Hearing - Middle Ear Development: Difference between revisions
(→Stapes) |
(→Stapes) |
||
| Line 148: | Line 148: | ||
'''Stapes Development''' (timing from <ref name=PMID"18581276"><pubmed>18581276</pubmed></ref>) | '''Stapes Development''' (timing from <ref name=PMID"18581276"><pubmed>18581276</pubmed></ref>) | ||
* 28 weeks - tympanic membrane of the stapes footplate undergoes a remodelling process with bony trabeculae deposited | * 28 weeks - tympanic membrane of the stapes footplate undergoes a remodelling process with bony trabeculae deposited | ||
|} | |||
{| | {| | ||
|+ '''Adult Stapes Anatomy''' | |+ '''Adult Stapes Anatomy''' | ||
Revision as of 15:39, 20 May 2011
Introduction
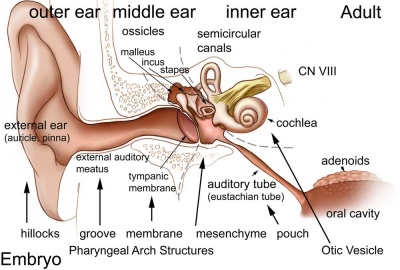
The middle ear bones (ossicles) are derived from first and second arch mesenchyme and the space in which these bones sit is derived from the first pharyngeal pouch.
Some Recent Findings
|
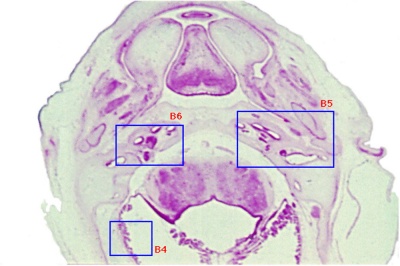
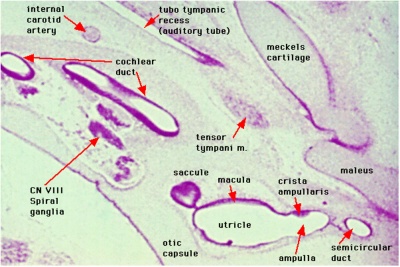
Week 8
Cross-section of human embryo Carnegie stage 22 during Week 8.
Middle ear structure visible are the primordial maleus, the developing tensor tympani muscle, the developing auditory tube (tubo tympanic recess) extending from the oral cavity towards the middle ear region. Note the ossicle is still embedded, and surrounded by, the mesenchyme of the head.
Ossicles
Middle ear development begins closely associated with head formation and involves both the foregut tube (pharynx) and the pharyngeal arches. Pharyngeal arches form the main anatomical structures of the head and neck, including all components of the middle and outer ear.
The three middle ear bones or auditory ossicles (malleus, incus, stapes) are formed from the cartilage template found within pharyngeal arch 1 and 2. These bones are commonly named the hammer (malleus), anvil (incus) and stirrup (stapes), and the cartilage bands are historically named after two German anatomists and are called Meckel’s cartilage (first pharyngeal arch; named after Johann Friedrich Meckel, 1781–1833) and Reichert’s cartilage (second pharyngeal arch; named after Karl Bogislaus Reichert, 1811–1883). There are several theories as to how each arch cartilage contributes individual components of the middle ear ossicles. For example, a recent study suggests a mesenchymal origin for the stapes rather than directly from Reichert's cartilage.[2] Meckel’s cartilage first appears histologically at Carnegie stage 16 and Reichert’s cartilage slightly later.
The early stages of auditory ossicle development all occur within the solid mesenchyme of the pharyngeal arches until the eighth month of development, then within a fluid-filled space for the final month, and finally only postnatal in the neonate in the air-filled tympanic cavity. This transition in auditory ossicle environment means that the middle ear does not function correctly until after birth, and any prenatal conduction to the cochlea must be mediated through bone conduction.
During development of the tympanic cavity, the auditory ossicles are held in their correct anatomic positions by supporting ligaments. Arch cartilages ossify by the process of endochondral ossification, where a pre-existing cartilage template is first formed and later replaced by bone. Endochondral ossification is the main process of bone formation throughout the entire skeleton, except for the cranial vault and the clavicle that ossify by a process of intramembranous ossification.
Initially, the malleus and incus form as a single structure, and it is only later that they separate to form two separate bones. Ossification continues through the entire fetal period, and the newly formed bones also have a transient bone marrow cavity. The marrow cavity is still present at birth, in both the malleus and the incus, and with continued ossification is lost during the first two years after birth. Postnatally, first the malleus and then the incus lose their marrow spaces.
Malleus
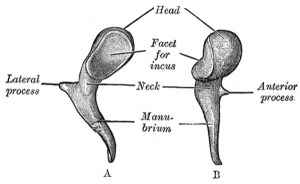
Malleus (left) A. From behind. B. From within. |
This ossicle was named from its resemblance to a hammer. The structure of the adult bone can be divided into a head, neck, and three processes (manubrium, anterior and lateral processes). In the fetus, of the three processes the anterior process is the longest and is in direct continuity with Meckel's cartilage. Malleus ossification is initiated in the fetal period.[3][4] The newborn and infant malleus head normally contains bone marrow, that is eventually replaced by bone.[5] Malleus Development (timing from [4])
|
| Component | Description | ||
| Head (capitulum mallei) | large upper extremity of the bone, oval in shape | articulates posteriorly with the incus, being free in the rest of its extent | facet for articulation with the incus is constricted near the middle (consists of an upper larger and lower smaller part nearly a right angle with each other) opposite the constriction (lower margin of the facet projects in the form of a process, cog-tooth or malleus spur) |
| Neck (collum mallei) | narrow contracted part, just beneath the head | below it is a prominence | various processes are attached to the prominence |
| Handle (manubrium mallei) | connected by its lateral margin with the tympanic membrane | directed downward, medialward, and backward | decreases in size toward its free end, which is curved slightly forward, and flattened transversely. Medial side, near its upper end, is a slight projection, into which the tendon of the tensor tympani is inserted |
| Anterior Process (processus anterior (Folii), processus gracilis) | delicate spicule from the eminence below the neck | directed forward to the petrotympanic fissure | to which it is connected by ligamentous fibers |
| Lateral Process (processus lateralis, processus brevis) | a slight conical projection from the root of the manubrium | directed laterally, and is attached to the upper part of the tympanic membrane | attached by means of the anterior and posterior malleolar folds, to the extremities of the notch of Rivinus. |
| (some text modified from Gray's Anatomy) |
Incus
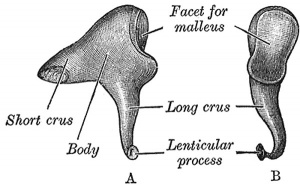
Incus (left) A. From within. B. From the front |
Originally named from resemblance to an anvil, onsists of a body and two crura.
The two crura diverge from one another nearly at right angles. Gray suggested the incus has more like a "premolar tooth" appearance, with two roots, which differ in length, and are widely separated from each other. Incus ossification is initiated in the fetal period.[6] The newborn and infant incus body normally contains bone marrow, that is eventually replaced by bone.[7] |
| Component | Description | ||
| Body (corpus incudis) | somewhat cubical but compressed transversely | anterior surface is a deeply concavo-convex facet | facet articulates with the head of the malleus |
| Short Crus (crus breve, short process) | somewhat conical in shape | projects almost horizontally backward | attached to the fossa incudis, in the lower and back part of the epitympanic recess |
| Long Crus (crus longum, long process) | descends nearly vertically behind and parallel to the manubrium of the malleus | bending medialward, ends in a rounded projection, the lenticular process | lenticular process is tipped with cartilage, and articulates with the head of the stapes |
Stapes
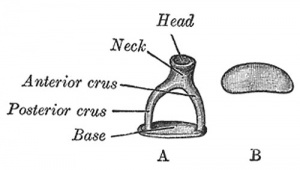
A. Left stapes. B. Base of stapes, medial surface. |
Originally named by its resemblance to a stirrup and structurally consists of a head, neck, two crura, and a base. Stapes Development (timing from [4])
|
| Component | Description | |
| Head (capitulum stapedis) | presents a depression, which is covered by cartilage | articulates with the lenticular process of the incus |
| Neck | constricted part of the bone, succeeding the head | gives insertion to the tendon of the Stapedius muscle |
| Two crura (crus anterius and crus posterius) | diverge from the neck , connected at their ends by a flattened oval plate | anterior is shorter and less curved than the posterior |
| Base (basis stapedis) | forms the foot-plate of the stirrup | fixed to the margin of the fenestra vestibuli by a ring of ligamentous fibers |
Middle Ear Muscles
The middle ear also contains the two smallest muscles of the body, the stapedius and tensor tympani muscles, which both differentiate from arch mesenchyme. These muscles form and differentiate in a similar fashion to other developing skeletal muscle. Initially myoblasts proliferate under the influence of growth factors in the region of where the muscle will form. Myoblasts are the embryonic undifferentiated single cells of all skeletal muscles.
- The adult tensor tympani is classed as a mixed muscle containing slow (type 1) and fast (type 2A, and probably 2X) muscle fibers.
- The adult mammalian stapedius muscle contains mainly (77%) fast oxidative glycolytic type muscle fibers and the avian muscle only contains fast fibers.
A recent study[8] of the stapedius region (see table below) and muscle development in 50 human embryos and fetuses between 38 days to 17 weeks post-conception identified 2 origins:
- for the tendon - derives from the internal segment of the interhyale
- for the belly - located in the second pharyngeal arch, medially to the facial nerve and near the interhyale
interhyale - term describing the internal part of the second pharyngeal arch that forms the tendon of the stapedius muscle
| Stage | CRL (mm) | Description |
| 13 | 6 | Presumptive stapedial area |
| 14 | 7 | Appearance of the stapedial anlage |
| 16 | 9 | Relationship between the stapedial artery and the stapedial anlage. Appearance of the interhyale |
| 17 | 12 | Delimitation of the parts of the stapedial anlage |
| 18 | 16 | Chondrogenesis phase. Start of involution of the stapedial artery |
| 20 | 18.5 | Delimitation of the ossicular anlages. Cartilaginous phase. Disappearance of the stapedial artery |
| 22 | 26 | Delimitation of the interhyale |
| 23 | 28 | Anlage of the stapedial muscle tendon |
| Data summarised from Table 1[8] |
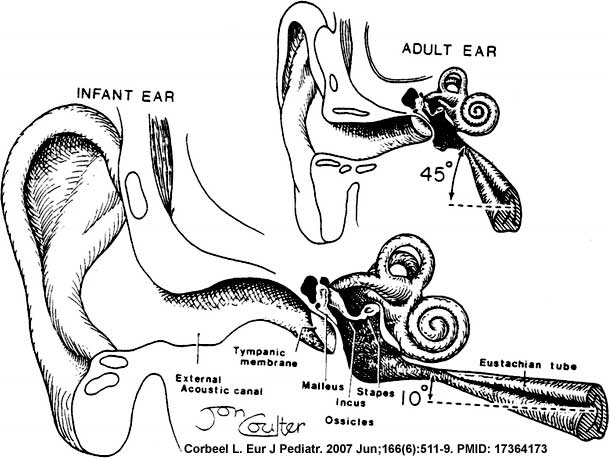
Tympanic Cavity
The auditory tube, eustachian tube (named after Bartolomeo Eustachi, 1500–1574), otopharyngeal or pharyngotympanic tube develops from the first pharyngeal pouch and is lined with endoderm. This narrow cavity links the pharynx to the middle ear and is continuous with the tympanic cavity. The auditory tube has two main functions: ventilation, to allow the equalization of pressure in the middle ear, and clearance, to allow the middle ear fluid continuously produced by the epithelial lining to drain from the middle ear.
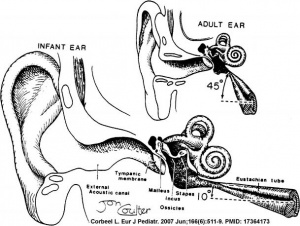
In normal human development, the auditory tube has an almost straight posterolateral to anteromedial pathway. The main growth of the auditory tube occurs in extension and lumen of the cartilaginous portion in the fetal period between weeks 16 to 28.
At birth, and in the young child, the tube is both shorter (8-9 mm) compared to the adult length (17-18 mm), runs almost horizontal and is narrower in diameter. Head growth in the child to adult size results in a longer wider tube that runs at approximately 45 degrees to the horizontal. The auditory tube is also normally closed and is opened by muscles—in the infant this is only a single muscle, the tensor palati muscle. In the adult the auditory tube is now opened by two separate muscles, the tensor palati and levator palati muscles.
he middle ear cavity or tympanic cavity is formed by an expansion of the pharynx. The initial early cavity lining is formed by the pharyngeal endoderm epithelium. The epithelium will then continue to expand, to eventually also line the entire mastoid antrum.
- derived from first pharyngeal pouch
- extends as tubotympanic recess - during week 5 recess contacts outer ear canal
- mesoderm between 2 canals forms tympanic membrane
- expands to form tympanic recess
- stalk of recess forms auditory tube(eustachian tube, pharyngotympanic tube)
Auditory Tube
(Eustachian, otopharyngeal or pharyngotympanic tube)
Connects middle ear cavity to nasopharynx portion of pharynx. Tube is normally closed and opened by muscles.
- Ventilation - pressure equalization in the middle ear
- Clearance - allow fluid drainage from the middle ear
Postnatal Changes
|
Adult
|
Adult Middle Ear
The adult middle ear, like the inner ear, eventually will lie within the petrous portion of temporal bone. Initially, both the middle and inner ear form within mesenchyme, embryonic connective tissue, forming the otic capsule, and this will also form the base of the skull. The mesenchyme differentiates first to form cartilage, forming a structure known as the chondrocranium. This initial cartilage is gradually replaced by bone forming at a number of sites within the cartilage, ossification centers. The initial bone that is formed also contains marrow spaces that disappear with ongoing ossification (Yokoyama et al., 1999). Between the weeks 16 to 24, centers of ossification appear in the remaining cartilage of the otic capsule, and these continue to ossify to eventually form mastoid process of temporal bone.
Ossicles
- develop from first and second pharyngeal arches
- tympanic cavity enlarges to incorporate
- coats with epithelia
- first arch mesoderm
- tensor tympani muscle
- malleus and incus
- second arch mesoderm
- stapedius muscle and stapes
Middle Ear Genes - gooscoid, RARs, Prx1, Otx2, Hoxa1, Hoxb1, endothelian related molecules
Additional Images
References
Reviews
<pubmed>21196256</pubmed>
Articles
<pubmed>21285435</pubmed>
Search PubMed
May 2010 "Middle Ear Development" All (2368) Review (226) Free Full Text (272)
Search Pubmed: Middle Ear Development | Ossicle Development | Malleus Development | Incus Development | Stapes Development
External Links
- Neuroscience Neuroscience - The Middle Ear
Glossary Links
- Glossary: A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | Numbers | Symbols | Term Link
Cite this page: Hill, M.A. (2024, May 2) Embryology Hearing - Middle Ear Development. Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/Hearing_-_Middle_Ear_Development
- © Dr Mark Hill 2024, UNSW Embryology ISBN: 978 0 7334 2609 4 - UNSW CRICOS Provider Code No. 00098G