2009 Lecture 20: Difference between revisions
| Line 122: | Line 122: | ||
respond to calcium levels | respond to calcium levels | ||
fetal calcium levels higher than maternal | fetal calcium levels higher than maternal | ||
==Thymus== | |||
Third Pharyngeal Pouch | |||
endoderm | |||
Week 6 | |||
diverticulum elongates | |||
hollow then solid | |||
ventral cell proliferation | |||
Thymic primordia | |||
surrounded by neural crest mesenchyme | |||
Thymus development | |||
epithelia/mesenchyme interaction | |||
==Pancreas== | |||
Functions | |||
exocrine (amylase, alpha-fetoprotein) | |||
99% by volume | |||
endocrine (pancreatic islets) | |||
1% by volume | |||
Pancreatic buds | |||
endoderm, covered in splanchnic mesoderm | |||
Pancreatic bud formation | |||
duodenal level endoderm, splanchnic mesoderm forms dorsal and ventral mesentery, dorsal bud (larger, first), ventral bud (smaller, later) | |||
Pancreas Endoderm | |||
pancreas may be opposite of liver | |||
Heart cells promote/notochord prevents liver formation | |||
Notochord may promote pancreas formation | |||
Heart may block pancreas formation | |||
Pancreas | |||
Duodenum growth/rotation | |||
brings ventral and dorsal buds together, fusion of buds | |||
Pancreatic duct | |||
ventral bud duct and distal part of dorsal bud, exocrine function | |||
Islet cells | |||
cords of endodermal cells form ducts | |||
From which cells bud off to form islets | |||
Early Pancreas - Stage 13 | |||
Human Pancreas Development | |||
Pancreatic Islets- Endocrine | |||
Islets of Langerhans | |||
4 cell types | |||
Alpha | |||
Glucagon | |||
mobilizes lipid | |||
Beta | |||
Insulin | |||
increase glucose uptake | |||
Delta | |||
Somatostatin, inhibits glucagon, insulin secretion | |||
F-cells | |||
pancreatic polypeptide | |||
Pancreas Function | |||
Exocrine function | |||
begins after birth | |||
Endocrine function | |||
hormone release | |||
from 10 to 15 weeks onward | |||
exact roles of hormones in regulating fetal growth? | |||
Pancreas Timetable | |||
Week 7 to 20 | |||
pancreatic hormones secretion increases | |||
small amount maternal insulin | |||
Week 10 | |||
glucagon (alpha) differentiate first, somatostatin (delta), insulin (beta) cells differentiate, insulin secretion begins | |||
Week 15 | |||
glucagon detectable in fetal plasma | |||
Beta cells | |||
stimulate fetal growth | |||
continue to proliferate to postnatal | |||
Infancy most abundant | |||
==Adrenal== | |||
Adrenal - Blood Supply | |||
Richly vascularized | |||
arterioles passing through cortex | |||
capillaries from cortex to medulla | |||
portal-like circulation | |||
Fetal Adrenals | |||
Adrenal Cortex Development | |||
Week 6 | |||
fetal cortex | |||
from mesothelium adjacent to dorsal mesentery | |||
Medulla | |||
neural crest cells from adjacent sympathetic ganglia | |||
Adult cortex | |||
mesothelium mesenchyme encloses fetal cortex | |||
Late Fetal Period | |||
differentiates to form cortical zones | |||
Birth | |||
zona glomerulosa, zona fasiculata present | |||
Year 3 | |||
zona reticularis present | |||
Fetal Adrenal Cortex | |||
Fetal Adrenal Cortex | |||
Movie: Neural Crest Migration | |||
Adrenal Medulla | |||
neural crest origin | |||
migrate adjacent to coelomic cavity | |||
neuron-like morphology | |||
2 cell types | |||
secrete epinepherine | |||
adrenaline 80% | |||
secrete norepinepherine | |||
noradrenaline 20% | |||
Hormones | |||
Fetal Cortex produces | |||
a steroid precursor (DEA) | |||
converted by placenta into estrogen | |||
Adult Medulla produces | |||
adrenalin (epinephrine) | |||
noradrenaline (norepinephrine) | |||
Fetal adrenal hormones | |||
influence lung maturation | |||
==Gonads== | |||
* Covered in previous Sexual Differentiation Lecture/Practical | |||
Gonad- mesoderm | |||
mesothelium and underlying mesenchyme | |||
Primordial germ cells | |||
Gonadal ridge | |||
mesothelium thickening, medial mesonephros | |||
Primordial Germ cells | |||
yolk sac, to mesentery of hindgut, to genital ridge of developing kidney | |||
Gonadal Ridge Stage 13 | |||
Gonad Differentiation | |||
testis-determining factor (TDF) from Y chromosome | |||
presence (testes) | |||
absence (ovaries) | |||
Testis | |||
8 Weeks | |||
mesenchyme, interstitial cells (of Leydig) secrete testosterone, androstenedione | |||
8 to 12 Weeks | |||
hCG stimulates testosterone production | |||
Sustentacular cells | |||
produce anti-mullerian hormone to puberty | |||
Ovary | |||
X chromosome genes regulate ovary development | |||
==Placenta== | |||
* Human chorionic gonadotrophin (hCG) - like leutenizing hormone, supports corpus luteum in ovary, pregnant state rather than menstrual | |||
maternal urine in some pregnancy testing | |||
* Human chorionic somatommotropin (hCS) - or placental lactogen stimulate (maternal) mammary development | |||
* Human chorionic thyrotropin (hCT) | |||
* Human chorionic corticotropin (hCACTH) | |||
progesterone and estrogens | |||
support maternal endometrium | |||
Relaxin | |||
Placenta | |||
Maternal (decidua) and Fetal (trophoblastic cells, extraembryonic mesoderm) components | |||
Endocrine function | |||
maternal and fetal precursors, synthesis and secretion | |||
Protein Hormones | |||
chorionic gonadotropin (hCG), chorionic somatomammotropin (hCS) or placental lactogen (hPL), chorionic thyrotropin (hCT), chorionic corticotropin (hCACTH) | |||
Steroid Hormones | |||
progesterone (maintains pregnancy) | |||
estrogens (fetal adrenal/placenta) | |||
hCG - up to 20 weeks, fetal adrenal cortex growth and maintenance | |||
hCS – rise through pregnancy, stimulates maternal metabolic processes, breast growth | |||
==Links== | ==Links== | ||
Revision as of 15:08, 3 October 2009
Introduction
The endocrine system resides within specific endocrine organs and both organs and tissues with other specific functions. Epithelia (ectoderm and endoderm) form the majority of the “ductless” endocrine glands like gastrointestinal and skin associated “ducted” glands. Differentiation of several also organs involves a epithelial/mesenchye interaction, seen in repeated in many differentiation of many different tissues. The endocrine glands produce hormones, which are distributed by the vascular system to the many body tissues, subsequently these organs are richly vascularized.
Hormones “orchestrate” responses in other tissues, including other endocrine organs, and these overall effects can be similar or different in different tissues. In addition, these hormone effects (like music) can be rapid, slow, brief, diurnal, or long-term. Hormone effects can be mimicked, stimulated, and blocked by therapeutic drugs, nutritional and environmental chemicals.
2008: Lecture - Endocrine Development | lecture 1 slide/page PDF | lecture 4 slides/page PDF |
2009: Medicine Lecture - Endocrine Development | lecture 1 slide/page PDF
Lecture Objectives
- Understanding of hormone types
- Understanding of endocrine gland development
- Understanding of endocrine developmental functions
- Brief understanding of endocrine abnormalities
Textbooks
In general, not dealt with as a system in many textbooks, so various chapters: nervous system, head, gastrointestinal tract, reproductive organs, etc.
- Human Embryology (3rd ed.) Larson
- The Developing Human: Clinically Oriented Embryology (6th ed.) Moore and Persaud Chapters 10: p230-233; Ch12: p280-282; Ch13: p319-347
Hormones
Hormone Types
- Amino acid derivatives - noradrenaline (norepinepherine), adrenalin (epinepherine) , thyroid hormone
- Proteins, peptides - thyroid stimulating hormone, leutenising hormone, follicle stimulating hormone
- Steroids - androgens, glucocorticoids, mineralocorticoids
Hormone Actions
- Autocrine - acts on self (extracellular fluid)
- Paracrine - acts locally (extracellular fluid)
- Endocrine - acts by secretion into blood stream (endocrine organs are richly vascularized)
Hormone Receptors
Hormones are recognised by either cell surface receptors (modified amino acids, peptides, proteins) or cytoplasmic/nuclear receptors (steroids).
Endocrine Origins
- Derived from epithelia - covering embryo, lining gastrointestinal tract, lining coelomic cavity
- Also mesenchymal contribution
Pineal Gland
- part of epithalmus - neurons, glia and pinealocytes
- pinealocytes secrete melatonin - cyclic nature of activity, melatonin lowest during daylight
- other activities - possibly gamete maturation, antioxidant effect, protect neurons?
Pineal Development
- Neuroectoderm - prosenecephalon then diencephalon
- caudal roof, median diverticulum, epiphysis
- Initially a hollow diverticulum, cell proliferation to solid, pinealocytes (neuroglia), cone-shaped gland innervated by epithalmus
Hypothalmus
Hypothalmus Development
- Neuroectoderm - prosenecephalon then diencephalon
- ventro-lateral wall intermediate zone proliferation
- Mamillary bodies - form pea-sized swellings ventral wall of hypothalamus
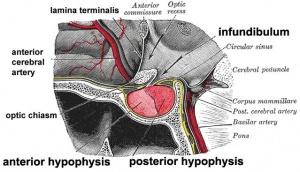
Pituitary
Pituitary Development
- Dual ectoderm origins
- Ectoderm - ectoderm roof of stomodeum, Rathke's pouch, adenohypophysis
- Neuroectoderm - prosenecephalon then diencephalon, neurohypophysis
Adenohypophysis
- Anterior wall proliferates - pars distalis
- Posterior wall little growth – pars intermedia
- Rostral growth around infundibular stem – pars tuberalis
Neurohypophysis
- Infundibulum – median eminence, infundibulum, pars nervosa
Pituitary Timeline
- Week 4 - hypophysial pouch, Rathke’s pouch, diverticulum from roof
- Week 5 - elongation, contacts infundibulum, diverticulum of diencephalon
- Week 6 - connecting stalk between pouch and oral cavity degenerates
- Week 10 - growth hormone and ACTH detectable
- Week 16 - adenohypophysis fully differentiated
- Week 20 to 24 - growth hormone levels peak, then decline
Fetal Thyroiud Hormone
- Initial secreted biologically inactivated by modification, late fetal secretion develops brown fat
- Iodine deficiency- during this period, leads to neurological defects (cretinism)
- Birth - TSH levels increase, thyroxine (T3) and T4 levels increase to 24 h, then 5-7 days postnatal decline to normal levels
Thyroid
- Functions from wk10, required for neural development, stimulates metabolism (protein, carbohydrate, lipid), reduced/absence = cretinism (see abnormalities)
Thyroid Development
- thyroid median endodermal thickening in the floor of pharynx, outpouch – thyroid diverticulum
- tongue grows, cells descend in neck
- thyroglossal duct - proximal end at the foramen cecum of tongue
- thyroid diverticulum - hollow then solid, right and left lobes, central isthmus
Thyroid Timeline
- 24 days - thyroid median endodermal thickening in the floor of pharynx, outpouch – thyroid diverticulum
- Week 11 - colloid appearance in thyroid follicles, iodine and thyroid hormone (TH) synthesis
growth factors (insulin-like, epidermal) stimulates follicular growth
Parathyroid
Parathyroid Hormone Increase calcium ions [Ca2+] stimulates osteoclasts increase Ca GIT absorption opposite effect to calcitonin secreted by chief cells Principal cells cords of cells Parathyroid Third and Fourth Pharyngeal Pouches Endoderm could also have ectoderm and neural crest 3rd Pharyngeal Pouch inferior parathyroid initially descends with thymus 4th Pharyngeal Pouch superior parathyroid Week 6 diverticulum elongate, hollow then solid, dorsal cell proliferation Fetal parathyroids respond to calcium levels fetal calcium levels higher than maternal
Thymus
Third Pharyngeal Pouch endoderm Week 6 diverticulum elongates hollow then solid ventral cell proliferation Thymic primordia surrounded by neural crest mesenchyme Thymus development epithelia/mesenchyme interaction
Pancreas
Functions exocrine (amylase, alpha-fetoprotein) 99% by volume endocrine (pancreatic islets) 1% by volume Pancreatic buds endoderm, covered in splanchnic mesoderm Pancreatic bud formation duodenal level endoderm, splanchnic mesoderm forms dorsal and ventral mesentery, dorsal bud (larger, first), ventral bud (smaller, later) Pancreas Endoderm pancreas may be opposite of liver Heart cells promote/notochord prevents liver formation Notochord may promote pancreas formation Heart may block pancreas formation Pancreas Duodenum growth/rotation brings ventral and dorsal buds together, fusion of buds Pancreatic duct ventral bud duct and distal part of dorsal bud, exocrine function Islet cells cords of endodermal cells form ducts From which cells bud off to form islets Early Pancreas - Stage 13 Human Pancreas Development Pancreatic Islets- Endocrine Islets of Langerhans 4 cell types Alpha Glucagon mobilizes lipid Beta Insulin increase glucose uptake Delta Somatostatin, inhibits glucagon, insulin secretion F-cells pancreatic polypeptide Pancreas Function Exocrine function begins after birth Endocrine function hormone release from 10 to 15 weeks onward exact roles of hormones in regulating fetal growth? Pancreas Timetable Week 7 to 20 pancreatic hormones secretion increases small amount maternal insulin Week 10 glucagon (alpha) differentiate first, somatostatin (delta), insulin (beta) cells differentiate, insulin secretion begins Week 15 glucagon detectable in fetal plasma Beta cells stimulate fetal growth continue to proliferate to postnatal Infancy most abundant
Adrenal
Adrenal - Blood Supply Richly vascularized arterioles passing through cortex capillaries from cortex to medulla portal-like circulation Fetal Adrenals Adrenal Cortex Development Week 6 fetal cortex from mesothelium adjacent to dorsal mesentery Medulla neural crest cells from adjacent sympathetic ganglia Adult cortex mesothelium mesenchyme encloses fetal cortex Late Fetal Period differentiates to form cortical zones Birth zona glomerulosa, zona fasiculata present Year 3 zona reticularis present Fetal Adrenal Cortex Fetal Adrenal Cortex Movie: Neural Crest Migration Adrenal Medulla neural crest origin migrate adjacent to coelomic cavity neuron-like morphology 2 cell types secrete epinepherine adrenaline 80% secrete norepinepherine noradrenaline 20% Hormones Fetal Cortex produces a steroid precursor (DEA) converted by placenta into estrogen Adult Medulla produces adrenalin (epinephrine) noradrenaline (norepinephrine) Fetal adrenal hormones influence lung maturation
Gonads
- Covered in previous Sexual Differentiation Lecture/Practical
Gonad- mesoderm mesothelium and underlying mesenchyme Primordial germ cells Gonadal ridge mesothelium thickening, medial mesonephros Primordial Germ cells yolk sac, to mesentery of hindgut, to genital ridge of developing kidney Gonadal Ridge Stage 13 Gonad Differentiation testis-determining factor (TDF) from Y chromosome presence (testes) absence (ovaries) Testis 8 Weeks mesenchyme, interstitial cells (of Leydig) secrete testosterone, androstenedione 8 to 12 Weeks hCG stimulates testosterone production Sustentacular cells produce anti-mullerian hormone to puberty Ovary X chromosome genes regulate ovary development
Placenta
- Human chorionic gonadotrophin (hCG) - like leutenizing hormone, supports corpus luteum in ovary, pregnant state rather than menstrual
maternal urine in some pregnancy testing
- Human chorionic somatommotropin (hCS) - or placental lactogen stimulate (maternal) mammary development
- Human chorionic thyrotropin (hCT)
- Human chorionic corticotropin (hCACTH)
progesterone and estrogens support maternal endometrium Relaxin Placenta Maternal (decidua) and Fetal (trophoblastic cells, extraembryonic mesoderm) components Endocrine function maternal and fetal precursors, synthesis and secretion Protein Hormones chorionic gonadotropin (hCG), chorionic somatomammotropin (hCS) or placental lactogen (hPL), chorionic thyrotropin (hCT), chorionic corticotropin (hCACTH) Steroid Hormones progesterone (maintains pregnancy) estrogens (fetal adrenal/placenta) hCG - up to 20 weeks, fetal adrenal cortex growth and maintenance hCS – rise through pregnancy, stimulates maternal metabolic processes, breast growth
Links
- UNSW Embryology: Stage 13/14 Embryo | Stage 22 Embryo | Selected Sections Stage 22 Embryo | Abnormal Endocrine Development | Pituitary Development | Thyroid Development | Adrenal Development | Pancreas Development See also GIT Notes- Pancreas | Endocrine Placenta | Hypothalmus | Parathyroid | Endocrine Adipose Tissue | Other Endocrine Tissues
- Embryo Images: Pituitary Development
Glossary Links
- Glossary: A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | Numbers | Symbols | Term Link
Course Content 2009
Embryology Introduction | Cell Division/Fertilization | Cell Division/Fertilization | Week 1&2 Development | Week 3 Development | Lab 2 | Mesoderm Development | Ectoderm, Early Neural, Neural Crest | Lab 3 | Early Vascular Development | Placenta | Lab 4 | Endoderm, Early Gastrointestinal | Respiratory Development | Lab 5 | Head Development | Neural Crest Development | Lab 6 | Musculoskeletal Development | Limb Development | Lab 7 | Kidney | Genital | Lab 8 | Sensory - Ear | Integumentary | Lab 9 | Sensory - Eye | Endocrine | Lab 10 | Late Vascular Development | Fetal | Lab 11 | Birth, Postnatal | Revision | Lab 12 | Lecture Audio | Course Timetable
Cite this page: Hill, M.A. (2024, May 2) Embryology 2009 Lecture 20. Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/2009_Lecture_20
- © Dr Mark Hill 2024, UNSW Embryology ISBN: 978 0 7334 2609 4 - UNSW CRICOS Provider Code No. 00098G