Trisomy 18
| Embryology - 27 Apr 2024 |
|---|
| Google Translate - select your language from the list shown below (this will open a new external page) |
|
العربية | català | 中文 | 中國傳統的 | français | Deutsche | עִברִית | हिंदी | bahasa Indonesia | italiano | 日本語 | 한국어 | မြန်မာ | Pilipino | Polskie | português | ਪੰਜਾਬੀ ਦੇ | Română | русский | Español | Swahili | Svensk | ไทย | Türkçe | اردو | ייִדיש | Tiếng Việt These external translations are automated and may not be accurate. (More? About Translations) |
LD40.2 Complete Trisomy 18
ICD-11 - LD40.2 Complete trisomy 18
|
Introduction
Q91 Edwards' syndrome and Patau's syndrome (ICD-11 beta) - LC20.3 Complete trisomy 18
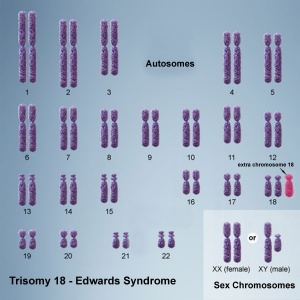
(Edwards Syndrome, 18T) An aneuploidy, first recognized as a specific clinical entity by the discovery of an extra chromosome 18 in babies with a particular pattern of malformation by independent groups[1][2][3] and named after one of the key authors, John Hilton Edwards.[1]
In many cases associated abnormalities include: fetal growth restriction, polyhydramnios and congenital heart defects.
Both trisomy 13 and trisomy 18 are generally considered fatal anomalies, with a majority of infants dying in the first year after birth[4], see also the recent Japanese study.[5]
Some Recent Findings
|
| More recent papers |
|---|
|
This table allows an automated computer search of the external PubMed database using the listed "Search term" text link.
More? References | Discussion Page | Journal Searches | 2019 References | 2020 References Search term: Trisomy 18 | Edwards Syndrome |
| Older papers |
|---|
| These papers originally appeared in the Some Recent Findings table, but as that list grew in length have now been shuffled down to this collapsible table.
See also the Discussion Page for other references listed by year and References on this current page.
|
Survival Rate
Stillbirths occurs prenatally in 40% cases with fetal demise also occurring before and during onset of labor.
| Time | Percentage |
|---|---|
| 24 h | 63% |
| 1 week | 43% |
| 1 month | 33% |
| 1 year | 3% |
| Survival rate from a Japanese study of 73 live-born infants.[5] Trisomy 18 | |
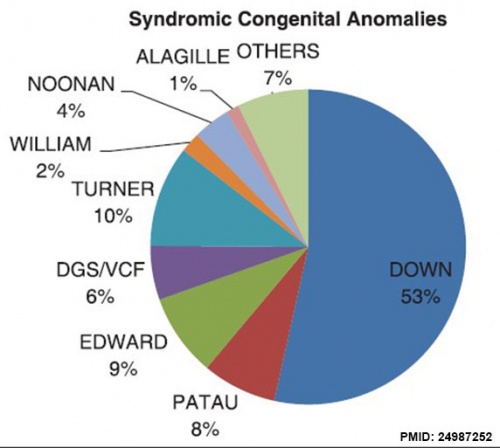
Prevalence
Abnormalities from USA Nationwide Inpatient Sample database (1998 to 2008)[11]
Features
| Frequency | Organ/System | Prevalent type of malformation |
|---|---|---|
| Common (>75%) | heart | septal defects, patent ductus arteriosus, and polyvalvular disease |
| Frequent (25-75%) | genitourinary | horseshoe kidney |
| Less frequent (5-25%) | gastrointestinal
central nervous system craniofacial eye limb |
omphalocele, esophageal atresia with tracheo-esophageal fistula, pyloric stenosis, Meckel diverticulum
cerebellar hypoplasia, agenesis of corpus callosum, polymicrogyria, spina bifida orofacial clefts microphthalmia, coloboma, cataract, corneal opacities radial aplasia/hypoplasia |
| Table modified from[9] | ||
Pedbase Entry
Definition
A chromosomal disorder resulting in a syndrome characterized by specific (small) dysmorphic features and organ malformations.
Epidemiology
incidence: 1/8000 live births most die in embryonic or fetal life 2nd most common autosomal aberration 2nd most common multiple malformation syndrome age of onset: newborn risk factors: advanced maternal age F > M (4:1)
History
1960 first recognized as a specific clinical entity by the discovery of an extra chromosome 18 in babies with a particular pattern of malformation by three independent groups (Edwards et al., Patau et al., Smith et al.)
Pathogenesis - Genetics
Trisomy 18
90% of cases due to meiotic nondisjunction less than 1% recurrence rate
Mosaicism
10% of cases due to postzygotic (postfertilization) mitotic nondisjunction leads to the partial clinical expression of Trisomy 18 with a longer survival
Translocations
very rare give rise to partial trisomy 18 syndromes short arm: causes non-specific clinical features with mild or no mental deficiency long arm: entire: clinically indistinguishable from trisomy 18 distal 1/3 -> : partial clinical picture of trisomy 18 with a longer survival and less profound mental retardation
Clinical Features
Dysmorphic Features
1. Facial
- microcephaly with prominent occiput
- narrow bifrontal diameter
- short palpabral fissures
- low-set malformed ears
- cleft lip +/- palate
- narrow palatal arch
- micrognathia
2. Skeletal
- neck - webbed
- chest - short sternum, widely spaced nipples
- hips - small pelvis, congenital dislocation of the hips, limited hip abduction
- extremities - phocomelia, rockerbottom feet or equinovarus, short dorsiflexed big toes, fixed flexion deformity of the fingers (overlapping of the 2nd and 5th fingers over the 3rd and 4th fingers), simple arch pattern of the fingers and toes, hypoplasia of fingernails, single crease of 5th finger or all fingers (absence of interphalangeal flexion creases), simian crease
Organ Malformations
1. Central Nervous System
- severe mental retardation
- hypotonia -> hypertonia
- neural tube defects
- poor suck and weak cry
- failure to thrive
- ocular anomalies
2. Respiratory
- apnea
3. Cardiovascular( >95%)
- major: VSD, ASD, PDA
- minor: transposition, ToF, coarctation, anomalous coronary artery, dextrocardia, aberrant subclavian artery, arteriosclerosis, PS, bicuspid aortic and/or pulmonic valves
4. Gastrointestinal
- inguinal, umbilical, and/or diaphragmatic hernia
- congenital defects: diastasis recti, heterotopic pancreas, malrotation, Meckel's, tracheoesophageal fistula
5. Genitourinary
- cryptorchidism
- congenital defects: double ureter, ectopic kidney, horseshoe kidney, hydronephrosis, polycystic kidney
Investigations
Imaging Studies
- to rule out organ malformations:
- cardiovascular anomalies - Echo
- gastrointestinal anomalies - Barium Swallow, Endoscope
- genitourinary anomalies - Ultrasound
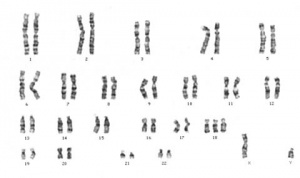
Karyotyping
Management
Supportive, very poor prognosis.
- 30% dying by 1 month of age
- 50% dying by 2 months of age
- 90% dying by 12 months of age
Genetic counselling, recurrence rate depends on genotype.
(modified from original 1999 Pedbase entry)
References
- ↑ 1.0 1.1 EDWARDS JH, HARNDEN DG, CAMERON AH, CROSSE VM & WOLFF OH. (1960). A new trisomic syndrome. Lancet , 1, 787-90. PMID: 13819419
- ↑ PATAU K, SMITH DW, THERMAN E, INHORN SL & WAGNER HP. (1960). Multiple congenital anomaly caused by an extra autosome. Lancet , 1, 790-3. PMID: 14430807
- ↑ SMITH DW, PATAU K, THERMAN E & INHORN SL. (1960). A new autosomal trisomy syndrome: multiple congenital anomalies caused by an extra chromosome. J. Pediatr. , 57, 338-45. PMID: 13831938
- ↑ Nelson KE, Hexem KR & Feudtner C. (2012). Inpatient hospital care of children with trisomy 13 and trisomy 18 in the United States. Pediatrics , 129, 869-76. PMID: 22492767 DOI.
- ↑ 5.0 5.1 5.2 Nagase H, Ishikawa H, Toyoshima K, Itani Y, Furuya N, Kurosawa K, Hirahara F & Yamanaka M. (2016). Fetal outcome of trisomy 18 diagnosed after 22 weeks of gestation: Experience of 123 cases at a single perinatal center. Congenit Anom (Kyoto) , 56, 35-40. PMID: 26104883 DOI.
- ↑ Goel N, Morris JK, Tucker D, de Walle HEK, Bakker MK, Kancherla V, Marengo L, Canfield MA, Kallen K, Lelong N, Camelo JL, Stallings EB, Jones AM, Nance A, Huynh MP, Martínez-Fernández ML, Sipek A, Pierini A, Nembhard WN, Goetz D, Rissmann A, Groisman B, Luna-Muñoz L, Szabova E, Lapchenko S, Zarante I, Hurtado-Villa P, Martinez LE, Tagliabue G, Landau D, Gatt M, Dastgiri S & Morgan M. (2019). Trisomy 13 and 18-Prevalence and mortality-A multi-registry population based analysis. Am. J. Med. Genet. A , 179, 2382-2392. PMID: 31566869 DOI.
- ↑ Farmakis SG, Barnes AM, Carey JC & Braddock SR. (2019). Solid tumor screening recommendations in trisomy 18. Am. J. Med. Genet. A , 179, 455-466. PMID: 30637956 DOI.
- ↑ Becker DA, Tang Y, Jacobs AP, Biggio JR, Edwards RK & Subramaniam A. (2019). Sensitivity of prenatal ultrasound for detection of trisomy 18. J. Matern. Fetal. Neonatal. Med. , 32, 3716-3722. PMID: 29712489 DOI.
- ↑ 9.0 9.1 Cereda A & Carey JC. (2012). The trisomy 18 syndrome. Orphanet J Rare Dis , 7, 81. PMID: 23088440 DOI.
- ↑ Miller DT, Adam MP, Aradhya S, Biesecker LG, Brothman AR, Carter NP, Church DM, Crolla JA, Eichler EE, Epstein CJ, Faucett WA, Feuk L, Friedman JM, Hamosh A, Jackson L, Kaminsky EB, Kok K, Krantz ID, Kuhn RM, Lee C, Ostell JM, Rosenberg C, Scherer SW, Spinner NB, Stavropoulos DJ, Tepperberg JH, Thorland EC, Vermeesch JR, Waggoner DJ, Watson MS, Martin CL & Ledbetter DH. (2010). Consensus statement: chromosomal microarray is a first-tier clinical diagnostic test for individuals with developmental disabilities or congenital anomalies. Am. J. Hum. Genet. , 86, 749-64. PMID: 20466091 DOI.
- ↑ Egbe A, Lee S, Ho D, Uppu S & Srivastava S. (2014). Prevalence of congenital anomalies in newborns with congenital heart disease diagnosis. Ann Pediatr Cardiol , 7, 86-91. PMID: 24987252 DOI.
Articles
Mudaliyar US & Mudaliyar SU. (2017). Strawberry skull in Edwards syndrome. BJR Case Rep , 3, 20170045. PMID: 30363185 DOI.
Reviews
Satgé D, Nishi M, Sirvent N & Vekemans M. (2016). A tumor profile in Edwards syndrome (trisomy 18). Am J Med Genet C Semin Med Genet , 172, 296-306. PMID: 27474103 DOI.
Roberts W, Zurada A, Zurada-ZieliŃSka A, Gielecki J & Loukas M. (2016). Anatomy of trisomy 18. Clin Anat , 29, 628-32. PMID: 27087248 DOI.
Janvier A, Farlow B & Barrington K. (2016). Cardiac surgery for children with trisomies 13 and 18: Where are we now?. Semin. Perinatol. , 40, 254-60. PMID: 26847083 DOI.
Cereda A & Carey JC. (2012). The trisomy 18 syndrome. Orphanet J Rare Dis , 7, 81. PMID: 23088440 DOI.
Rosa RF, Rosa RC, Zen PR, Graziadio C & Paskulin GA. (2013). Trisomy 18: review of the clinical, etiologic, prognostic, and ethical aspects. Rev Paul Pediatr , 31, 111-20. PMID: 23703053
Search Pubmed
Search Pubmed: trisomy 13 | Edwards Syndrome
External Links
External Links Notice - The dynamic nature of the internet may mean that some of these listed links may no longer function. If the link no longer works search the web with the link text or name. Links to any external commercial sites are provided for information purposes only and should never be considered an endorsement. UNSW Embryology is provided as an educational resource with no clinical information or commercial affiliation.
- Medlineplus - Trisomy 18
- Trisomy 18 Organization
- Better Health Victoria - trisomy disorders
- SOFT USA Support Organization For Trisomy 18, 13, and Related Disorders
- SOFT UK Support Organisation for trisomy 13/18 and related disorders
- Trisomy 18 Support Program
- The Chromosome 18 Registry & Research Society
Glossary Links
- Glossary: A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | Numbers | Symbols | Term Link
Cite this page: Hill, M.A. (2024, April 27) Embryology Trisomy 18. Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/Trisomy_18
- © Dr Mark Hill 2024, UNSW Embryology ISBN: 978 0 7334 2609 4 - UNSW CRICOS Provider Code No. 00098G