ANAT2241 Lymphatic Tissue and Immune System
| ANAT2241 This practical support page content is not part of the virtual science practical class and provides additional information for student self-directed learning purposes. All practical class pages are located on Moodle - ANAT2241 |
General Objective
To know the structure and function of lymphoid tissues and organs.
Specific Objectives
- To know the two principal components of lymphatic tissue: reticular tissue (reticular cells, reticular fibres, macrophages) and lymphatic cells.
- To recognise the different arrangements of lymphatic tissue in the different organs: diffuse and nodular (follicular) lymphatic tissue, lymph nodes, and tonsils.
- To describe the structure of a lymph node and to identify cortex, medulla, trabeculae, medullary cords and sinusoidal system. To know the significance of the paracortical zone of the node.
- To describe the microanatomy of the spleen, including red and white pulp, blood vessels of red and white pulp, splenic sinusoids and cells.
- To describe the structure of the thymus gland and its morphological changes during development.
- To appreciate the differences between T-lymphocytes and B-lymphocytes.
Learning Activities
Examine the following virtual slides, identify, draw and label the features listed and note their function where appropriate:
Virtual Slides: Lymphatic Tissue and Immune System
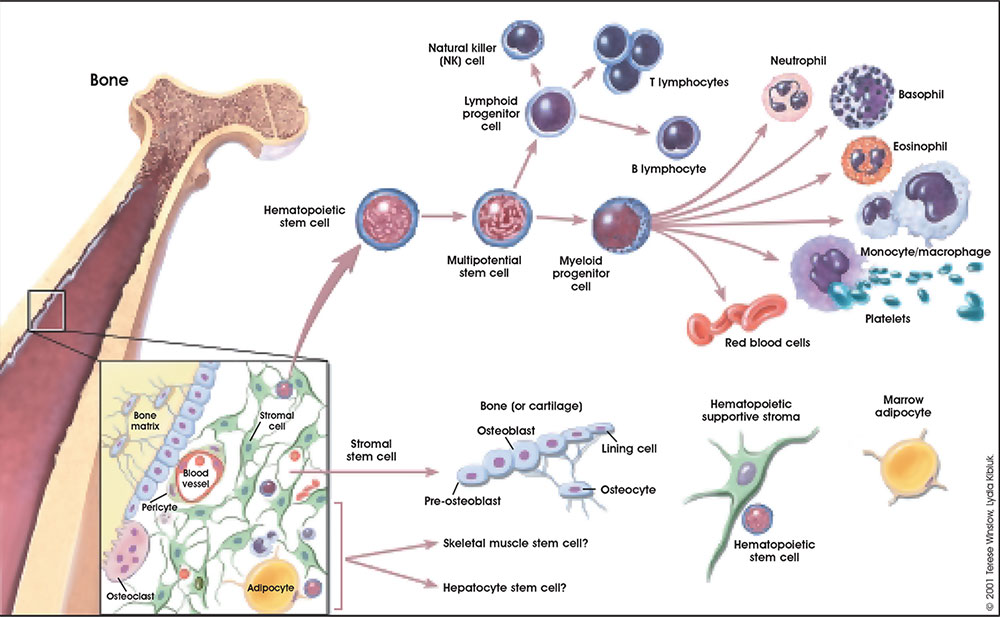
The circulating blood is a liquid connective tissue consisting of cells (red and white blood cells), fragments of cells (platelets) and liquid (plasma). The different cell types are all derived from haemopoietic stem cells located in the bone marrow. Red blood cells (RBCs) have a metabolic role, in carrying oxygen to tissues and carbon dioxide to the lungs. White blood cells (WBCs or leukocytes) have a role in the body’s defence, and are an important clinical indicator of disease.
Find an area in the smear where the red blood cells are spread out and individual cells can be identified.
Identify:
- Red blood cells (7-8 um diameter anucleate biconcave disc)
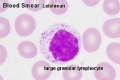
- White blood cells: neutrophils, eosinophils, basophils, lymphocytes and monocytes (basophils are normally rare).
Note the presence or absence of granules, shape of the nucleus and relative cell sizes. Also identify platelets.
Virtual Slide Box: 2. Bone Marrow Smear Slide
- Do not attempt to identify all the cells in the bone marrow smear, but compare its appearance with that of the blood smear.
- Haematopoiesis (hematopoiesis) is the process of blood cell differentiation and occurs mainly in the bone marrow.
- This bone marrow smear will contain a large number of differentiating blood cells: band cells and normoblasts.
- The largest cells visible are megakaryocytes, which are responsible for platelet production.
Lymphocyte differentiation begins in the bone marrow and continues in central lymphoid organs (bone marrow - B cells and thymus - T cells), then in the peripheral lymphoid organs (lymph nodes, spleen).
Blood Histology
Lymphocyte Electron Micrographs
- Blood Histology: Blood Development | Blood Cell Number Table | Lymphocyte 1 | Lymphocyte 2 | Lymphocyte 3 | Lymphocyte 4 | Monocyte 1 | Monocyte 2 | Monocyte 3 | Monocyte 4 | Neutrophils 1 | Neutrophil 2 | Neutrophil 3 | Neutrophil 4 | Eosinophil 1 | Eosinophil 2 | labeled Neutrophil and Eosinophil | unlabeled - Neutrophil and Eosinophil | Basophil 1 | Basophil 2 | Basophil 3 | Platelet 1 | Platelet 2 | Reticulocyte | Megakaryocyte | Movie | Bone Marrow Histology | Category:Blood
| Blood Cells |
|---|
Adult human blood cell numbers shown in the table below is for reference purposes.
Blood Cell NumbersThe adult ranges of cells / 1 litre (l), total blood volume is about 4.7 to 5 litres. Blood Development | Blood Histology Red Blood Cells
Leukocytes (white blood cells)
Granulocytes
Non-Granulocytes
Lymphocytes
Platelets
|
- Bone Marrow Histology: Blood Development | Marrow overview | Megakaryocyte | Megakaryocyte detail | Myelocyte | Normoblast | Reticulocyte | Blood Histology | Bone Development | Category:Blood
Blood Questions
- What is the normal blood haematocrit range?
- Does this haematocrit differ for male/female?
- What is the function of the various blood cells?
- Which tissues have very large numbers of white blood cells and why?
- In histology tissue sections which blood vessel (artery/vein) is more likely to contain blood cells?
Lymphoid Tissue
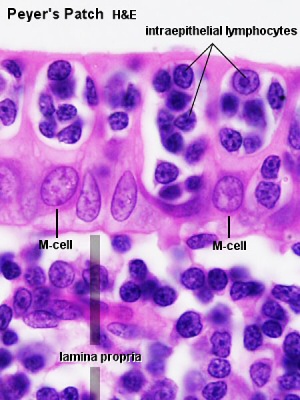
Lymphoid (or lymphatic) tissues consist of dense accumulations of lymphocytes in many different body regions, typically at sites that provide a route of entry of pathogens or sites that are prone to infections. Depending on their precise location these lymphoid tissues may be epithelia associated and referred to as mucosa-associated lymphoid tissue (MALT) or bronchus-associated lymphoid tissue (BALT). The gastrointestinal tract tonsils and Peyer's patches are examples of mucosa-associated lymphoid tissues.
Thymus
Virtual Slide Box: 3. Infant Thymus slide
Section of a thymus lobe of an infant.
The thymus changes its histological appearance from infant to puberty to adult, in a process called involution (replacement of cortical lymphoid tissue by adipose tissue) and there is also an increase in the size of thymic corpuscles.
At low magnification: note the surrounding connective tissue capsule along the surface. The thymus is divided into many smaller lobules by connective tissue septa extending inward from the capsule. These lobues have a cortex (dark staining) and a medulla (pale staining). The interlobular septa do not penetrate into the medulla, and lobules are joined together in the medulla. Some septa may carry blood vessels and efferent lymphatic vessels.
At high magnification: Cortex has a dense layer of closely packed cells (developing and maturing T lymphocytes, thymocytes). Medulla consist of an eosinophilic central mass surrounded by concentrically arranged epithelial cells (Hassalls corpuscles). Do not confuse them with blood vessels.
Compare the appearance of the infant with the adult thymus (below).
Blood-Thymic Barrier
Spleen

Virtual Slide Box: 5. Spleen
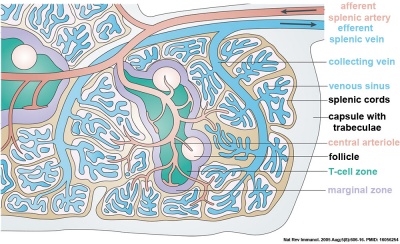
The spleen in fetal life is a site for blood formation (hematopoiesis). The adult spleen has 2 main functions: immune, as a major site of antigen presentation for the circulation system and removal of aged erythrocytes from the circulation. The spleen has a dense connective tissue capsule, which contains trabeculae running into the interior of the spleen forming incomplete compartments (as in the thymus). The stroma is mainly composed of reticular connective tissue and cells. There is a Hilum, which contains arteries and veins, but unlike a lymph node, there are no lymphatics. It should also be noted that the spleen cannot be divided into a medulla and cortex, which helps differentiate it from the thymus or a lymph node.
The spleen is a major site of antigen presentation for the circulation system, and in fetal life, it is a site for hematopoiesis. It also functions in removing senescent erythrocytes from the circulation. The spleen is surrounded by a dense connective tissue capsule, which contains trabeculae running into the interior of the spleen forming incomplete compartments. The stroma is mainly composed of reticular connective tissue and cells. There is a Hilum, which contains arteries and veins, but unlike a lymph node, there are no lymphatics. It should also be noted that the spleen cannot be divided into a medulla and cortex, which helps differentiate it from the thymus or a lymph node.
| Spleen Overview | Red Pulp |
|---|---|
|
|
Identify connective tissue capsule, trabeculae, white pulp, red pulp, lymphatic nodules, and central arterioles.
The two main interior divisions of the spleen are white and red pulp.
White pulp (Malpighian follicles, white nodules, splenic lymphoid nodules) consists of a sheath of lymphoid cells surrounding an eccentrically located central arteriole. The T lymphocytes immediately surrounding the central arteriole are referred to as periarterial lymphatic sheaths (PALS). Surrounding that is a layer of peripheral white pulp (PWP), which is composed of B lymphocytes. Antigen enters the white pulp from the central arteriole, activates the PALS, which then activates the PWP. The marginal zone on the periphery of the white pulp is believed to be an important area for trapping antigens and initiation of immune responses. Both lymphocytes and macrophages are present in the marginal zone.
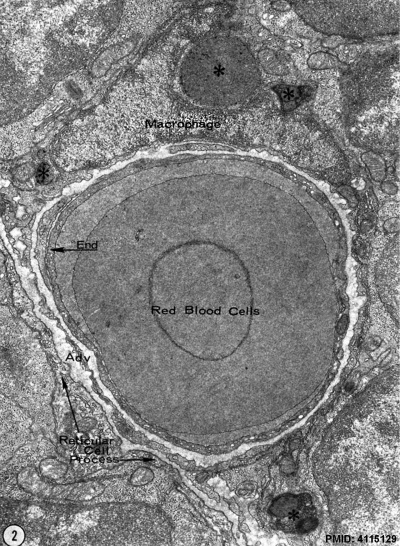
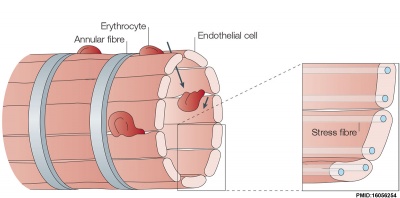
The red pulp consists of splenic cords of Billroth and splenic sinusoids. The splenic cords of Billroth contain reticular cells, macrophages, lymphocytes, plasma cells, and erythrocytes. The splenic sinusoids are modified capillaries with an exceptionally wide lumen and spaces in the wall to allow cells to squeeze in and out. Macrophages are also able to extend processes into the sinusoid, allowing them to identify senescent red blood cells.
Blood enters the spleen via the splenic artery at the hilum. The blood then travels through the trabecular arteries, central arterioles, penicillar arterioles, capillaries, splenic sinusoids, trabecular veins, and finally out the splenic vein at the hilum. Virtual Slide Box: 5. Spleen
(monkey silver stain)
Spleen silver-stained to show connective tissue reticular fibers (black), compare this with the silver-stained lymph node.
- Spleen Histology
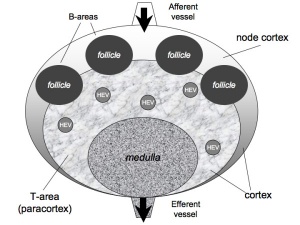
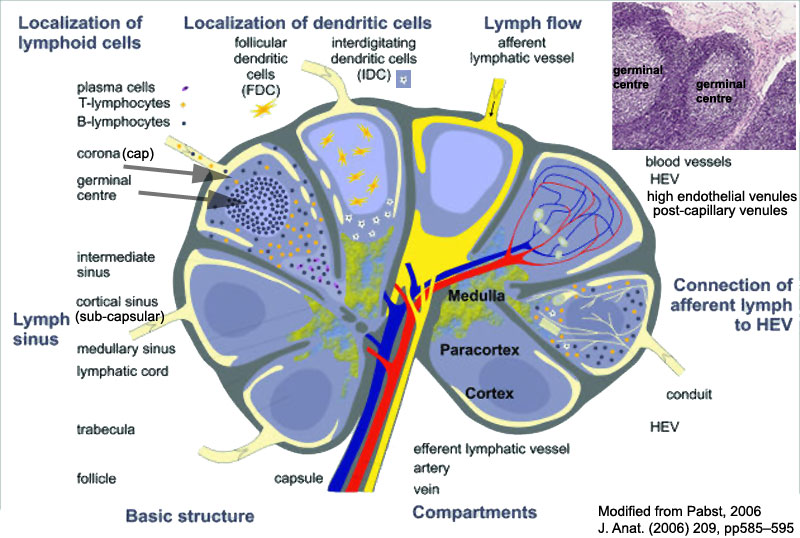
Lymph Node
- Lymph Node Histology: Subcapsular Sinus | Follicle | Germinal Centre | Medullary Cords and Sinuses | High Endothelial Venules | Macrophages | Node cartoons
Virtual Slide Box: 6. Lymph Node
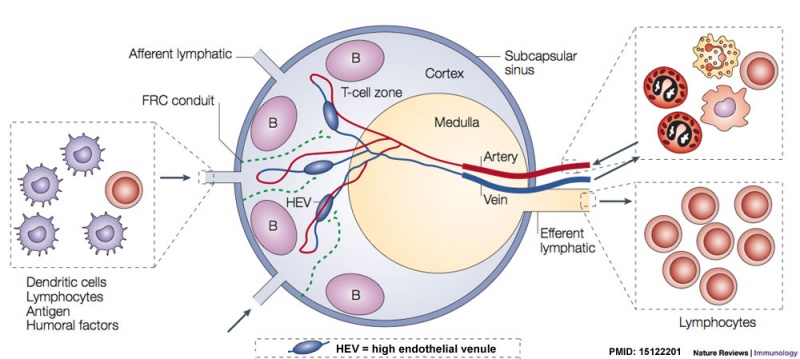
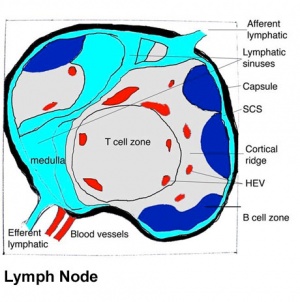
Lymph nodes are peripheral lymphoid organs involved in helping the body defend against foreign organisms. Lymph, which contains antigen and antigen presenting cells, flows from local tissue lymphatic vessels and enters the subcapsular sinus. The lymph then filters though the intermediate sinuses, into the medullary sinuses, and finally out the efferent lymphatic vessels at the hilum before it is returned to the circulation. B and T cells are numerous in the lymph node, and they enter through afferent arteries, enter the lymphoidal tissue across specialized vessels called high-endothelial venules, and return to the circulation via efferent veins.
Identify the following features: the connective tissue capsule, the trabeculae, the subcapsular sinus (lying immediately below the capsule), the intermediate sinus (lying next to a trabecula), outer cortex (composed of lymphatic nodules follicles), the inner cortex (non-nodular area between outer cortex and medulla) and the medulla (with medullary cords and medullary sinuses).
Virtual Slide Box: 7. Lymph Node (silver stain)
Lymph node silver stained to show connective tissue reticular fibers (black).
Identify reticular fiber distribution in: capsule, trabeculae, subcapsular sinuses, intermediate sinuses, lymphoid nodules, the inner cortex, and the medulla.
- Lymph Node Histology: Subcapsular Sinus | Follicle | Germinal Centre | Medullary Cords and Sinuses | High Endothelial Venules | Macrophages | Node cartoons
| <html5media height="400" width="400">File:Mouse_adult_lymph_node_03.mp4</html5media> | Adult Mouse Lymph Node - T cells within the medullary sinus.
Passive, unidirectional flow of T cells within the medullary sinus. |
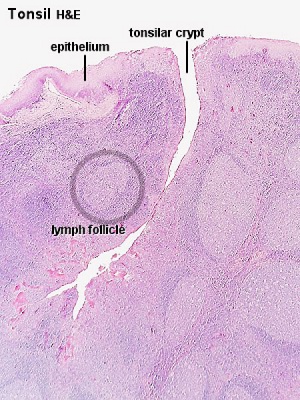
Tonsil
Virtual Slide Box: 8. Lingual tonsil (tongue)
The lingual tonsils are numerous small tonsils located at the base of the tongue. They are covered by a stratified squamous epithelium, but are not enclosed by a capsule. Salivary glands and skeletal muscle are directly adjacent to the tonsil.
Virtual Slide Box: 9. Pharyngeal tonsil
Closely packed lymph nodules comprise the outer portion of this organ. The pharyngeal tonsil is covered with a pseudostratified columnar epithelium with cilia (typical of respiratory tract).
Virtual Slide Box: 10. Appendix
The appendix (vermiform appendix) anatomy is as a finger-like structure that arises from the cecum. The length (2.5-13 cm) is longer in both infants and children and also has more abundant lymphatic tissue in early life. The wall structure is similar to the small intestine (though with no villi), nor plicae circularis.
Lymph nodules surround the lumen of the gastrointestinal tract and extend from the mucosa into the submucosa. Note in this section most of the muscularis mucosa has been obliterated by lymphatic invasion.
- Immune Images: Oesophagus MALT | Colon MALT | Peyer's patch overview | Peyer's patch detail | Cartoon - IEL development | Cartoon - IEL function | Cartoon - IEL differentiation | Mesenteric Lymph Nodes overview | Palatine Tonsil | Tonsil | Immune System Development
Lymphatic Questions
- What is the difference between stroma and parenchyma?
- Which cells make reticular fibers?
- Why are lymphoid tissues associated with the gastrointestinal tract and respiratory tissues?
- What is an antigen and what does it produce in the immune system?
- Where can tonsilar tissue be found in the gastrointestinal tract?
Terms
A few key terms associated with the Lymphoid system.
- adenoid - (Greek " +-oeides = in form of) in the form of a gland, glandular; the pharyngeal tonsil.
- Afferent lymph - vessel carrying lymph towards a node.
- anastomose - joining of two tubes or structures together.
- Antibody mediated immunity - the immune function of plasma cells (active B lymphocytes) secreting antibody which binds antigen.
- antibodies - mammals have five classes (IgA, IgD, IgE, IgG, and IgM)
- antigen - any substance that is recognised by the immune system and stimulates antibody production.
- appendix - is a gut-associated lymphoid tissue (GALT) located at the beginning of the colon. The anatomy is as a finger-like structure that arises from the cecum. The length (2.5-13 cm) is longer in both infants and children and also has more abundant lymphatic tissue in early life. The wall structure is similar to the small intestine (though with no villi), nor plicae circularis. Lymph nodules surround the lumen of the gastrointestinal tract and extend from the mucosa into the submucosa.
- B lymphocyte (cell) - historically named after a structure called the bursa of Fabricius in birds, a source of antibody-producing lymphocytes. These cells develop in the bone marrow. (More? Electron micrographs of nonactivate and activated lymphocytes)
- BALT - Bronchus Associated Lymphoid Tissue
- band cell - (band neutrophil or stab cell) seen in bone marrow smear, a cell undergoing granulopoiesis, derived from a metamyelocyte, and leading to a mature granulocyte. Also occasionally seen in circulating blood.
- cecum - (caecum, Latin, caecus = "blind") within the gastrointestinal tract a pouch that connects the ileum with the ascending colon of the large intestine.
- cell - has a specific cell biology definition, but is often used instead of "lymphocyte" when describing B and T cells.
- Cell-mediated immunity - the immune function of T lymphocytes.
- "clockface" - a term used to describe the appearance of plasma cell nuclei due to the clumping of the chromatin at the nucleus periphery. More clearly seen in tissue plasma cells that the bone marrow smear, where they are sometimes confused with the basophilic erythroblasts.
- cords of Billroth - spleen cellular columns located in red pulp. surrounded by splenic sinusoids. Cords contain reticular cells, macrophages, lymphocytes, plasma cells and erythrocytes.
- cortex - outer layer, used in association with medulla (innner layer or core) a general description that can be applied to describing an organ with a layered structure.
- dendritic cell - (DC, antigen-presenting cell, APC) cells that present antigens and induce a primary immune response in resting naïve T lymphocytes. In 2011 Ralph M. Steinman received half the Nobel Prize half of the award to to Ralph M. Steinman for his discovery of the dendritic cell and its role in adaptive immunity.
- Effector cells - the immune functioning (active) B and T lymphocytes.
- Efferent lymph - vessel carrying lymph away from a node.
- GALT - Gut Associated Lymphatic Tissue
- haemopoiesis (hemopoiesis) formation of blood cells.
- Hassall's corpuscle - thymic corpuscle.
- high endothelial venule - (HEV) the specialised post-capillary venous region that enables blood lymphocytes to enter a lymph node.
- IgA - the main class of antibody in secretions (saliva, tears, milk, and respiratory and intestinal secretions).
- IgD - the immunoglobulin B cell starts to produce as a cell-surface molecule after leaving the bone marrow.
- IgE - bind Fc receptors (surface of mast cells in tissues and basophils in the blood).
- IgG - the major class of immunoglobulin in the blood.
- IgM - the first class of antibody made by a developing B cell, which may switch to making other classes of antibody.
- immunodeficiency - when one or more components of the immune system is defective. (More? Immunobiology - immunodeficiency)
- involution - in the thymus refers to the replacement, mainly in the cortex, of cells by adipose tissue. (More? PubMed- thymus involution) | Cancer Medicine - Thymomas and Thymic Tumors)
- lamina propria - a layer of loose connective tissue found underneath the epithelium of mucosa.
- Leukocyte- (Greek, lukos= clear, white) white blood cell.
- lingual- related to the tongue.
- lymph node - connective tissue encapsulated lymphoid organ (1mm - 2cm in size), positioned in the pathway of lymph vessels.
- M cell - (microfold cell) found in the follicle-associated epithelium of the Peyer's patch. Function to transport gut lumen organisms and particles to immune cells across the epithelial barrier.
- macrophage - a large highly motile white blood cell which engulfs foreign material (bacteria etc) and both degenerating cells and cell fragments. Differentiates from a monocyte and found in many different tissues and locations. (More? Immunobiology - Defects in phagocytic cells are associated with persistence of bacterial infection)
- MALT - Mucosa Associated Lymphoid Tissue
- medulla - inner layer or core, used in association with cortex (outer layer) a general description that can be applied to describing an organ with a layered structure.
- Memory Cell - effector T cell (lymphocyte)
- normoblast - seen in bone marrow smear, a developing erythroblast (red blood cell) that still retains a nucleus.
- parenchyma - (Greek = enkeim "to pour in") cells forming the functional cells of an organ or tissue. These cells carry out the function of the organ at a cellular level, and are not the structural cells, connective tissue, extracellular matrix (stromal).
- periarterial lymphoid sheath - (PALS) in the spleen the white pulp that surrounds the central arteries. (T-lymphocytes,macrophages and plasma cells)
- Plasma Cell - active B cell (lymphocyte) which is secreting antibody. Located in either bone marrow or peripheral lymphoid tissues, these cells have and increased cytoplasmic volume (due to increase rough endoplasmic reticulum) in comparison to the inactive (non-secreting) lymphocyte.
- sentinel lymph node - the hypothetical first lymph node or group of nodes reached by metastasizing cancer cells from a primary tumour.
- splenic sinusoids - enlarged spleen capillary spaces located in red pulp and surrounding cords of Billroth.
- stroma - (Greek = "a cover, table-cloth, bedding") tissue forming the framework/support of an organ or tissue. That is the structural cells which form connective tissue and secrete extracellular matrix, rather than the functional cells (parenchymal). All organs can therefore be functionally divided into these 2 components, stromal/parenchymal.
- Subcapsular sinus (=marginal sinus) space lying under the connective tissue capsule which receives lymph from afferent lymphatic vessels.
- Thymic corpuscle (=Hassall's corpuscle) a mass of concentric epithelioreticular cells found in the thymus. The number present and size tend to increase with thymus age. (see classical description of Hammar, J. A. 1903 Zur Histogenese und Involution der Thymusdriise. Anat. Anz., 27: 1909 Fiinfzig Jahre Thymusforschung. Ergebn. Anat. Entwickl-gesch. 19: 1-274.)
- thymic epitheliocytes - reticular cells located in the thymus cortex that ensheathe the cortical capillaries, creating and maintain the microenvironment necessary for the development of T-lymphocytes in the cortex.
- T lymphocyte (cell) - named after thymus, where they develop, the active cell is responsible for cell-mediated immunity. (More? Electron micrographs of nonactivate and activated lymphocytes)
- thymus - an immune/endocrine (thymic hormone) organ involved in the maturation of T lymphocytes (T-cells). Thymus Development
- tonsils - lymph nodules embedded in the mucus membranes located at the back of the mouth and top of the throat. The overlying epithelium helps identify the location.
- vermiform appendix - see appendix, anatomical region containing gut-associated lymphoid tissue located within the gastrointestinal tract at the beginning of the colon. The anatomy is as a finger-like structure that arises from the cecum. The length (2.5-13 cm) is longer in both infants and children and also has more abundant lymphatic tissue in early life. The wall structure is similar to the small intestine (though with no villi), nor plicae circularis. Lymph nodules surround the lumen of the gastrointestinal tract and extend from the mucosa into the submucosa.
Course Links
- Histology Glossary: A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | ANAT2241 Support | Histology | Histology Stains | Embryology Glossary
| Common Histology Stains | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Practical Support
- Pages can be accessed from any internet connected computer.
ANAT2241 Support Links: The Virtual Microscope | Covering and Lining Epithelia | Glandular Epithelia | CT Components | CT Types | Bone, Bone Formation and Joints | Muscle | Nervous | Blood | Eye | Cardiovascular | Respiratory | Integumentary | Gastrointestinal | Gastrointestinal Organs | Lymphatic and Immune | Endocrine | Urinary | Female Reproductive | Male Reproductive | Histology Stains | Histology Drawings | Practicals Health and Safety 2013 | Moodle - 2019
ANAT2241 This practical support page content is not part of the science practical class and provides only background information for student self-directed learning purposes.
Cite this page: Hill, M.A. (2024, April 28) Embryology ANAT2241 Lymphatic Tissue and Immune System. Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/ANAT2241_Lymphatic_Tissue_and_Immune_System
- © Dr Mark Hill 2024, UNSW Embryology ISBN: 978 0 7334 2609 4 - UNSW CRICOS Provider Code No. 00098G