ANAT2341 Lab 4 - Abnormal Placenta
| ANAT2341 Lab 4: Introduction | Implantation and Villi | Decidua and Cord | Abnormal Placenta | Cardiovascular | Online Assessment | Group Project |
Diagnostic Techniques
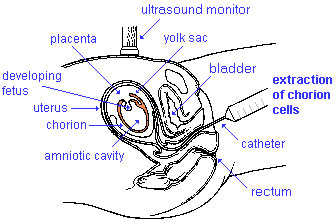
Chorionic Villus Sampling
|
Chorionic Villus Sampling test is done in the 10th to 12th week after the first day of the mother's last menstrual period. The test is done by looking at cells taken from the chorionic membrane or placenta. No anaesthetic is required, and a test result is usually available in two to three weeks.
When the test is carried out by an obstetrician experienced in the technique, the risk of miscarriage related to the test is about 2%. Potential disadvantages include maternal cell contamination, placental mosaicism and failure to obtain an adequate specimen. This may result in the need for a repeat procedure or amniocentesis.
|
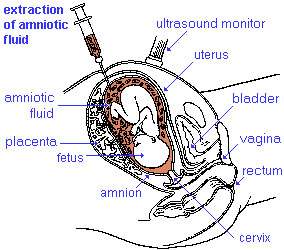
Amniocentesis
|
Amniocentesis is a prenatal diagnostic test carried out mainly between 14th to 18th week of pregnancy. Amniotic fluid is taken from the uterus, sent to a diagnostic laboratory and embryonic cells isolated from the amniotic fluid. No anaesthetic is required, and a result is usually obtained in about three to four weeks. When the test is carried out by an obstetrician experienced in the technique, the risk of a miscarriage related to the test is about 1 %.
|
What does a DNA Sequencer look like?
Ultrasound
Placenta - position, size and structure.
|
| Ultrasound 12wk |
| Page | Play |
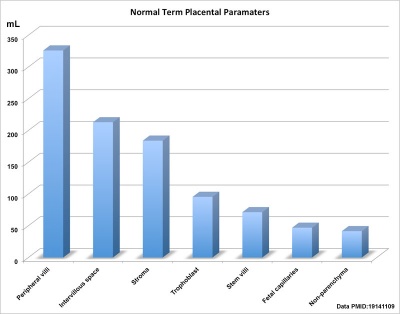
Placenta Term Parameters
There are a variety of diagnostic and morphological measurements that can be made of the placenta during pregnancy and at term.
Simple measurements of overall placental diameter, thickness and volume:
- placental diameter - is measured in the transverse section by calculating the maximum dimensions of the chorionic surface.
- placental thickness - is measured at its mid-portion from the chorionic plate to the basilar plate, on a longitudinal plane (less than 4 cm at term). Excludes any abnormalities (fibroids, myometrial contractions, or venous lakes). The placental thickness approximates in millimeters to the weeks of gestation.
- placental volume - is measured by a range of different methods and calculations, more recently with three-dimensional ultrasound.
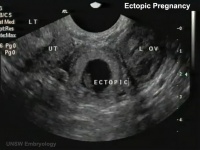
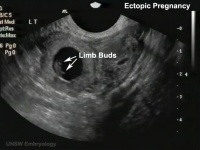
Ectopic Implantation
Ectopic pregnancy is also a high-risk maternal medical condition with an approximate incidence of 1.5 to 2 % in reported pregnancies. There is some indication that the incidence may be increasing (United States has increased from 4.5 per 1,000 pregnancies in 1970 to an estimated 19.7 per 1,000 pregnancies in 1992[1]). In Australia, the incidence of ectopic pregnancy was 17.4 per 1000 births in 1990 and 16.2 per 1000 in 1998.
| Tubal Ectopic | Bicornuate Uterus Ectopic | ||||||
|---|---|---|---|---|---|---|---|
|
|
|

|
|

|
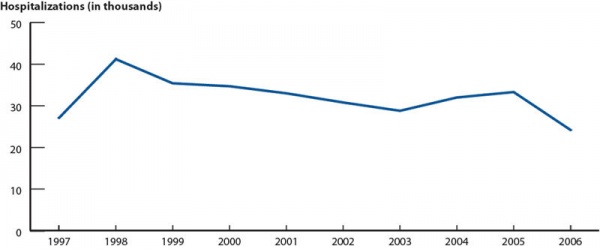
USA Ectopic Pregnancies (1997-2006)
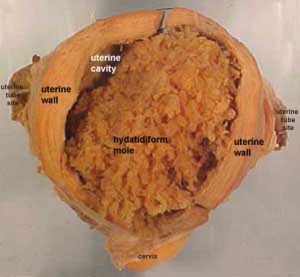
Genetic - Hydatidiform Mole
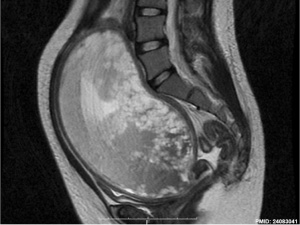
Another type of abnormality is when only the conceptus trophoblast layers proliferates and not the embryoblast, no embryo develops, this is called a "hydatidiform mole" (HM), which is due to the continuing presence of the trophoblastic layer, this abnormal conceptus can also implant in the uterus. The trophoblast cells will secrete human chorionic gonadotropin (hCG), as in a normal pregnancy, and may appear maternally and by pregnancy test to be "normal". Prenatal diagnosis by ultrasound analysis demonstrates the absence of a embryo.
There are several forms of hydatidiform mole: partial mole, complete mole and persistent gestational trophoblastic tumor.
- Complete Mole - Only paternal chromosomes, chromosomal genetic material from the ovum (egg) is lost, by an unknown process.
- Partial Mole - Ultrasound of partial mole confirmed by triploidy, chromosomal (genetic) material from the ovum (egg) is retained and the egg is fertilized by one or two sperm.
On ultrasound the tumour has a "grape-like" placental appearance without enclosed embryo formation. Following a first molar pregnancy, there is approximately a 1% risk of a second molar pregnancy.
- The incidence of hydatidiform mole varies between ethnic groups, and typically occurs in 1 in every 1500 pregnancies.
- All hydatidiform mole cases are sporadic, except for extremely rare familial cases.
- Links: Hydatidiform Mole | Week 2 - Abnormalities
Uterine Implantation Abnormalities
The placenta is a mateno-fetal organ which begins developing at implantation of the blastocyst and is delivered with the fetus at birth. As the fetus relies on the placenta for not only nutrition, but many other developmentally essential functions, the correct development of the placenta is important to correct embryonic and fetal development.
In addition to the above genetic abnormalities, there can be anatomical, associated with degree or site of inplantation, structure (as with twinning), to placental function, placento-maternal effects (pre-eclampsia, fetal erythroblastosis) and finally mechanical abnormalities associated with the placental (umbilical) cord.
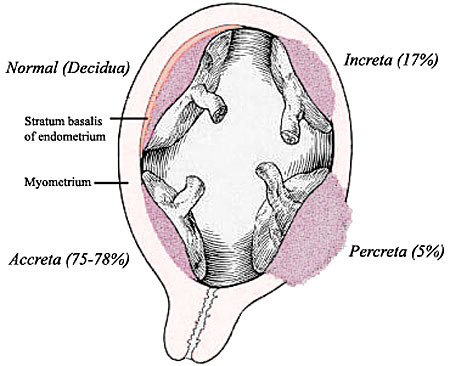
- Placenta Accreta - abnormal adherence, with absence of decidua basalis. The incidence of placenta accreta also significantly increases in women with previous cesarean section compared to those without a prior surgical delivery.
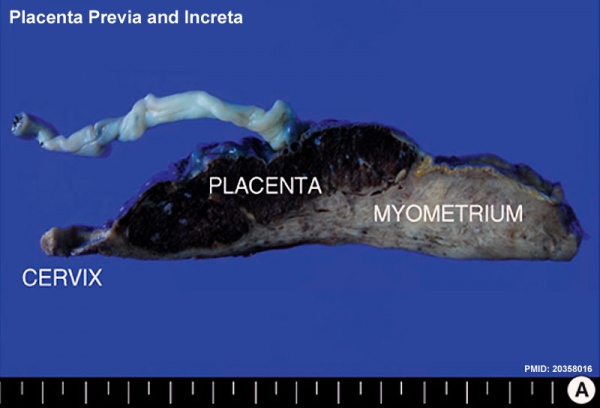
- Placenta Increta - occurs when the placenta attaches deep into the uterine wall and penetrates into the uterine muscle, but does not penetrate the uterine serosa. Placenta increta accounts for approximately 15-17% of all cases.
- Placenta Percreta - placental villi penetrate myometrium and through to uterine serosa.
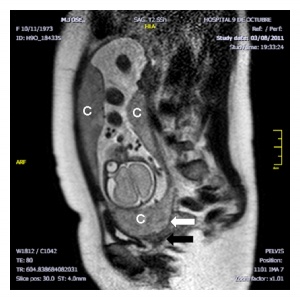
- Placenta Previa - In this placenatal abnormality, the placenta overlies internal os of uterus, essentially covering the birth canal. This condition occurs in approximately 1 in 200 to 250 pregnancies. In the third trimester and at term, abnormal bleeding can require cesarian delivery and can also lead to Abruptio Placenta. Ultrasound screening programs during 1st and early 2nd trimester pregnancies now include placental localization. Diagnosis can also be made by transvaginal ultrasound.
- Vasa Previa - (vasa praevia) placental abnormality where the fetal vessels lie within the membranes close too or crossing the inner cervical os (opening). Two main associations; 1. velamentous insertions (25–62%) and 2. vessels crossing between lobes in succenturiate or bilobate placentas (33–75%)
- Multilobed Placenta Succenturiata - an accessory portion attached to the main placenta by an artery or vein.
- Abruptio Placenta - a retroplacental blood clot formation, abnormal haemorrhage prior to delivery.
- Chronic Intervillositis - (massive chronicintervillositis, chronic histiocytic intervillositis) Rare placental abnormality and pathology defined by inflammatory placental lesions, mainly in the intervillous space (IVS), with a maternal infiltrate of mononuclear cells (monocytes, lymphocytes, histiocytes) and intervillous fibrinoid deposition.
Circumvallate Placenta
|
Circumvallate placenta is an abnormally shaped placenta where the chorionic membranes are not inserted at the edge of the placenta, but are located inward from the margins toward the placental cord. The membranes are described as "doubled back" over the fetal surface of the placenta. |
Cord Abnormalities
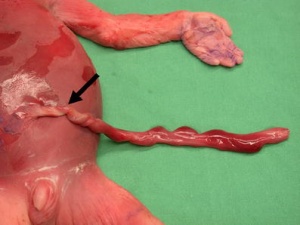
Velamentous Cord Insertion of the Placenta
The placental cord inserts into the chorion laeve (placental membranes) away from the edge of the placenta. The placental vessels are therefore unprotected by Wharton's jelly where they traverse the membranes before they come together into the umbilical cord.
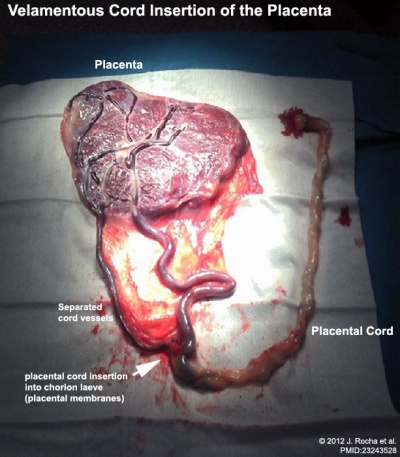
|

|
| Placenta velamentous cord | Bilobed placenta with velamentous cord |
This can also be associated with vasa previa (see above) or haemorrhage caused if the vessels are damaged when the membranes are ruptured prior to birth. The condition is more common in monozygotic twins (15%) and triplets.
Cord Length
Excessively short or long cords (see additional information on cord page). Abnormally long cords may wrap around either extremities or neck of the fetus.
Cord Vessel Number
Cord with only one artery and one vein.
Cord Knotting
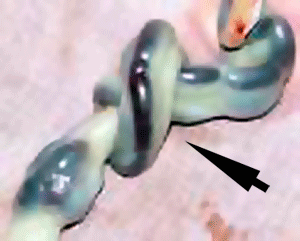
Cord knotting can occur (1%) in most cases these knots have no effect, in some cases of severe knotting this can prevents the passage of placental blood.
Umbilical cord torsion
Rare umbilical cord torsion, even without knot formation can also affect placental blood flow, even leading to fetal demise.
- ↑ <pubmed>7823895</pubmed>
| ANAT2341 Lab 4: Introduction | Implantation and Villi | Decidua and Cord | Abnormal Placenta | Cardiovascular | Online Assessment | Group Project |
| ANAT2341 Course Timetable | |||
|---|---|---|---|
| Week (Mon) | Lecture 1 (Mon 1-2pm) | Lecture 2 (Tue 3-4pm) | Practical (Fri 1-3pm) |
| Week 2 (1 Aug) | Introduction | Fertilization | Lab 1 |
| Week 3 (8 Aug) | Week 1 and 2 | Week 3 | Lab 2 |
| Week 4 (15 Aug) | Mesoderm | Ectoderm | Lab 3 |
| Week 5 (22 Aug) | Early Vascular | Placenta | Lab 4 |
| Week 6 (29 Aug) | Gastrointestinal | Respiratory | Lab 5 |
| Week 7 (5 Sep) | Head | Neural Crest | Lab 6 |
| Week 8 (12 Sep) | Musculoskeletal | Limb Development | Lab 7 |
| Week 9 (19 Sep) | Renal | Genital | Lab 8 |
| Mid-semester break | |||
| Week 10 (3 Oct) | Public Holiday | Stem Cells | Lab 9 |
| Week 11 (10 Oct) | Integumentary | Endocrine | Lab 10 |
| Week 12 (17 Oct) | Heart | Sensory | Lab 11 |
| Week 13 (24 Oct) | Fetal | Birth and Revision | Lab 12 |
|
ANAT2341 2016: Moodle page | ECHO360 | Textbooks | Students 2016 | Projects 2016 | |||