LA04 Congenital hydrocephalus
| ICD-11
|
LA04 Congenital hydrocephalus
- A disease caused by failure of the brain to correctly develop during the antenatal period. This condition is characterized by a rapid increase in head circumference or an unusually large head size due to excessive accumulation of cerebrospinal fluid in the brain. This condition may also present with vomiting, sleepiness, irritability, downward deviation of the eyes, or seizures. Confirmation is through observation of cerebrospinal fluid within cerebral ventricles by imaging.
LA04.0 Hydrocephalus with stenosis of the aqueduct of Sylvius - (HSAS) or Bickers-Adams syndrome is characterised by the association of hydrocephaly, severe intellectual deficit, spasticity and adducted thumbs, and is part of the L1 syndrome.
|
| International Classification of Diseases ICD-11 20 Developmental anomalies (beta draft)
|
| ICD-11 Beta Draft - NOT FINAL, updated on a daily basis, It is not approved by WHO, NOT TO BE USED for CODING except for agreed FIELD TRIALS.
Chapter 20 Developmental anomalies, only a few examples of the draft ICD-11 Beta coding and tree structure for "structural developmental anomalies" within this section are shown in the table below.
|
| Mortality and Morbidity Statistics - 20 Developmental Anomalies
|
Structural Developmental Anomalies
- Structural developmental anomalies of the nervous system
- LA00 Anencephaly or similar anomalies
- LA01 Cephalocele
- LA02 Spina bifida
- LA03 Arnold-Chiari malformation type II
- LA04 Congenital hydrocephalus
- LA05 Cerebral structural developmental anomalies
- LA06 Cerebellar structural developmental anomalies
- LA07 Structural developmental anomalies of the neurenteric canal, spinal cord or vertebral column
- LA0Y Other specified structural developmental anomalies of the nervous system
- LA0Z Structural developmental anomalies of the nervous system, unspecified
- Structural developmental anomalies of the eye, eyelid or lacrimal apparatus
- LA10 Structural developmental anomalies of ocular globes
- LA11 Structural developmental anomalies of the anterior segment of eye
- LA30 Structural developmental anomalies of lens or zonula
- LA31 Structural developmental anomalies of the posterior segment of eye
- LA32 Structural developmental anomalies of eyelid, lacrimal apparatus or orbit
- LA3Y Other specified structural developmental anomalies of the eye, eyelid or lacrimal apparatus
- LA3Z Structural developmental anomalies of the eye, eyelid or lacrimal apparatus, unspecified
- Structural developmental anomalies of the ear
- LA40 Structural anomaly of eustachian apparatus
- LA41 Minor anomalies of pinnae
- LA42 Structural developmental anomalies of ear causing hearing impairment
- LA43 Otocephaly
- LA44 Accessory auricle
- LA4Y Other specified structural developmental anomalies of the ear
- LA4Z Structural developmental anomalies of the ear, unspecified
- Structural developmental anomalies of the face, mouth or teeth
- LA50 Structural developmental anomalies of teeth and periodontal tissues
- LA51 Structural developmental anomalies of mouth or tongue
- Clefts of lip, alveolus or palate
- LA70 Congenital velopharyngeal incompetence
- LA71 Facial clefts
- LA72 Facial asymmetry
- LA73 Macrocheilia
- LA74 Microcheilia
- LA75 Compression facies
- LA76 Pierre Robin syndrome
- LC20 Dermoid cyst
- LA7Y Other specified structural developmental anomalies of the face, mouth or teeth
- LA7Z Structural developmental anomalies of the face, mouth or teeth, unspecified
- Structural developmental anomalies of the neck
- Structural developmental anomalies of the respiratory system
- Structural developmental anomalies of the circulatory system
- Structural developmental anomaly of heart and great vessels
- LB00 Congenital heart or great vessel related acquired abnormality
- LB01 Congenital anomaly of atrioventricular or ventriculo-arterial connections
- LB02 Congenital anomaly of the mediastinal veins Congenital anomaly of atria or atrial septum
- LB20 Congenital anomaly of atrioventricular valves or septum
- LB21 Congenital anomaly of ventricles and ventricular septum
- LB22 Functionally univentricular heart
- LB23 Congenital anomaly of ventriculo-arterial valves and adjacent regions
- LB24 Congenital anomaly of great arteries including arterial duct
- LB25 Anomalous position-orientation of heart
- LB26 Total mirror imagery
- LB27 Left isomerism
- LB28 Congenital anomaly of coronary arteries
- LB29 Structural developmental anomalies of the pericardium
- LB2Y Other specified structural developmental anomaly of heart and great vessels
- LB2Z Structural developmental anomaly of heart and great vessels, unspecified
- LB30 Structural developmental anomalies of the peripheral vascular system
- LB30.1 Capillary malformations
- LB30.2 Lymphatic malformations
- LB30.21 Macrocystic lymphatic malformation
- LB30.22 Microcystic lymphatic malformation
- LB30.23 Cystic hygroma in fetus
- BD23.1 Primary lymphoedema
- EK91 Yellow nail syndrome
- LC5F.26 Noonan syndrome
- LB30.2Y Other specified lymphatic malformations
- LB30.2Z Lymphatic malformations, unspecified
- LB30.3 Peripheral venous malformations
- LB30.4 Peripheral arteriovenous malformations
- LB30.5 Peripheral arterial malformations
- LB30.6 Pulmonary arteriovenous fistula
- LB30.Y Other specified structural developmental anomalies of the peripheral vascular system
- LB30.Z Structural developmental anomalies of the peripheral vascular system, unspecified
- LB3Y Other specified structural developmental anomalies of the circulatory system
- LB3Z Structural developmental anomalies of the circulatory system, unspecified
- Structural developmental anomalies of the diaphragm, abdominal wall or umbilical cord
- Structural developmental anomalies of the digestive tract
- Structural developmental anomalies of the liver, biliary tract, pancreas or spleen
- Structural developmental anomalies of the urinary system
- Structural developmental anomalies of the female genital system
- Structural developmental anomalies of the male genital system
- Structural developmental anomalies of the breast
- Structural developmental anomalies of the skeleton
- Structural developmental anomalies of the skin
- Structural developmental anomalies of the adrenal glands
|
| Multiple developmental anomalies or syndromes
|
| Chromosomal anomalies, excluding gene mutations
|
| Conditions with disorders of intellectual development as a relevant clinical feature
|
| LD6Y Other specified developmental anomalies
LD6Z Developmental anomalies, unspecified
|
| CD-11 Beta Draft - NOT FINAL, updated on a daily basis, It is not approved by WHO, NOT TO BE USED for CODING except for agreed FIELD TRIALS.
See also International Classification of Diseases
ICD-10
|
Introduction

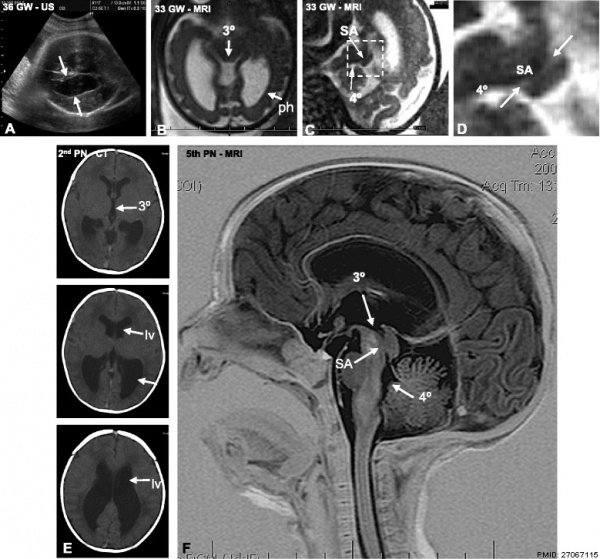
MRI Congenital hydrocephalus.
[1]This is a defect of cerebrospinal fliud (CSF) flow, excess fluid production or impaired fluid absorption and can be congenital or acquired. Estimated incidence of 1 in 1000 live births the condition leads to enlarged ventricles and head, separated skull cranial sutures and fontanelles. Obstruction of CSF flow can occur at any time (prenatally or postnatally) and leads to accumulation of within the ventricles. The time of onset will have different effects and should be compared to the equilivant neurological events that are occuring.
Ventricular obstruction usually occurs at the level of the narrowest site, the cerebral aqueduct (aqueduct stenosis), but can occur elsewhere, and can be caused by viral infection or zoonotic disease.
Severe ventriculomegaly is defined by fetal ultrasound as enlargement of the ventricular atria, with a diameter of greater than 15 mm in the transventricular plane.
- Links: hydrocephalus | neural abnormalities | ventricular
Some Recent Findings
- Cerebro-venous hypertension: a frequent cause of so-called "external hydrocephalus" in infantsCite error: Invalid
<ref> tag; name cannot be a simple integer. Use a descriptive title "External hydrocephalus (eHC) is commonly defined as a subtype of infant "hydrocephalus" consisting of macrocepahly associated with enlarged subarachnoid space and no or mild ventriculomegaly. This status is thought to be related to impaired CSF absorption because of arachnoid villi immaturity. However, other factors like the venous system might be involved in the development of the clinical picture. Seventeen patients with the typical clinical feature of eHC were included. In 15, venous sinus abnormalities were found. There was a significant correlation between the volume of the widened cortical subarachnoid space (CSAS) and the number of venous sinus segments affected. Conversely, ventricular volume was not correlated. These results support the hypothesis that impaired venous outflow plays a major role in external hydrocephalus development. Raised venous pressure increases intracranial pressure accelerating head growth, resulting in an enlargement of the cortical subarachnoid space. Increased venous pressure increases the capillary bed pressure and brain turgor preventing ventricular space to enlarge forcing displacement of ventricular CSF to the subarachnoid space. As a result, ventriculomegaly is rarely found. The descriptive term "external hydrocephalus" implying a primary etiology within the CSF system is misleading and this work supports the notion that venous hypertension is the leading cause of the clinical picture."
- Spontaneous Ventriculostomy into the Subdural Space in a Neonate with Congenital Hydrocephalus[2] "We report a case of spontaneous temporary resolution of congenital hydrocephalus due to drainage into the subdural space, which is not a physiological space for cerebrospinal fluid (CSF). This is the first report of spontaneous drainage of CSF into the subdural space, and we term it "ventriculosubdurostomy." We highlight the fact that spontaneous resolution of hydrocephalus due to drainage into a nonphysiological CSF space is temporary."
- Diagnosis, treatment, and long-term outcomes of fetal hydrocephalus[3] "This study analyzed 156 cases of fetal hydrocephalus treated at Osaka National Hospital from 1992 to 2011 to review current methods for diagnosing and treating fetal hydrocephalus, and for estimating its clinical outcome. This was a retrospective study of a single institute (Osaka National Hospital). Of 156 cases in total, 37% were diagnosed as isolated ventriculomegaly, 50% as another type of malformation (36 cases of myelomeningocele, six of holoprosencephaly, three of Dandy-Walker syndrome, one case of Joubert syndrome, 12 of arachnoid cyst, nine of encephalocele, three of atresia of Monro and eight of corpus callosum agenesis, and 13% as secondary hydrocephalus. Diagnoses were made between 13 and 40 weeks of gestation (average 27 weeks). Diagnosis was made before 21 weeks of gestation in 24% of cases, from the first day of 22 weeks to the sixth day of 27 weeks in 27%, and after the first day of 28 weeks in 49%. With the exclusion of 17 aborted cases and 40 cases in which the patients were too young to evaluate or lost during follow-up, the final outcome was analyzed for 90 cases. Of these, 17% of the patients died, 21% showed severe retardation, 13% moderate retardation, 26% mild retardation, and 23% showed a good outcome. The long-term outcome was mostly influenced by the basic disease and accompanying anomaly. The time of diagnosis showed no correlation with outcome. Hydrocephalus associated with arachnoid cyst, atresia of Monro, and corpus callosum agenesis, and hydrocephalus due to fetal intracranial hemorrhage, resulted in good outcomes. By contrast, holoprosencephaly, hydrocephalus associated with encephalocele, syndromic hydrocephalus, and hydrocephalus due to fetal virus infection led to poor outcomes. For accurate diagnosis and proper counseling, established protocols are important for the diagnosis and treatment of fetal hydrocephalus, including not only fetal sonography, fetal magnetic resonance imaging, and TORCH (toxoplasma, rubella, cytomegalovirus, herpes simplex) screening test, but also chromosomal and gene testing."
|
| More recent papers
|
|
This table allows an automated computer search of the external PubMed database using the listed "Search term" text link.
- This search now requires a manual link as the original PubMed extension has been disabled.
- The displayed list of references do not reflect any editorial selection of material based on content or relevance.
- References also appear on this list based upon the date of the actual page viewing.
References listed on the rest of the content page and the associated discussion page (listed under the publication year sub-headings) do include some editorial selection based upon both relevance and availability.
More? References | Discussion Page | Journal Searches | 2019 References | 2020 References
Search term: Congenital Hydrocephalus | ventriculomegaly
|
Aqueduct of Sylvius
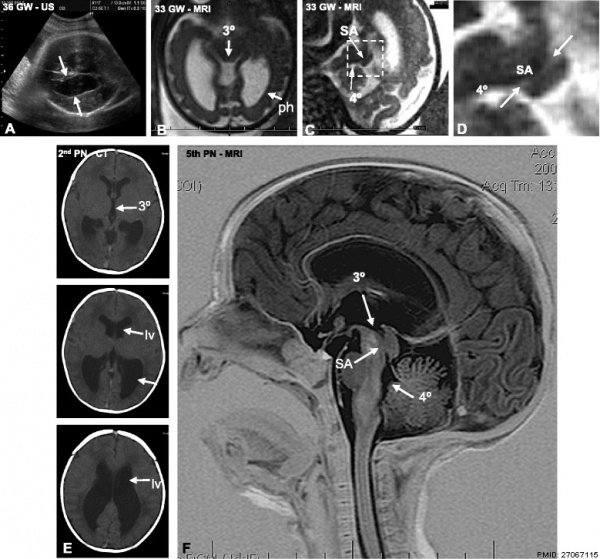
Progressive obliteration of the aqueduct of Sylvius in hydrocephalus[4]
|
- a Ultrasound of fetal patient at 36 GW showing dilation of the lateral ventricles (arrows).
- b MRI at 33 GW. The third ventricle (3°) and posterior horns of the lateral ventricles (ph) are dilated.
- c MRI at 33 weeks. Stenosis of the SA is shown.
- d Detailed magnification of the area framed in C showing stenosis of the SA. 4°, fourth ventricle.
- e CT at 39 GW (or the 2nd PN day). The lateral (LV) and third (3°) ventricles are dilated.
- f MRI of the brain on the 5th postnatal day, sagittal T2 imaging. The SA is obliterated
|
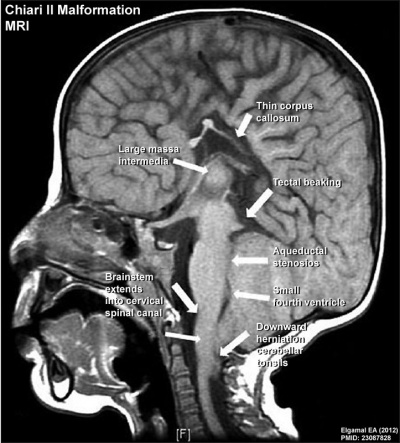
Arnold-Chiari syndrome
ICD - Q07 Other congenital malformations of nervous system - Q07.0 Arnold-Chiari syndrome
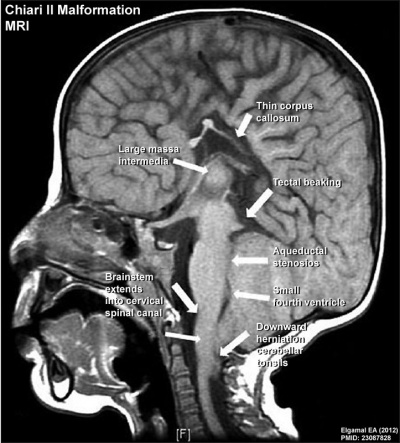
Magnetic Resonance Image Sagittal T1-weighted image showing Chiari II malformation.[5]
Treatment
Ventriculoperitoneal Shunt

Ventriculoperitoneal shunt
[6]Ventriculoperitoneal (VP) shunting is a surgical procedure that commenced in the 1960's to treat hydrocephalus and relieve increased pressure inside the skull due to excess cerebrospinal fluid (CSF) on the brain. A catheter is placed inside of the brain ventricle, the catheter is then tunneled under the skin from the scalp down into the abdominal cavity, where the other end opens into the peritoneal cavity. The catheter contains a valve (located in the skin behind the ear) that opens when pressure builds up around the brain. Complication can include: infections (8-10%), catheter blockage, over-drainage and movement of the catheter.
- Links: Medline Plus article
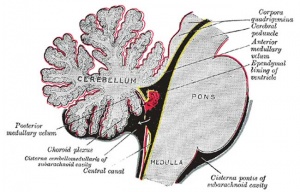
Third Ventriculostomy
An endoscopic surgical technique where a small perforation is made in the thinned floor of the third ventricle, allowing cerebrospinal fluid (CSF) out of the blocked ventricular system and into the interpeduncular cistern 9 (Cisterna interpeduncularis) that is also a normal CSF space. This was an early surgical technique, reported as early as 1922, that has revived with modern magnetic resonance imaging (MRI) and surgical endoscopic techniques that result in less damage. Due to the location of the surgery complications can include: bleeding, endocrine disfunction, and diabetes insipidus.
External Hydrocephalus
External hydrocephalus (cerebro-venous hypertension) consists of macrocepahly associated with enlarged subarachnoid space and no or mild ventriculomegaly. It has been suggested that it is impaired venous outflow, rather than impaired CSF absorption from immature arachnoid villi, is the primary etiology within the CSF system.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title Venous sinus abnormalities correlated with the volume of the widened cortical subarachnoid space (CSAS) and the number of venous sinus segments affected, ventricular volume was not correlated.
References
- ↑ Bokhari R & Baeesa S. (2012). Remote cerebellar hemorrhage due to ventriculoperitoneal shunt in an infant: a case report. J Med Case Rep , 6, 222. PMID: 22846583 DOI.
- ↑ Krishna Pillai M, Kariyattil R, Rubene L, Kumar R, Govindaraju V & Kochummen K. (2018). Spontaneous Ventriculostomy into the Subdural Space in a Neonate with Congenital Hydrocephalus. Pediatr Neurosurg , , . PMID: 29627843 DOI.
- ↑ Yamasaki M, Nonaka M, Bamba Y, Teramoto C, Ban C & Pooh RK. (2012). Diagnosis, treatment, and long-term outcomes of fetal hydrocephalus. Semin Fetal Neonatal Med , 17, 330-5. PMID: 23089488 DOI.
- ↑ Ortega E, Muñoz RI, Luza N, Guerra F, Guerra M, Vio K, Henzi R, Jaque J, Rodriguez S, McAllister JP & Rodriguez E. (2016). The value of early and comprehensive diagnoses in a human fetus with hydrocephalus and progressive obliteration of the aqueduct of Sylvius: Case Report. BMC Neurol , 16, 45. PMID: 27067115 DOI.
- ↑ Elgamal EA. (2012). Natural history of hydrocephalus in children with spinal open neural tube defect. Surg Neurol Int , 3, 112. PMID: 23087828 DOI.
- ↑ Whiley SP, Mantokoudis G, Ott D, Zimmerman H & Exadaktylos AK. (2012). A review of full-body radiography in nontraumatic emergency medicine. Emerg Med Int , 2012, 108129. PMID: 23243508 DOI.
Reviews
Venkataramana NK. (2011). Hydrocephalus Indian scenario - A review. J Pediatr Neurosci , 6, S11-22. PMID: 22069421 DOI.
Search PubMed
Search Bookshelf: Congenital Hydrocephalus
Search Pubmed: Congenital Hydrocephalus | Ventriculoperitoneal Shunt
External Links
External Links Notice - The dynamic nature of the internet may mean that some of these listed links may no longer function. If the link no longer works search the web with the link text or name. Links to any external commercial sites are provided for information purposes only and should never be considered an endorsement. UNSW Embryology is provided as an educational resource with no clinical information or commercial affiliation.
Glossary Links
- Glossary: A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | Numbers | Symbols | Term Link
Cite this page: Hill, M.A. (2026, February 27) Embryology Abnormal Development - Congenital Hydrocephalus. Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/Abnormal_Development_-_Congenital_Hydrocephalus
- What Links Here?
- © Dr Mark Hill 2026, UNSW Embryology ISBN: 978 0 7334 2609 4 - UNSW CRICOS Provider Code No. 00098G