Birth: Difference between revisions
| Line 19: | Line 19: | ||
:"...one should count back 3 months from the first day of the last menses, then add 15 days for primiparas or 10 days for multiparas, instead of using the common algorithm for Naegele's rule."<ref><pubmed>2342739</pubmed></ref> | :"...one should count back 3 months from the first day of the last menses, then add 15 days for primiparas or 10 days for multiparas, instead of using the common algorithm for Naegele's rule."<ref><pubmed>2342739</pubmed></ref> | ||
==USA Live Births and Fertility Rates== | ==Birth Statistics== | ||
===USA Live Births and Fertility Rates=== | |||
2007 Data <ref>USA National Vital Statistics System - [http://www.cdc.gov/nchs/births.htm Birth Data]</ref> | 2007 Data <ref>USA National Vital Statistics System - [http://www.cdc.gov/nchs/births.htm Birth Data]</ref> | ||
Number of births: 4,317,119 | Number of births: 4,317,119 | ||
Revision as of 08:57, 14 June 2010
Introduction
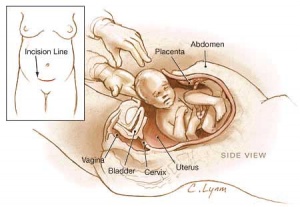
Birth or parturition is a critical stage in development, representing in mammals a transition from direct maternal support of fetal development, physical expulsion and establishment of the newborns own respiratory, circulatory and digestive systems. These notes only cover the biological processes surrounding birth including fetal signaling changes and maternal signaling changes. Note that there is a growing worldwide trend in developed countries toward caesarean section delivery. There are a great number of comprehensive, scientific and general, books and articles that cover birth, childbirth or parturition. The time surrounding birth is known as the perinatal period.
- --Mark Hill 09:00, 6 August 2009 (EST) Page under development - notice removed when completed.
| Apgar test | Guthrie test | Neonatal Development
Textbooks
- Human Embryology (2nd ed.) Larson Chapter 15 pp471-488
- The Developing Human: Clinically Oriented Embryology (6th ed.) Moore and Persaud Chapter 7 pp129-167
Gestation Period
Historically, Franz Carl Naegele (1777-1851) developed the first scientific rule for estimating length of a pregnany. The median duration of gestation for first births from assumed ovulation to delivery was 274 days (just over 39 weeks). For multiple births, the median duration of pregnancy was 269 days (38.4 weeks).
- "...one should count back 3 months from the first day of the last menses, then add 15 days for primiparas or 10 days for multiparas, instead of using the common algorithm for Naegele's rule."[1]
Birth Statistics
USA Live Births and Fertility Rates
2007 Data [2] Number of births: 4,317,119 Birth rate: 14.3 per 1,000 population Fertility rate: 69.5 births per 1000 women aged 15-44 years Percent born low birthweight: 8.2% Percent unmarried: 39.7%
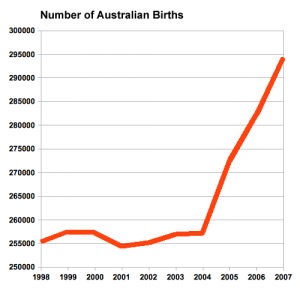
Australian Data
Childbirth
- Parturition (Latin, parturitio = "childbirth") describes expelling the fetus, placenta and fetal membranes and is probably initiated by fetus not mother.
- Preterm birth - Risks of preterm birth in abnormal low birth weight (intrauterine growth restriction) and high (large for gestational age) categories are 2- to 3-fold greater than the risk among appropriate-for-gestational-age infants.
- Maternal labor - uterine contractions and dilation of cervix, process under endocrine regulation
- Placenta and fetal membranes - (Latin, secundina = "following") expelled after neonate birth
Uterine Myometrial Changes
- Smooth muscle fibers - hypertrophy not proliferation
- Stretching of myometrium - stimulates spontaneous muscular contraction, during pregnancy progesterone inhibits contraction
- Stimulating contraction - increased estrogen levels (placental secretion sensitizes smooth muscle), increased oxytocin levels (fetal oxytocin release- force and frequency of contraction), fetal pituitary prostaglandin production (estrogen and oxytocin stimulate endometrial production of prostaglandin)
Progesterone
- maintains pregnancy - initially synthesized by corpus luteum, then levels maintained by placenta
- hyperpolarizes myometrial cells (-65 mV), reduces excitability and conductivity
- Level in plasma may fall just before parturition, definitely decreases following delivery of placenta
Estrogens
- Group of steroidal hormones, peak when parturition begins
- induce increased synthesis of actomyosin and ATP in myometrial cells
- alter membrane potential (-50 Mv) enhances excitation/conduction
- act to directly increase myometrial contraction
- indirectly by increasing oxytocin from pituitary gland
- Estriol - synthesized by fetus and placenta
Oxytocin
- Peptide hormone (8aa) from maternal posterior pituitary, initiation and maintenance of labour (synthetic form labour induction)
- myometrium sensitivity to oxytocin (increased by estrogen, decreased by progesterone)
- stimulus for release - mechanical stimulation of uterus, cervix and vagina (ethanol inhibits release)
Prostaglandins
- hydroxy fatty acids - sythesized by placenta, amniotic fliud contains mainly PGF2 alpha, causes myometrial contraction (also in maternal plasma)
- PGF2 alpha and PGE2 - used to induce labour (intravenous, oral, intravaginal, intraamniotic)
- Aspirin inhibitor of PG synthesis - leads to increased duration of pregnancy
External Environment
- mainly shown in other species parturition occurs in peaceful undisturbed surroundings, stress may have an inhibitory effect on oxytocin release
- Most human births occur at night (peak at 3am) diurnal rhythm influence
Labor Stages
Stage 1 - dilatation
- uterine contractions 10 minutes apart, function to dilate cervix fetal membranes rupture releasing amnion, 7 -12 hours (longer for first child)
Stage 2 - expulsion
- uterine contractions push fetus through cervix and vagina, contractions 2-3 minutes apart, 20 - 50 minutes
Stage 3 - placental
- following child delivery contractions continue to expel placenta. haematoma separates placenta from uterine wall, separation occurs at spongy layer of decidua basalis, 15 minutes
Stage 4 - recovery
- continued myometrial contraction closes spiral arteries, 2+ hours
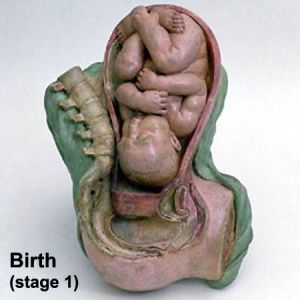
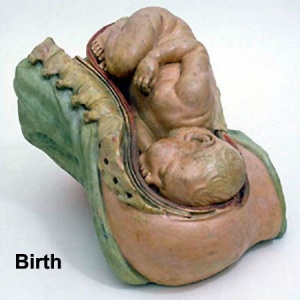
Historic Birth Models
About The Models - a series of models commissioned by Giuseppe Galletti (? - 1819) currently held in the Institute and Museum of the History of Science (Italy) Istituto e Museo di Storia della Scienza (IMSS). Giuseppe Galletti and others used terracotta and wax models that he had commissioned in Florence between 1770 and 1775 to train surgeons and midwives.
About The Models - One of a series of models commissioned by Giuseppe Galletti (? - 1819) currently held in the Institute and Museum of the History of Science (Italy) Istituto e Museo di Storia della Scienza (IMSS). Giuseppe Galletti and others used terracotta and wax models that he had commissioned in Florence between 1770 and 1775 to train surgeons and midwives. Wax models are life-sized and the terracotta versions are reduced to a 1:3 scale.
- Galletti models: birth | Week 10 Fetus Model | Week 16 Fetus Model | Week 24 Fetus Model | Stage 1 Terracotta Model 1 | Stage 2 Terracotta Model 2 | Stage 1 Wax Model | Breech Birth 1 | Breech Birth 2 | Breech Birth 3 | Breech Birth Wax Model | Placenta Previa | Category:Galletti1770 | 17th and 18th Century Anatomies | Embryology History | Embryology Models
Image Source: Institute and Museum of the History of Science http://brunelleschi.imss.fi.it/museum/esim.asp?c=500156 Thanks to Sabina Bernacchini from Institute and Museum of the History of Science (Italy) IMSS for allowing reproduction of selected images from the Surgery and Obstetrics exhibition on this embryology education site.
Cite this page: Hill, M.A. (2024, May 8) Embryology Birth. Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/Birth
- © Dr Mark Hill 2024, UNSW Embryology ISBN: 978 0 7334 2609 4 - UNSW CRICOS Provider Code No. 00098G
Additional Images
See Category:Birth
Birth Weights
| Birth weight (grams) | less 500 | 500 – 999 | 1,000 – 1,499 | 1,500 – 1,999 | 2,000 – 2,499 | 2,500 – 2,999 | 3,000 – 3,499 | 3,500 – 3,999 | 4,000 – 4,499 | 4,500 – 4,999 | 5,000 or more |
| Classification | Extremely Low Birth Weight | Very Low Birth Weight | Low Birth Weight | Normal Birth Weight | High Birth Weight | ||||||
Extremely Low Birth Weight
Less than 500 grams (1 lb 1 oz or less)
500 – 999 grams (1 lb 2 oz – 2 lb 3 oz)
Very Low Birth Weight
1,000 – 1,499 grams (2 lb 4 oz – 3 lb 4 oz)
Low Birth Weight
1,500–1,999 grams (3 lb 5 oz – 4 lb 6 oz)
2,000–2,499 grams (4 lb 7 oz – 5 lb 8 oz)
Normal Birth Weight
2,500–2,999 grams (5 lb 9 oz – 6 lb 9 oz)
3,000–3,499 grams (6 lb 10 oz – 7 lb 11 oz)
3,500–3,999 grams (7 lb 12 oz – 8 lb 13 oz)
High Birth Weight (macrosomia)
4,000–4,499 grams (8 lb 14 oz – 9 lb 14 oz)
4,500–4,999 grams (9 lb 15 oz – 11 lb 0 oz)
5,000 grams or more (11 lb 1 oz or more)
The primary causes of VLBW are premature birth (born <37 weeks gestation, and often <30 weeks) and intrauterine growth restriction (IUGR), usually due to problems with placenta, maternal health, or to birth defects. Many VLBW babies with IUGR are preterm and thus are both physically small and physiologically immature.
References
- ↑ <pubmed>2342739</pubmed>
- ↑ USA National Vital Statistics System - Birth Data
Search Pubmed: Birth
| System Links: Introduction | Cardiovascular | Coelomic Cavity | Endocrine | Gastrointestinal Tract | Genital | Head | Immune | Integumentary | Musculoskeletal | Neural | Neural Crest | Placenta | Renal | Respiratory | Sensory | Birth |