BGDA Practical Placenta - Maternal Decidua
| Practical 14: Implantation and Early Placentation | Villi Development | Maternal Decidua | Cord Development | Placental Functions | Diagnostic Techniques | Abnormalities |
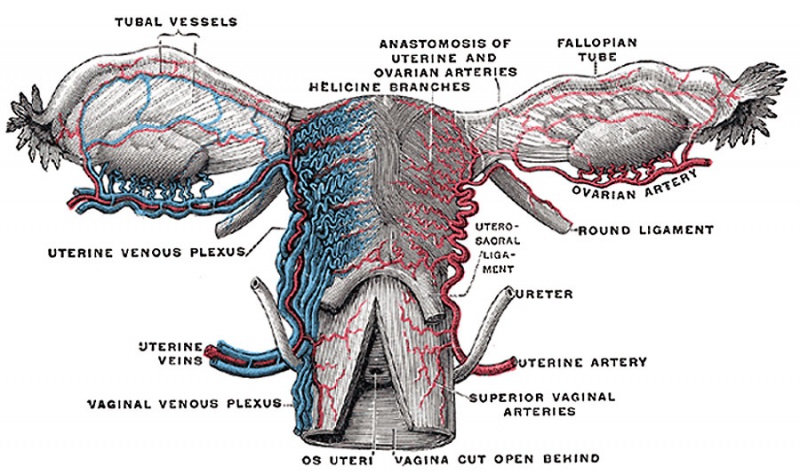
Uterus
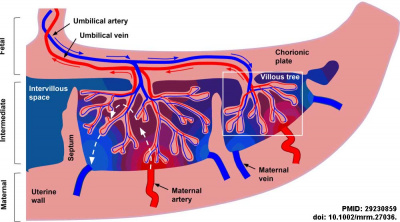
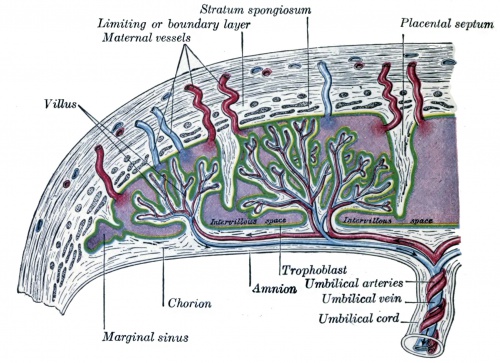
Human placenta classified as Haemochorial where the chorion comes in direct contact with maternal blood.
During pregnancy:
- maternal blood volume increases (from non-pregnant state) by about 50%.
- uterine blood flow increases 10 to 12 fold.
- Blood flow increase is due to the trophoblast cell invasion of the spiral arteries opening them into blood-filled spaces of the placenta.
Menstrual Changes
- Endometrium - 3 layers in secretory phase of menstrual cycle: compact, spongy, basal.
- Myometrium - muscular layer outside endometrium, contracts in parturition.
- Perimetrium - tunica serosa of the uterus continuous with the peritoneal wall.
Endometrial Layers
- Compact - implantation occurs in this layer, dense stromal cells, uterine gland necks, capillaries of spiral arteries.
- Spongy - swollen stromal cells, uterine gland bodies, spiral arteries.
- Basal - not lost during menstruation or childbirth, own blood supply.
Uterine glands
- still well-developed and highly active at 6 weeks (GA).
- gradually regress in length and epithelium height as the first trimester advances.
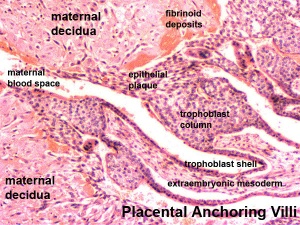
Decidual Reaction
Process (decidualization) of endometrial stromal cells (fibroblast-like) change in morphology (polygonal cells) and protein expression and secretion.
- occurs initially at site of implantation and includes both cellular and matrix changes
- reaction spreads throughout entire uterus, not at cervix
- deposition of fibrinoid and glycogen and epithelial plaque formation (at anchoring villi)
- presence of decidual cells are indicative of pregnancy
Fibrinoid layer - (Nitabuch's layer) is thought to act to prevent excessively deep implantation.
Artery Dilatation - due to extravillous trophoblast cells invading uterine wall and maternal spiral arteries replacing both smooth muscle with fibrinoid material and part of vessel endothelium. There is also a proliferation of maternal blood vessels.
Cervix - at mouth of uterus, secretes mucus (CMP), forms a plug/barrier, mechanical and antibacterial.
Decidua
The endometrium becomes the decidua and forms 3 distinct anatomical regions (at approx 3 weeks)
|
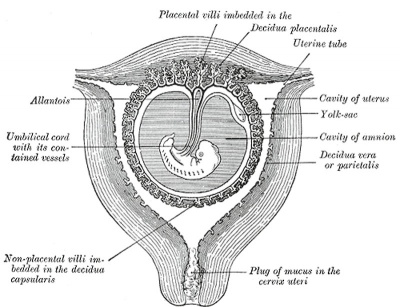
Historic drawing showing decidua parts |
Maternal Blood Flow
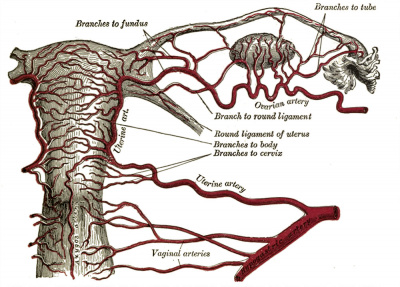
| Uterine Blood Supply | Uterine Arterial Distribution |
|---|---|
|
|
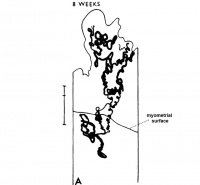
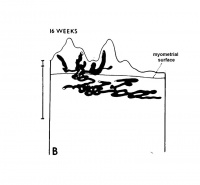
| Maternal Placental Artery Remodelling | ||||
|---|---|---|---|---|
|
|
|
|
|
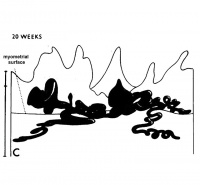
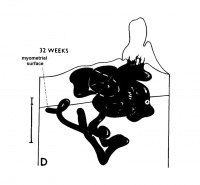
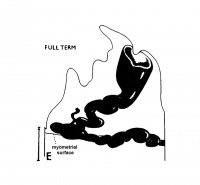
| GA 8 weeks | GA 16 weeks | GA 20 weeks | GA 32 weeks | term |
Maternal blood pressure normally decreases or remains unchanged during pregnancy while both cardiac output and vascular volume are increased. Uterine blood flow changes are principally due to a decrease in uterine vascular resistance. There is also an associated structural enlargement of both the uterine arterial and venous trees, reduced vascular tone (vasodilation) and placenta development.
Uteroplacental blood flow (UPBF) was historically measured by a number of different mathematical calculations and probe methods, currently the method involves transvaginal doppler ultrasonography.
In human singleton pregnancies, uteroplacental blood flow (UPBF) begins at 20–50 ml/min and increases (linearly) to 450–800 ml/min, with twin pregnancy values in excess of 1 l/min.[2]
Uterine Artery Diameter
The following data is from a study of 18 pregnant women using ultrasound and doppler analysis of the uterine artery.[3]
- GA week 21 doubled (from 1.4 to 2.8 mm).
- GA week 21 to 30 remained constant (2.9mm).
- GA week 30 to 36 increased (to 3.4 mm).
Uterine artery mean flow velocity also increased nearly eight times from non-pregnant (8.4 cm/second) to GA week 36 (61.4 cm/second).
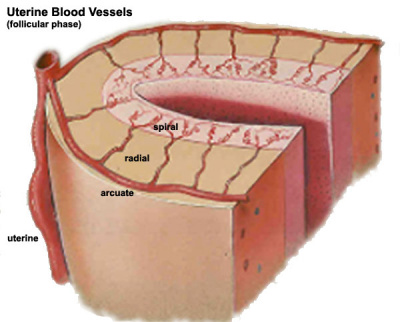
Arcuate and Radial Arteries
These branches from the paired uterine arteries also remodel enlarging in lumen diameter between 25 to 220% with either no change or an increase in wall thickness. Arcuate arteries also elongate either by longitudinal growth or by the progressive straightening of these coiled vessels.
- Links: ultrasound | cardiovascular
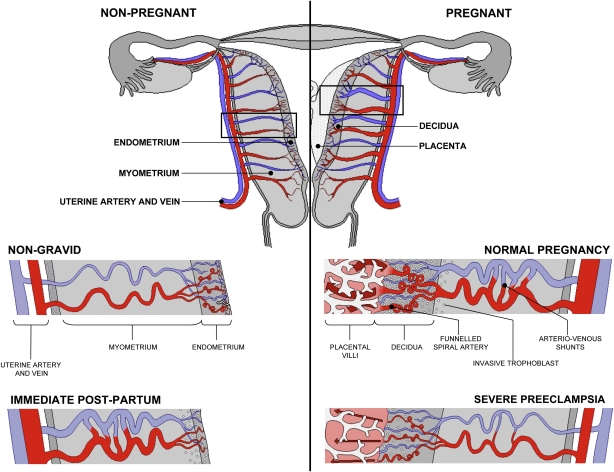
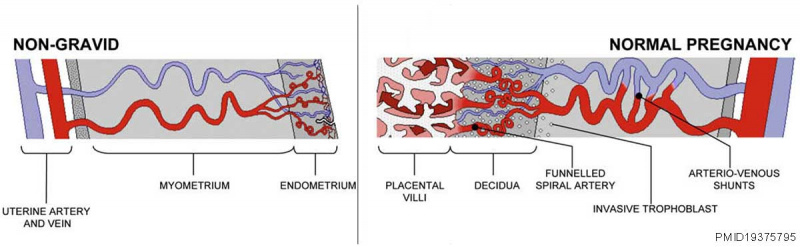
Uterine Vasculature - Non-pregnant, Pregnant and Immediate Post-partum
Diagrammatic representation of uterine and placental vasculature (red shading = arterial; blue shading = venous) in the non-pregnant, pregnant and immediate post-partum state.
- Normal pregnancy is characterized by the formation of large arteriovenous shunts (anastomoses) that persist in the immediate post-partum period.
- bypasses both the uterine capillary network and the intervillous space and regulate the pressure within the maternal blood-filled spaces.
- Extravillous cytotrophoblast invasion in normal pregnancy (diamonds) extends beyond the decidua into the inner myometrium resulting in the formation of funnels at the discharging tips of the spiral arteries.
- Pregnancies complicated by severe preeclampsia are characterized by minimal arterio-venous shunts, and thus narrower uterine arteries. Contrast with severe preeclampsia.
Maternal Decidua Interactive Component
| Attempt the Quiz - Maternal Decidua | ||
|---|---|---|

Here are a few simple Quiz questions that relate to Maternal Decidua from the practical.
|
| Practical 14: Implantation and Early Placentation | Villi Development | Maternal Decidua | Cord Development | Placental Functions | Diagnostic Techniques | Abnormalities |
Additional Information
| Additional Information - Content shown under this heading is not part of the material covered in this class. It is provided for those students who would like to know about some concepts or current research in topics related to the current class page. |
The maternal uterine endometrium stromal cells (fibroblast-like) are transformed by steroid hormones (progesterone) and embryonic signals into the decidua.
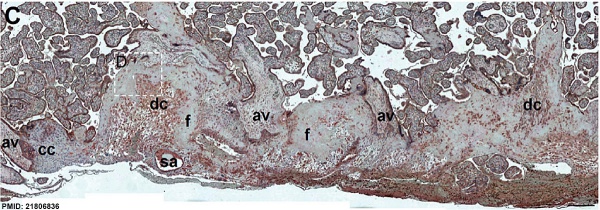
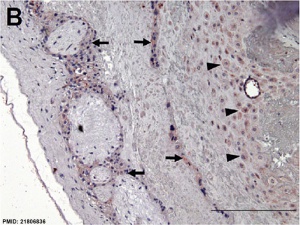
Immunostained placenta and decidua.[4]
SERPINE2 was extensively detected in decidual cells (dc), cytotrophoblasts, extravillous trophoblasts at the junction zone of the cell column (cc) and anchoring villi (av), and the endothelia of the spiral artery (sa); and weak staining was found in fibrinoids (f) and the villous mesenchyme.
Historic Drawings
Placental Classification
Classification of placenta is on the basis of histological (microscopic) structural organization and layers between fetal and maternal circulation.
Three main groups:
- Haemochorial - placenta where the chorion comes in direct contact with maternal blood (human).
- Endotheliochorial - maternal endometrial blood vessels are bare to their endothelium and these comes in contact with the chorion (dog, cat).
- Epitheliochorial - maternal epithelium of the uterus comes in contact with the chorion, considered as primitive (pig, cow).
The presence of these three differing types of placenta have also been used to describe the pattern mammalian evolution.
Fibrinoid
Exist as 2 forms of extracellular matrix:
- Fibrin-type fibrinoid is a maternal blood-clot product which replaces degenerative syncytiotrophoblast
- Matrix-type fibrinoid is secreted by invasive extravillous trophoblast cells.
Fibrinoid layer (Nitabuch's layer) is thought to act to prevent excessively deep implantation.
Decidualization
Process of endometrial stromal cells (fibroblast-like) change in morphology (polygonal cells) and protein expression and secretion (specific decidual proteins: prolactin, insulin-like growth factor binding protein-1, tissue factor, interleukin-15, and VEGF).
- Estrogen and progesterone - receptive phase, luminal and glandular epithelial cells change in preparation for blastocyst adplantation.
- Human Chorionic gonadotropin - luminal epithelium endoreplication leading to epithelial plaque formation.
- Human Chorionic gonadotropin - trophoblast invasion and decidualization of human stromal fibroblasts.
Pregnant Uterine Blood Flow
- arterial blood supplies the uterus and cervix (arteries, arterioles, capillary network, venules and vein).
- spiral arteries supplies the intervillous space (functionally like a large capillary network).
- arterial and venous shunts circulation (arteriovenous anastomoses), bypasses both the uterine capillary network and the intervillous space.
See Review[5]
Artery Dilatation
Due to extravillous trophoblast cells invading uterine wall and maternal spiral arteries replacing both smooth muscle with fibrinoid material and part of vessel endothelium. There is also a proliferation of maternal blood vessels.
Anastomoses
During normal pregnancy large anastomoses, arteriovenous "shunts", form that regulate both blood pressure and flow within the placenta. Shunts bypasses both the uterine capillary network and the intervillous space and regulate the pressure within the maternal blood-filled spaces. These shunts persist within the uterus in the initial birth period, and are smaller in severe preeclampsia.
Other Changes
- Endoreplication - rounds of nuclear DNA replication without intervening cell or nuclear division (mitosis).
- Cytokines - of maternal origin also act on placental development.
- Natural Killer (NK) cells
- 30% of all the decidual cells towards the end of the first trimester of pregnancy.
- Present in the maternal decidua in large numbers (70%, normal circulating blood lymphocytes 15%) close to the extravillous trophoblast cells.
- Normally have a cytolytic potential against virus-infected and tumor-transformed cells.
Preeclampsia
- Preeclampsia - describes maternal high blood pressure and protein in the urine after the 20th week (GA) late 2nd or 3rd trimester of pregnancy. This may be due to factors from the placenta.
- Eclampsia - seizures (convulsions) in a pregnant woman that are not related to a preexisting brain condition.
Terms
| Placenta Terms (expand to view) |
|---|
with an incidence of about 2.8 per 1,000 pregnancies, there is also a rarer form of extra-abdominal varices.PMID 24883288
with an incidence of about 2.8 per 1,000 pregnancies, there is also a rarer form of extra-abdominal varices. PMID 24883288
|
| Other Terms Lists |
|---|
| Terms Lists: ART | Birth | Bone | Cardiovascular | Cell Division | Endocrine | Gastrointestinal | Genital | Genetic | Head | Hearing | Heart | Immune | Integumentary | Neonatal | Neural | Oocyte | Palate | Placenta | Radiation | Renal | Respiratory | Spermatozoa | Statistics | Tooth | Ultrasound | Vision | Historic | Drugs | Glossary |
References
- ↑ Slator PJ, Hutter J, McCabe L, Gomes ADS, Price AN, Panagiotaki E, Rutherford MA, Hajnal JV & Alexander DC. (2018). Placenta microstructure and microcirculation imaging with diffusion MRI. Magn Reson Med , 80, 756-766. PMID: 29230859 DOI.
- ↑ Osol G & Mandala M. (2009). Maternal uterine vascular remodeling during pregnancy. Physiology (Bethesda) , 24, 58-71. PMID: 19196652 DOI.
- ↑ Palmer SK, Zamudio S, Coffin C, Parker S, Stamm E & Moore LG. (1992). Quantitative estimation of human uterine artery blood flow and pelvic blood flow redistribution in pregnancy. Obstet Gynecol , 80, 1000-6. PMID: 1448242
- ↑ 4.0 4.1 Chern SR, Li SH, Chiu CL, Chang HH, Chen CP & Tsuen Chen EI. (2011). Spatiotemporal expression of SERPINE2 in the human placenta and its role in extravillous trophoblast migration and invasion. Reprod. Biol. Endocrinol. , 9, 106. PMID: 21806836 DOI.
- ↑ Gyselaers W & Peeters L. (2013). Physiological implications of arteriovenous anastomoses and venous hemodynamic dysfunction in early gestational uterine circulation: a review. J. Matern. Fetal. Neonatal. Med. , 26, 841-6. PMID: 23339488 DOI.
| Practical 14: Implantation and Early Placentation | Villi Development | Maternal Decidua | Cord Development | Placental Functions | Diagnostic Techniques | Abnormalities |