2010 Lecture 8
Introduction
This lecture is an introduction to the development and functions of the placenta.
The placenta (Greek, plakuos = flat cake) named on the basis of this organs appearance. The placenta a mateno-fetal organ which begins developing at implantation of the blastocyst and is delivered with the fetus at birth. Only recently have we begun to understand the many different functions this organ carries out in addition to its role in embryonic nutrition. This lecture follows on the concepts of cardiovascular development covered in the previous lecture.
The placenta and placental blood at birth has recently been seen as a new source for stem cells in bone marrow replacement therapy in many diseases. (More? Stem Cells - Cord Blood)
- Lectopia Lecture Audio
Lecture Objectives
- Understanding of placental villi development
- Understanding of placental structure
- Understanding of placental functions
- Brief understanding of placental abnormalities
Textbook References
- Human Embryology Larson Ch7 p151-188 Heart, Ch8 p189-228 Vasculature
- The Developing Human: Clinically Oriented Embryology (6th ed.) Moore and Persaud Ch14: p304-349
Other textbooks
- Before we Are Born (5th ed.) Moore and Persaud Ch12; p241-254
- Essentials of Human Embryology Larson Ch7 p97-122 Heart, Ch8 p123-146 Vasculature
- Human Embryology Fitzgerald and Fitzgerald Ch13-17: p77-111
UNSW Embryology Links
- Placenta Slides Placenta Lecture 8 2008 | Placenta Lecture 2008 - 1 slide/page | Placenta Lecture 2008 Slides - 4 slides/page | Placenta Lecture 2008 Slides - 6 slides/page
- Placenta Movies Heart Movies | Heart Looping | Atrial Septation | Realignment | Ventricular Septation | Heart Septation Models | Historic Heart Movie |
- Placenta Notes Introduction | Abnormalities | Stage 13/14 | Human (Stage22) | Histology | Villi Development | Maternal Decidua | Vascular Beds | Molecular | Postnatal | Endocrine Placenta
Nutrition
- Histiotrophic nutrition describes early placental development and the form of intital transfer of nutrition from maternal to embryo.
- Hemotrophic nutrition describes the later blood-borne nutrition.
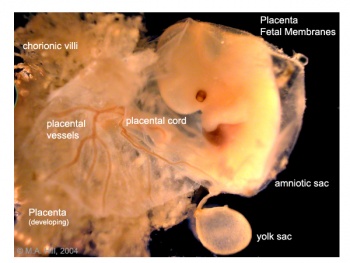
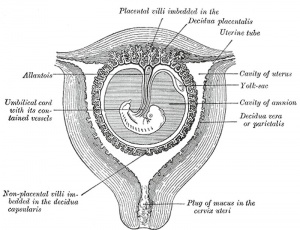
Fetal Membranes
Placenta at Birth
- Placenta (Greek, plakuos = flat cake)
- embryonic/maternal organ
- villous chorion/decidua basalis
- continuous with amniotic and chorionic sacks
Dimensions
- at birth - discoid up to 20cm diameter and 3 cm thick (term) and weighs 500-600 gm
- Shapes - accessory placenta, bidiscoid, diffuse, horseshoe
- maternal and embryonic surface, both delivered at parturition
- retention may cause uterine hemorrhage
Maternal Surface
- Cotyledons - form cobblestone appearance, originally placental septa formed grooves
- covered with maternal decidua basalis
Fetal Surface
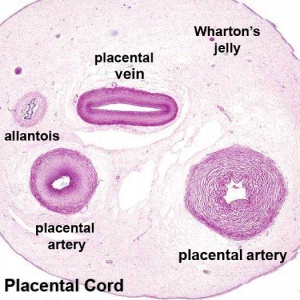
- umbilical cord attachment - cord 1-2 cm diameter, 30-90cm long
- covered with amniotic membrane and attached to chorionic plate
- umbilical vessels branch into chorionic vessels which anastomose
Placenta:fetal and maternal surfaces
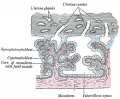
Placental Classification
Classification of placenta is on the basis of histological (microscopic) structural organization and layers between fetal and maternal circulation, giving 3 main groups:
- Haemochorial - placenta where the chorion comes in direct contact with maternal blood (human)
- Endotheliochorial - maternal endometrial blood vessels are bare to their endothelium and these comes in contact with the chorion. (dogs, cats)
- Epitheliochorial - maternal epithelium of the uterus comes in contact with the chorion.considered as primitive (pigs, cows)
The presence of these three differing types of placenta have also been used to describe the pattern mammalian evolution. See also Placental Layers
Placental Types
- Discoid in humans, mice, insectivores, rabbits, rats, and monkeys.
- Zonary in dogs, cats, bears and seals.
- Cotyledenary in cows, deer, goat, and giraffe.
- Diffuse in horses, pigs, camels, lemurs, opossums, kangaroos, and whales
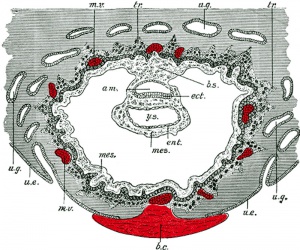
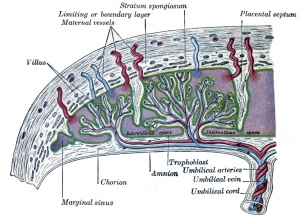
Chorionic Villi
- primary villi - week 2, first stage of chorionic villi development, trophoblastic shell cells (syncitiotrophoblasts and cytotrophoblasts) form finger-like extensions into maternal decidua.
- secondary villi - week 3, second stage of chorionic villi development, extraembryonic mesoderm grows into villi, covers entire surface of chorionic sac.
- tertiary villi third stage of chorionic villi development, mesenchyme differentiates into blood vessels and cells, forms arteriocapillary network, fuse with placental vessels, developing in connecting stalk
- stem villi - or anchoring villi, cytotrophoblast cells attached to maternal tissue.
- branched villi - or terminal villi, grow from sides of stem villi, region of main exchange, surrounded by maternal blood in intervillous spaces.
Chorionoic Villi Location
- originally cover entire chorionic surface and become restricted to decidua basalis region forming 2 regions
- Frondosum - "leafy" where villi are mainly located
- Capsularis - smooth chorion, where villi are absent or not abundant
Chorionoic Villi Trimester Development
Trimester 1 and 2
- In the first two trimesters immature intermediate villi, developmental steps towards the stem villi.
Trimester 3
- Mature intermediate villi develop during the last trimester, produce numerous terminal villi.
- Terminal villi are not active outgrowths caused by proliferation of the trophoblast, but rather passive protrusions induced by capillary coiling due to excessive longitudinal growth of the fetal capillaries within the mature intermediate villi.
- The arrangement of the capillary bed in the terminal villi can vary from simple U-like loops to a richly branched network due to capillary elongation and sprouting.
(Data from PMID: 2327595)
Placental Function
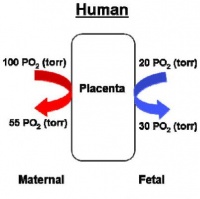
- 4 layers separate maternal and fetal blood: syncitiotrophoblast, cytotrophoblast, villi connective tissue and fetal capillary endothelium
- 3 main functions: metabolism, transport and endocrine
Placental Metabolism
Synthesizes: glycogen, cholesterol, fatty acids
- provides nutrient and energy
Placental Transport
gases and nutrition
- oxygen, carbon dioxide, carbon monoxide
- water, glucose, vitamins
- hormones, mainly steroid not protein
- electrolytes
- maternal antibodies
- waste products - urea, uric acid, bilirubin
- drugs and their metabolites (fetal drug addiction)
- infectious agents (cytomegalovirus, rubella, measles, microorganisms)
Placental Endocrine
- Human chorionic gonadotrophin (hCG) - like leutenizing hormone, supports corpus luteum
- Human chorionic somatommotropin (hCS) (or placental lactogen) - hormone level increases in maternal blood through pregnancy, decreases maternal insulin sensitivity (raising maternal blood glucose levels and decreasing maternal glucose utilization) aiding fetal nutrition ("anti-insulin" function)
- Human chorionic thyrotropin (hCT) - Peptide placental hormone, similar to anterior pituitary released thyroid stimulating hormone (TSH), which along with human chorionic gonadotrophin (hCG) is thought to act on maternal thyroid. There is little recent research published on this hormone, its level and activities.
- Human chorionic corticotropin (hCACTH) - placental hormone thought to have corticotropin (ACTH)-like activity, increasing maternal cortisol levels.
- Steroid Hormones
- progestins - progesterone, support of the endometrium and suppress uterine smooth muscle contractility.
- estrogens - estriol, stimulate growth of the myometrium and mammary gland development.
- both hormones support maternal endometrium
- Relaxin - Humans high levels early in pregnancy than at birth promotes angiogenesis probably plays a role in development of the uterus/ placenta than in the birth process
Placental Blood vessels
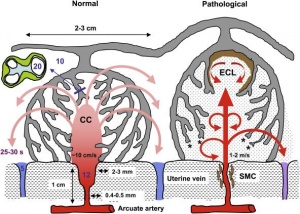
- form initially in the connecting stalk (then umbilical cord) anastomose in chorioni
- extend maternally toward chorionic villi
- extend embryonically to the sinus venosus and dorsal aorta
Arteries - paired, carry deoxygenated blood (from dorsal aorta) and waste products to the placental villi
Veins - paired initially then only left at end of embryonic period, carry oxygenated blood to the embryo (sinus venosus) Parturition (Childbirth) Overview
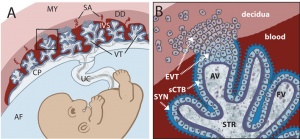
Fetal Placenta
Trophoblast cells are the major source of placental hormones.
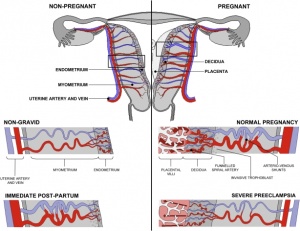
Placental growth hormone (PGH) is mainly expressed in the syncytiotrophoblast cells (PGH differs from pituitary derived growth hormone by 13 amino acids). extravillous cytotrophoblast - arise from anchoring villi invade the uterine spiral arteries, generating fibrinoid material and endovascular trophoblastic cells. syncytiotrophoblast
Fetal Blood Vessels At least 2 phases of development during pregnancy driven by vascular endothelial growth factor (VEGF):
- Initially cytotrophoblasts are the cellular stimulus to vasculogenesis and angiogenesis.
- Later Hofbauer (lacental villi macrophages of mesenchymal origin) and stromal cells take over the stimulation of blood vessel development.
Placenta Human chorionic gonadotrophin (hCG) After implantation cells within the developing placenta (syncitiotrophoblasts) synthesize and secrete Human chorionic gonadotrophin (hCG) into the maternal bloodstream. The main function of serum hCG is to maintain the corpus luteum in the maternal ovary and therefore maintain the early pregnancy, that is block the menstrual cycle. Later the placenta itself supports the pregnancy.
Maternal Placenta
Fibrinoid - said to exist as 2 forms of extracellular matrix:
- Fibrin-type fibrinoid is a maternal blood-clot product which replaces degenerative syncytiotrophoblast
- Matrix-type fibrinoid is secreted by invasive extravillous trophoblast cells.
Fibrinoid layer (Nitabuch's layer) is thought to act to prevent excessively deep implantation.
Decidualization - process of endometrial stromal cells (fibroblast-like) change in morphology (polygonal cells) and protein expression and secretion (specific decidual proteins: prolactin, insulin-like growth factor binding protein-1, tissue factor, interleukin-15, and VEGF).
- Estrogen and progesterone - receptive phase, luminal and glandular epithelial cells change in preparation for blastocyst adplantation.
- Human Chorionic gonadotropin - luminal epithelium endoreplication leading to epithelial plaque formation.
- Human Chorionic gonadotropin - trophoblast invasion and decidualization of human stromal fibroblasts.
Artery Dilatation - due to extravillous trophoblast cells invading uterine wall and maternal spiral arteries replacing both smooth muscle with fibrinoid material and part of vessel endothelium. There is also a proliferation of maternal blood vessels.
Other changes
- Endoreplication - rounds of nuclear DNA replication without intervening cell or nuclear division (mitosis).
- Cytokines - of maternal origin also act on placental development.
- Natural Killer (NK) cells - 30% of all the decidual cells towards the end of the first trimester of pregnancy. These lymphocytes are present in the maternal decidua in large numbers (70%, normal circulating blood lymphocytes 15%) close to the extravillous trophoblast cells. Have a cytolytic potential against virus-infected and tumor-transformed cells.
Placental Abnormalities
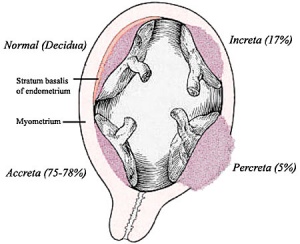
- Placenta Accreta - abnormal adherence, with absence of decidua basalis. The incidence of placenta accreta also significantly increases in women with previous cesarean section compared to those without a prior surgical delivery.
- Placenta Increta - occurs when the placenta attaches deep into the uterine wall and penetrates into the uterine muscle, but does not penetrate the uterine serosa. Placenta increta accounts for approximately 15-17% of all cases.
- Placenta Percreta - placental villi penetrate myometrium and through to uterine serosa.
- Placenta Previa - In this placenatal abnormality, the placenta overlies internal os of uterus, essentially covering the birth canal. This condition occurs in approximately 1 in 200 to 250 pregnancies. In the third trimester and at term, abnormal bleeding can require cesarian delivery and can also lead to Abruptio Placenta. Ultrasound screening programs during 1st and early 2nd trimester pregnancies now include placental localization. Diagnosis can also be made by transvaginal ultrasound.
- Vasa Previa - (vasa praevia) placental abnormality where the fetal vessels lie within the membranes close too or crossing the inner cervical os (opening). This occurs normally in 1:2500-5000 pregnancies and leads to complications similar too those for Placenta Previa.Type II is defined as the condition where the fetal vessels are found crossing over the internal os connecting either a bilobed placenta or a succenturiate lobe with the main placental mass. Some recent evidence of successful in utero laser ablation of type II vasa previa at 22.5 weeks of gestation.
- Abruptio Placenta - a retroplacental blood clot formation, abnormal hemorrhage prior to delivery.
- Chronic Intervillositis - (massive chronicintervillositis, chronic histiocytic intervillositis) Rare placental abnormality and pathology defined by inflammatory placental lesions, mainly in the intervillous space (IVS), with a maternal infiltrate of mononuclear cells (monocytes, lymphocytes, histiocytes) and intervillous fibrinoid deposition.
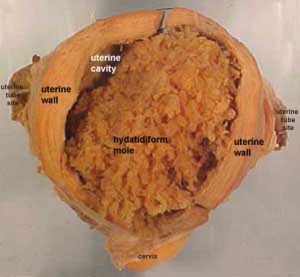
- Hydatidiform mole - placental tumor with no embryo development. Several forms of hydatidiform mole: partial mole, complete mole and persistent gestational trophoblastic tumor. Many of these tumours arise from a haploid sperm fertilizing an egg without a female pronucleus (the alternative form, an embryo without sperm contribution, is called parthenogenesis). The tumour has a "grape-like" placental appearance without enclosed embryo formation. Following a first molar pregnancy, there is approximately a 1% risk of a second molar pregnancy.
Links: Placental Abnormalities
Placental Cord Abnormalities
There are few abnormalities associated with umbilical cord development, other that abnormally short or long cords, which in most cases do not cause difficulties. In some cases though, long cords can wrap around limbs or the fetus neck, which can then restrict blood flow or lead to tissue or nerve damage, and therefore effect develoment.
- Cord knotting - can also occur (1%) in most cases these knots have no effect, in some cases of severe knotting this can prevents the passage of placental blood.
- Cord torsion - Rare event where even without knot formation can also affect placental blood flow, even leading to fetal demise.
Links: Placental Abnormalities | WebPath - umbilical cord knot 1 | WebPath - umbilical cord knot 2 | WebPath - Pseudoknot of umbilical cord, gross | WebPath - Torsion of umbilical cord, gross | WebPath - Torsion of umbilical cord, with fetal demise, gross
Placental Infections
- Several infective agents may cross into the placenta from the maternal circulation, as well as enter the embry/fetal circulation. The variety of bacterial infections that can occur during pregnancy is as variable as the potential developmental effects, from virtually insignificant to a major developmental, abortive or fatal in outcome.
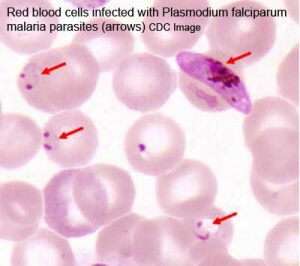
- Pregnant women have an increased susceptibility to malaria infection. Malarial infection of the placenta by sequestration of the infected red blood cells leading to low birth weight and other effects. There are four types of malaria caused by the protozoan parasite Plasmodium falciparum (main), Plasmodium vivax, Plasmodium ovale, Plasmodium malariae). This condition is common in regions where malaria is endemic with women carrying their first pregnancy (primigravida).
Placental Pathology
MH - content in this section is not examinable.
- Chronic Villitis - can occur following placental infection leading to maternal inflammation of the villous stroma, often with associated intervillositis. The inflammation can lead to disruption of blood flow and necrotic cell death.
- Massive Chronic Intervillositis (MCI) - maternal blood-filled space is filled with CD68-positive histiocytes and an increase in fibrin, occuring more commonly in the first trimester.
- Meconium Myonecrosis - prolonged meconium exposure leads to toxic death of myocytes of placental vessels (umbilical cord or chorionic plate).
- Neuroblastoma - a fetal malignancy that leads to an enlarged placenta, with tumor cells in the fetal circulation and rarely in the chorionic villi.
- Thrombophilias - (protein C or S deficiency, factor V Leiden, sickle cell disease, antiphospholipid antibody) can generate an increased fibrin/fibrinoid deposition in the maternal or intervillous space, this can trap and kill villi.
Take the Quiz
References
Textbooks
- The Developing Human: Clinically Oriented Embryology (8th Edition) by Keith L. Moore and T.V.N Persaud
- Larsen’s Human Embryology by GC. Schoenwolf, SB. Bleyl, PR. Brauer and PH. Francis-West -
Additional Textbooks
- Before We Are Born (5th ed.) Moore and Persaud
- Essentials of Human Embryology
- Human Embryology Fitzgerald and Fitzgerald
- Human Embryology and Developmental Biology Carlson
Online Textbooks
- Developmental Biology by Gilbert, Scott F. Sunderland (MA): Sinauer Associates, Inc.; c2000 - Figure 11.30. Human embryo and placenta after 40 days of gestation | Figure 15.11. Transfer of oxygen from the mother to the fetus in human embryos | Formation of extraembryonic membranes | Figure 15.9. Circulatory system of the early avian embryo
- Endocrinology: An Integrated Approach Nussey, S.S. and Whitehead, S.A. London:Taylor & Francis; c2001
Search
- Bookshelf placenta | placental villi development |
- Pubmed placenta development | placenta | placental villi |
Reviews
- Vogel P. [See Related Articles] The current molecular phylogeny of Eutherian mammals challenges previous interpretations of placental evolution. Placenta. 2005 Sep-Oct;26(8-9):591-6.
- Cross JC. [See Related Articles] How to make a placenta: mechanisms of trophoblast cell differentiation in mice--a review. Placenta. 2005 Apr;26 Suppl A:S3-9.
- Simmons DG, Cross JC. [See Related Articles] Determinants of trophoblast lineage and cell subtype specification in the mouse placenta. Dev Biol. 2005 Aug 1;284(1):12-24.
- Rama S, Rao AJ. [See Related Articles] Regulation of growth and function of the human placenta. Mol Cell Biochem. 2003 Nov;253(1-2):263-8.
- Evain-Brion D, Malassine A. [See Related Articles] Human placenta as an endocrine organ. Growth Horm IGF Res. 2003 Aug;13 Suppl A:S34-7.
External Links
- Comparative Placentation
- University of Ottawa - Histology - Placenta
- Virtual Microscopy Histology fetal-membranes | female reproductive
Placenta Terms
- after-birth - term used to describe the delivery of placenta and placental membranes following birth of the child.
- allantois - an endodermal diverticulum from the hindgut which extends from the superior end of the developing bladder into the adjacent placental cord.
- anastomose - term used to describe the connection between two tubes. Applied to describe the connection between peripheral blood vessels without an intervening capillary bed.
- angiogenesis development of new vessels from already existing vessels, this process is secondary to vasculogenesis which is the initial formation of first blood vessels by differentiation of pluripotent mesenchymal cells (extraembryonic mesoderm).
- angioblasts form clusters or blood islands on surface of yolk sac.
- capsularis
- chorionic sac fetal membrane that surrounds the developing embryo.
- cord knotting umbilical cord knotting occurs in 1%, prevents the passage of placental blood. pseudoknots also occur usually with no effect.
- cotyledons maternal side cobblestone appearance, originally placental septa formed grooves is covered with maternal decidua basalis.
- cytotrophoblast extraembryonic cells of trophoblastic shell surrounding embryo, contribute to villi and placental membranes.
- decidua basalis reaction occurs in maternal endometrium at site of, and following, blastocyst implantation. Seen as a deposition of glycogen and proliferation of blood vessels. (see also decidualization)
- decidualization process by which uterine stromal cells differentiate in response to both steroid hormones and embryonic signals into large epitheliod decidual cells. This process is essential for the progress of implantation and establishing fetal-maternal communication.
- endocrine function of placenta:
- Human chorionic gonadotrophin (hCG) like leutenizing hormone, supports corpus luteum
- Human chorionic somatommotropin (hCS) or placental lactogen, stimulate mammary development
- Human chorionic thyrotropin (hCT)
- Human chorionic corticotropin (hCACTH)
- progesterone and estrogens support maternal endometrium
- relaxin- role in parturition, softens ligaments
- fetal drug addiction occurs when drugs used maternally cross the placental barrier and can establish addiction in the unborn fetus.
- fetal erythroblastosis (Haemolytic Disease of the Newborn), an immune problem from fetus Rh+ /maternal Rh-, leakage from fetus causes anti-Rh antibodies, which is then dangerous for a 2nd child.
- frondosum-
- haemocytoblasts (hemangioblast) stem cells for embryonic blood cell formation, often appearing as a "cluster" or "island".
- Haemolytic Disease of the Newborn - see fetal erythroblastosis.
- hemotrophic nutrition - Term used to describe in late placental development the transfer of blood-borne nutrition from maternal to embryo/fetus compared to early [#histiotrophic_nutrition histiotrophic nutrition]. (More? Uterine glands provide histiotrophic nutrition for the human fetus during the first trimester of pregnancy. Burton GJ, Watson AL, Hempstock J, Skepper JN, Jauniaux E. J Clin Endocrinol Metab. 2002 Jun;87(6):2954-9. PMID: 12050279 | J Clin Endocrinol Metab.)
- histiotrophic nutrition - Term used to describe in early placental development the intital transfer of nutrition from maternal to embryo (histiotrophic nutrition) compared to later blood-borne nutrition ([#hemotrophic_nutrition hemotrophic nutrition]). Histotroph is the nutritional material accumulated in spaces between the maternal and fetal tissues, derived from the maternal endometrium and the uterine glands. This nutritional material is absorbed by phagocytosis initially by blastocyst trophectoderm and then by trophoblast of the placenta. in later placental development nutrition is by the exchange of blood-borne materials between the maternal and fetal circulations, hemotrophic nutrition. (More? Uterine glands provide histiotrophic nutrition for the human fetus during the first trimester of pregnancy. Burton GJ, Watson AL, Hempstock J, Skepper JN, Jauniaux E. J Clin Endocrinol Metab. 2002 Jun;87(6):2954-9. PMID: 12050279 | J Clin Endocrinol Metab.)
- Hofbauer cells - placental villi macrophages of mesenchymal origin with potentially additional functions (vasculogenesis/angiogenesis, villi remodeling, regulation of stromal water content) to their macrophage role.
- Human chorionic gonadotrophin- (hCG) like leutenizing hormone, supports corpus luteum
- Human chorionic somatommotropin - (hCS) or placental lactogen - hormone level increases in maternal blood through pregnancy, decreases maternal insulin sensitivity (raising maternal blood glucose levels and decreasing maternal glucose utilization) aiding fetal nutrition.
- Human chorionic thyrotropin- (hCT) placental derived hormone equivilant to thyroid
- Human chorionic corticotropin- (hCACTH) placental derived hormone equivilant to corticotropin (ACTH) from the pituitary.
- methyldopa - (alpha methyldopa) A central alpha agonist used to lower blood pressure. Used as an antihypertensive drug to lower blood pressure in pre-eclampsia, acting by either a direct or indirect central vasodilatory mechanism. A recent study suggests this drug may have a direct effect on placental and/or endothelial cell function in pre-eclampsia patients, altering angiogenic proteins. Drug commercial brandname (USA) "Aldomet", also available in combination with other drugs: methyldopa and chlorothiazide "Aldochlor", methyldopa and hydrochlorothiazide "Aldoril". (More? Placenta Abnormalities - Pre-eclampsia | Medline Plus - Methyldopa | Effect of antihypertensive therapy with alpha methyldopa on levels of angiogenic factors in pregnancies with hypertensive disorders. Khalil A, Muttukrishna S, Harrington K, Jauniaux E. PLoS ONE. 2008 Jul 23;3(7):e2766. PMID: 18648513)
- maternal antibodies- antibodies from the mother's immune system that are capable of crossing placental barrier. They can provide immune protection to the embryo, but may also participate in immune disease (fetal erythroblastosis).
- maternal sinusoids- placental spaces around chorionic villi that are filled with maternal blood. Closest maternal/fetal exchange site.
- Nitabuch's layer (fibrinoid layer) layer formed at maternal/fetal interface during placentation and is thought to act to prevent excessively deep conceptus implantation. Fibrin-type fibrinoid (maternal blood-clot product) and matrix-type fibrinoid (secreted by invasive extravillous trophoblast cells).
- placenta- (Gk. plakuos= flat cake) describes its typical mature discoid shape (20cm diameter and 3 cm thick at term,weighs 500-600 gm).
- placenta accreta- abnormal, adherence with absence of decidua basalis.
- placental arteries- paired, carry deoxygenated blood and waste from the embryo (dorsal aorta->internal iliacs->PA)
- placental blood- blood found within the placental vessels. Obviously part of the fetal blood, but can be collected at birth for theraputic use containing blood stem cells (see cord blood banks).
- placental blood vessels- form initially in the connecting stalk (then umbilical cord), anastomose in chorioni and extend maternally toward chorionic villi, extend embryonically to the sinus venosus and dorsal aorta.
- placental layers- 4 layers separate maternal and fetal blood: syncitiotrophoblast, cytotrophoblast, villi connective tissue, and fetal capillary endothelium.
- placenta percreta- abnormal, villi penetrate myometrium.
- placenta previa- placenta overlies internal os of uterus, abnormal bleeding, may require cesarian delivery.
- placental veins- paired initially then usually only one left at end of embryonic period, carry oxygenated blood to the embryo (sinus venosus)
- primary villi- develop week 2, consist of trophoblastic shell cells both syncitiotrophoblasts and cytotrophoblasts. Form finger-like extensions into the maternal endometrium.
- protein hormone- usually a protein distributed in the blood that binds to membrane receptors on target cells in different tissues. Do not easliy cross placental barrier.
- relaxin- hormone.
- secondary villi- develop week 3, extraembryonic mesoderm grows into villi, initially covers entire surface of chorionic sac.
- sinus venosus- cavity into which all major embryonic paired veins supply (vitelline, placental, cardinal)
- syncitiotrophoblast- extraembryonic cells of trophoblastic shell surrounding embryo, outside the cytotrophoblast layer, involved with implantation of the blastocyst by eroding extracellular matrix surrounding maternal endometrial cells at site of implantation, also contribute to villi. (dark staining, multinucleated)
- tertiary villi- develop week 4, mesenchyme within secondary villi differentiates into blood vessels and cells, forms arteriocapillary network, fuse with placental vessels developing in connecting stalk.
- trophoblast-
- umbilical cord- fetal attachment cord 1-2 cm diameter, 30-90cm long, covered with amniotic attached to chorionic plate, umbilical vessels (artery, vein) branch into chorionic vessels. Vessels anastomose within the placenta.
- vasculogenesis formation of first blood vessels by differentiation of pluripotent mesenchymal cells (extraembryonic mesoderm) followed by angiogenesis which is the development of new vessels from already existing vessels.
- villi- initially outgrowth of the trophoblastic shell which involve other tissues with development. Develop in sequence (primary, secondary, tertiary) with mature villi being stem por branched type.
- virus- small infectious agent able to cross placental barrier. Can infect embryo and cause developmental abnormalities. (e.g. cytomegalovirus, rubella, measles)
- vitelline- Blood vessels cover entire surface of yolk sac and connect to embryo through yolk stalk
- Arteries- arises from dorsal aorta and contribute to adult GIT arteries.
- Veins- empties into sinus venosus and contribute to the adult portal system.
- waste products products of cellular metabolism and cellular debris, e.g.- urea, uric acid, bilirubin
- Wharton's jelly placental cord (umbilical cord) gelatinous connective tissue composed of myofibroblast-like stromal cells, collagen fibers, and proteoglycans. Increases in volume (myxomatous, connective tissue embedded in mucus) at parturition to assist closure of placental blood vessels. Matrix cells from Wharton's jelly have recently been identified as a potential source of stem cells. This placental cord substance is named after Thomas Wharton (1614-1673) an English physician and anatomist who first described it.
Glossary Links
- Glossary: A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | Numbers | Symbols | Term Link
Course Content 2009
Embryology Introduction | Cell Division/Fertilization | Cell Division/Fertilization | Week 1&2 Development | Week 3 Development | Lab 2 | Mesoderm Development | Ectoderm, Early Neural, Neural Crest | Lab 3 | Early Vascular Development | Placenta | Lab 4 | Endoderm, Early Gastrointestinal | Respiratory Development | Lab 5 | Head Development | Neural Crest Development | Lab 6 | Musculoskeletal Development | Limb Development | Lab 7 | Kidney | Genital | Lab 8 | Sensory - Ear | Integumentary | Lab 9 | Sensory - Eye | Endocrine | Lab 10 | Late Vascular Development | Fetal | Lab 11 | Birth, Postnatal | Revision | Lab 12 | Lecture Audio | Course Timetable
Cite this page: Hill, M.A. (2026, February 26) Embryology 2010 Lecture 8. Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/2010_Lecture_8
- © Dr Mark Hill 2026, UNSW Embryology ISBN: 978 0 7334 2609 4 - UNSW CRICOS Provider Code No. 00098G