2010 Lecture 23
Fetal Development and Birth
<Flowplayer height="400" width="380" autoplay="true">fetal growth.flv</Flowplayer>
Introduction
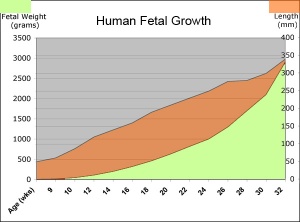
The fetal period (9-36 weeks) is about continued differentiation of organs and tissues, most importantly this period is about growth both in size and weight.
The long Fetal period (4x the embryonic period) is a time of extensive growth in size and mass as well as ongoing differentiation of organ systems established in the embryonic period and do so at different times. For example, the brain continues to grow and develop extensively during this period (and postnatally), the respiratory system differentiates (and completes only just before birth), the urogenital system further differentiates between male/female, endocrine and gastrointestinal tract begins to function.
- First Trimester (1 - 12 weeks) - embryonic and early fetal
- Second Trimester (13 - 24 weeks) - organ development and function, growth
- Third Trimester (25 - 40 weeks) - organ function and rapid growth
Textbooks
- Human Embryology (3rd ed.) Larson Chapter 15: Fetal development and the Fetus as Patient p481-499
- The Developing Human: Clinically Oriented Embryology (8th ed.) Moore and Persaud Chapter 6. The Fetal Period: Ninth Week to Birth
- Color Atlas of Clinical Embryology (2nd ed.) Moore, Persaud and Shiota Ch3: 9th to 38th weeks of human development p50-68
| Fetal Links: fetal | Week 10 | Week 12 | second trimester | third trimester | fetal neural | Fetal Blood Sampling | fetal growth restriction | birth | birth weight | preterm birth | Developmental Origins of Health and Disease | macrosomia | BGD Practical | Medicine Lecture | Science Lecture | Lecture Movie | Category:Human Fetus | Category:Fetal | |||
|
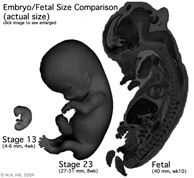
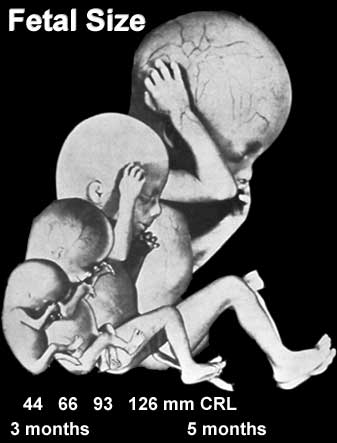
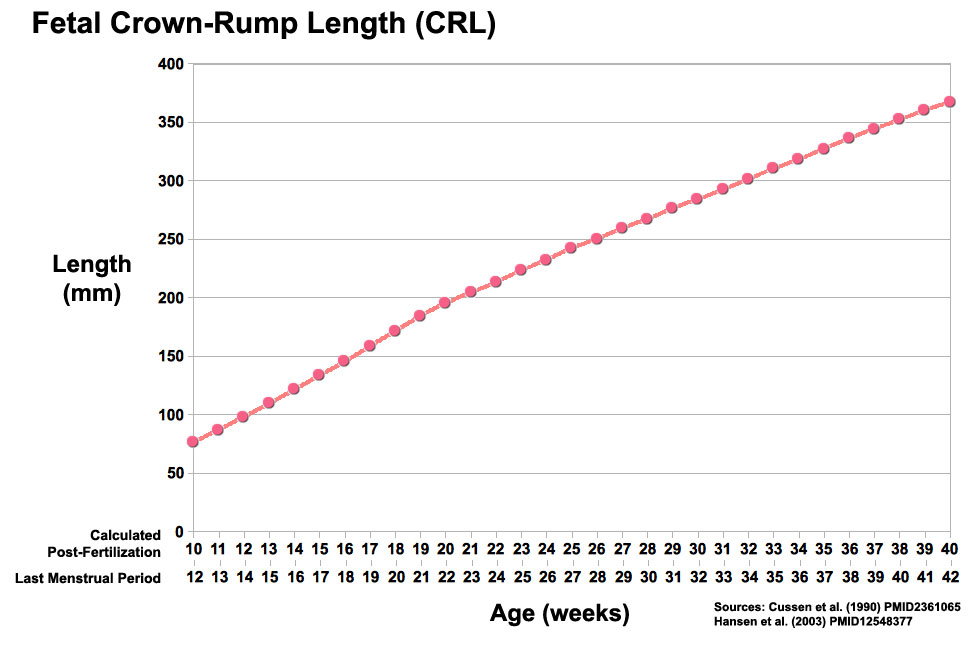
Fetal Size
Fetal length change is greatest in the middle period (second trimester).
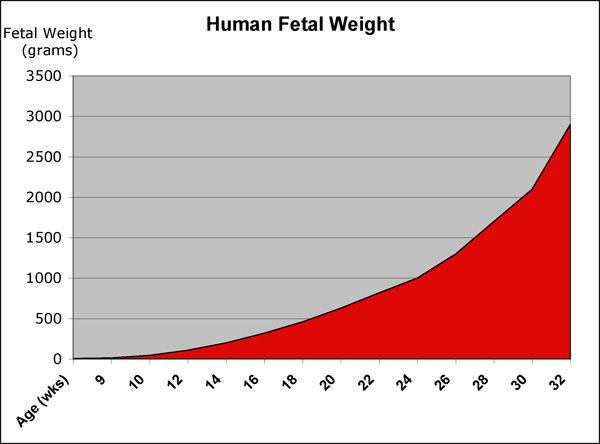
Fetal Weight
See also Fetal origins hypothesis and Normal Development - Birth - Low Birth Weight
Birth Weight
| Birth weight (grams) | less 500 | 500 – 999 | 1,000 – 1,499 | 1,500 – 1,999 | 2,000 – 2,499 | 2,500 – 2,999 | 3,000 – 3,499 | 3,500 – 3,999 | 4,000 – 4,499 | 4,500 – 4,999 | 5,000 or more |
| Classification | Extremely Low Birth Weight | Very Low Birth Weight | Low Birth Weight | Normal Birth Weight | High Birth Weight | ||||||
The primary causes of VLBW are premature birth (born <37 weeks gestation, and often <30 weeks) and intrauterine growth restriction (IUGR), usually due to problems with placenta, maternal health, or to birth defects. Many VLBW babies with IUGR are preterm and thus are both physically small and physiologically immature.
Fetal Neural
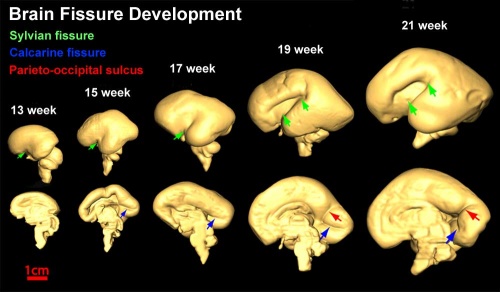
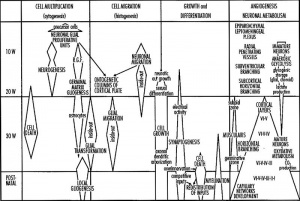
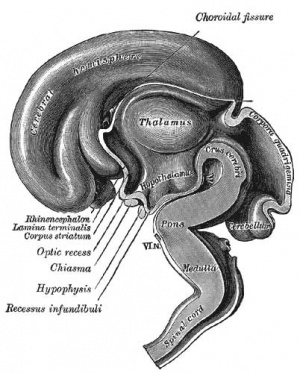
During the fetal period there is ongoing growth in size, weight and surface area of the brain and spinal cord. Microscopically there is ongoing: cell migration, extension of processes, cell death and glial cell development.
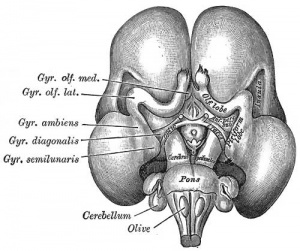
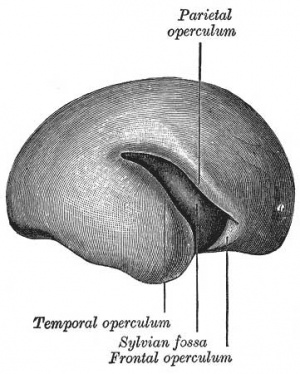
Cortical maturation (sulcation and gyration) and vascularization of the lateral surface of the brain starts with the insular cortex (insula, insulary cortex or insular lobe) region during the fetal period. This cerebral cortex region in the adult brain lies deep within the lateral sulcus between the temporal lobe and the parietal lobe.
- sulcation - The process of brain growth in the second to third trimester which forms sulci, grooves or folds visible on fetal brain surface as gyri grow (gyration). Abnormalities of these processes can lead to a smooth brain (lissencephaly).
- gyration - The development of surface folds on the brain (singular, gyrus)
Insular Gyral and Sulcal Development
- 13-17 gestational weeks - appearance of the first sulcus
- 18-19 gestational weeks - development of the periinsular sulci
- 20-22 gestational weeks - central sulci and opercularization of the insula
- 24-26 gestational weeks - covering of the posterior insula
- 27-28 gestational weeks - closure of the laeteral sulcus (Sylvian fissure or lateral fissure)
(Data from: Afif A, etal., 2007)
- Between 29-41 weeks volumes of: total brain, cerebral gray matter, unmyelinated white matter, myelinated, and cerebrospinal fluid (from MRI)
- grey matter- mainly neuronal cell bodies; white matter- mainly neural processes and glia.
- total brain tissue volume increased linearly over this period at a rate of 22 ml/week.
- Total grey matter also showed a linear increase in relative intracranial volume of approximately 1.4% or 15 ml/week.
- The rapid increase in total grey matter is mainly due to a fourfold increase in cortical grey matter.
- Quantification of extracerebral and intraventricular CSF was found to change only minimally.
(Text - modified from Huppi etal., (1998) Quantitative magnetic resonance imaging of brain development in premature and mature newborns. Ann Neurol 43(2):224-235.)
Neural development will continue after birth with substantial growth, death and reorganization occuring during the postnatally (MH - postnatal not described in this current lecture)
Fetal Cardiovascular
MH - covered in last week's lecture Late Vascular Development.
- fetal neutrophils, monocytes, and macrophages are produced
- mononuclear phagocytes do not mature until after birth
Immune System
- maternal placenta transfer of IgG not other immunoglobulin isotypes.
- fetal lymphocytes (mature T and B cells) produced not activated
MH - see Postnatal lecture - maternal milk IgG and IgA antibodies, leukocytes, secretory IgA, lactoferrin, lysozyme, and oligosaccharides and glycoconjugates that are receptor analogs for microbial adhesins and toxins.
Fetal Respiratory
MH - covered in lecture Respiratory Development.
Month 3-6 - lungs appear glandular, end month 6 alveolar cells type 2 appear and begin to secrete surfactant.
Month 7 - respiratory bronchioles proliferate and end in alveolar ducts and sacs.
Lung Stages
- week 4 - 5 embryonic
- week 5 - 17 pseudoglandular
- week 16 - 25 canalicular
- week 24 - 40 terminal sac
- late fetal - 8 years alveolar
Fetal Genital
MH - introduced in the Genital Development lecture.
Gonad Descent
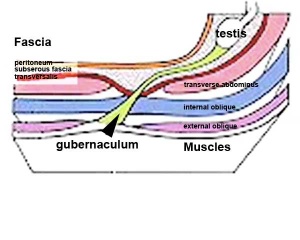
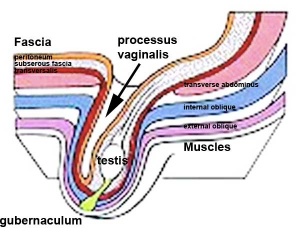
- Both kidney and gonads develop retroperitoneally, with the gonads moving into the abdomen or eventually into the scrotal sacs.
- During fetal development the gubernaculum and fetal growth in both male and female, changes the gonads’ relative positions finally reaching their adult locations.
Both female and male gonads undergo anatomical descent.
- Ovaries ‐ undergo caudal and lateral shifts to be suspended in the broad ligament of the uterus, gubernaculum does not shorten, it attaches to paramesonephric ducts, causing medial movement into the pelvis.
- Testes ‐ two anatomical phases in descent, transabdominal and transinguinal, under the influence of the shortening gubernaculum.
The testis (white) lies in the subserous fascia (spotted) a cavity processus vaginalis evaginates into the scrotum, and the gubernaculum (green) attached to the testis shortens drawing it into the scotal sac. As it descends it passes through the inguinal canal which extends from the deep ring (transversalis fascia) to the superficial ring (external oblique muscle). Descent of the testes into the scrotal sac begins generally during week 26 and may take several days. The animation shows the path of a single testis.
Incomplete or failed descent can occur unilaterally or bilaterally, is more common in premature births, and can be completed postnatally.
Data from a recent study of male human fetal (between 10 and 35 weeks) gonad position.
- 10 to 23 weeks - (9.45%) had migrated from the abdomen and were situated in the inguinal canal
- 24 to 26 weeks - (57.9%) had migrated from the abdomen
- 27 to 29 weeks - (16.7%) had not descended to the scrotum
Fetal Endocrine
Pituitary Hormones
- HPA axis established by week 20
- Pituitary functional throughout fetal development
Thyroid Hormone
- required for metabolic activity, also in the newborn
- important for neural development
Parathyroid Hormone
- newborn has total calcium levels (approx 20 grams) accumulated mainly in the 3rd trimester (weeks 28–40)
- fetal parathyroid hormone (PTH) potentially available from 10–12 weeks and PTH does not cross the placenta
- fetus relatively hypercalcemic, active transplacental transport of Ca2+ to fetus
- maternal serum - calcium ions (Ca2+), inorganic phosphate (Pi) and PTH concentrations are within the non-pregnant normal range throughout pregnancy.
- maternal bone turnover increases in the 3rd trimester.
(Based on Endocrinology - Materno—fetal calcium balance)
Pancreatic Hormones
- maternal diabetes can affect fetal pancreas development (increase in fetal islet beta cells).
Gonadal Hormones
- testosterone - required during fetal development for external genital development and internal genital tract in male.
- estrogens - secreted inactive precursor converted to active form by placenta.
Endocrinology - Control of steroid production in the fetal gonads | Neuroscience - The Effect of Sex Hormones on Neural Circuitry
Fetal Origins Hypothesis
Maternal derived abnormalities relate to lifestyle, environment and nutrition and while some of these directly effect development. There is also growing evidence that some effects are more subtle and relate to later life health events. This theory is based on the early statistical analysis carried out by Barker of low birth weight data collected in the early 1900's in the south east of England which he then compared with these same babies later health outcomes. The theory was therefore originally called the "Barker Hypothesis" and has recently been renamed as "fetal origins" or "programming".
- Links: Fetal Origins Hypothesis
Birth Introduction
There are a great number of comprehensive, scientific and general, books and articles that cover Parturition, Birth or Childbirth.
Birth or parturition is a critical stage in development, representing in mammals a transition from direct maternal support of fetal development, physical expulsion and establishment of the newborns own respiratory, circulatory and digestive systems.
Textbooks
- Human Embryology (2nd ed.) Larson Chapter 15 p471-488
- The Developing Human: Clinically Oriented Embryology (6th ed.) Moore and Persaud Chapter 7 p129-167
Gestation Period
The median duration of gestation for first births from assumed ovulation to delivery was 274 days (just over 39 weeks). For multiple births, the median duration of pregnancy was 269 days (38.4 weeks).
- "...one should count back 3 months from the first day of the last menses, then add 15 days for primiparas or 10 days for multiparas, instead of using the common algorithm for Naegele's rule." Reference: Mittendorf R, Williams MA, Berkey CS, Cotter PF. The length of uncomplicated human gestation. Obstet Gynecol. 1990 Jun;75(6):929-32
Historically, Franz Carl Naegele (1777-1851) developed the first scientific rule for estimating length of a pregnany.
Childbirth
- Parturition (Latin, parturitio = "childbirth") describes expelling the fetus, placenta and fetal membranes and is probably initiated by fetus not mother.
- Preterm birth - Risks of preterm birth in abnormal low birth weight (intrauterine growth restriction) and high (large for gestational age) categories are 2- to 3-fold greater than the risk among appropriate-for-gestational-age infants.
- Maternal labor - uterine contractions and dilation of cervix, process under endocrine regulation
- Placenta and fetal membranes - (Latin, secundina = "following") expelled after neonate birth
Uterine Myometrial Changes
- Smooth muscle fibers - hypertrophy not proliferation
- Stretching of myometrium - stimulates spontaneous muscular contraction, during pregnancy progesterone inhibits contraction
- Stimulating contraction - increased estrogen levels (placental secretion sensitizes smooth muscle), increased oxytocin levels (fetal oxytocin release- force and frequency of contraction), fetal pituitary prostaglandin production (estrogen and oxytocin stimulate endometrial production of prostaglandin)
Progesterone
- maintains pregnancy - initially synthesized by corpus luteum, then levels maintained by placenta
- hyperpolarizes myometrial cells (-65 mV), reduces excitability and conductivity
- Level in plasma may fall just before parturition, definitely decreases following delivery of placenta
Estrogens
- Group of steroidal hormones, peak when parturition begins
- induce increased synthesis of actomyosin and ATP in myometrial cells
- alter membrane potential (-50 Mv) enhances excitation/conduction
- act to directly increase myometrial contraction
- indirectly by increasing oxytocin from pituitary gland
- Estriol - synthesized by fetus and placenta
Oxytocin
- Peptide hormone (8aa) from maternal posterior pituitary, initiation and maintenance of labour (synthetic form labour induction)
- myometrium sensitivity to oxytocin (increased by estrogen, decreased by progesterone)
- stimulus for release - mechanical stimulation of uterus, cervix and vagina (ethanol inhibits release)
Prostaglandins
- hydroxy fatty acids - sythesized by placenta, amniotic fliud contains mainly PGF2 alpha, causes myometrial contraction (also in maternal plasma)
- PGF2 alpha and PGE2 - used to induce labour (intravenous, oral, intravaginal, intraamniotic)
- Aspirin inhibitor of PG synthesis - leads to increased duration of pregnancy
External Environment
- mainly shown in other species parturition occurs in peaceful undisturbed surroundings, stress may have an inhibitory effect on oxytocin release
- Most human births occur at night (peak at 3am) diurnal rhythm influence
Labor Stages
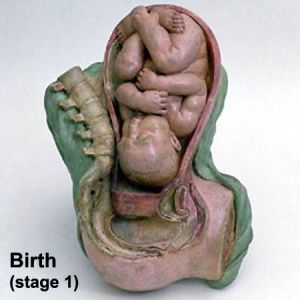
Stage 1 - dilatation
- uterine contractions 10 minutes apart, function to dilate cervix fetal membranes rupture releasing amnion, 7 -12 hours (longer for first child)
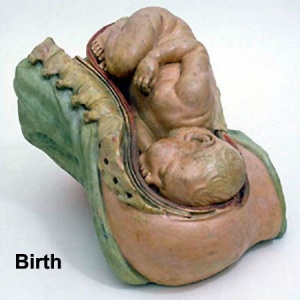
Stage 2 - expulsion
- uterine contractions push fetus through cervix and vagina, contractions 2-3 minutes apart, 20 - 50 minutes
Stage 3 - placental
- following child delivery contractions continue to expel placenta. haematoma separates placenta from uterine wall, separation occurs at spongy layer of decidua basalis, 15 minutes
Stage 4 - recovery
- continued myometrial contraction closes spiral arteries, 2+ hours
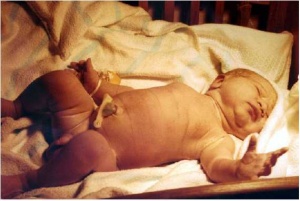
Newborn Homoeostasis
Newborn has to establish new functioning systems in a balanced and regulated manner (homoeostasis).
- lung function
- circulatory changes
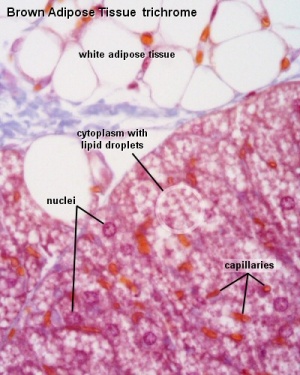
- thermoregulation
- endocrine function
- nutrition
- gastrointestinal tract function
- waste
- kidney function
Glucocorticoids - have an important role in the preparation for birth, including involvement in lung and cardiac development, and the maturation of enzymes in a variety of pathways.
Respiration
- Lungs at birth collapsed and fluid-filled - replaced with air by powerful inspiratory movement and absorption through the alveoli
- Lung epithelia has to rapidly change from its prenatal secretory function to that of fluid absorbtion.
- initiated by a late fetal change in alveolar epithelial cell (AEC) chloride and fluid secretion to sodium and fluid absorption.
- absorption requires sodium-potassium ATPase (Na-K-ATPase) together with apical sodium entry mechanisms (Epithelial Sodium Channels, ENaC)
- Fetal thyroid hormone is thought to have a hormonal role in this developmental switch
- These changes and pressure also lead to the pulmonary sytem becoming activated and changes in the circulatory shunting that existed before birth.
- During the late fetal period regular fetal breathing movements (FBM) also occur preparing both the skeletomuscular sysyem and lungs mechanically for respiration.
- Respiratory Rate is higher than adult (30 breaths/minute).
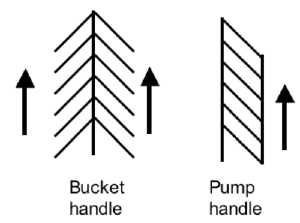
- Rib Orientation - Infant rib is virtually horizontal, allowing diaphragmatic breathing only. Adult rib orientation is oblique (both anterior and lateral views), allows for pump-handle and bucket handle types of inspiration.
Postnatal Development - Respiratory
Cardiovascular
- Umbilical Vasculature - The umbilical blood vessel cavity is lost postnatally over the course of weeks to months after birth. The adult anatomical remnant of the umbilical vein between the umbilicus and liver is the ligamentum teres.
- Foramen Ovale - two separate forms of foramen ovale closure; functional and structural. Functional closure begins at the first breath and is rapid. Structural (anatomical) closure is much slower and generally occurs before the end of the first year.
- Ductus Arteriosus - a direct connection between the pulmonary trunk and the dorsal aorta. Postnatal closure occurs initially by by smooth muscle contraction and begins at the first breath and is rapid, completed within the first day (about 15 hr after birth). Anatomical closure is much slower occuring by 2–3 weeks after birth (33% of infants), by 2 months (90% of infants) and by 1 year (99% of infants). The adult anatomical remnant of the ductus arteriosus is the ligamentum arteriosum.
- Ductus Venosus - connects portal and umbilical blood to the inferior vena cava. Functional closure occurs postnatally within hours. Structural closure commences days after birth and completes by 18 to 20 days. The adult anatomical remnant of the ductus venosus is the ligamentum venosum (a dorsal fissure on the liver).
Neonatal Testing
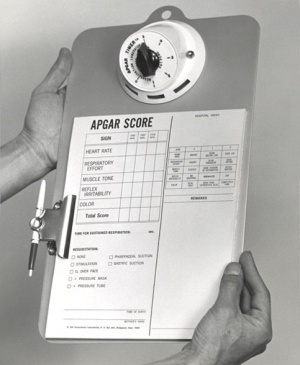
Apgar Test
A historic neonatal test designed by Dr Virginia Apgar[1] used in nearly all maternity clinics to assess the newborn infants well being assigned scores for each of 5 indicators: Heart Rate, Respiratory Effort, Reflex Irritability, Muscle Tone, Colour Measured at one and five minutes after birth the Score values are totalled for all indicators: 7-10 is considered normal, 4-7 may require resuscitative measures, 3 and below require immediate resuscitation. In recent years there has been some controversy of the relevance and accuracy of some of the criteria used in this test, though many feel it is still an invaluable initial assessment tool particularly where medical services are limited.
- Measured at one and five minutes after birth.
- The Score values are totalled for all indicators
- 7 to 10 is considered normal
- 4 to 7 may require resuscitative measures
- 3 and below require immediate resuscitation
| Indicator | Score 0 | Score 1 | Score 2 |
| Activity (muscle tone) |
Limp; no movement | Some flexion of arms and legs | Active motion |
| Pulse (heart rate) |
No heart rate | Fewer than 100 beats per minute | At least 100 beats per minute |
| Grimace (reflex response) |
No response to airways being suctioned | Grimace during suctioning | Grimace and pull away, cough, or sneeze during suctioning |
| Appearance (color) |
The baby's whole body is completely bluish-gray or pale | Good color in body with bluish hands or feet | Good color all over |
| Respiration (breathing) |
Not breathing | Weak cry; may sound like whimpering, slow or irregular breathing | Good, strong cry; normal rate and effort of breathing |
Reference: Apgar, V. A proposal for a new method of evaluation of the newborn infant. Curr Res Anesth Analg. 1953 Jul-Aug;32(4):260-7. PMID:13083014
- Links: Apgar test
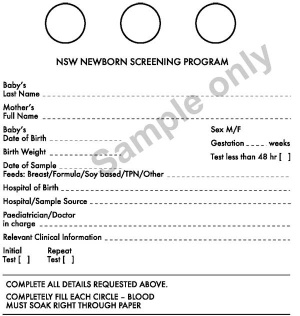
Guthrie Test
A blood screening test developed by Dr Robert Guthrie (1916-95) at University of Buffalo.[2] The test is carried out on neonatal (newborn) blood detecting markers for a variety of known disorders (phenylketonuria (PKU), hypothyroidism and cystic fibrosis). In the Australian states of NSW and Victoria, the Guthrie Cards are currently stored indefinitely.
- Links: Guthrie test
Heart
- An electrocardiogram (ECG / EKG) is an electrical recording of the heart which may identify electrical disorders including long QT syndrome.
Hip Displasia
- Non-specific hip instability is a common finding in newborns, particularly in females.
- More than 80% of clinically unstable hips at birth resolve spontaneously. Screening newborns for Developmental dysplasia of the hip (DDH) shows an incidence in infants between 1.5 and 20 per 1000 births. This incidence is influenced by several factors (diagnostic criteria, gender, genetic and racial factors, and age of the population).
Links: Musculoskeletal Abnormalities- Congenital Dislocation of the Hip | [hipdyssyn.pdf Screening for Developmental Dysplasia of the Hip PDF] | Screening for developmental dysplasia of the hip. Evidence synthesis no. 42. Rockville, Md.: Agency for Healthcare Research and Quality http://www.ahrq.gov/downloads/pub/prevent/pdfser/hipdyssyn.pdf | U.S. Preventive Service Task Force. Screening for developmental dysplasia of the hip: recommendation statement. Am Fam Physician. 2006 Jun 1;73(11):1992-6.
Hearing
- The incidence of significant permanent hearing loss is approximately 1-3/1000 newborns.
- Neonatal hearing screening is carried out in the USA, UK and in Australia (2002 NSW Statewide Infant Screening Hearing Program, SWISH) There is a general guide giving a timetable for a number of simple responses that a neonate should make if hearing has developed normally.
- State Wide Infant Screening Hearing Program (SWISH) a newborn hearing testing program using an automated auditory response technology (AABR). Program was introduced in NSW Australia in 2002 across 17 area health service coordinators. It is thought that in NSW 86,000 births/year = 86-172 babies potentially born with significant permanent hearing loss.
- Automated Auditory Brainstem Response (AABR) uses a stimulus which is delivered through earphones and detected by scalp electrodes. The test takes between 8 to 20 minutes and has a sensitivity 96-99%.
Premature Birth
| Year | < 34 weeks % | 34-36 weeks % | total preterm % |
| 1990 | 3.3 | 7.3 | 10.6 |
| 1995 | 3.3 | 7.7 | 11 |
| 2000 | 3.4 | 8.2 | 11.6 |
| 2005 | 3.6 | 9.1 | 12.7 |
Data from: Prevention of preterm birth: a renewed national priority Damus K. Curr Opin Obstet Gynecol. 2008 Dec;20(6):590-6 PMID: 18989136
Australia Recommendations
Perinatal care at the borderlines of viability: a consensus statement based on a NSW and ACT consensus workshop (February 2005) published in The Medical Journal of Australia 2006; 185 (9): 495-500.
- < 23 weeks survival is minimal and the risk of major morbidity is so high that initiation of resuscitation is not appropriate.
- 23 weeks active treatment may be discussed, but would be discouraged in NSW/ACT neonatal intensive care units.
- 23 to 25 weeks otherwise normal infant, there is an increasing obligation to treat. However, it is acceptable medical practice not to initiate intensive care if parents so wish, following appropriate counselling.
- 24 weeks antenatal transfer to a tertiary centre for fetal reasons is indicated. The option of non-initiation of intensive care/resuscitation should be offered.
- 25 weeks active treatment is usually offered, but the option of non-initiation of intensive care/resuscitation (presence of adverse fetal factors such as twin-to-twin transfusion, intrauterine growth restriction or chorioamnionitis) should also be discussed.
- 26 weeks + otherwise normal infant the obligation to treat is very high, and treatment should generally be initiated unless there are exceptional circumstances.
Abnormalities
Teratology
How different environmental effects during the pregnancy may influence outcomes. A teratogen (Greek, teraton = monster) is defined as any agent that causes a structural abnormality (congenital abnormalities) following fetal exposure during pregnancy. The overall effect depends on dosage and time of exposure (see critical periods below).
Absolute risk - the rate of occurrence of an abnormal phenotype among individuals exposed to the agent. (e.g. fetal alcohol syndrome)
Relative risk - the ratio of the rate of the condition among the exposed and the nonexposed. (e.g. smokers risk of having a low birth weight baby compared to non-smokers) A high relative risk may indicate a low absolute risk if the condition is rare.
Mutagen - a chemical or agent that can cause permanent damage to the deoxyribonucleic acid (DNA) in a cell. DNA damage in the human egg or sperm may lead to reduced fertility, spontaneous abortion (miscarriage), birth defects and heritable diseases.
Fetotoxicant - is a chemical that adversely affects the developing fetus, resulting in low birth weight, symptoms of poisoning at birth or stillbirth (fetus dies before it is born).
Synergism - when the combined effect of exposure to more than one chemical at one time, or to a chemical in combination with other hazards (heat, radiation, infection) results in effects of such exposure to be greater than the sum of the individual effects of each hazard by itself.
Toxicogenomics - the interaction between the genome, chemicals in the environment, and disease. Cells exposed to a stress, drug or toxicant respond by altering the pattern of expression of genes within their chromosomes. Based on new genetic and microarray technologies.
Critical Periods
There are many birth associated abnormalities, only a few examples are listed below.
Labor Abnormalities
- Premature Labor - occurs 7 -10% in humans, contributes 75% perinatal mortalities
- Underdeveloped Systems - particularly respiratory, surfactant, hyaline membrane disease (see respiratory development lecture)
Placental Abnormalities
- placenta accreta - abnormal adherence, with absence of decidua basalis
- placenta percreta - villi penetrate myometrium
- placenta previa - placenta overlies internal os of uterus, abnormal bleeding, cesarian delivery
Breech Delivery
- Historically, breech-born children were called agrippi, meaning "delivered with difficulty" (aegre parti).
- Breech position - occurs in about 3% of fetuses when buttocks or lower limb are presented to the birth canal rather than normal cephalic (head-first) position (presentation).
- Associated increased - perinatal mortality, perinatal morbidity, recurrence in successive siblings
Current research suggests that genetically that both men and women delivered in breech presentation at term could also contribute to an increased risk of breech delivery in their offspring. ([#18369204 Nordtveit TI, etal., 2008])
Meconium aspiration syndrome
- meconium is formed from gut and associated organ secretions as well as cells and debris from the swallowed amniotic fluid.
- Meconium accumulates during the fetal period in the large intestine (bowel). It can be described as being a generally dark colour (green black) , sticky and odourless.
- Normally this meconium is defaecated (passed) postnatally over the first 48 hours and then transitional stools from day 4.
- Abnormally this meconium is defaecated in utero, due to oxygen deprivation and other stresses. Premature discharge into the amniotic sac can lead to mixing with amniotic fluid and be reswallowed by the fetus. This is meconium aspiration syndrome and can damage both the developing lungs and placental vessels.
Necrotizing Enterocolitis
Occurs postnatally in mainly in premature and low birth weight infants (1 in 2,000 - 4,000 births). The underdeveloped gastointestinal tract appears to be susceptible to bacteria, normally found within the tract,to spread widely to other regions where they damage the tract wall and may enter the bloodstream.
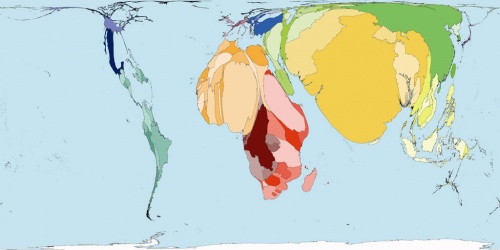
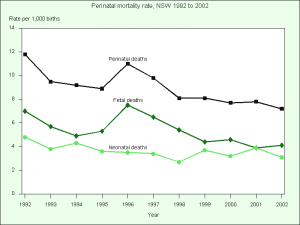
Stillbirth and Perinatal Death
The distorted world map above shows the relative distribution of early neonatal death by country. Note the over-representation of Africa and Asia compared with Europe, USA and Australia. [3]
New South Wales (2002)
Perinatal deaths (period up to 7 days after birth)
- 613 perinatal deaths were reported
- Unexplained antepartum deaths: 26.3% of perinatal deaths (or 39.2% of stillbirths)
- Spontaneous preterm labour: 20.6% (less than 37 weeks gestation)
- Congenital abnormality: 16.8%
- Antepartum haemorrhage: 8.5%
- Specific perinatal conditions: 7.3%, of which twin-twin transfusion accounted for 2.3% of deaths
- Hypertension (high blood pressure): 5.5%
- Perinatal infection: 4.4%
- Maternal disease: 4.4%
- Hypoxic peripartum death: 3.8%
Neonatal deaths (four weeks/month after birth)
- extreme prematurity was most common cause (39.6%)
- congenital abnormality (19.3%)
- neurological disease (13.4%)
- cardio-respiratory conditions (11.9%)
- infection (8.4%)
Data from Report of the New South Wales Chief Health Officer, 2004 (accessed 19Oct05)
Birth Terms
amniotomy - birth medical procedure thought to speed labor, where the amniotic sac is artificially ruptured using a tool (amniohook).
breech - fetal buttocks presented first and can also occur in different forms depending on presentation (complete breech, frank breech, footing breech, knee breech).
decidual activation - increased uterine proteolysis and extracellular matrix degradation.
dilatation - opening of the cervix in preparation for birth (expressed in centimetres).
effacement - shortening or thinning of the cervix, in preparation for birth.
forceps - mechanical "plier-like" tool used on fetal head to aid birth.
fetal macrosomia - clinical description for a fetus that is too large, condition increases steadily with advancing gestational age and defined by a variety of birthweights. In pregnant women anywhere between 2 - 15% have birth weights of greater than 4000 grams (4 Kg, 8 lb 13 oz).
membrane rupture - breaking of the amniotic membrane and release of amniotic fluid (water breaking).
morbidity - (Latin, morbidus = "sick" or "unhealthy") refers to a diseased state, disability, or poor health due to any cause.
presentation - how the fetus is situated in the uterus.
presenting part - part of fetus body that is closest to the cervix.
second stage of labour - passage of the baby through the birth canal into the outside world.
Vacuum Extractor - suction cap device used on fetal head to aid birth.
Vertex Presentation (cephalic presentation) where the fetus head is the presenting part, most common and safest birth position.
Glossary Links
- Glossary: A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | Numbers | Symbols | Term Link
Course Content 2010
Embryology Introduction | Cell Division/Fertilization | Lab 1 | Week 1&2 Development | Week 3 Development | Lab 2 | Mesoderm Development | Ectoderm, Early Neural, Neural Crest | Lab 3 | Early Vascular Development | Placenta | Lab 4 | Endoderm, Early Gastrointestinal | Respiratory Development | Lab 5 | Head Development | Neural Crest Development | Lab 6 | Musculoskeletal Development | Limb Development | Lab 7 | Kidney | Genital | Lab 8 | Sensory | Stem Cells | Stem Cells | Endocrine | Lab 10 | Late Vascular Development | Integumentary | Lab 11 | Birth, Postnatal | Revision | Lab 12 | Lecture Audio | Course Timetable
Cite this page: Hill, M.A. (2026, February 27) Embryology 2010 Lecture 23. Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/2010_Lecture_23
- © Dr Mark Hill 2026, UNSW Embryology ISBN: 978 0 7334 2609 4 - UNSW CRICOS Provider Code No. 00098G