2009 Lecture 20
Introduction
The endocrine system resides within specific endocrine organs and both organs and tissues with other specific functions. Epithelia (ectoderm and endoderm) form the majority of the “ductless” endocrine glands like gastrointestinal and skin associated “ducted” glands. Differentiation of several also organs involves a epithelial/mesenchye interaction, seen in repeated in many differentiation of many different tissues. The endocrine glands produce hormones, which are distributed by the vascular system to the many body tissues, subsequently these organs are richly vascularized.
Hormones “orchestrate” responses in other tissues, including other endocrine organs, and these overall effects can be similar or different in different tissues. These signaling pathways are often described as "axes" the two major types are the: HPA (Hyothalamus-Pituitary-Adrenal) and HPG (Hypothalamus-Pituitary-Gonad). These hormone effects (like music) can be rapid, slow, brief, diurnal, or long-term. Hormone effects can be mimicked, stimulated, and blocked by therapeutic drugs, nutritional and environmental chemicals. Importantly, fetal endocrine development is required for normal fetal growth and differentiation.
- Lecture Audio Lecture Date: 06-10-2009 Lecture Time: 12:00 Venue: BioMed E Speaker: Mark Hill Endocrine
2013: Current lecture
2009: Medicine Lecture - Endocrine Development | lecture 1 slide/page PDF
2008: Lecture - Endocrine Development | lecture 1 slide/page PDF | lecture 4 slides/page PDF |
Lecture Objectives
- Understanding of hormone types
- Understanding of endocrine gland development
- Understanding of endocrine developmental functions
- Brief understanding of endocrine abnormalities
Textbooks
In general, not dealt with as a system in many textbooks, so various chapters: nervous system, head, gastrointestinal tract, reproductive organs, etc.
- Human Embryology (3rd ed.) Larson Chapter 9 Gastrointestinal, Chapter 10 Gonad, Kidney Chapter 12 Head
- The Developing Human: Clinically Oriented Embryology (6th ed.) Moore and Persaud Chapters 10: p230-233; Ch12: p280-282; Ch13: p319-347
Hormones
Hormone Types
- Amino acid derivatives - noradrenaline (norepinepherine), adrenalin (epinepherine) , thyroid hormone
- Proteins, peptides - thyroid stimulating hormone, leutenising hormone, follicle stimulating hormone
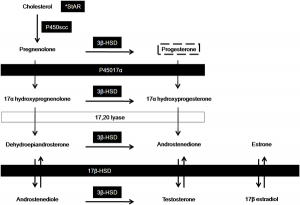
- Steroids - androgens, glucocorticoids, mineralocorticoids
Hormone Actions
- Autocrine - acts on self (extracellular fluid)
- Paracrine - acts locally (extracellular fluid)
- Endocrine - acts by secretion into blood stream (endocrine organs are richly vascularized)
Hormone Receptors
Hormones are recognised by either cell surface receptors (modified amino acids, peptides, proteins) or cytoplasmic/nuclear receptors (steroids).
MH - Interested in hormone history? Listen ABC Radio Ockham's Razor 2005-07-31 6.2 Mb mp3 Centenary of the word 'hormone', Sydney medical scientist and writer Dr John Carmody commemorates the centenary of the entry of the word 'hormone' into the English language.
Endocrine Origins
- Derived from epithelia - covering embryo, lining gastrointestinal tract, lining coelomic cavity
- Also mesenchymal contribution
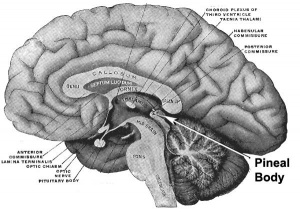
Pineal Gland
UNSW Embryology - Pineal Development
- part of epithalmus - neurons, glia and pinealocytes
- pinealocytes secrete melatonin - cyclic nature of activity, melatonin lowest during daylight
- inhibit hypothalamic secretion of GnRH until puberty, pineal gland then rapidly regresses.
- other activities - possibly gamete maturation, antioxidant effect, protect neurons?
Pineal Development
- Neuroectoderm - prosenecephalon then diencephalon
- caudal roof, median diverticulum, epiphysis
- Initially a hollow diverticulum, cell proliferation to solid, pinealocytes (neuroglia), cone-shaped gland innervated by epithalmus
Hypothalamus
Lecture - Head Development | Lecture - Early Neural Development | Lecture - Late Neural Development | UNSW Embryology - Hypothalmus Development
Hormones - Thyrotrophin releasing hormone (TRH), Corticotrophin releasing hormone (CRH), Arginine vasopressin (AVP), Gonadotrophin releasing hormone (GnRH), Growth hormone releasing hormone (GHRH), Somatostatin, Prolactin relasing factor (PRF), Dopamine
Hypothalamus Development
- Neuroectoderm - prosenecephalon then diencephalon
- ventro-lateral wall intermediate zone proliferation
- Mamillary bodies - form pea-sized swellings ventral wall of hypothalamus
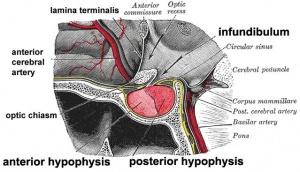
Pituitary
Lecture - Head Development | UNSW Embryology - Pituitary Development
Anterior pituitary hormones - Thyroid-stimulating hormone (TSH), Adrenocorticotrophic hormone (ACTH), Luteinizing hormone (LH), Follicle-stimulating hormone (FSH), Somatotrophin/growth hormone (GH), Prolactin (PRL), Melanocyte-stimulating hormone (MSH)
Posterior pituitary hormones - Oxytocin, Arginine vasopressin
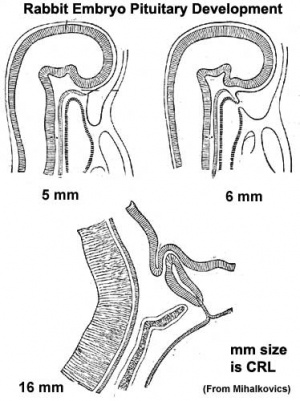
Pituitary Development
- Dual ectoderm origins
- Ectoderm - ectoderm roof of stomodeum, Rathke's pouch, adenohypophysis
- Neuroectoderm - prosenecephalon then diencephalon, neurohypophysis
Adenohypophysis
- Anterior wall proliferates - pars distalis
- Posterior wall little growth – pars intermedia
- Rostral growth around infundibular stem – pars tuberalis
Neurohypophysis
- Infundibulum – median eminence, infundibulum, pars nervosa
Pituitary Timeline
- Week 4 - hypophysial pouch, Rathke’s pouch, diverticulum from roof
- Week 5 - elongation, contacts infundibulum, diverticulum of diencephalon
- Week 6 - connecting stalk between pouch and oral cavity degenerates
- Week 10 - growth hormone and ACTH detectable
- Week 16 - adenohypophysis fully differentiated
- Week 20 to 24 - growth hormone levels peak, then decline
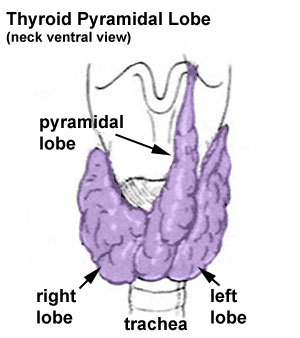
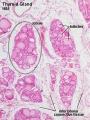
Thyroid
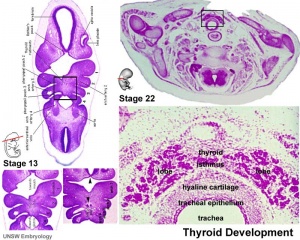
Lecture - Head Development | UNSW Embryology - Thyroid Development
- Functions from wk10, required for neural development, stimulates metabolism (protein, carbohydrate, lipid), reduced/absence = cretinism (see abnormalities)
Hormones - (amino acid derivatives) Thyroxine (T4), Triiodothyronine (T3)
Thyroid Development
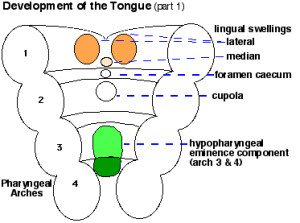
- thyroid median endodermal thickening in the floor of pharynx, outpouch – thyroid diverticulum
- tongue grows, cells descend in neck
- thyroglossal duct - proximal end at the foramen cecum of tongue thyroglossal duct
- thyroid diverticulum - hollow then solid, right and left lobes, central isthmus
Thyroid Timeline
- 24 days - thyroid median endodermal thickening in the floor of pharynx, outpouch – thyroid diverticulum
- Week 11 - colloid appearance in thyroid follicles, iodine and thyroid hormone (TH) synthesis
growth factors (insulin-like, epidermal) stimulates follicular growth
Fetal Thyroid Hormone
- Initial secreted biologically inactivated by modification, late fetal secretion develops brown fat
- Iodine deficiency- during this period, leads to neurological defects (cretinism)
- Birth - TSH levels increase, thyroxine (T3) and T4 levels increase to 24 h, then 5-7 days postnatal decline to normal levels
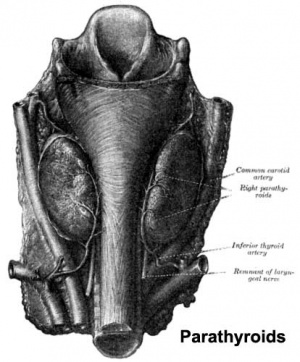
Parathyroid
Lecture - Head Development | UNSW Embryology - Parathyroid
- Parathyroid Hormone - Increase calcium ions [Ca2+], stimulates osteoclasts, increase Ca GIT absorption (opposite effect to calcitonin)
- Adult Calcium and Phosphate - Daily turnover in human with dietary intake of 1000 mg/day
- secreted by chief cells
Principal cells cords of cells
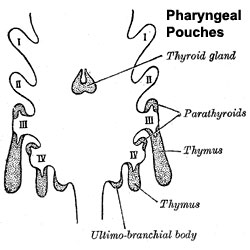
Parathyroid Development
- Endoderm - third and fourth pharyngeal pouches, could also have ectoderm and neural crest
- 3rd Pharyngeal Pouch - inferior parathyroid, initially descends with thymus
- 4th Pharyngeal Pouch - superior parathyroid
- Week 6 - diverticulum elongate, hollow then solid, dorsal cell proliferation
- Fetal parathyroids - respond to calcium levels, fetal calcium levels higher than maternal
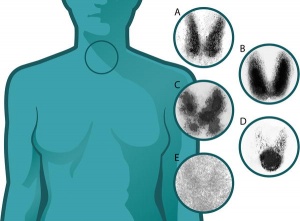
Thymus
Lecture - Head Development | UNSW Embryology - Thymus Development
- Thymus - bone-marrow lymphocyte precursors become thymocytes, and subsequently mature into T lymphocytes (T cells)
- Thymus hormones - thymosins stimulate the development and differentiation of T lymphocytes
Thymus Development
- Endoderm - third pharyngeal pouch
- Week 6 - diverticulum elongates, hollow then solid, ventral cell proliferation
- Thymic primordia - surrounded by neural crest mesenchyme, epithelia/mesenchyme interaction
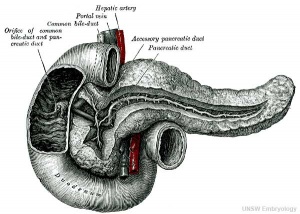
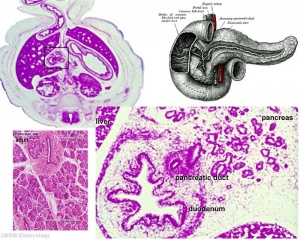
Pancreas
Lecture- Gastrointestinal Tract Development | UNSW Embryology - Pancreas Development see also GIT Notes- Pancreas
- Functions - exocrine (amylase, alpha-fetoprotein), 99% by volume; endocrine (pancreatic islets) 1% by volume
- Exocrine function - begins after birth
- Endocrine function - from 10 to 15 weeks onward hormone release
- exact roles of hormones in regulating fetal growth?
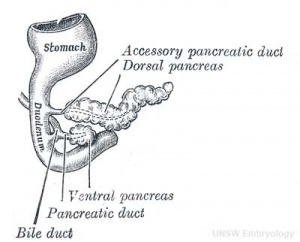
Pancreas Development
- Pancreatic buds - duodenal level endoderm, splanchnic mesoderm forms dorsal and ventral mesentery, dorsal bud (larger, first), ventral bud (smaller, later)
- Pancreas Endoderm - pancreas may be opposite of liver
- Heart cells promote/notochord prevents liver formation
- Notochord may promote pancreas formation
- Heart may block pancreas formation
- Duodenum growth/rotation - brings ventral and dorsal buds together, fusion of buds
- Pancreatic duct - ventral bud duct and distal part of dorsal bud, exocrine function
- Islet cells - cords of endodermal cells form ducts, from which cells bud off to form islets
Pancreatic Islets
- Islets of Langerhans - 4 endocrine cell types
- Alpha - glucagon, mobilizes lipid
- Beta - insulin, increase glucose uptake
- Beta cells, stimulate fetal growth, continue to proliferate to postnatal, in infancy most abundant
- Delta - somatostatin, inhibits glucagon, insulin secretion
- F-cells - pancreatic polypeptide
Pancreas Timeline
- Week 7 to 20 - pancreatic hormones secretion increases, small amount maternal insulin
- Week 10 - glucagon (alpha) differentiate first, somatostatin (delta), insulin (beta) cells differentiate, insulin secretion begins
- Week 15 - glucagon detectable in fetal plasma
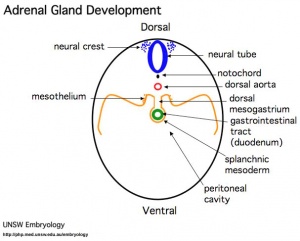
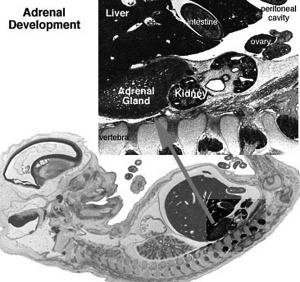
Adrenal
Lecture - Neural Crest Development | UNSW Embryology - Adrenal Development
- Richly vascularized - arterioles passing through cortex, capillaries from cortex to medulla, portal-like circulation
- Fetal Cortex - produces a steroid precursor (DEA), converted by placenta into estrogen
- Adult Medulla - produces adrenalin (epinephrine), noradrenaline (norepinephrine)
- Fetal adrenal hormones - influence lung maturation
Adrenal cortical hormones - (steroids) Cortisol, Aldosterone, Dehydroepiandrosterone
- zona glomerulosa - regulated by renin-angiotensin-aldosterone system controlled by the juxtaglomerular apparatus of the kidney.
- zona fasciculata - regulated by hypothalamo-pituitary axis with the release of CRH and ACTH respectively.
Adrenal medullary hormones - (amino acid derivatives) Epinephrine, Norepinephrine
Adrenal Development
- Fetal Adrenals - fetal cortex later replaced by adult cortex
- Week 6 - fetal cortex, from mesothelium adjacent to dorsal mesentery; Medulla, neural crest cells from adjacent sympathetic ganglia
- Adult cortex - mesothelium mesenchyme encloses fetal cortex
Adrenal Cortex
- Late Fetal Period - differentiates to form cortical zones
- Birth - zona glomerulosa, zona fasiculata present
- Year 3 - zona reticularis present
Endocrinology - Adrenal Cortex Development
Adrenal Medulla
- neural crest origin, migrate adjacent to coelomic cavity, initially uncapsulated and not surrounded by fetal cortex, cells have neuron-like morphology
- 2 cell types - secrete epinepherine (adrenaline) 80%; secrete norepinepherine (noradrenaline* 20%
Gonad
Lecture - Genital Development | UNSW Embryology - Gonads see also previous Sexual Differentiation Lecture/Practical
HPG Axis - Endocrinology - Simplified diagram of the actions of gonadotrophins
Gonad Development
- mesoderm - mesothelium and underlying mesenchyme, primordial germ cells
- Gonadal ridge - mesothelium thickening, medial mesonephros
- Primordial Germ cells - yolk sac, to mesentery of hindgut, to genital ridge of developing kidney
Differentiation
- testis-determining factor (TDF) from Y chromosome: presence (testes), absence (ovaries)
Testis
- 8 Weeks, mesenchyme, interstitial cells (of Leydig) secrete testosterone, androstenedione
- 8 to 12 Weeks - hCG stimulates testosterone production
- Sustentacular cells - produce anti-mullerian hormone to puberty
Ovary
- X chromosome genes regulate ovary development
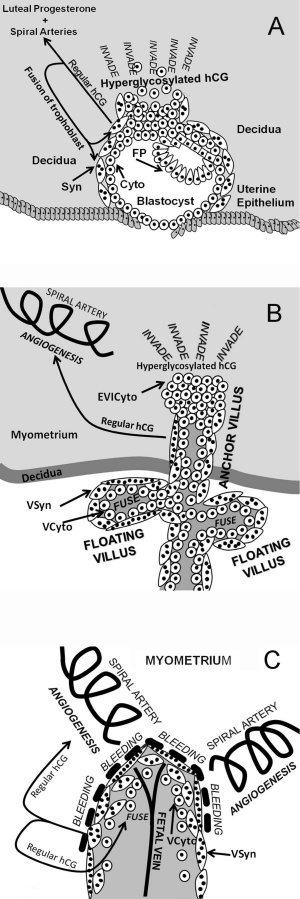
Placenta
Lecture - Placenta Development | UNSW Embryology - Endocrine Placenta
- Human chorionic gonadotrophin (hCG) - like leutenizing hormone, supports corpus luteum in ovary, pregnant state rather than menstrual, maternal urine in some pregnancy testing
- Human chorionic somatommotropin (hCS) - or placental lactogen stimulate (maternal) mammary development
- Human chorionic thyrotropin (hCT)
- Human chorionic corticotropin (hCACTH)
- progesterone and estrogens - support maternal endometrium
- Relaxin
- Placenta - Maternal (decidua) and Fetal (trophoblastic cells, extraembryonic mesoderm) components
- Endocrine function - maternal and fetal precursors, synthesis and secretion
- Protein Hormones - chorionic gonadotropin (hCG), chorionic somatomammotropin (hCS) or placental lactogen (hPL), chorionic thyrotropin (hCT), chorionic corticotropin (hCACTH)
- hCG - up to 20 weeks, fetal adrenal cortex growth and maintenance
- hCS – rise through pregnancy, stimulates maternal metabolic processes, breast growth
- Steroid Hormones - progesterone (maintains pregnancy), estrogens (fetal adrenal/placenta)
- Protein Hormones - chorionic gonadotropin (hCG), chorionic somatomammotropin (hCS) or placental lactogen (hPL), chorionic thyrotropin (hCT), chorionic corticotropin (hCACTH)
Other Endocrine
UNSW Embryology - Other Endocrine Tissues
Endocrine Heart
- Atrial natriuretic peptide (ANP) - Increase Filtration rate / decrease Na+ reabsorption
- Endothelins - ET-1, ET-2, ET-3, Vasoconstriction / Increase NO
- Nitric oxide (NO) - Vasodilatation
Endocrine Kidney
- Renin - Increase Angiotensin-aldosterone system
- Prostaglandins - decrease Na+ reabsorption
- Erythropoietin - Increase Erythrocyte (rbc) production
- 1,25 (OH)2 vitamin D - calcium homeostasis
- Prekallikreins - Increase Kinin production
GIT Endocrine
Enteric control of digestive function
- Gastrin - Secreted from stomach (G cells), role in control of gastric acid secretion
- Cholecystokinin - small intestine hormone, stimulates secretion of pancreatic enzymes and bile
- Secretin - small intestine hormone (epithelial cells), stimulates secretion of bicarbonate-rich fluids from pancreas and liver
Adipose Tissue
UNSW Embryology - Endocrine Adipose Tissue
- Leptin - polypeptide hormone produced in adipose and many other tissues with also many different roles
- Adiponectin - regulation of energy homeostasis and glucose and lipid metabolism, as well as acting as an anti-inflammatory on the cellular vascular wall
- Resistin - (for resistance to insulin, RETN) a 108 amino acid polypeptide and the related resistin-like protein-beta (Resistin-like molecule-beta, RELMbeta) stimulate endogenous glucose production
Endocrine Functional Changes
- Puberty- Increased activity
- Menopause- Decreased activity
- Disease (diabetes, thyroid, kidney) suggested trends that genetics, health, nutrition, lifestyle may influence time that these events occur
- Pharmaceutical impact - birth control, steroids, Hormone Replacement Therapy (HRT)
Abnormalities
NIH Genes & Disease Chapter 41 - Glands and Hormones
Pineal
- hypoplasia - associated with retinal disease.
- tumours - in children are associated with abnormal puberty development.
Pituitary
- craniopharyngeal canal - Rathke's pouch abnormality, from the anterior part of the fossa hypophyseos of the sphenoid bone to the under surface of the skull.
- pituitary tumours (adenomas) - several abnormalities associated with abnormal levels of the hormonal output of the pituitary.
- Growth hormone (GH) adenomas - benign pituitary tumors lead to chronic high GH output levels, that may lead to acromegaly.
- Cushing's disease - caused either by a pituitary adenoma produces excess adrenocorticotropic hormone (ACTH, corticotropin) or due to ectopic tumors secreting ACTH or corticotropin-releasing hormone (CRH).
Thyroid
- Pyramidal lobe - from isthmus (50% of people) attached to hyoid bone distal end of thryoglossal duct.
- Congenital hypothyroidism - approximately 1 in 3000 births, associated with neurological abnormalities.
- Lingual thyroid gland - failure of thyroid descent.
- Thyroglossal cyst - persistance of thyroglossal duct. Image - thyroglossal duct
- Thyroglossal fistula - partial degeneration of the thyroglossal duct.
- Abnormal development of the thyroid - incomplete or excessive descent.
- Childhood hypothyroidism delays ossification and bone mineralization.
Iodine Deficiency
- A teaspoon of iodine, total lifetime requirement, cannot be stored for long periods by our body, tiny amounts are needed regularly
- Areas of endemic iodine deficiency, where soil and therefore crops and grazing animals do not provide sufficient dietary iodine to the populace
- food fortification and supplementation - Iodized salt programs and iodized oil supplements are the most common tools in fight against IDD
Parathyroid
- Usually four glands are present (2 on each side), but three to six glands have been found in human.
- Lower parathyroid glands arise from the third pharyngeal pouch and descend with the thymus. Variable descent can lead to a range of adult locations, from just beneath the mandible to the anterior mediastinum.
Pancreas
- Type 1 Diabetes - juvenile onset diabetes, more severe form of illness, increases risk of blindness, heart disease, kidney failure, neurological disease, T-lymphocyte-dependent autoimmune disease, infiltration and destruction of the islets of Langerhans, Approx 16 million Americans
- Type 2 Diabetes - loosely defined as "adult onset" diabetes, becoming more common cases of type 2 diabetes seen in younger people
- Risk of developing diabetes - environmental factors (food intake and exercise play an important role, either overweight or obese), Inherited factors (genes involved remain poorly defined)
Adrenal
- Congenital Adrenal Hyperplasia (CAH) - family of inherited disorders of adrenal steroidogenesis enzymes which impairs cortisol production by the adrenal cortex. Androgen excess leads newborn females with external genital ambiguity and postnatal progressive virilization in both sexes.
- Enzymes most commonly affected: 21-hydroxylase (21-OH), 11beta-hydroxylase, 3beta-hydroxysteroid dehydrogenase.
- Enzymes less commonly affected: 17alpha-hydroxylase/17,20-lyase and cholesterol desmolase.
- Pheochromocytomas (PCC) - Catecholamine-producing (neuro)endocrine tumor located in the adrenal medulla. Similar catecholamine-producing tumors outside the adrenal gland are called paragangliomas (PGL).
Endocrine Disruptors
Exogenous chemicals that interfere with the function of hormones. There are 3 main mechanisms: mimic, block or interfere.
Mimic - effects of natural hormones by binding receptors
- Diethylstilbestrol - (DES or diethylstilbetrol) a drug prescribed to women from 1938-1971 to prevent miscarriage in high-risk pregnancies. Acts as a potent estrogen (mimics natural hormone) and therefore a potential endocrine disruptor. Female fetus, increased risk abnormal reproductive tract and cancer. Male fetus, abnormal genitalia. Banned by USA FDA in 1979 as a teratogen, previously used as livestock growth promoter.
Block - binding of a hormone to receptor or hormone synthesis
- Finasteride - chemical used to prevent male pattern baldness and enlargement of prostate glands. An anti-androgen (blocks synthesis of dihydrotestosterone) and therefore a potential endocrine disruptor, exposed pregnant women can impact on male fetus genetial development.
- Vinclozolin - a dicarboximide fungicide, perinatal exposure in rats inhibits morphological sex differentiation. In adult rats, shown to cause gonad tumours (Leydig cell) and atrophy. Chemical has androgen-antagonist (antiandrogenic) activity, metabolies compete with natural androgen
Interfere - with hormone transport or elimination
- Polychlorinated biphenyl pollutants - (PCBs) Rats exposed to PCBs have low levels of thyroid hormone. Compete for binding sites of thyroid hormone transport protein. Without being bound to this protein, thyroid hormones are excreted from the body (McKinney et al. 1985; Morse et al. 1996)
Links
- UNSW Embryology: Stage 13/14 Embryo | Stage 22 Embryo | Selected Sections Stage 22 Embryo | Abnormal Endocrine Development | Pituitary Development | Thyroid Development | Adrenal Development | Pancreas Development See also GIT Notes- Pancreas | Endocrine Placenta | Hypothalmus | Parathyroid | Endocrine Adipose Tissue | Other Endocrine Tissues
- Embryo Images: Pituitary Development
References
- Endocrinology: An Integrated Approach Nussey, S.S. and Whitehead, S.A. London:Taylor & Francis; c2001 Major hormone types
- Genes and Disease, Bethesda (MD): National Library of Medicine (US), NCBI Chapter 41 - Glands and Hormones
Search
- Bookshelf endocrine | pineal gland | hypothalamus | pituitary gland | thyroid gland | parathyroid gland | thymus gland | endocrine pancreas | adrenal gland
- Pubmed endocrine development
Histology
Adult
Embryonic
Terms
adrenocorticotropin - (ACTH or corticotropin) anterior pituitary, peptide hormone
antidiuretic hormone - (ADH) hypothalamus, peptide hormone
atrial natriuretic factor - (ANP) heart, , peptide hormone
calcitonin - (CT) C cells of thyroid, peptide hormone
follicle stimulating hormone - (FSH) pituitary, protein hormone
growth hormone - (GH) pituitary, peptide hormone
human chorionic gonadotropin - (hCG) pancreas glycoprotein hormone with 2 subunits (alpha and beta joined non covalently). Similar in structure to luteinizing hormone (LH), hCG exists in multiple hormonal and non-endocrine agents (regular hCG, hyperglycosylated hCG and the free beta-subunit of hyperglycosylated hCG). PMID: 19171054
lutenizing hormone - (LH) pituitary, protein hormone
melaocyte stimulating hormone - (MSH) pituitary, peptide hormone
prolactin - (PRL) pituitary, peptide hormone
parathyroid hormone - (PTH) parathyroid, peptide hormone
thyroid hormone - (TH) thyroid,amino acid derivative
thyroid stimulating hormone - (TSH) pituitary, protein hormone
Glossary Links
- Glossary: A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | Numbers | Symbols | Term Link
Course Content 2009
Embryology Introduction | Cell Division/Fertilization | Cell Division/Fertilization | Week 1&2 Development | Week 3 Development | Lab 2 | Mesoderm Development | Ectoderm, Early Neural, Neural Crest | Lab 3 | Early Vascular Development | Placenta | Lab 4 | Endoderm, Early Gastrointestinal | Respiratory Development | Lab 5 | Head Development | Neural Crest Development | Lab 6 | Musculoskeletal Development | Limb Development | Lab 7 | Kidney | Genital | Lab 8 | Sensory - Ear | Integumentary | Lab 9 | Sensory - Eye | Endocrine | Lab 10 | Late Vascular Development | Fetal | Lab 11 | Birth, Postnatal | Revision | Lab 12 | Lecture Audio | Course Timetable
Cite this page: Hill, M.A. (2026, February 27) Embryology 2009 Lecture 20. Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/2009_Lecture_20
- © Dr Mark Hill 2026, UNSW Embryology ISBN: 978 0 7334 2609 4 - UNSW CRICOS Provider Code No. 00098G