BGDA Practical 12 - Third Trimester
| Practical 12: Embryo to Fetus | Second Trimester | Third Trimester | Birth | Neonatal | Abnormalities |
Introduction
Identify changes in fetal size and the systems that have ongoing developmental features during the third trimester.
- Weight
- Ossification
- Respiratory
- Genital
- Neural
- Cardiovascular
- Renal
- Growth - Fetal Growth Restriction, Developmental Origins of Health and Disease
- Survival issues for early delivery
Week 24+
- Earliest potential survival expected if born.
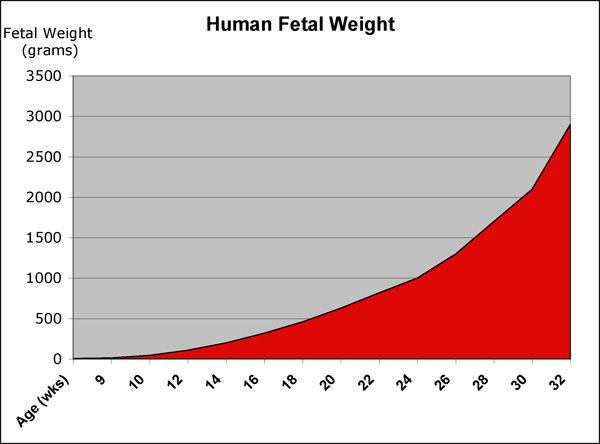
- Most of the serious illness and mortality is concentrated in the 1 to 2 percent of infants who are born at less than GA 32 weeks (week 30) and who weigh less than 1500 g.
Class Models
Observe the differences between the fetus and uterus at the end of the second trimester and at term.
- size and weight
- head and limb proportions
Fetal Weight
Ossification
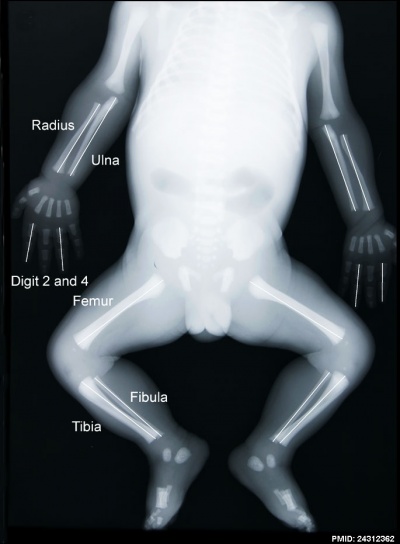
|
Fetal skeleton x-ray
Ossification that commenced towards the end of the embryonic period, continues through the second and third trimester. When does the skeleton complete its ossification?
Note:
|
Endocrine
During the third trimester fetal endocrine organs are differentiated and secreting fetal hormones.
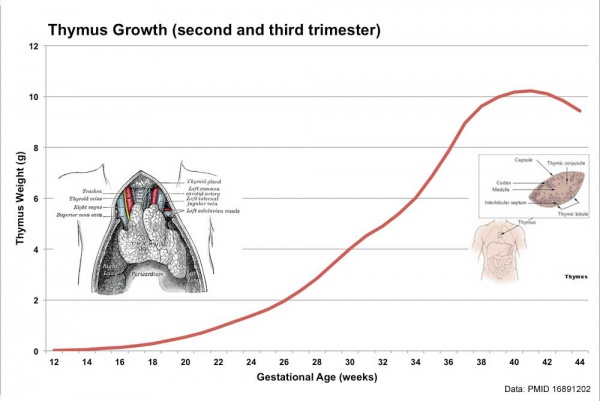
Endocrine - Fetal thymus weight growth
Respiratory
Week 24 to 40 lung histology - terminal sac, end month 6 alveolar cells type 2 appear and begin to secrete surfactant
|
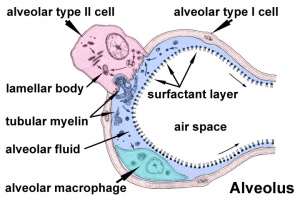
|
Genital
|
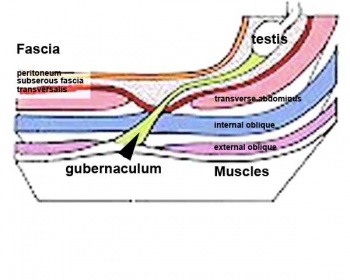
Testes DescentThe linked animation shows the descent of the testes (between week 7 to 38, birth). Descent of the testes into the scrotal sac begins generally during week 26 and may take several days.
Incomplete or failed descent can occur unilaterally or bilaterally, is more common in premature births, and can be completed postnatally. (see also cryptorchidism). |
|
|
| Start of testis descent | End of testis descent |
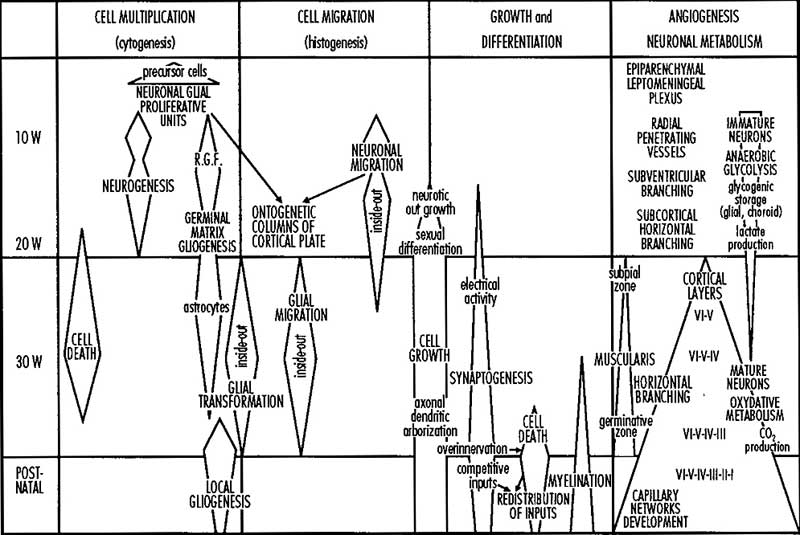
Neural
|
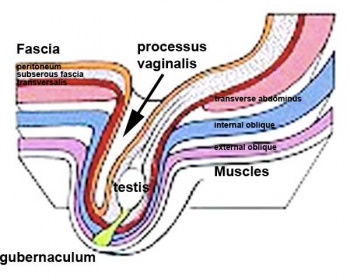
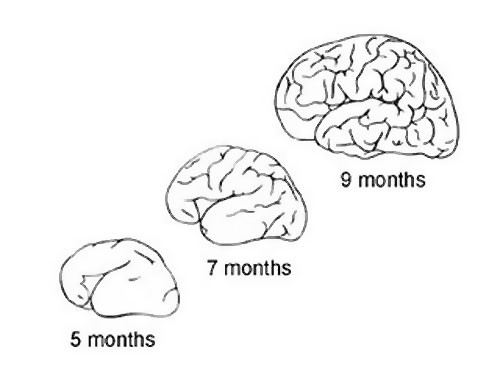
Comparison of brain growth through the third trimester.
|
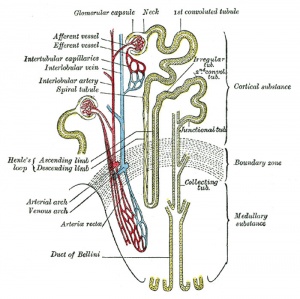
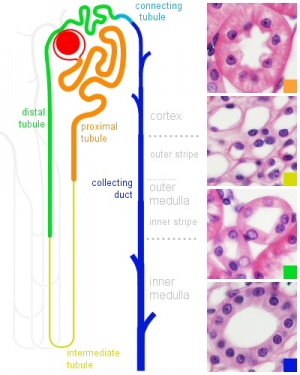
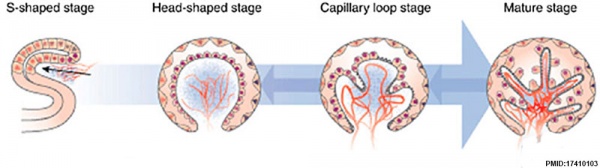
Renal
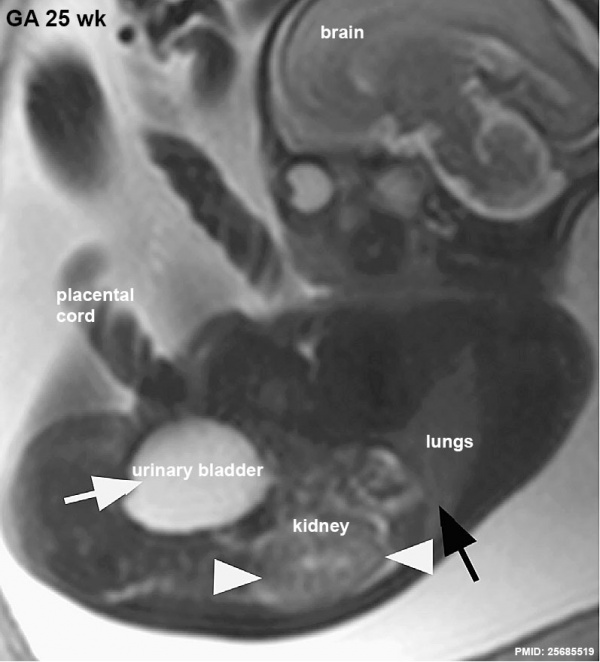
The functional unit of the kidney is the nephron and the process of their initial formation is called nephrogenesis. During development nephron number increases from about 15,000 at 15 weeks (GA 17 weeks) increasing to about the adult number by 36 weeks. Each adult kidney typically contains about 750,000 nephrons, though the total number can vary significantly from as few as 250,000 to as many as 2,000,000.
MRI appearance of normal fetal kidneys.(GA 25)
In humans, nephrogenesis only occurs before birth, though nephron maturation continues postnatally.
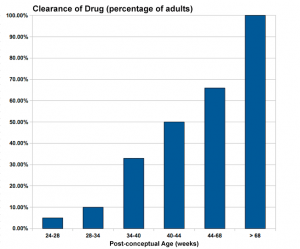
Infant Drug Clearance
|
||||||||||||||||||
Teratogen (Greek, teraton = monster) Any agent that causes a structural abnormality following exposure during pregnancy. The overall effect depends on dosage and time of exposure.
Fetal Growth
Fetal Growth Restriction
The term "Fetal Growth Restriction" (FGR) or intrauterine growth restriction (IUGR) are used to describe when the fetus does not reach full growth potential. This is usually determined by clinical sonography calculations of fetal weight, fetal size, or symmetry.
Developmental Origins of Health and Disease (DOHaD)
Environmental derived abnormalities relate to maternal lifestyle, environment and nutrition and while some of these directly effect embryonic development, there is also growing evidence that some effects are more subtle and relate to later life health events. This theory, now called "developmental origins of health and disease" (DOHAD or DOHaD) and also previously Fetal Origins Hypothesis, is based on the early statistical analysis carried out by David Barker (1938 - 2013) of low birth weight data collected in the early 1900's in the south east of England which he then compared with these same babies later health outcomes. The theory was therefore originally called the "Barker Hypothesis" and has recently been renamed as "fetal origins" or "programming". Several origins have been suggested including: fetal undernutrition, endocrine (increased cortisol exposure), genetic susceptibility and accelerated postnatal growth.
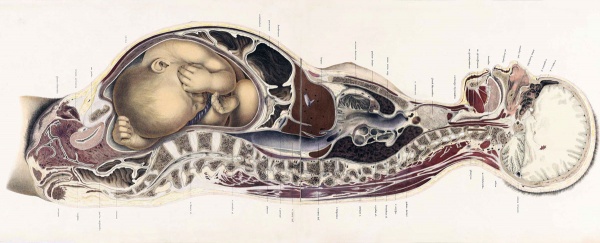
Maternal Anatomy
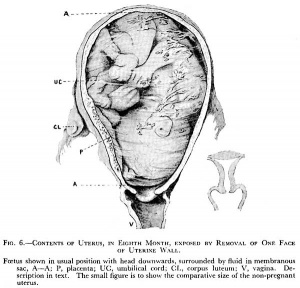
There are many maternal physiological changes during and after pregnancy. This section introduces just the anatomical changes that must occur to simply accomodate the growing fetus in the second and third trimester. Watch the 2017 animation and observe the historic gross anatomy section.
<html5media width="600" height="400">https://www.youtube.com/embed/yE-l1stWkT4</html5media>
The Position of the Uterus and Fetus at Term (1872).[1]
Third Trimester Interactive Component
| Attempt the Quiz - Third Trimester | ||
|---|---|---|

Here are a few simple Quiz questions that relate to Third Trimester development from the practical.
|
| Practical 12: Embryo to Fetus | Second Trimester | Third Trimester | Birth | Neonatal | Abnormalities |
Additional Information
| Additional Information - Content shown under this heading is not part of the material covered in this class. It is provided for those students who would like to know about some concepts or current research in topics related to the current class page. |
- Links: third trimester
Bone Timeline
bone timeline the linked page shows details of individual bones completion of ossification. You do not need to know the detailed timeline of skeletal ossification for this class.
Postnatal Abnormality
Features include:
- Instability: 1:60 at birth; 1:240 at 1 wk: Dislocation untreated; 1:700
- congenital instability of hip, later dislocates by muscle pulls or gravity
- familial predisposition female predominance
- Growth of femoral head, acetabulum and innominate bone are delayed until the femoral head fits firmly into the acetabulum
Vitamin D[2]
- Role in bone development, growth, and the maturation of tissues (lung and brain).
- Fetus is dependent on the mother in terms of Vitamin D
- Maternal Vitamin D deficiency results in a Vitamin D deficient newborn.
Abnormal Neural
Quantitative Folding Pattern Analysis of Early Primary Sulci in Human Fetuses with Brain Abnormalities[3]
- "Aberrant gyral folding is a key feature in the diagnosis of many cerebral malformations. However, in fetal life, it is particularly challenging to confidently diagnose aberrant folding because of the rapid spatiotemporal changes of gyral development. Currently, there is no resource to measure how an individual fetal brain compares with normal spatiotemporal variations. In this study, we assessed the potential for automatic analysis of early sulcal patterns to detect individual fetal brains with cerebral abnormalities. ... Automated analysis of interrelated patterning of early primary sulci could outperform the traditional gyrification index and has the potential to quantitatively detect individual fetuses with emerging abnormal sulcal patterns."
- Gyrification index - a metric that quantifies the amount of cortex buried within the sulcal folds as compared with the amount of cortex on the outer visible cortex.[4] (More? Watch the JoVE Video)
Third Trimester
(Clinical Week 28)
| Links: human timeline | first trimester timeline | second trimester timeline | third trimester timeline | ||
| Event | ||
| Clinical third trimester |  hearing 3rd Trimester - vibration acoustically of maternal abdominal wall induces startle respone in fetus. hearing 3rd Trimester - vibration acoustically of maternal abdominal wall induces startle respone in fetus.
| |
| respiratory Month 7 - respiratory bronchioles proliferate and end in alveolar ducts and sacs | ||
|
tooth Week 29 - Permanent premolars (correspond to the milk molars) appear. | ||
|
Genital male gonad (testes) descending | ||
| nail fingernails reach digit tip | ||
| neural brain cortical sulcation - primary sulci present[5] | ||
| neural brain cortical sulcation - insular, cingular, and occipital secondary sulci present[5] | ||
 Nail Development toenails reach digit tip Nail Development toenails reach digit tip
Lens Development - lens growth and interocular distance plateaus after 36 weeks of gestation[6] | ||
| Birth |  Clinical Week 40 Clinical Week 40
Heart pressure difference closes foramen ovale leaving a fossa ovalis thyroid TSH levels increase, thyroxine (T3) and T4 levels increase to 24 h, then 5-7 days postnatal decline to normal levels adrenal - zona glomerulosa, zona fasiculata present | |
References
- ↑ Braune W. An atlas of topographical anatomy after plane sections of frozen bodies. (1877) Trans. by Edward Bellamy. Philadelphia: Lindsay and Blakiston.
- ↑ Yılmaz B, Aygün C & Çetinoğlu E. (2018). Vitamin D levels in newborns and association with neonatal hypocalcemia. J. Matern. Fetal. Neonatal. Med. , 31, 1889-1893. PMID: 28610460 DOI.
- ↑ Im K, Guimaraes A, Kim Y, Cottrill E, Gagoski B, Rollins C, Ortinau C, Yang E & Grant PE. (2017). Quantitative Folding Pattern Analysis of Early Primary Sulci in Human Fetuses with Brain Abnormalities. AJNR Am J Neuroradiol , 38, 1449-1455. PMID: 28522661 DOI.
- ↑ Schaer M, Cuadra MB, Schmansky N, Fischl B, Thiran JP & Eliez S. (2012). How to measure cortical folding from MR images: a step-by-step tutorial to compute local gyrification index. J Vis Exp , , e3417. PMID: 22230945 DOI.
- ↑ 5.0 5.1 Garel C, Chantrel E, Brisse H, Elmaleh M, Luton D, Oury JF, Sebag G & Hassan M. (2001). Fetal cerebral cortex: normal gestational landmarks identified using prenatal MR imaging. AJNR Am J Neuroradiol , 22, 184-9. PMID: 11158907
- ↑ Paquette LB, Jackson HA, Tavaré CJ, Miller DA & Panigrahy A. (2009). In utero eye development documented by fetal MR imaging. AJNR Am J Neuroradiol , 30, 1787-91. PMID: 19541779 DOI.
BGDA: Lecture 1 | Lecture 2 | Practical 3 | Practical 6 | Practical 12 | Lecture Neural | Practical 14 | Histology Support - Female | Male | Tutorial
Glossary Links
- Glossary: A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | Numbers | Symbols | Term Link
Cite this page: Hill, M.A. (2024, April 28) Embryology BGDA Practical 12 - Third Trimester. Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/BGDA_Practical_12_-_Third_Trimester
- © Dr Mark Hill 2024, UNSW Embryology ISBN: 978 0 7334 2609 4 - UNSW CRICOS Provider Code No. 00098G