ANAT2341 Lab 7
| Embryology - 6 May 2024 |
|---|
| Google Translate - select your language from the list shown below (this will open a new external page) |
|
العربية | català | 中文 | 中國傳統的 | français | Deutsche | עִברִית | हिंदी | bahasa Indonesia | italiano | 日本語 | 한국어 | မြန်မာ | Pilipino | Polskie | português | ਪੰਜਾਬੀ ਦੇ | Română | русский | Español | Swahili | Svensk | ไทย | Türkçe | اردو | ייִדיש | Tiếng Việt These external translations are automated and may not be accurate. (More? About Translations) |
Muscle Development
Introduction
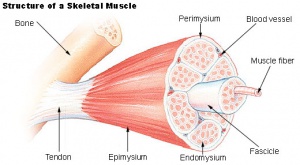
This laboratory concerns the development and differentiation of skeletal muscle, fibre type differentiation, muscle stem cells and muscle disease.
The histology of skeletal muscle has been covered in ANAT2241.
Objectives
- Understand the origin, differentiation and development of skeletal muscle tissue.
- Know what is meant by patterning, conversion and adult plasticity of muscle fibre type.
- Develop an understanding of research methods for studying skeletal muscle abnormalities.
Muscle Contraction
| Crossbridge animation | Component proteins |
|---|---|
|
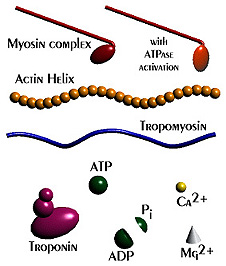
|
| Sarcomere Animation | Muscle Histology |
|
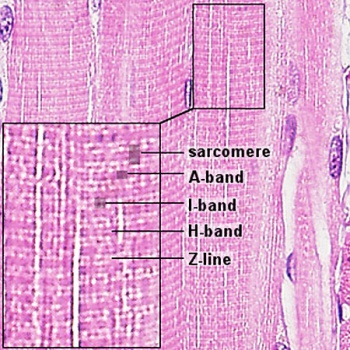
|
Sarcomere - Electron Microscopy
| Virtual Slides | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
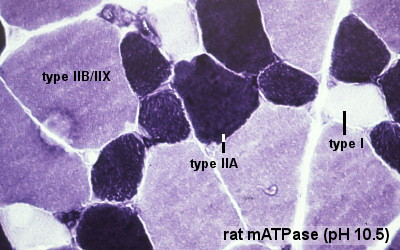
Muscle Fibre Types
Muscle Embryology
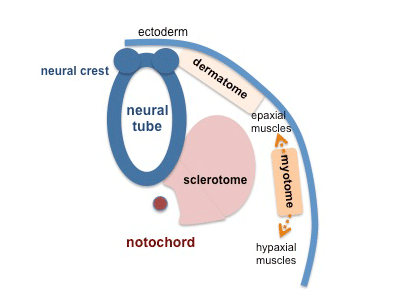
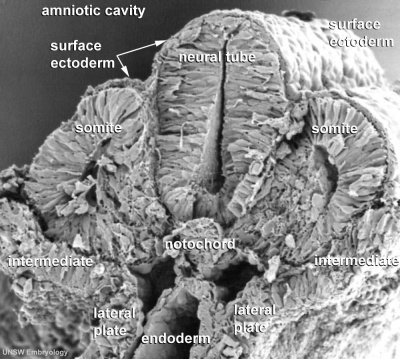
- Determined - when cells are located within the somite myotome.
- Migrate - small cell population moves to location of adult muscle.
- Proliferate - as myoblasts, single nuclei cells.
- Fuse - to form myotubes, the primitive skeletal muscle fibre not yet showing sarcomeres.
- Differentiate - express contractile proteins
Muscle Stem Cells
| Satellite cells | |
|---|---|
|
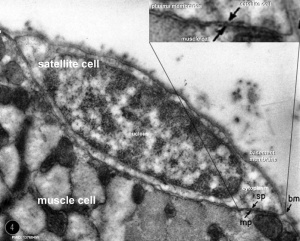
|
| Satellite cell molecular markers |
|---|
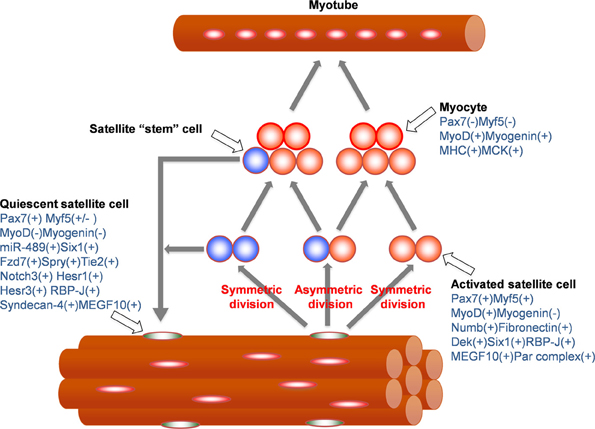
Muscle satellite cell markers[1] (Note - for this class you do not need to know these markers). |
Muscle Innervation
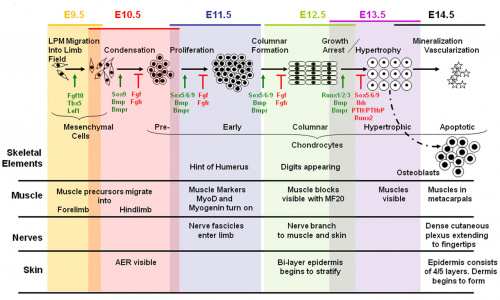
Mouse Limb Tissue Development (muscle, nerve, skeletal)
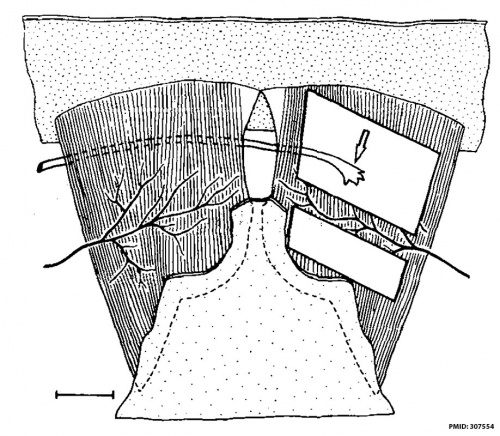
Basal lamina control of innervation site
Muscular Dystrophies
Dystrophy refers to the degeneration of a tissue, muscular dystrophy is degeneration of skeletal muscle.
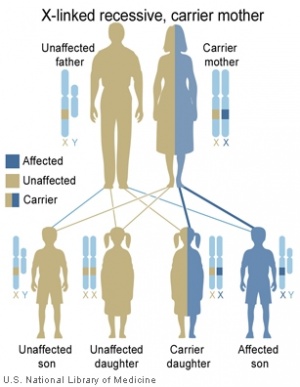
- Duchenne Muscular Dystrophy - (DMD) The most common occuring in boys and in Duchenne Muscular Dystrophy (DMD). PMID 3319190 PMID 2447503
- Becker Muscular Dystrophy - (BMD) Similar to DMD but allows muscles to function better than in DMD, slower progression, make a shortened form of the mutated protein.
- Autosomal Recessive Muscular Dystrophy - Dystroglycan, a protein that associates with both dystrophin and membrane molecules, is a candidate gene for the site of the mutation in autosomal recessive muscular dystrophies. A knockout mouse has been generated that has early developmental abnormalities.
- Myotonic Dystrophy - An inherited disorder in which the muscles contract but have decreasing power to relax. With this condition, the muscles also become weak and waste away. The myotonic dystrophy gene, found on chromosome 19, codes for a protein kinase that is found in skeletal muscle, where it likely plays a regulatory role. The disease is "amplified" through generations probably by a similar GC expansion associated with Huntington disease.
- Facioscapulohumeral Muscular Dystrophy - (FSHD) This form of muscular dystrophy is an autosomal dominant genetic disorder characterized by progressive muscle weakness and wasting that typically begins in the face, shoulder-girdle and upper arm. Currently thought to relate to an impaired muscle regeneration process.
Lab 7 Assessment Questions
TBA
Search
Bookshelf - Muscle Development
Terms
- anterior tibialis - (tibialis anterior) skeletal muscle situated on the lateral side of the tibia and is a direct flexor of the foot at the ankle-joint.
- cardiomyopathy - heart muscle begins to dilate, stretching and becomes thinner, associated with DMD boys and some DMD carrier girls.
- carrier females - (carrier mother, carrier) X-linked recessive inheritance seen with DMD and a range of other inherited disorders where the gene is recessive and located on the X chromosome.
- cis-acting elements - DNA sequences that through transcription factors or other trans-acting elements or factors, regulate the expression of genes on the same chromosome.
- corticosteroids - used as a pharmacologic agents in DMD treatment these are the synthetic glucocorticoids; prednisone and its active metabolite prednisolone and
deflazacort an inactive prodrug.
- dystrophy - Refers to the degeneration of a tissue, a muscular dystrophy is the degeneration of skeletal muscle.
- enhancer - A cis-regulatory sequence that can regulate levels of transcription from an adjacent promoter. Many tissue-specific enhancers can determine spatial patterns of gene expression in higher eukaryotes. Enhancers can act on promoters over many tens of kilobases of DNA and can be 5' or 3' to the promoter they regulate.
- extensor digitorum longus - (EDL) skeletal muscle situated at the lateral part of the front of the leg and extend the phalanges of the toes, and, continuing their action, flex the foot upon the leg.
- Gtf2ird1 - General Transcription Factor 2 -I Repeat domain-containing protein 1. OMIM: Gtf2ird1
- multiplex ligation-dependent probe amplification - (MLPA) a genetic test used to identify disorders including DMD.
- muscle biopsy - a clinical test where a small part of the muscle is removed to analyse structure, fibre type and muscle protein abnormalities.
- MusTRD1 - muscle TFII-I repeat domain-containing protein 1.
- MyHC - acronym for myosin heavy chain.
- myoblast - the undifferentiated mononucleated muscle cell progenitor, which in skeletal muscle fuses to form a myotube, that in turn expresses contractile proteins to form a muscle fibre.
- myosin heavy chain - protein forming the thick filament of the sarcomere and the motor for actin-myosin contraction. There are 17 different myosin classes.
- myosin ATPase - the enzyme activity of myosin head that moves along actin filaments by coupling the hydrolysis of ATP to conformational changes.
- myotube - the initial multinucleated cell formed by fusion of myoblasts during skeletal muscle development.
- promoter - A regulatory region a short distance upstream from the 5' end of a transcription start site that acts as the binding site for RNA polymerase II. A region of DNA to which RNA polymerase IIbinds in order to initiate transcription.
- regulatory sequence - (regulatory region, regulatory area) is a segment of DNA where regulatory proteins such as transcription factors bind preferentially.
- serum creatine kinase - CK is an intracellular enzyme found in tissues with high ATP requirement, like muscle. Serum levels are raised in DMD 10–20 times (or higher 50–200 times) the upper limit of normal level before the age of 5 years.
- soleus - slow skeletal muscle situated immediately in front of the gastrocnemius and when standing taking its fixed point from below, steadies the leg upon the foot and prevents the body from falling forward.
- Troponin - striated muscle contraction is regulated by the calcium-ion-sensitive, multiprotein complex troponin and the fibrous protein tropomyosin. Troponin has 3 subunits (TnC, TnI, TnT) and is located on the actin filament. OMIM: Troponin I slow
External Links
External Links Notice - The dynamic nature of the internet may mean that some of these listed links may no longer function. If the link no longer works search the web with the link text or name. Links to any external commercial sites are provided for information purposes only and should never be considered an endorsement. UNSW Embryology is provided as an educational resource with no clinical information or commercial affiliation.
- Blue Histology Skeletal Muscle histology
- PLOS Currents - Muscular Dystrophy
- OMIM
- Primer Skeletal Muscle Fiber Type: Influence on Contractile and Metabolic Properties
Glossary Links
- Glossary: A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | Numbers | Symbols | Term Link
Cite this page: Hill, M.A. (2024, May 6) Embryology ANAT2341 Lab 7. Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/ANAT2341_Lab_7
- © Dr Mark Hill 2024, UNSW Embryology ISBN: 978 0 7334 2609 4 - UNSW CRICOS Provider Code No. 00098G
References
- ↑ <pubmed>25364710</pubmed>
| ANAT2341 Course Timetable | |||
|---|---|---|---|
| Week (Mon) | Lecture 1 (Mon 1-2pm) | Lecture 2 (Tue 3-4pm) | Practical (Fri 1-3pm) |
| Week 2 (1 Aug) | Introduction | Fertilization | Lab 1 |
| Week 3 (8 Aug) | Week 1 and 2 | Week 3 | Lab 2 |
| Week 4 (15 Aug) | Mesoderm | Ectoderm | Lab 3 |
| Week 5 (22 Aug) | Early Vascular | Placenta | Lab 4 |
| Week 6 (29 Aug) | Gastrointestinal | Respiratory | Lab 5 |
| Week 7 (5 Sep) | Head | Neural Crest | Lab 6 |
| Week 8 (12 Sep) | Musculoskeletal | Limb Development | Lab 7 |
| Week 9 (19 Sep) | Renal | Genital | Lab 8 |
| Mid-semester break | |||
| Week 10 (3 Oct) | Public Holiday | Stem Cells | Lab 9 |
| Week 11 (10 Oct) | Integumentary | Endocrine | Lab 10 |
| Week 12 (17 Oct) | Heart | Sensory | Lab 11 |
| Week 13 (24 Oct) | Fetal | Birth and Revision | Lab 12 |
|
ANAT2341 2016: Moodle page | ECHO360 | Textbooks | Students 2016 | Projects 2016 | |||