Paper - Concerning the origin and nature of certain malformations of the face, head, and foot
| Embryology - 30 Apr 2024 |
|---|
| Google Translate - select your language from the list shown below (this will open a new external page) |
|
العربية | català | 中文 | 中國傳統的 | français | Deutsche | עִברִית | हिंदी | bahasa Indonesia | italiano | 日本語 | 한국어 | မြန်မာ | Pilipino | Polskie | português | ਪੰਜਾਬੀ ਦੇ | Română | русский | Español | Swahili | Svensk | ไทย | Türkçe | اردو | ייִדיש | Tiếng Việt These external translations are automated and may not be accurate. (More? About Translations) |
Keith A. Concerning the origin and nature of certain malformations of the face, head, and foot. (1940) Br. J. of Surgery.
| Historic Disclaimer - information about historic embryology pages |
|---|
| Pages where the terms "Historic" (textbooks, papers, people, recommendations) appear on this site, and sections within pages where this disclaimer appears, indicate that the content and scientific understanding are specific to the time of publication. This means that while some scientific descriptions are still accurate, the terminology and interpretation of the developmental mechanisms reflect the understanding at the time of original publication and those of the preceding periods, these terms, interpretations and recommendations may not reflect our current scientific understanding. (More? Embryology History | Historic Embryology Papers) |
Concerning the Origin and Nature of Certain Malformations of the Face, Head, and Foot
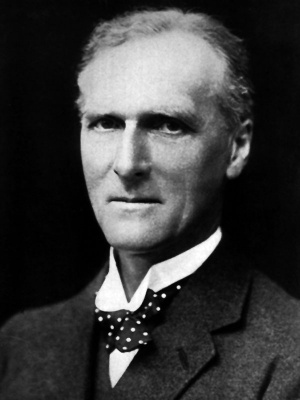
By Sir Arthur Keith, F.R.S.
Rather more than thirty years ago I gave a series of demonstrations at the Royal College of Surgeons of England on specimens—some 250 in number—illustrating congenital malformations of the face. Amongst them was a form, depicted in Figs. 84, 85, which I found difficult of explanation. A furrow or groove is seen to pass from the angle of the mouth; it may reach the external auditory meatus as in Fig. 84, or it may cease at or near the anterior border of the masseter as in Fig. 85. In Fig. 84 the groove is still open, and has a pink lining membrane.
Fig. 84. Photograph of a child of 14 months
Fig. 85. Photograph of a ho in which the groove showing a congenitaf groove on right check. (0. H. shown in Fig. 84 has become led by scar tissue. Edz'ngzan’s case.) There is a tag or appendage growing from the scar.
The tragus is divided (supemumerary auricle). The letter which accompanied this photograph has een mislaid, so that I am unable to acknowledge its donor.)
In Fig. 85 the groove has been filled up by cicatricial tissue; a tag-like appendix grows from the scar; the tragus of the car has an accessory cartilaginous process placed beside it. As is usual in such cases there is in Fig. 84 an open fissure at the outer angle of the mouth; the groove continued the line of the fissure. These small pedunculated processes of skin are often present. Fig. 86, taken from a photograph loaned to me by the late Prof. William Wright, shows a child with such a process (I) and the position of processes in two other cases (2. 3). In Dr. Wright’s case, too, the tragus shows a division or accessory auricle (4). In Fig. 87 these tags are represented by an ‘ amniotic adhesion ’—which after encircling the left arm ends on the inner surface of the placenta, where it is joined by another ‘ adhesion ’ which issues from an occipital meningocele. This case was reported by von Winckel?
FIG. 86.—Taken from the photograph of a child in which there was a congenital . crease crossing the left cheek from mouth FIG. 87.—A fibrous band (amniotic adhesions arising along to ear. I, A cutaneous tag; 2, 3, The the site of an ear-mouth congenital groove in a 5.‘, months foetus. position of tags on two other cases; 4, A Another band is of similar nature and arises from the apex of an divided tragus ; 5, The position of the ear occipital meningocele. I. Band; 2. Umbilical cord ; 3. Placenta; (first) cleft—were it to persist. 4, Meningocele. (After mm Winckel.)
Streeter’s Fetal Dysplasia
Many other cases have been reported3, but so far no satisfactory explanation of their production has been given. The explanation I am now to offer is based on a research carried out by Dr. George L. Streeter,‘ who has presided over the Department of Embryology of the Carnegie Institution, Washington, for many years and whose important contributions to our knowledge of the development of the human body deserve to be better known to surgeons than they now are. By 1930 Dr. Streeter had at his disposal 16 cases of a condition he speaks of as “focal deficiencies in foetal tissues”, but which, as its aetiology is as yet imperfectly understood, I propose to name, in the meantime, ‘ Streeter’s foetal dysplasia ’. It is the source of many forms of congenital malformation. Dr. Streeter is inclined to ascribe the lesions which become manifest in the foetus as it develops to a fault inherent in the chromosomes of the fertilized ovum. This may be so, but in the meantime, for reasons I shall adduce later, it is more profitable for us to regard the fault as lying in a temporary—or
Fig. 88. The medial “pm permanent—breakdown in the circulatory system of the
gr thed leftbfopt agd leg €54/the fuetus. I S CSCH E III! CIEXC. I87‘ . . gxtrgeter.)
Let us examine the outward signs of Streeter’s dysplasia as manifested in his youngest case, a male foetus, I4 weeks of age (sitting height 86 mm.), removed by operation, with membranes intact. The mother had suffered from uterine fibroids and metrorrhagia; the foetus had been dead some weeks before the date of operation; the placenta was “ delicate and easily torn”. In Fig. 88 is shown the left foot and leg of this foetus. The distal parts of all the toes have been lost by a process of ‘ foetal necrosis ’; round the leg, just above the ankle, is a circular necrotic groove filled with exudative tissue in which there is embedded a constricting ring or anklet of fibrous tissue. On the right leg there is a corresponding groove and ring, but the toes are intact. The anklets of the two sides had become joined, so that the legs were bound together. Three fingers of the left hand and all the digits of the right hand were encircled by fibrous wrappings of the same exudative material and the parts distal to the wrappings were undergoing separation and necrosis. Clearly we are witnessing a stage in the process which gives rise to intra-uterine amputations.
In Fig. 89 a section along the right leg of this foetus is given to show the arrangement of parts in the groove which contains the constricting ring of fibrous tissue. On one side (A) the groove is occupied by a loosely organized exudate, near the base of which two strands of the constricting fibrous ring are seen on section. The base of the mass springs from a necrotic layer of fascia—under which there is a bending in and compression of the muscular stratum. The epidermis has become detached—but above A a remnant is seen to descend to the bottom of the groove—which had been covered with cutaneous epithelium. When the necrotic layer of fascia, with which the exudative mass in the groove is continuous, is traced upwards and downwards it is seen to become continuous with both the cutis and the deep fascia, these two being widely separated, both above and below the groove, by subcutaneous tissue. At the bottom of the groove, then, cutis and deep fascia become fused into a single fibrous stratum; on the other side of the leg (B) cutis, deep fascia, muscle, and periosteum are fused into one stratum. The stratum on this side of the leg is not necrotic but remains very much alive and has grown out to form a tag-like appendage, covered with epithelium, and in every way comparable to the dermal tags found springing from the buccal grooves of the face. At each side of the base of the tag and within the groove are seen sections of the armular constricting fibrous band.
Fig. 89. Section along the right leg of the same fa:tus to show the necrotic annular groove and the structures contained within it—a diagrammatic rendering of Dr. Streeter’s illustration (Fig. 14, Plate I). I. Cutis; 2. Deep fascia; 3, Muscle; 4, Epidennis; 5, Organized exudate; 6. Bands; 7, Tibia; 8, Fibula; 9, Tag. For further explanation, see text.
If we examine the lesion in the hands of this foetus we shall obtain more light on the peculiarities of fcntal dysplasia. The initial lesions lead on to intra—uterine necrosis and amputation. In Fzg. 90 a dorsal View of the left hand is depicted ; three digits are wrapped in fibrous exudate 5 at the proximal margin of the fibrous bands a line of separation has been demarcated. Fig. 91 is taken from Dr. Streeter’s section of the right hand, which exposes a longitudinal view of the thumb. All the soft tissues of the thumb are seen to end opposite the middle of the proximal phalanx in a circular mass of organized fibrous tissue; the part of the thumb distal to the fibrous ring is disorganized and on its way to being shed. The epidermis is seen, on the dorsal aspect of the thumb, to end in a thickening at the proximal base of the fibrous ring. The fibrous ring on the dorsal aspect of the thumb is adjacent to, and partly adherent with, a constricting band which surrounded an adjacent finger.
Fig. 90. Dorsal aspect of the left hand of the foetus described in the text. I. Fibrous band ; 2. Line of separation. (After _Str¢ezer.)
FIG. 91. A longitudinal section of the thumb of the right hand of the same fetus, showin the tissues ending in a fibrous.ring which surroun s the proximal phalanx. The distal part of the thumb is semi-necrotic. On the dorsal aspect of the thumb the fibrous ring is made up of _two pans: the distal part surrounded an adiacent digit. I. Band; 2. Subcutaneous tissue; 3. Proximal phalanx; 4. Tendon; 5. Epidermis, dorsal aspect ; 6. Band of 3rd finger; 7. Distal part of thumb. (Diagrammatized from Dr Streeter’s illustration, Fig. 15, Plate 1.)
Fig. 92. Left foot of a female ftztus, 27 weeks FIG. 93.—Section across crease shown in Fi . 92, of age, illustrating a stage in the progress of Streeter’s made so as to expose the fibrous (amniotic) ban , also dysplasia. I. Scar; 2. Band; 3. Crease. (After shown in Fig. 9?. I. Deep fascia; 2. Epidermis; Stream.) 3. Band.
A later stage in the progress of Streeter’s dysplasia is illustrated by the specimens shown in Figs. 92, 93. They are taken from a case of Dr. Streeter’s—-a foetus of about 27 weeks, and therefore some I 3 weeks older than the foetus we have just been describing. In the present instance the right foot had become shed or amputated above the ankle and the stump was healing. The amputated foot was found in the cavity of the amnion ; in size it corresponded to that of a foetus of about 16 weeks. The left foot of this case is shown in Fig. 92. Above the ankle there is a transverse crease from which issues a fibrous cord. A section along the base of this cord and across the crease is shown in Fig. 93. The base of the cord appears to issue from the deep fascia and passes through the epidermis, finally becoming devoid of epithelial covering. The more superficial fibres of the cord are nucleated. It is also important to note other pathological lesions in the left foot—namely, scarred tissue on the medial side of the ankle and in the subcutaneous tissue over the dorsum of the foot, which is dense and contracted. Digits in both hands are embedded in fibrous bands ; the distal parts of some of the digits have been shed.
Such then are the external manifestations of Streeter’s dysplasia. The condition at the end of the 6th month of foetal life shows many changes from those we have noted at the end of the 3rd month. But even at the end of the 3rd month the dysplastic condition must have reached an advanced stage. Circumstantial evidence points to the end of the 2nd month of development as the period of incidence. It is then that toes and fingers, the most common sites of this disorder, are just assuming their discrete shapes.
We have noted Dr. Streeter’s opinion that the defects just described are due to a developmental factor inherent in localized areas of tissue in the distal parts of the limbs of afflicted foetuses. Were a surgeon to approach such cases and note the signs with which he is familiar in cases of gangrene, he would immediately suspect a breakdown in the supply of blood to the developing extremities. He would the more readily look for a temporary or permanent failure in the general circulatory system seeing that all four limbs are usually affected to a greater or less extent. He would examine the placenta and umbilical cord for evidence of such a failure and if he did so in Dr. Streeter’s cases he would find in nearly every one evidence of defect and circulatory failure. At the end of the 2nd month of development, which appears to be the period at which foetal dysplasia of the limbs usually begins, the placenta is undergoing a rapid expansion and is therefore in its most vulnerable phase of growth.
Gangrene of the hands and feet of a fcntus of the 3rd month follows a totally different course from that seen in the limbs of an adult. In the first place, the tissues of the foetus are less dependent on blood-supply for health and growth than are the same tissues in an adult. The human heart begins to beat about the 24th day; until then the tissues are dependent on lymph seepage ; it is not until towards the end of the 2nd month that a cardiac circulation is fully established. Foetal tissues have a higher degree of vitality and individual response than have mature tissues. Some foetal tissues, such as the fibroblasts of the skin and deep fascia, respond in a particularly vigorous manner when cut off from their bloodsupply. In Figs. 89, 91, 93, the fibrous outgrowths, which are formed at lines of partial or of complete separation of tissues, spring from the deep fascia.
In the second place, foetal limbs are suspended in amniotic fluid, and kept at body temperature, circumstances which are, as Dr. Streeter has pointed out, particularly favourable for ‘ tissue culture ’. When the rings of separation first appear on digits and distal parts of the limbs, there must be a free exudate of lymph along the lines or grooves of tissue separation. Into these grooves of separation fibroblasts of the deep fascia and cutis spread and there multiply, thus forming fibrous cords or bands. Even along such a fibrous process as is depicted in Fig. 93 there must be a seepage of lymph from the deeper tissues of the foetal limb. In this way are formed all of these pathological formations known as ‘ amniotic bands ’ 5 all of them are formed from and by the foetus at sites of tissue injury.
We have made this long detour in our narrative in order to clear up the nature of certain anomalous fissures, creases, and integumentary processes which occasionally mar the human face. Before returning to a consideration of these deformities, however, there are still two other embryological researches we must take into consideration.
Vascularization of the External Coverings of the Head
One of these researches is by Miss Ellen B. Finley,5 a pupil of Prof. Florence Sabin. In Fzg. 94 I take the liberty of reproducing one of her illustrations, because
in length and in the 8th week of development. The process of vessel formation (angiogenesis) which leads to vascularization of the scalp is seen spreading upwards in the temporal and occipital regions of the head.
FIG. 94. Profile of a foetus 23 mm.
FIG. 95. The point reached by the wave of scalp vascularization in the 9th week. (After Miss Finley.)
FIG. 96. To illustrate the manner in which the scalp becomes vascularized. I, Vascular wave; I. Avascular zone; 2, Angioblastic zone;
2, Ear. (After Ellen B. Finley, ‘ Contributfons to Embryology ’, 1922.)
3. Capillary plexus ; 4, Definitive vessels. (After Miss Finley.) 4 (Q
It depicts a human foetus at the stage of development which marks, as we suspect, the onset of Streeter’s focal dysplasia. The fingers are already formed; the toes are in process of demarcation. Two waves of vascular tissue, one in front of the ear, the other behind, . are ascending on the temporal and occipital regions of the head of the foetus; above these waves the scalp and coverings of the skull are still devoid of a blood-supply. Hochstetter of Vienna drew attention to this vascular invasion of the scalp in I916 ; Miss Finley investigated the mode and rate of its growth. I can best summarize her observations by drawing the reader’s attention to Figs. 95, 96, which are based on her original illustrations. Fig. 95 shows the line reached in the scalp of a foetus a week older than that depicted in Fig. 94. A week later still—that is, about the end of the Ioth week—the waves of invasion on each side of the head will have met along the midline, thus completing the vascularization of the scalp. It is important to note the manner in which the growing margin of the wave is advanced. Miss Finley found that the mesenchyme of the scalp, just in advance of the growing margin, becomes transformed into red blood-cells and vascular endothelium; the scalp is not invaded by new vessels sprouting from the old, but provides the material for vascular extension.
Let us suppose, for a moment, that during the extension of the vascular network into the scalp, a partial and temporary breakdown‘ of the placental circulation should take place 3 then we may justly infer that it would be the growing margin of vascularization that would sulfer the chief damage. Prof. H. A. Harris“ has demonstrated that the growing ends of long bones reflect the illnesses of childhood, for instead of normal bone being laid at the growing disc a dense plate is /i‘ r formed. At the growing margin of vascularization of the SCa1P dense _ FIG. 9_7.—The most common type of amniotic adhefibrous tiSSu€ results: giving rise to congenital defects of the scalp (Fig. 97). We may transfer these observations to the dysplasia described by Dr. Streeter in developing feet and hands, for, as we have seen, the initial damage falls on subcutaneous strata, corresponding to those of the scalp. At the end of the 2nd month of development the distal parts of the human extren1ities—hands and feet—are still in the capillary stage of vascularization.
Congenital Defects in the Mid-Dorsal Line
The other embryological research I have to touch upon is that made by my old friend Dr. N. W. Ingalls.7 He has described a series of human foetuses, which were in the 2nd and 3rd months of development, all of them showing plastic defects along the rnid-dorsal line of the body. So far as the clinical histories of these foetuses are available they point to a circulatory failure, with cystic villi in the placenta, a more or less avascular condition of the umbilical cord, hydramnios, then death in the 2nd or 3rd month of development, with expulsion from the uterus some weeks after foetal death. Along the midline of the foetal head Dr. Ingalls noted blebs or collections of fluid which may be situated under the epidermis or more deeply, in the subdermal tissues. He noted in particular that areas of the fascial tissues along the mid-dorsal line of back and head were behaving in a way very similar to that of fascial tissues at the lines of separation in Streeter’s dysplasia. Dr. Ingalls also called attention to the fact that the dysplasia may not take the linear form seen in the digits and ankle, but may involve an irregular area of dermal and subdermal tissues of greater or less extent. Dr. Streeter noted such areas on the limbs of several of his cases (see Fig. 107).
The activities and responses noted in dermal and subdermal tissues along the midline of the head and back of the foetuses described by Dr. Ingalls are of the same nature as those we have noted in Streeter’s dysplasia. As further evidence in support of this inference I call attention to the occurrence of a circulatory (placental) failure, the occasional occurrence of amniotic adhesions, and the fact that dysplastic lesions of the digits and feet may accompany the midline changes described by Dr. Ingalls. We infer that the failure of circulation in such foetuses as have just been noted will fall first and most severely on the vascularization of the subdermal tissues of the midline which takes place during the later weeks of the 2nd month and the earlier part of the 3rd month. Meningoceles.—Meningoceles are structures of obscure origin; they occur along the mid-dorsal line of the head, the two most common sites being occipital and frontal. Dr. Ingalls’ research seems to me to throw light on the origin of meningoceles and to bring them into the same category of lesions as those which we have seen in Streeter’s dysplasia. In Fig. 98 we have copied one of his illustrations—a side view of a foetus at the end of the 2nd month of development and showing a ‘ bleb ’ situated in the midline of the occipital region. The covering of the bleb is translucent and sub-ectodermal in origin; blood has leaked into its fluid content. The chorionic villi were found to be “ swollen, irregular, and smaller cystic forms are quite plentiful”, from which we infer there must have been a defective placental circulation. Suppose the circulatory breakdown proved to be temporary and that the foetus continued to develop, what would have happened to the occipital bleb? I take it that its walls would have collapsed and that the dermal and subdermal tissues thus exposed would have formed a weak fibrous wall over the 4th ventricle—the possible site of a meningocele.
FIG. 98. Profile view of the left side of a fetus at the FIG. 99.—Dorsal_ view of a pathological end of the 2nd month of development (25 mm. in length) in embryo, 18-5 mm. in length, but showing which there is a large subepidermal bleb over the region of evidence of arrested development, in which the 4th ventricle. I. Umbilical cord; 2. Bleb. (After N. W. there is a dysplastic area over the 4th ventricle. Ingalls.) I. Dysplastic area. (After N. W. Ingallx.)
The foetus depicted in Fzjg. 99 presents us with a different and earlier lesion. This foetus shows many signs of arrested development and represents a stage which is younger than that seen in Fig. 98 by about two weeks. “In the dorsal midline ”, to quote Dr. Ingalls’s words, “ about the region of the lower rhombencephalon, there is a small, transversely elongated, somewhat smoother, discoloured area, slightly greenish in colour. It is roughly reniform in outline, sharply marked from the surrounding parts, slightly elevated and measures about 3 by I mm.” The discoloured area, when sectioned, showed extensive histological changes, especially in the connective tissue immediately under the discoloured epithelium. The densely cellular fibroblastic area was sharply circumscribed. The fibroblastic reaction seen here seems to be of the same nature as that which Dr. Streeter has described in connexion with necrosis of the digits. If hydrocephalus were to set in, as it often does in foetuses which are the subjects of the lesions we are dealing with, then this area over the roof of the 4th ventricle would provide a favourable site for the origin of an occipital meningocele. We can understand, too, why an exudate occurs in lesions which are accompanied by the formation of “amniotic adhesions” of the kind illustrated in Figs. 87 and 97. In the case of the foetus depicted in Fig. 99 there must have been a circulatory collapse, for the chorion was “ very thin, villi were absent save in one area ” and “ no vessels were to be seen anywhere ”..
Congenital Facial Defects
Buccal Grooves and Creases.—We are now in a position to return to a consideration of the congenital grooves and scars which cross the human cheek— from the angle of the mouth towards the ear—which they may reach. When they do reach the ear the tragus is usually subdivided (see Fig. 86). The appearance and character of these grooves are similar to those presented by the feet and hands in cases of Streeter’s dysplasia, and to the lesions described by Dr. Ingalls in the
P.)
FIG. lC0.—The point reached in the development of FIG. 10l.—The same embryo seen in full face. the face of the human embryo towards the end of the |. Mid-brain; 2, Cerebral vesicle; 3. Mesial nasal 6th week (10 mm. in length). As seen in profile. I. Mid- process; 4, Lateral nasal process; 5. Maxillary brain; 2. Cerebral vesicle; 3. Lateral nasal process; 4, process; 6. Cheek; 7. Fronto-nasal process; 8. Mesial nasal process ; 5. Nose; 6, Maxillary process ; 7, Mandibular process. (After Prafessar 5'. E. Frazer.) Mandibular process; 8. Hyoid process; 9, Ear; IO, Cheek; ll, 4th ventricle ; I2, Eye. (After Professor 3'. E. Frazer.)
scalp and along the mid-dorsal line of the head and spine. The integumentary tags which spring from facial grooves are of the same nature as those which may be found in grooves of separation at the ankle (see Fig. 89). Further, it will be clear from Figs. IOO, IOI (which represent the condition of the mandibular and maxillary processes in the face of a human embryo towards the end of the 6th week of development) that these two processes spring from a common base which occupies all the space between the eye and ear, this common area representing the groundwork of the cheek. It is true that the angle of the mouth makes an approach to the ear, _but as development proceeds the mouth is advanced by growth of tissue within the foetal cheek, not by a union of the adjacent free borders of the maxillary and mandibular processes. In certain cases the whole thickness of the cheek may necrose, leaving part or the whole an open cleft from mouth to ear. An open condition of the cleft is spoken of as macrostoma.
The buccal grooves or creases, then, do not represent the edges of an ununited embryological cleft, such as occurs in hare-lip, but have to be accounted for in some other manner. As we shall see later, Dr. E. Wolffs, on subjecting the heads of fowl embryos to measured exposures of X rays, thus damaging the tissues which go to form the maxillary and mandibular processes, produced a superficial defect similar to the congenital lesion we find on the human cheek. In the chick the chief defect lies in the superficial or dermal structures—just as is the case in mandibular maxillary creases of the human foetus. The congenital crease which appears on the human cheek lies between two developmental territories—between the mesoderm of the mandibular and of the maxillary processes. Each foetal process has its own independent blood-supply ; that of the maxillary process being the internal maxillary artery, while the mandibular is supplied by the vessel which becomes subsequently the inferior dental. The congenital linear lesions of the cheek appear to develop along the line at which the vascularization of the mandibular process meets with that of the maxillary process. It is along lines of vascular union that corresponding defects are apt to occur in the dorsal midline of the body where right and left processes of vascularization meet. When we find the buccal crease at its earliest point of development I expect it will show a superficial or complete linear necrosis, with exudate, the formation of fibrous bands, amniotic adhesions, healing, and integu— mentary tags (see Fig. 87). In brief, I regard buccal creases as a facial manifestation of Streeter’s dysplasia. The facial artery which crosses the ventral ends of the mandibular and maxillary territories in the later months of ftrtal life, is a secondary formation.
Median Cleft of Lower Lip and Mandible.—In Fig. I02 is depicted a case of median cleft of the lower lip and of the mandible, which occurred in the practice of Sir Wm. MacCormick, of Sydney; he presented a model of the case liHauar1):dcii1ai'i)¢i2ibTe‘IIJfn a° ‘i‘§lla°i.f§é’ f4di=iol§ii:§r, to the Museum of the Royal College of Surgeons
' d 1 ' 1 ' h ‘ ' . . . of sthgtlggniralsgnacisilcofsihg arigtme liifiimigii of England. As W111 be seen in Fzg. 101, the
ventral ends of the mandibular arches are not
normally separated by a cleft; being formed within the lower margin of the embryonic mouth (stomodaeum). This is a midline lesion of the same kind as Dr. Ingalls described in connexion with the midline of the dorsum of the head and back. The margins of the cleft have the cicatricial appearance of dysplastic lesions. Schwalbe“ figures a similar case and also one
in which the fissure has undergone cicatricial healing. CERTAIN CONGENITAL MALFORMATIONS I83
Oro-temporal Cleft.—In Fig. 103 an uncommon form of dysplastic lesion is illustrated. It crosses the right check of a full-time foetus, passing from the angle of the mouth to end in a wide depression in the right temporal region, where the floor is formed by a dense membrane, representing all the tissues on the lateral wall of the head from skin to dura mater; a similar cleft crosses the left cheek. It will be remembered that in severe cases of Streeter’s dysplasia of the extremities all the tissues, from skin to bone, are involved (Fig. 89). So it is there. It will be observed that this fissure crosses the territory of the I ‘ maxillary processes; the lesion does not fall, as others we have described, at the junction of two territorial areas. A similar fissure is illustrated in Fig. 112.
Extreme Foetal Defects.——We now pass on to the consideration of dysplastic lesions of the face which are acconjpanied maldevelopmcnts of FIG. l03.—A dysplastic lesion crossing the cheek of a full-time child from the mouth to the right tern oral region. thC facial CICIIICIIIS I0 SllCh CXIICIIIC I . Upper parietal area; 2, Temporal area of cle t; 3. Lower degrees that they cease to concern us 5iiii.:ic1aair%.i11e4£zgX§°1x2I."Eis?'Ai3zii:i3i.,pii/‘Z.iiioiisgf) (Tm from a surgical point of view, and are mainly of pathological interest. In Fig. 104, which has been drawn from a fulltime foetus (No. 356 in the Teratological Collection of the Museum of the Royal College of Surgeons of England), the various processes which grow into the stomodaeum to form the face have been arrested at an early stage of development,
FIG. 104.—Dysplastic and other malformations in FIG. 105.—Face of full-time fetus with ectopic the face of a full-time fcetus. I, Integumentary tag, cranial membranes and a dysplastic malformation of at the end of a dys lastic crease (2), which begins at the face. I and 9, Massed ectopic and dysplastic the outer canthus o the eye; 3. Fronto-nasal process membranes of brain; 2. Right nostril; 3, Right maxilcarrying median part of the upper lip and premaxilla ; lary process ; 4, Lower lip; 5. Left maxillary process; 4, Right maxillary process; 5. Lower lip- 6. Left 6. Left eye 5 7, Left lateral nasal process ; B. Dysplastic maxillary ‘process 5 7. Fibrous, dysplastic bat-id’ ; 8. Left furrow between the left lateral and left mesial nasal pronostril an nasal process; 9. Right lateral nasal process. cesses, ending above in the ectopic mass of membranes.
a wide cleft, separating the maxillary .and nasal processes, remaining below and to the mesial side of the left eye. Extending from the outer canthus of the right eye there is a trace of a crease which ends in a tag situated in the right temporal region.
This dysplastic crease lies at the junction of two vascular territories, namely, the frontal, supplied from the ophthalmic branch of the internal carotid, and the superficial temporal, from the external carotid. A fibrous band is seen to cross the left upper eyelid—an additional sign of dysplasia. This specimen also interests us from another point of view. The dysplastic lesions are accompanied by a severe arrest in the process of facial development. Complete failures in the union of the nasal and maxillary processes are so frequently combined with dysplastic lesions (Fig. 105) that we may suspect that they share in the same pathological disturbance.
In evidence of the statement just made, I cite two more of Dr. Streeter’s cases. One of these is illustrated in Fig. 106; it is that of an infant, 5 months of age, in which there is double hare-lip and cleft palate, with dysplastic lesions in fingers and toes. These lesions I have supposed to make their appearance towards
FIG. l06.—A. Face of an infant of 5 months, showing non-union of nasal and maxillary processes: I. Right lateral nasal process ; 2, Skin of median part of upper lip, and 3, the premaxilla—both formed in the fronto—nasal process; 4, Maxillary process. B, Fingers of the right hand showing constrictions on fourth and fifth digits. C. Digits of the right foot; the distal part of the great toe has undergone intra-uterine amputation, while the distal parts of the second and third toes have been partially destroyed.
the end of the second month of development, but if the facial clefts and the constriction of the digits arise from the same pathological state (a breakdown in the placental circulation) and at the same time, then the onset is earlier than I have stated. For if reference is made to Fig. IOI, which shows the point reached in the development of the face at the end of the 6th week, then we have to go back to this early stage to account for the facial cleft.
In Fig. 107 there are depicted associated lesions in another of Dr. Streeter’s foetuses. The case is that of a full-time, stillborn foetus with massed ectopic membranes on the head and a nasal cleft or furrow——a1most a replica of the condition shown in the specimen depicted in Fig. 105, save that the nasal furrow lies along the right side of the nose instead of on the left side, as in the previous case. With these lesions in the head of the case described by Dr. Streeter, there were associated typical dysplastic lesions of both feet and of the left hand. The condition of the left foot and leg is represented in Fig. I07, B. There is a deep annular crease or furrow, which fuses at its inner limits with the deep fascia of the leg, but its sides are now lined with normal skin. The great toe, which had undergone intra-uterine amputation in the right foot, is practically intact, but the distal parts of the second and third toes are in process of separation or have separated. There are also cicatricial areas on the dorsum of the foot and on the extensor aspect of the leg, indicated in Fig. 107, B.
Anencephaly.—Now the dysplastic lesions of the extremities are associated with ectopia of the brain with a suflicient frequency to raise the suspicion that they may be manifestations of the same underlying pathological disturbance occurring during the development of the foetus. If this is so, and if all the lesions are simultaneous in onset—which they need not be—then we have to seek for the disturbance at a still earlier stage of development. The arrest which brings about anencephaly or ectopia of the brain must be traced back to defects occurring in the 4th week of development.
FIG. 107.—A, Head and face of a full-time fcetus, showing the membranes of the brain massed and exposed on the head, with a dysplastic furrow or depression ascending in the nose from the mouth to the exposed membranous mass: I, Right eye; 2, Right lateral part of nose; 3. Right maxillary process ; 4. Lower lip ; 5. Left maxillary process ; 6, Left eye ; 7, Median and left part of the nose ; 8, Dysplastic furrow ; 9. I0. Ectopic membranous masses. B. Left leg, showing : I, Dysplastic area on leg; 2. Annular dysplastic furrow; 3, Dysplastic lesions of toes; 4. Dysplastic area on dorsum of foot.
Dodds and De Angelis9 have described a human foetus showing a very early stage in the development of anencephaly; their description helps us to understand some of the lesions we are dealing with. A profile view of their specimen is reproduced in Fig. 108, and a dorsal view in Fig. I09. The foetus is only I6-5 mm. in length and is probably at the end of its 2nd month, yet development of the brain has been arrested at the stage reached in the 4th week, when the neural plates, which should become enclosed to form the brain, and the mesodermal tissue, which should provide membranous and cranial coverings, lie exposed on the cephalic extremity of the embryo.
We have here a repetition of the same kind of failure which at the caudal end of the embryo gives rise to spina bifida. Our authors found, as occurs in cases of spina bifida, that all the issuing cranial nerves and their attached ganglia had been formed with the exception, in this case, of the 8th nerve. In the face they found a double hare-lip and the limb buds showed some degree of arrest. Almost the 186 THE BRITISH JOURNAL OF SURGERY whole of the neural plate, which here remains exposed to the action of the amniotic fluid, has disappeared, only one area remaining attached to the underlying mass which represents the membranous coverings of the brain. In our illustration an interrupted line (4) marks the junction of skin with the membranous vascular masses exposed on the head of this ftetus. In the latter part of the third week and earlier part of the fourth, had development pursued its usual course, these lines, now situated on the sides of the head, would have met along the rnid-dorsal line and embryological union or ‘ healing ’ would have taken place.” When a section is made across the line at which the skin meets with the membranous mass——at a later stage than that represented in Figs. I08, Io9—the appearance presented is very similar to that
Fig. 108. Profile of a human fcetus, 16-5 mm. in length and at about the end of the 2nd month of development. I. Detached part of the neural platethe only part that was found ; 2, Masses representing membranes of the thalamencephalon; 3, Masses representing the cerebral membranes; 4. Line along which skin meets with capsular tissues of skull and brain; 5, Eye ; 6. Median fissure of face ; 7, Ear ; 8, Membranous mass of hind-brain ; 9. Membranous mass of midI0. Funnel-shaped opening leading to central
brain; (Figs. 108, 109 after Doddr and canal of spinal cord. De Angelis.)
FIG. 109.—Dorsal view of the same fcetus. The numbers have the same significance as in Fig. 108.
met with in the dysplastic lesions described by Dr. Streeter (Fig. 110). At the bottom of the crease or furrow the subcutaneous tissue of the scalp is
replaced by a dense fibrous stratum, which passes into the adjacent vascular membranous mass. Fibrous or desmoplastic bands are extruded from the mass. This marginal zone is the most common site of ‘ amniotic ’ adhesions.
The dimensions of the vascular membranous masses which crown the heads of anencephalic foetuses have often puzzled me. When we remember: (I) That the cerebral circulation is possible only within an enclosed capsule; and (2) That such vascular tissues exposed to the amniotic fluid at body temperature are thus placed in the most favourable circumstances for ‘tissue culture ’—then we can understand the changes which take place, particularly the formation of adhesive bands in the exudates of lymph. Anencephaly is so often combined with other forms of embryological failure, such as hare-lip, cleft palate, and other signs of Streeter’s
dysplasia, that one may well suspect that the underlying pathology is the same for
a1l—a nutritional disturbance.
Now at the time the medullary plates are rising up
FIG. 110.—Section of the head of a full-time anencephalic foetus at the junction of the skin and membranes. tissue; 4, Scalp.
The section was made near the mid-line.
I, Membranes; 2. Groove; 3, Cicatricial
to be enclosed, the circulation of blood is only about to be initiated. In Fig. III I reproduce a case published by von Winckelz to illustrate the formation of ‘ amniotic
after the brain has become It also throws light on the two
adhesions ’ enclosed.
cases depicted in Figs. 105, 107, where clefts of the nose are associated with anencephalic masses on the head. In Fig. 111 the fibrous bands pass up the forehead to end in tissue masses which are extruded on the crown of the head; each band commences at the margins of what was an olfactory pit and fold. Such bands I presume to be formed within necrotic grooves just as are the fibrous anklets and bracelets in Streeter’s dysplasia. As the head expanded, these bands, being resistant, have dragged the olfactory pits towards the crown of the head.
Why should necrotic grooves be formed along the line of these bands? The area between the bands is that supplied by the terminal branches (frontal) of the ophthalmic arteries. The areas outside the bands are supplied by the supra—orbital vessels and by
FIG. 11l. Head of human fetus with symmetrical fibrous (amniotic) bands on the forehead, double hare-lip. and cleft palate._ I. 9. Right and left frontal bands; 2. 2. Right and left olfactory pits drawn up by bands; 3. F1-onto-nasal process; 4. Right upper lip ;_ 5. Lower li ; 6, Band formed in oro-orbital groove; . Left ear; 8. Left upper li ; I0. Extrusion masses (meningoceles ?): (Afitr von Winckcl.)
the temporal branches of the external carotid. As in other cases of dysplasia of the face and head, the necrotic groove and bands are formed along marginal areas.
In Fig. II2 an anencephalic condition is combined with three examples of dysplastic fissure of the face. The case was recorded by Marchand.“ On the right cheek a fissure passes from the angle of the mouth to the temporal region, as in the specimen depicted in Fig. 103 3 on the left cheek a fissure or crease ascends from mouth to orbit (as in Fig. I13), while a continuation into the left temporal
FIG. lI2.—A case recorded by Marchand showing dys- FIG. ll3.—Woman with dysplastic fissure plastic fissures of the face. I, Anencephalic masses; 2. (healed) passing from left upper lip to left lower Right oro-temporal fissure ; 3, Left om-orbital fissure; 4, eyelid. (SchwaIbe.)
Left fronto—temporal fissure.
region corresponds to the temporal crease shown in Fig. 104. Here we have dysplastic fissures at three sites associated with an anencephalic condition.
Fissure from Lip to Eyelid.—There is no dysplastic lesion of the kind shown in Fig. 113 in the Museum of the Royal College of Surgeons of England; nor have I had the fortune to see one, and yet Schwalbe“ depicts this condition in 5 cases. The scar line in Fig. 113 passes upwards on the right check from upper lip to lower eyelid, lateral to the position of the embryological groove in which the nasal duct is formed. Like the fissure shown in Figs. I03, I12, the scar line crosses the territory of that part of the cheek formed by the maxillary process, but in Fig. 113 it lies near to the junction of this process with the lateral nasal. Lateral to the scar is the area supplied by the infra-orbital branch of the internal maxillary artery, while medial to it is the nasal area fed by terminal branches S). of the ophthalmic artery. I suppose that the necrotic groove is formed along the junction
I of these two vascular areas.
FIG. 1l4.—A fine fibrous band uniting the -Band Tongue to Palate.-—Fl:g. rluggum of'fl;eB{ong1.1e3[oPplgx-fially rem ,I,.,1,,ei 114 is a drawing made from a preparation in ¢,,,,f,'§fi’,,f’R_;;__2{‘ A;,,,,;,.,§,“}f,;,_ ‘2o§f$_‘§’ "W" the Teratological Collection of the Royal
College of Surgeons Museum. It represents the tongue and palate of an anencephalic foetus in which the posterior part of the median fissure of the palate remained ununited: a fine fibrous band passes from the palatal cleft to the fraenum of the tongue. We have seen, in connexion with dysplastic lesions of the extremities, how neighbouring parts may become united by the organization of exudates of lymph. We have also seen that severe degrees of hare-lip and cleft palate may be associated with dysplastic lesions of the limbs and anencephalic conditions of the heads. This specimen supplies further evidence that a common pathology underlies all of these conditions. A case figured by Schwalbe“ (Part III, p. 175, Fzg. 114) shows a fibroplastic exudate in connexion with cleft palate.
Dysplastic Lesions in Mice
Just before Dr. Streeter’s monograph appeared Dr. Halsey I. Bagg“ published an account of a breed of mice in which he had succeeded in producing dysplastic lesions of an hereditary nature. The mice, the subjects of his observation, were the progeny of normal mice which had been exposed to a series of brief doses of X rays, with the object of injuring their germ plasm. In the progeny of these mice appeared a proportion of descendants which suffered from the following lesions: small or absent eyes ; kidneys absent on one or both sides, in some cases polycystic ; dysplastic lesions of the feet. In about 80 per cent of cases of dysplasia of the feet there was no renal lesion; in 50 per cent there was no ocular lesions. It was not until he had inbred the dysplastic mice and had reached the eighth generation that Dr. Bagg began a systematic examination of the lesions of the limbs. He developed a technique which permitted him to expose the foetus in the uterus, to mark its condition, to close the uterus, and so note the progress from, say, the 13th day, when lesions began to appear, until birth on the 20th day. For example, 67 embryos were exposed in the uterus of the mother on the 13th day—-of these, 6 showed foot lesions in the earliest stage; 52 embryos were exposed on the I 5th day—of these, 6 showed defects; on the 17th day, 18 of 75 had foot defects. Of 5200 embryos born during the period of observation (5 years) 432 suffered from dysplasia of the feet—rather more than 8 per cent. By mating parents showing extreme degrees of dysplasia he obtained a much higher percentage of defectives : in one case 3 out of a litter of 4.
Fzg. II5 is a diagrammatized representation of an early stage in the development of a dysplastic lesion on the dorsum of the foot of a foetal mouse. The section was made by Dr. Bagg on a foetus which he removed from the mother on the I 5th day of her pregnancy, and which corresponds to the stage of development reached by the human foetus at the end of the 2nd month. A bleb has suddenly appeared in the subcutaneous tissue of the dorsum of the foot, the usual site, and contains a clear lymph, into which has just occurred an effusion of blood. The site of the effusion is seen at the base of the bleb (Fig. II 5, 3) where fibroblasts appear to be in a state of activity.
This bleb on the dorsum of the mouse’s foot is similar in all essential detail to that described by Dr. Ingalls in the occipital region of an early human foetus and illustrated in this article by Fig. 98.
Dr. Bagg attributes the formation of such a bleb “ to a localized arrest of development of part of the foetal foot . . . associated with a perivascular lymph stasis.” Now a localized arrest of development need not give rise to efiusion of lymph and blood; only a localized necrosis of foetal tissue could occasion such a train of events, and the most probable cause of necrosis is a localized failure in the circulation of blood.
Nowhere has Dr. Bagg recorded the state of the placenta in these dysplastic embryos, although placental lesions, were they present, would not likely escape his vigilant eye. When the circulation of a fmtus falls to the lowest ebb, as in a parasitic twin, large lymph cysts or hygromata form in its subcutaneous tissues. This is best seen in a twin foetus which has become dependent for blood-supply on the circulation of its host twin 13. The active agent which brings about this localized anaemia and necrosis in dysplasia faatalis still awaits discovery.
The stage reached a week later by the lesion shown in Fig. 115 is shown by another specimen illustrated in Fig. 116. The bleb is now replaced by a cap of dense necrotic tissue, made up of epidermis and haemorrhagic débris. Around the margin of the necrotic area the cutaneous epithelium is dipping inwards; in the
FIG. 1l6.—Section of the distal end of the foot of a moue, one day old, showing later sta e of a dysplastic lesion on the dorsal aspect. I, Epit elium ; 2.
FIG. ll5.—Longitudinal section.of the right hind foot of a foetal mouse, 14 days, showing an early stage of a dysplastic lesion. I. Fused hallux and 2nd toe;
2. Blood efi'used into bleb; 3. Site at which effusion has taken place; 4, Bleh formed in the subcutaneous tissue of the dorsum of the foot; 5. Skin and subcutan Remnant of distal phalanx with termination of cutaneous _epithelium;_ 3.1-hemorrhage ; 4. Necrotic tissue, includmg epithelium and red blood-cor uscles; 5. Fibrous
eous tissue; 6. Tibia ; 7, Os calcis; 8. Shaft of 3 meta tissue in state of reaction; 6, pithelium dipping tarsal; 9, Third toe. (After Bagg.)
inwards at edge of necrotic tissues. (After Bagg.)
base of the area, where there is a small haemorrhage, the fibrous tissue is actively proliferating towards the necrotic mass. Part of the distal end of the toe has become necrotic and been lost.
Now the lesion just described is similar in all respects to the dysplastic lesions of foot and digits described in the human foetus by Dr. Streeter. There is, however, one important difference 3 the profuse formation of fibrous (amniotic) bands is absent. This difference must be attributed to a time factor. After the onset of the lesion the mouse has only a week to spend in the amniotic fluid before birth occurs, whereas the human foetus is exposed to intra-uterine conditions for a period of 6 or 7 months. In mice, as in men, dysplastic lesions bring about intrauterine amputations, distortion of feet and hands, and union of digits.
Congenital Club Foot
The most common site of a dysplastic bleb in Dr. Bagg’s strain of mice was the dorsal surface of the feet—both fore and hind. The effect of such lesions is to produce clubbing of the feet. In 432 mice born with deformity of the limbs, clubbing was present in 306 of them. Now, the lesion being usually on the dorsal side of the foot, the cicatrization which follows brings about a dorsiflexion of the foot—the deformity in man known as talipes calcaneus. In the Royal College of Surgeons Teratological Collection, there is a full time human fetus (No. 434) with talipes calcaneus and necrotic areas on digits, showing the same lesions as in Dr. Bagg’s mice ; another example is figured by von Winckel? Amongst the 306 instances of club-foot amongst mice 291 were of the talipes calcaneus form, and only 9 showed plantar flexion with inversion of the foot—talipes equinus varus ; 6 others showed plantar flexion and distortion. Amongst human cases of club-foot the percentage of types of club-foot is reversed.
When one considers how different the human foot is from that of the mouse, and how far apart man and mouse are in the scale of evolution, a difference in the manifestations of the same disease need not astonish us. If a lesion of the nature described by Dr. Bagg were to form in the medial plantar aspect of the foot of an early human foetus between inner malleolus and 0s calcis, then the pathological manifestations—the cicatrical contraction of all the ligamentous structures attached to calcaneus, internal malleolus, and navicular tuberosity which we find in cases of club-foot in man—would be produced. I have no longer access to early foetal material in which the first manifestations of clubbing must appear, but I have no doubt that those who search will discover that what Dr. Bagg has found concerning the production of club-foot in mice is also true of club-foot in man. In brief, I am convinced that congenital club-foot in all its human forms is but one of the many ways in which Streeter’s dysplasia becomes manifest in our foetal bodies.
A high proportion of the dysplastic feet of mice shows division of a digitusually the hallux or pollex. This is also so in human families which suffer from a dysplastic taint. If division of a digit is a dysplastic manifestation, then we have to ascribe the onset of these disorders to the time at which digits make their first appearance—namely in the 6th week.
Summary
The object of this paper is to throw light on certain obscure congenital fissures and scars of the human face exemplified by two cases depicted in Figs. 84, 85. The conclusion reached is that these facial fissures are of the same nature as lesions described by Dr. George L. Streeter in the limbs of human foetuses—lesions attended by the formation of fibrous rings and bands (so-called amniotic adhesions) and intra-uterine local necroses and amputations. The author proposes to distinguish the disorder which underlies such manifestations as a distinct clinical entity under the provisional name of ‘ Streeter’s fcetal dysplasia ’ (dysplasia foetalis).
Further light on foetal dysplasia is thrown by two other embryological researches—one carried out in the laboratory of Prof. Florence Sabin by Miss Ellen Finley on the vascularization of the external coverings of the head; the other by Dr. N. W. Ingalls, who has described lesions along the mid-dorsal line of the human fcetus giving rise to certain cysts and scars which manifest dysplastic changes, often attended by the formation of ‘ amniotic adhesions ’. The 192 THE BRITISH JOURNAL OF SURGERY
author therefore regards congenital scars, and defects of the scalp, meningoceles (occipital and frontal), spina bifida, and the various degrees of anencephaly as manifestations of the same foetal dysplastic disorder.
The various forms of dysplastic lesions of the face are then examined and exemplified, and the conclusion is drawn that all such lesions are caused by a local necrosis probably due to a circulatory failure which may be placental in origin. The failure occurs along marginal areas where capillary formation is in progress. The lesions become manifest at two stages of human development: (1) Towards the end of the first month; (2) Towards the end of the second month.
‘ Amniotic adhesions ’ are never formed by a failure in the separation of the amnion from the embryo, but are always produced by and from the foetus—as a result of a dysplasia in foetal tissues. They are the result, not the cause, of foetal malformations. It would be well to substitute the name ‘ desmoplast ’ (tlecrmie, a bond) for amniotic adhesions and to give the name desmoplasia to the process of their formation.
Dr. H. J. Bagg has bred a strain of mice which are particularly liable to dysplastic lesions of the feet. Members of this dysplastic strain are the descendants of parents which were subjected to brief doses of X rays, with the result that the parent germ plasm was damaged—a damage which has been transmitted in their descendants as far as the nineteeth generation. Dysplasia in Dr. Bagg’s strain of mice —manifested by local necrosis, union of digits, and club-foot—has thus been made hereditary. The author is of opinion that the congenital lesions which Dr. Bagg observed in foetal mice are of the same nature as those which Dr. Streeter observed in the extremities of human foetuses. Although the matter requires further investigation, it seems highly probable that all forms of congenital club-foot in man are of dysplastic origin.
The author takes this opportunity of acknowledging the assistance given by the artist, Miss Barc1ay—Smith, who is responsible for the preparation of all the illustrations. Acknowledgements are also due to Dr. A. J. E. Cave and Mr. W. R. Le Fanu, of the Royal College of Surgeons of England.
References
KEITH, Sir A., Brit. Med. 3‘our., 1909, 2, 310, 363, 438.
2 VON WINCKEL, F., Sammlung klin. Vortrdge u. Volkmann ; neue Folge Gynr‘z'kol., 1904, No. I37.
3 EDINGTON, G. H., Glasgow Med. _70ur., 1909, 1|, 338; MORGAN, J. H., Proc. Roy. Med.-Chir. Soc., 1881, 9, 94; FRICKE, H. F., Beitr. z. Anat. Physiol. Pathol. :4. T herapi, 1:32, 30, 287 (6 cases). See also BALLAN'rYNE’s article in Teratologie, I895, , I .
4 Streeter GL. Focal deficiencies in foetal tissues and their relation to intrauterine amputation. (1930) Contrib. Embryol., Carnegie Inst. Wash. 22: 4.
5 FINLEY, ELLEN B., Ibz'd., 1922, I4, 155.
6 HARRIS, H. A., Bone Growth in Health and Disease, 1933.
7 INGALLS, N. W., Amer. four. Pathol., 1932, 8, 525 (on congenital defects which occur along the mid-dorsal line of the human body); Amer. four. Obst. and Gynecol., 1933, 25, 861 (on congenital defects of the scalp).
8 WOLFE, E., Arch. d’Anat., d’Histol. et d’Embryol., 1934, I8, I45, 231.
”DODDS and DE ANGELIS, Anat. Record, 1937, 67, 499.
‘° KEITH, Sir A., Brit. Med. _7our., 1921, 2, 137. (There I have described the process of embryological closure as akin to that of the healing of surgical wounds.)
1‘ SCHWALBE, E., Die Morphologie der Missbildungen des Menschen und der Tiere, 1913, Part III, 191 (Fig. 123).
12 BAGG, H. J., Amer. four. Anat., 1929, 43, 167.
13 KEITH, Sir A., “ The Anatomy and Nature of two Acardiac Foetuses ”, Tram. Obstet. Soc. Lond., 1900, 42, 99.
Cite this page: Hill, M.A. (2024, April 30) Embryology Paper - Concerning the origin and nature of certain malformations of the face, head, and foot. Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/Paper_-_Concerning_the_origin_and_nature_of_certain_malformations_of_the_face,_head,_and_foot
- © Dr Mark Hill 2024, UNSW Embryology ISBN: 978 0 7334 2609 4 - UNSW CRICOS Provider Code No. 00098G