive_Tract_Histology
- © Dr Mark Hill 2026, UNSW Embryology ISBN: 978 0 7334 2609 4 - UNSW CRICOS Provider Code No. 00098G