Introduction
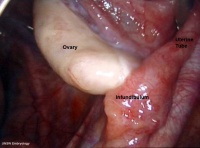
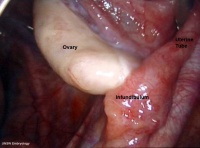
Adult human ovary peritoneal surface (viewed by endoscopy)
This current page provides background support information for Medicine phase 1 BGD Histology Practical Virtual Slides. Page does not form part of the BGDA practical class virtual slides.
Young, B., Lowe, J., Stevens, A. & Heath, J. (2006) Wheater’s Functional Histology. A Text and Colour Atlas 5th ed. Churchill Livingstone, Edinburgh. ISBN 0-443-06850X. UNSW Online
Objectives
- Gain an overview of the microanatomy of the female reproductive system.
- Undertake a microscopical examination of the ovary, oviduct, uterus, cervix, vagina and mammary glands. The functional significance of the various histological structures identified will be discussed.
Ovary
The external surface of the ovary has a cuboidal epithelium (germinal epithelium) overlying a dense connective tissue layer (tunica albuginea). The outer epithelium is continuous with the peritoneum (serosa) forming a peritoneal fold (mesovarium) between the anterior border of the ovary with the posterior layer of the broad ligament of the uterus.
Ovary structure (regions)
- cortex - cellular connective tissue containing the developing follicles.
- medulla - loose connective tissue containing blood vessels, lymphatics and nerves.
Ovarian Follicle
|
Beginning at puberty, the ovarian primordial follicle goes through a number of developmental stages leading to the release of an oocyte at ovulation at about the middle of the menstrual cycle.
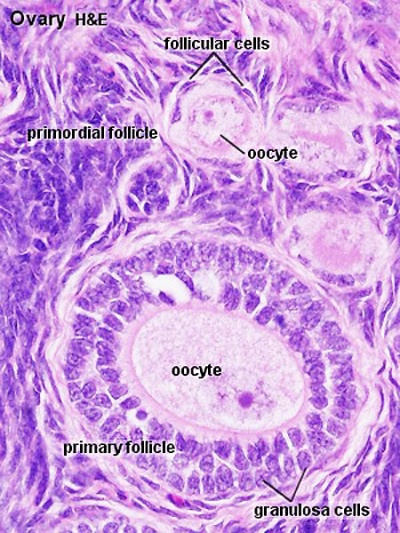
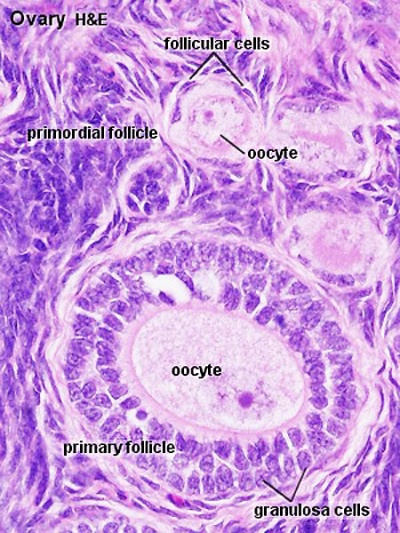
Primordial Follicle
- located in the cortex just beneath tunica albuginea.
- One layer of flattened follicular cells surround the oocyte (about 30 µm in diameter).
- nucleus of the oocyte is positioned eccentric in the cell. It appears very light and contains a prominent nucleolus.
- most organelles of the oocyte aggregate in the centre of the cell, where they form the vitelline body.
Primary Follicle
(preantral)
- first morphological stage that marks the onset of follicular maturation
- previously flattened cell surrounding the oocyte now form a cuboidal or columnar epithelium surrounding the oocyte.
- cytoplasm has a granular appearance, reason also called granulosa cells.
- continued proliferation of these cells will result in the formation of a stratified epithelium (with a distinct basement membrane) surrounding the oocyte.
- zona pellucida becomes visible.
- extracellular matrix formed by glycoproteins between interdigitating processes of oocyte and granulosa cells.
- parenchymal cells of the ovary surrounding the growing follicle become organised in concentric sheaths, the theca folliculi.
|
|
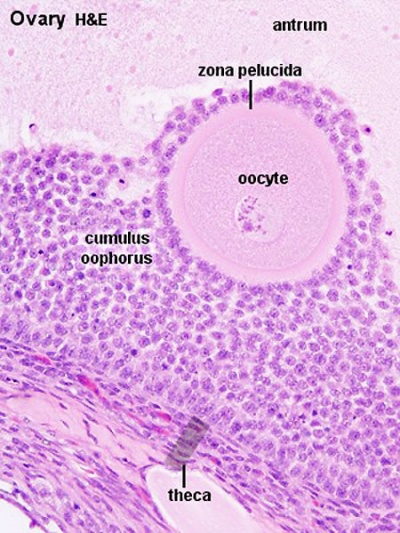
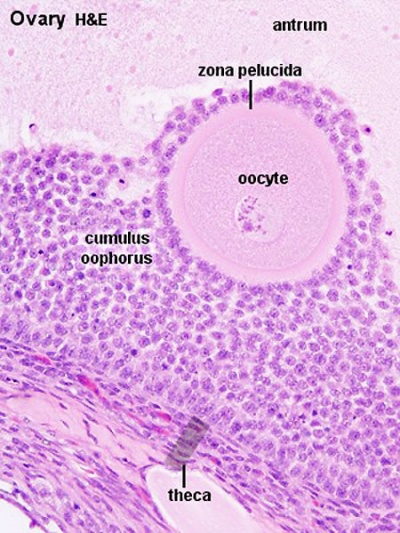
Secondary Follicle
(antral)
- small fluid-filled spaces become visible between the granulosa cells as the follicle reaches a diameter of about 400 µm.
- spaces enlarge and fuse to form the follicular antrum
- defining feature of the secondary follicle.
- oocyte is now located on one wall of the follicle in the cumulus oophorus.
- theca folliculi differentiates to form 2 layers the theca interna and a theca externa
- theca interna - spindle-shaped or polyhedral cells start to produce estrogens (also increased vascularization).
- theca externa - highly cellular connective tissue with smooth muscle cells.
- oocyte of the secondary follicle reaches a diameter of about 125 µm.
- follicle itself reaches a diameter of about 10-15 mm.
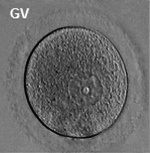
Preovulatory Follicle
(Graafian, tertiary, mature follicle)
- increases further in size (in particular in the last 12h before ovulation).
- stigma (macula pellucida) ovarian surface swelling formed by enlarging follicle.
- thinning of the capsule, progressive restriction of the blood flow.
- prior to ovulation the cumulus oophorus separates from the follicular wall.
- oocyte floats freely in the follicular antrum, follicular fluid.
- still surrounded by granulosa cells which form the corona radiata.
- Ovulation - follicle ruptures at the stigma, oocyte, supporting cells and follicular fluid released from the ovary.
|
|
Corpus Luteum
- The corpus luteum cells work together in the production of ovarian hormones that support the initial pregnancy.
- Initial growth of the corpus luteum requires leutenizing hormone ( LH) from the adenohypophysis.
- Later growth of the corpus luteum requires human chorionic gonadotrophin (hCG) from the implanting conceptus (trophoblast cells).
- Progesterone is synthesized from cholesterol by both the large and small luteal cells upon luteal maturation.
Theca Lutein Cells
- the darker stained cells.
- derived from the theca interna of the original follicle.
- lack microvilli on the surface.
- lack the aromatase enzyme.
- produce androgens for the granulosa lutein cells to convert.
Granulosa Lutein Cells
- the lighter stained cells.
- derived from the granulosa cells of the original follicle.
- contain aromatase enzyme.
- produce estrogen and progesterone from the androgens produced by the theca lutein cells.
theca and granulosa lutein cells
|

|
Corpus Albicans
Hormone secretion in the corpus luteum ceases within 14 days after ovulation if the oocyte is not fertilised. In this case, the corpus luteum degenerates into a corpus albicans - whitish scar tissue within the ovaries.
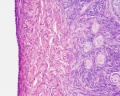
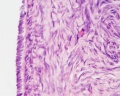
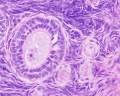
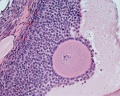
Ovary Histology
Tunica albuginea, Germinal epithelium x40
Primary follicle, primordial follicle, oocyte, x40
Secondary follicle, cumulus oophorus, zona pelucida, granulosa cells, oocyte x20
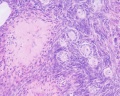
Corpus luteum, theca lutein cells, granulosa lutein cells, Loupe
Corpus luteum, theca lutein cells, granulosa lutein cells, x10
Corpus luteum, theca lutein cells, granulosa lutein cells, x40
Corpus albicans, primary follicle, primordial follicle, granulosa cells, oocyte x20
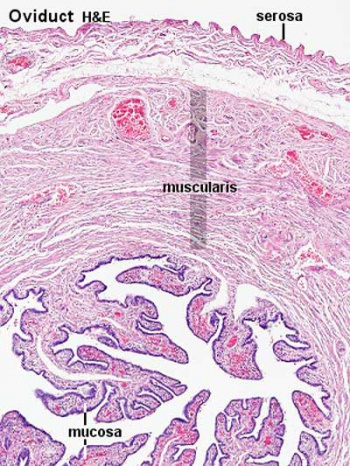
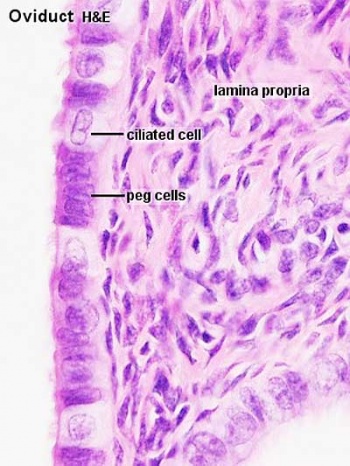
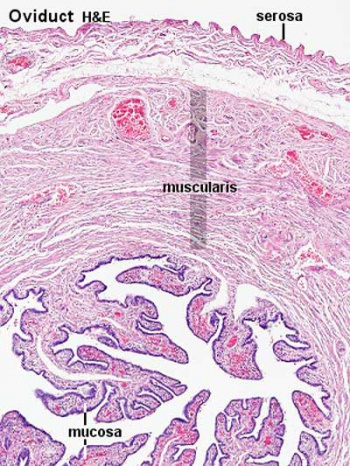
Uterine Tube
(oviduct, Fallopian tube)
- uterine tube acts as a conduit for the oocyte, from the ovaries to the uterus.
- consists of a mucosa and a muscularis.
- peritoneal surface of the oviduct is lined by a serosa and subjacent connective tissue.
| Overview
|
Mucosa
|
|
|
Muscularis
- inner circular muscle layer and an outer longitudinal layer.
- inner longitudinal layer is present in the isthmus and the intramural part.
- peristaltic muscle action for the transport of spermatozoa and oocyte.
|
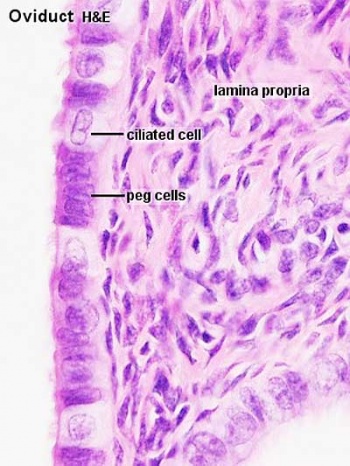
Mucosa
- ciliated and secretory epithelium resting on a cellular lamina propria.
- number of ciliated cells and secretory cells varies along the tube.
- also varied by ovarian hormones during menstrual cycle.
- secretory activity varies during the menstrual cycle, and resting secretory cells are also referred to as peg-cells. Some of the secreted substances are thought to nourish the oocyte and the very early embryo.
|
Tube Regions

|
| infundibulum
|
ampulla
|
isthmus
|
intramural
|
| funnel-shaped (up to 10 mm in diameter) end of the oviduct. Finger-like extensions of its margins, the fimbriae, are closely applied to the ovary. Ciliated cells are frequent.
|
mucosal folds, or plicae, and secondary folds which arise from the plicae divide the lumen of the ampulla into a very complex shape. Fertilization usually takes place in the ampulla.
|
narrowest portion (2-3 mm in diameter) of the tube located in the peritoneal cavity. Mucosal folds are less complex and the muscularis is thick. An inner, longitudinal layer of muscle is present in the isthmus.
|
penetrates the wall of the uterus. The mucosa is smooth, and the inner diameter of the duct is very small.
|
Uterus
- parts - body (upper two-thirds) and cervix.
- walls - mucosal layer, the endometrium, and a fibromuscular layer, the myometrium.
- peritoneal surface of the uterus is covered by a serosa.
Myometrium
- smooth muscle fibres form several layers with preferred orientations.
- muscular tissue hypertrophies during pregnancy.
- GAP-junctions between cells become more frequent.
Endometrium
- simple columnar epithelium (ciliated cells and secretory cells) and an underlying thick connective tissue stroma.
- mucosa is invaginated to form many simple tubular uterine glands.
- glands extend through the entire thickness of the stroma.
- stromal cells of the endometrium are embedded in a network of reticular fibres.
Menstrual cycle
- hormones alter the endometrium.
- only the uterus body mucosa takes part in the menstrual cycle.
- endometrial layers (based on changes)
- basalis - remains during menstruation, functions as a regenerative zone for the functionalis.
- functionalis - lost during menstruation, functions as the site of cyclic changes in the endometrium.
Gland - proliferative phase
- secretory phase - corpus luteum hormone (progesterone) after ovulation promotes production and secretion by the endometrial glands.
- Uterus Histology Links: Labeled - proliferative phase | Labeled - gland proliferative phase | Labeled - secretory phase | Unlabeled - secretory phase | Unlabeled - late secretory phase | Labeled - gland secretory phase | Menstrual Cycle | Uterine Gland | Uterus Development
- Links: Menstrual Cycle - Histology
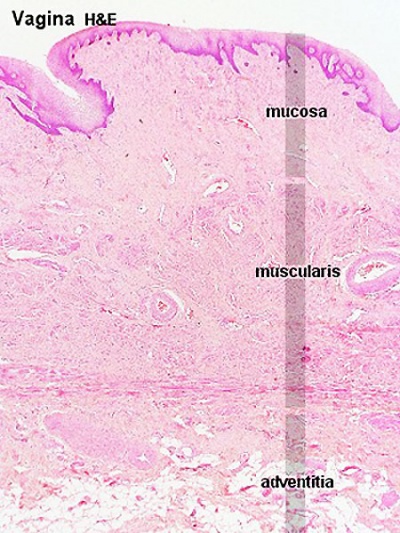
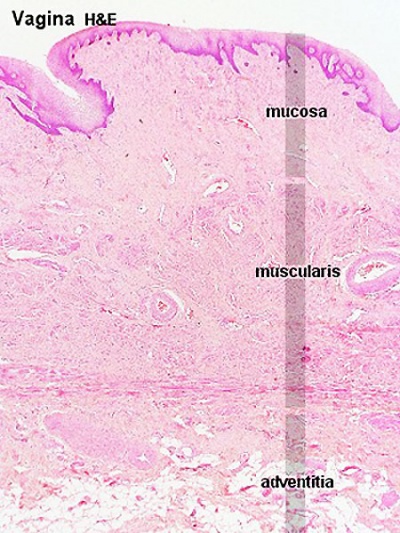
Vagina
Virtual slides - vagina
The wall of the vagina fibromuscular tube consists of 3 layers:
- mucosa
- muscularis
- adventitia
Mucosa
- stratified squamous nonkeratinized epithelium
- deep stratum basalis, intermediate stratum spinosum, superficial layers of flat eosinophilic cells.
- glycogen acted upon by lactobacillus acidophilus to acidify lumen.
- rests on a cellular lamina propria (many leukocytes).
- towards the muscularis some vascular cavernous spaces may be seen (erectile tissue).
Muscularis
- inner circular and outer longitudinal layers of smooth muscle
- bulbospongiosus muscle - (striated) forms an inferior sphincter around the vagina
Adventitia
- adventitia bordering the muscularis is fairly dense and contains many elastic fibres.
- outer part of the adventitia loose connective tissue with a prominent venous plexus.
|
|
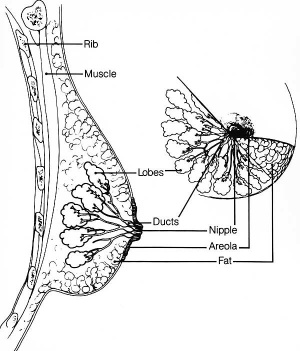
Mammary Gland
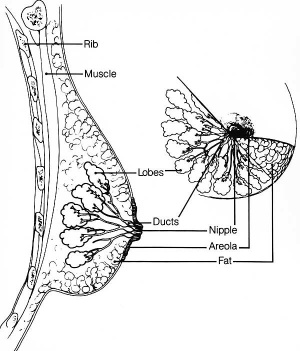
Adult female mammary anatomy cartoon
Virtual slides - Mammary gland inactive | Mammary gland active
The mammary glands are modified glands of the skin and their development is similar to that of sweat glands.
- compound branched alveolar glands, secretory unit is the alveolus
- consist of 15-25 lobes separated by dense interlobar connective tissue and fat.
- each lobe contains an individual gland.
- lactiferous duct - excretory duct of each lobe with own opening on the nipple.
Alveolus
- inner layer of cuboidal secretory epithelial cells
- apocrine secretion - lipids
- merocrine secretion - proteins (exocytosis)
- outer layer of myoepithelial cells
- located between the secretory cells and the surrounding basal lamina.
- contraction helps force the milk from the secretory alveoli into the ducts.
Note - plasma cells in the stroma also secrete antibodies (dimeric IgA) and released into the milk, to provides passive immunity to the suckling young.
| Lactiferous duct
|
Lactating mammary gland
|
Apocrine secretion
|

|

|

|
- Links: mammary gland | milk
Terms
- corona radiata - layer of cells of cumulus oophorus remaining attached to zona pellucida of oocyte after ovulation.
- corpus - (Latin, corpus = body).
- corpus albicans - (Latin, corpus = body + albicans = "whitish") a degenerating corpus luteum in the ovary.
- corpus luteum - (Latin, corpus = body + luteum = yellow) major endocrine organ which is the remains of ovarian follicle after ovulation; yellow in ovary of cow where de Graaf (q.v.) first saw it.
- cortex - (Latin = rind, or bark) outer layer of an organ.
- cumulus oophorus - (Latin = cumulus = a little mound + Greek oon = egg + phorus = bearing) part of the wall of an ovarian follicle surrounding and carrying the oocyte.
- fimbria - (Latin, fimbria = a fringe) the fringed open ovarian end of the uterine tube.
- follicle - (Latin, folliculus = little bag).
- hilum - or hilus (Latin,= a trifle; depression in a seed) a depression at vascular entrance/exit of a gland or organ.
- lactobacillus acidophilus (Latin acid-loving milk-bacillus) gram positive bacteria that grows readily at low pH (below pH 5.0) and ferment sugars into lactic acid.
- mesothelium - epithelium (serosa) that lines the peritoneum, pleurae, and pericardium. Embryonically derived from epithelialisation of mesoderm.
- mesovarium - short peritoneal fold connecting the anterior border of the ovary with the posterior layer of the broad ligament of the uterus.
- medulla - (Latin, medulla = pith, marrow) the inner portion of an organ, in contrast to cortex.
- menstrual - (Latin, menstruus = monthly) relating to the monthly female sexual cycle.
- mucosa - (Latin, = mucous membrane) thin layer which lines body cavities and passages formed by epithelium and lamina propria.
- oocyte - (Greek, öon = egg + kytos = hollow vessel (cell) the female germ cell in the ovary.
- parenchyma - (Greek," + enkeim = to pour in) the essential functional cells of an organ as opposed to its stroma.
- salpinx - (Greek, = a trumpet) the uterine tube.
- serosa - (Latin, serum = whey; a pale fluid) a serous membrane lining body cavities.
- stroma - (Greek, = a cover, table-cloth, bedding) term for the internal supporting frame-work of a tissue, or organ, as opposed to its parenchyma.
- tunica albuginea - a dense, white, fibrous sheath enclosing a part or organ.
- uterine tube - (oviduct, Fallopian tube)
- uterus - (Latin, = womb, from uter = a large goatskin bag used as a wine-skin).
- zona pellucida - (Latin, zona = a girdle + perlucere = to shine through) the refractile layer of glycoclayx (ECM) surrounding oocyte in a growing ovarian follicle.
- Histology Glossary: A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | ANAT2241 Support | Histology | Histology Stains | Embryology Glossary
Additional Information
| Additional Information - Content shown under this heading is not part of the material covered in this class. It is provided for those students who would like to know about some concepts or current research in topics related to the current class page.
|
Development
Links: Female | ovary | oocyte | uterus | vagina
Follicle Classification
Be aware that there are several different nomenclatures used for classifying the stages of follicle maturation.
Ovarian reserve - refers to the number of oocytes available (for possible fertilization) at the different times during female reproductive life.[1]
| Oocyte terms
|
| Oocyte Development
Note there are additional specific term glossaries available listed at bottom of this table.
- antral follicle - (secondary) the stage following preantral in the decription of the sequence ovarian follicle development.
- antrum - (L. a cave), cavity; a nearly-closed cavity or bulge. In the ovary this refers to the follicular fluid-filled space within the follicle.
- atretic follicle - An ovarian follicle that fails to mature and degenerates. Also called "atresia" refering to the process of degeneration of the ovarian follicle. This process can occur at any stage of follicle development (folliculogenesis).
- clomiphene citrate - drug taken orally to promote the process of follicle/egg maturation.
- COCs - (cumulus-oocyte complexes) term used in Assisted Reproductive Technology to describe the ovulated Graafian follicle consisting of the oocyte surrounded by a packed layers of cumulus cells.
- corona radiata - Layer of follicle cells of cumulus oophorus remaining directly attached to zona pellucida of the oocyte. These cells communicate with the oocyte through the zone pellucida, also called granulosa cells.
- corpus albicans - (L. corpus = body, L. albicans = whitish); a degenerating corpus luteum in ovary.
- corpus luteum - (L. corpus = body, L. luteum = yellow) The remains of the ovulating ovarian follicle after ovulation, that acts as the initial endocrine organ supporting pregnancy and preventing menstruation (loss of the endometrial lining). de Graaf first observed it in the ovary of a cow as a yellow structure.
- cortical - (L. corticalis) at the outside (like the bark of a tree), usually combined with medulla meaning the core.
- cumulus oophorus - (L. cumulus = a little mound G. oon = egg + phorus = bearing); part of the wall of an ovarian follicle surrounding and carrying the ovum (oocyte).
- first polar body - a small cytoplasmic exclusion body contains the excess DNA from the oocyte meiosis formed during meiosis 1.
- follicle - (L. folliculus = little bag,dim. of L. follis). A structure which develops in the ovary and contains a developing egg (oocyte).
- follicle stimulating hormone - (FSH, gonadotropin) A glycoprotein hormone secreted by anterior pituitary (adenohypophysis gonadotrophs, a subgroup of basophilic cells) and acts on gametogenesis and other systems in both males and females. Females, FSH acts on the ovary to stimulate follicle development. Males, acts on the testis Sertoli cells to increase androgen-binding protein (ABP) that binds androgens and has a role in spermatogenesis. pituitary
- follicular fluid - the fluid found in the antrum of a secondary follicle. Secreted by cells in the wall of the follicle. This fluid is released along with the oocyte at ovulation.
- germinal epithelium - cellular component covering surface of ovary, it is continuous with mesothelium covering mesovarium. Note that it is a historical misnomer, as it is not the actual site of germ cell formation.
- Graafian follicle - named after Regnier de Graaf (1641-1673), an historic Dutch physician embryologist who studied pregnancy using rabbits.
- granulosa cells - the supporting cells that surround the developing egg within the follicle thecal layers.
- homologs - maternal and paternal homologous chromosomes.
- Izumo1 - a protein located on the equatorial segment of acrosome-reacted spermatozoa recognizes its receptor Juno, on the oocyte surface, for plasma membrane binding and fusion. Named for a Japanese shrine dedicated to marriage. OMIM609278
- Juno - (folate receptor-δ; FOLR-δ) a glycophosphatidylinositol (GPI)-anchored, cysteine-rich glycoprotein on the oocyte surface for fertilisation that is the receptor of Izumo1 on the spermatozoa, for plasma membrane binding and fusion. OMIM615737
- luteinizing hormone - (LH, gonadotropin, lutropin, Interstitial Cell Stimulating Hormone, ICSH) glycoprotein hormone releasd from anterior pituitary hormone that acts on the gonad and has a role in male and female reproduction. Female, LH triggers ovulation (release of the oocyte). Male, LH stimulates testis interstital cell (Leydig cell) production of testosterone. Have been used clinically in humans for the treatment of female infertility.
- meiosis - oocyte reductive (diploid to haploid) cell division, with 1 round of DNA replication is followed by 2 rounds of chromosome segregation. The process beginning in the fetus and only completed at fertilization.
- mesovarium - mesentry of the ovary formed from a fold of the broad ligament that attaches the ovary.
- medullary - (L. medius = in the middle) relating to the medulla; pith, marrow, inner portion of an organ. Usually combined with cortex (cortical) meaning the outer layer.
- oocyte - (Greek, oo = egg, ovum) The term used to describe the haploid egg or ovum formed within the ovary (female gonad) and released to enter the uterine tube and be transported to the uterus. The mature oocyte is the cell released from the ovary during ovulation.
- oogenesis - (Greek, oo = egg + genesis = origin, creation, generation) process of diploid oogonia division and differentiation into an haploid oocyte (egg) within the ovary (female gonad). Mammalian meiosis will only be completed within the oocyte if fertilization occurs.
- oogonia - (Greek, oo = egg) diploid germ cells within the ovary (female gonad) which provide the primary oocytes for oocyte (egg) formation. In humans, all oogonia form primary oocytes within the ovary before birth.
- oolemma - (zona pellucida, vitelline membrane).
- oophorus - (Greek, oo = egg + phorus = carrying, egg-bearing) cumulus oophorus, used to describe the granulosa cells within the follicle that tether or link the oocyte to the wall of the follicle.
- ovarian reserve - Clinical term for the number of oocytes (non-growing follicles) available for possible fertilization at the different times during female reproductive life. A blood test for Anti-Mullerian Hormone (AMH) levels is used clinically as a measure of the ovarian reserve. human graph
- ovastacin - an oocyte released enzyme following fertilization that cleaves ZP2 protein to prevent polyspermy.
- ovulation - release of the oocyte from the mature follicle. In humans generally a single oocyte is released from a cohort of several maturing follicles.
- ovum - oocyte, note that historically this same term was also used to describe the early stages following fertilisation.
- polar body - small cytoplasmic exclusion body contains the excess DNA from the oocyte meiosis reductive division. The first polar body formed during meiosis 1, the second and sometimes third polar bodies are formed from meiosis 2 at fertilization.
- polyspermy - abnormal fertilization by more that a single spermatozoa, may generate a hydatidiform mole.
- preantral follicle - (primary) the stage following primordial in the description of the sequence ovarian follicle development.
- primary follicle - (preantral) the stage following primordial in the description of the sequence ovarian follicle development.
- primordial follicle - the first stage in the description of the sequence ovarian follicle development. Present in the ovary from birth, located in the stroma of the ovary cortex beneath the tunica albuginea. The primordial follicle is the oocyte and the surrounding follicular cells.
- primordial germ cell - oocyte present in the primordial follicle ovary from birth, located in the stroma of the ovary cortex beneath the tunica albuginea. The primordial follicle is the oocyte and the surrounding follicular cells.
- second polar body - a small cytoplasmic exclusion body contains the excess DNA from the oocyte formed during meiosis 2 at fertilization.
- secondary follicles - the stage following primary in the description of the sequence ovarian follicle development.
- stromal cells - in the ovary, cells surrounding the developing follicle that form a connective tissue sheath (theca folliculi). This layer then differentiates into 2 layers (theca interna, theca externa). This region is richly vascularized and involved in hormone secretion.
- superovulation therapy - a fertility drug treatement (oral clomiphene citrate and/or injectable FSH with or without LH) aimed at stimulating development/release of more than one follicle during a single menstrual cycle.
- tertiary follicle - (preovulatory, Graffian) the stage following secondary in the description of the sequence ovarian follicle development.
- theca folliculi - stromal cells in the ovary, cells surrounding the developing follicle that form a connective tissue sheath. This layer then differentiates into 2 layers (theca interna, theca externa). This region is vascularized and involved in hormone secretion.
- theca externa - stromal cells forming the outer layer of the theca folliculi surrounding the developing follicle. Consisting of connective tissue cells, smooth muscle and collagen fibers.
- theca interna - stromal cells forming the inner layer of the theca folliculi surrounding the developing follicle. This vascularized layer of cells respond to LH (leutenizing hormone) synthesizing and secreting androgens which are processed into estrogen.
- transzonal projection - (TZP) ovarian follicle term describing the cellular membraneous extension from the granulosa cell through the zona pellucida to the oocyte cell membrane where it forms gap junctions or adherens junctions allowing signalling and adhesion between the two cells.
- tunica albuginea - dense connective tissue layer lying near the ovary surface, a layer of simple squamous to cuboidal epithelial covers this layer. A similar named structure is found in male genital system.
- uterus - site of embryo implantation and development. Uterine wall has 3 major layers: endometrium, myometrium, and perimetrium. Endometrium can be further divided into the functional layer (shed/lost during menstruation) and basal layer (not lost during menstruation).
- zinc sparks following fertilization the oocyte releases a burst of zinc atoms in brief bursts (zinc sparks) has a role in zonal pellucida induced structural changes (hardening) along with ovastacin cleavage of ZP2 protein.
- zona hardening - following fertilization the structural changes that occur to the zona pellucida to prevents further spermatozoa binding acting as a block to polyspermy.
- zona pellucida - extracellular layer lying directly around the oocyte underneath follicular cells. Has an important role in egg development, fertilization and blastocyst development. This thick extracellular matrix consists of glcosaminoglycans and 3 glycoproteins (ZP1, ZP2, ZP3). (More? Zona pellucida)
|
Mammary Gland
| Tanner Stages (Expand to open)
|
Tanner Stages
| Tanner Stage
|
Genitals (male)
|
Breasts (female)
|
Pubic hair (male and female)
|
| I
|
prepubertal (testis volume < 1.5 ml
small penis (3 cm or less)
(age 9 and younger)
|
no glandular tissue
areola follows the skin contours of the chest (prepubertal)
(age 10 and younger)
|
no pubic hair at all (prepubertal state)
(age 10 and younger)
|
| II
|
testis volume 1.6 to 6 ml
skin on scrotum thins, reddens and enlarges
penis length unchanged
(age 9–11)
|
breast bud forms
with small area of surrounding glandular tissue
areola begins to widen
(age 10–11.5)
|
small amount of long, downy hair with slight pigmentation at the base of the penis and scrotum (males) or on the labia majora (females)
(age 10–11.5)
|
| III
|
testis volume 6 to 12 ml
scrotum enlarges further
penis begins to lengthen to about 6 cm
(age 11–12.5)
|
breast begins to become more elevated
and extends beyond the borders of the areola, which continues to widen but remains in contour with surrounding breast
(age 11.5–13)
|
hair becomes more coarse and curly
begins to extend laterally
(age 11.5–13)
|
| IV
|
testis volume 12 to 20 ml
scrotum enlarges further and darkens
penis increases in length to 10 cm and circumference
(age 12.5–14)
|
increased breast size and elevation
areola and papilla form a secondary mound projecting from the contour of the surrounding breast
(age 13–15)
|
adult–like hair quality
extending across pubis but sparing medial thighs
(age 13–15)
|
| V
|
testis volume > 20 ml
adult scrotum and penis of 15 cm in length
(age 14+)
|
breast reaches final adult size
areola returns to contour of the surrounding breast
with a projecting central papilla
(age 15+)
|
hair extends to medial surface of the thighs
(age 15+)
|
|
|
Note that while typical ages are shown in brackets within the table, this is not a system for determining age.
Based upon W.A. Marshall and J.M. Tanner, published stages for girls (1969[2]) and boys (1970[3]).
Links: Tanner stages | puberty | genital | Female | Male
|
|
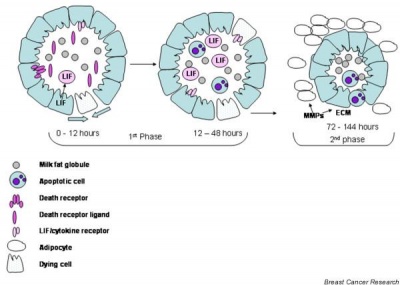
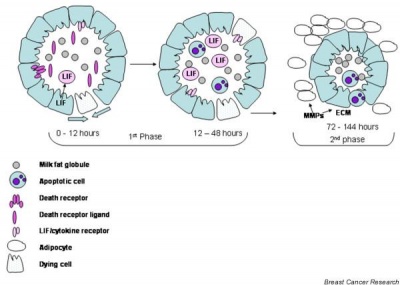
After the infant ceases breast feeding, weaning, the mammary gland milk-producing epithelial cells undergo a process called "involution", that requires cell apoptosis (programmed cell death).
Breast Cancer
In 1994, two breast cancer susceptibility genes were identified BRCA1 on chromosome 17 and BRCA2 on chromosome 13.
When an individual carries a mutation in either BRCA1 or BRCA2, they are at an increased risk of being diagnosed with breast or ovarian cancer at some point in their lives. Normal function of these genes was to participate in repairing radiation-induced breaks in double-stranded DNA. It is though that mutations in BRCA1 or BRCA2 might disable this mechanism, leading to more errors in DNA replication and ultimately to cancerous growth. (text modified from: NCBI genes and disease)
References
- ↑ Wallace WH & Kelsey TW. (2010). Human ovarian reserve from conception to the menopause. PLoS ONE , 5, e8772. PMID: 20111701 DOI.
- ↑ Marshall WA & Tanner JM. (1969). Variations in pattern of pubertal changes in girls. Arch. Dis. Child. , 44, 291-303. PMID: 5785179
- ↑ Marshall WA & Tanner JM. (1970). Variations in the pattern of pubertal changes in boys. Arch. Dis. Child. , 45, 13-23. PMID: 5440182
BGDA: Lecture 1 | Lecture 2 | Practical 3 | Practical 6 | Practical 12 | Lecture Neural | Practical 14 | Histology Support - Female | Male | Tutorial
Glossary Links
- Glossary: A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | Numbers | Symbols | Term Link
Cite this page: Hill, M.A. (2026, March 1) Embryology BGDA Practical - Female Reproductive Tract Histology. Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/BGDA_Practical_-_Female_Reproductive_Tract_Histology
- What Links Here?
- © Dr Mark Hill 2026, UNSW Embryology ISBN: 978 0 7334 2609 4 - UNSW CRICOS Provider Code No. 00098G