2009 Lecture 15
Kidney Development
Introduction
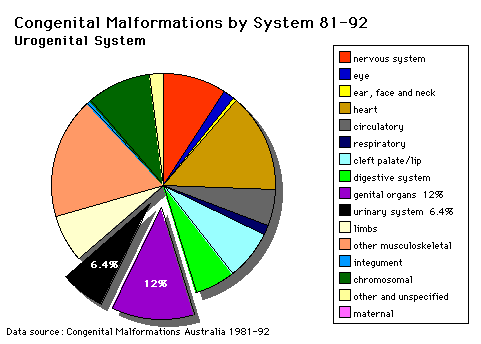
The paired adult kidneys filter blood, excrete waste, reabsorb water and have endocrine functions. In the embryo, there are several stages in their development closely linked to genital development. The nephron, the functional unit of the kidney, is also a classical epithelial/mesenchyme type of interaction.
The urinary system is developmentally and anatomically associated with genital development, often described as the urogenital system. Tomorrow's lecture will describe the associated genital development.
Lecture Objectives
- Understand the 3 main stages of kidney development.
- Understand development of the nephron and renal papilla.
- Brief understanding of the mechanisms of nephron development.
- Understand the development of the cloaca, ureter and bladder.
- Brief understanding of abnormalities of the urinary system.
Textbook References
- The Developing Human: Clinically Oriented Embryology (8th Edition) by Keith L. Moore and T.V.N Persaud - Moore & Persaud Chapter 13 p303-346
- Larsen’s Human Embryology by GC. Schoenwolf, SB. Bleyl, PR. Brauer and PH. Francis-West - Chapter 10 p261-306
- Lectopia Audio Lecture Date: 21-09-2009 Lecture Time: 12:00 Venue: CLB 5 Speaker: Mark Hill Renal
2008 Lecture: Lecture 11 | 1 slide/page viewing 48 pages | 4 slide/page printing 12 pages | 6 slide/page printing 8 pages
Background
- Mesoderm then intermediate mesoderm
- Vascular Development
- Gastrointestional
- Cloacal development
- Endocrine - covered in future lecture/lab
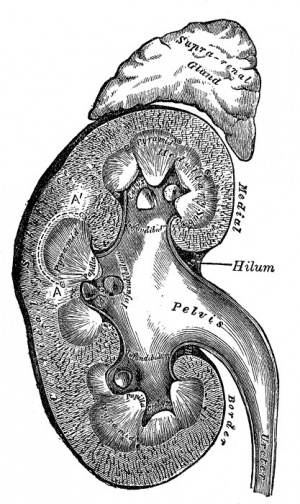
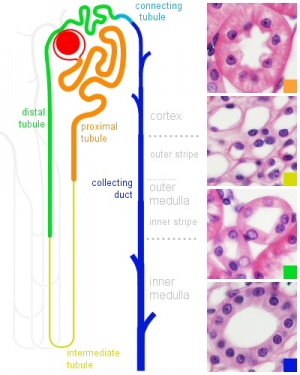
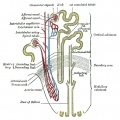
Kidney Anatomy
- Nephron - Functional unit of kidney
- Humans up to 1 million
- Filtration of waste from blood
- Endocrine
- Blood pressure regulation
Ureter
- Bladder - Urine storage
- Endoderm allantois
Mesoderm
- Intermediate mesoderm - Lies between somites and lateral plate Intermediate mesoderm
Cervical Nephrotomes, Mesonephros and Metanephros Movie
Intermediate Mesoderm
- development occurs laterally symmetrical (left right)
- intermediate mesoderm lying beside the dorsal aorta
- initially form mesonephric tubules (epithelial)
- these tubules connect to a common duct, mesonephric duct
- the mesonephric duct then extends within the mesoderm, rostro-caudally
- eventually making contact with the cloaca
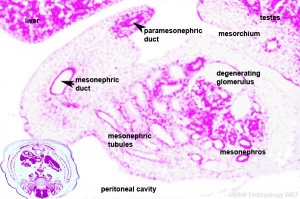
Mesonephric Duct
Later in development, both the mesonephric duct and the cloaca both continue to differentiate and undergo extensive remodelling (and renaming)
Uteric Bud
- arise near the cloacal connection of the mesonephric duct
- branch from the mesonephric duct laterally into the intermediate mesoderm
- induce the surrounding mesoderm to differentiate - metanephric blastema
- this mesoderm will in turn signal back to differentiate the uteric bud
Epithelial - mesenchymal interaction
Uteric Bud forms - ureter, pelvis, calyces, collecting ducts
Metanephric Blastema
- forms glomeruli, capsule, nephron tubules
- this development continues through fetal period
Nephros Development
- 3 pairs during development
- pronephros
- mesonephros
- metanephros
Pronephros
- week 4 few cells in cervical region fish
- Human E18, Mouse E7.5pronephric duct forms first with associated nephrogenic mesenchyme
- grows rostro caudally cervical -> cloaca
- E22 nephrogenic mesenchyme differentiates to form pronephroi not functional in mammals degenerates rapidly
Mesonephros
- Human E24, Mouse E9.5 caudal to pronephros
- forms by induction from pronephros
- pronephric duct now becomes mesonephric duct (also called Wolffian Duct)
Metanephros
- Human E35-37, Mouse E11 epithelia bud at end of mesonephric duct uteric bud and associated metanephric mesenchyme
Stage 13 3D movie | Stage 22 3D movie
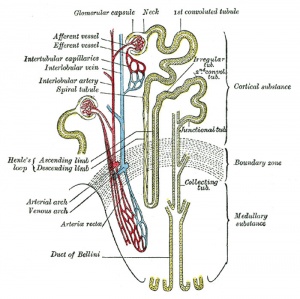
Uteric Bud
- induced by metanephric mesenchyme to differentiate
- forms collecting tubules, renal pelvis, ureter
- metanephric mesenchyme induced by uteric to differentiate forms nephron
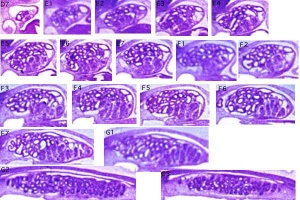
Nephron
Development has four developmental stages:
- vesicle (V) stage (13-19 weeks)
- S-shaped body (S) stage ( 20-24 weeks)
- capillary loop (C) stage (25-29 weeks)
- maturation (M) stage (infants aged 1-6 months)
- mean glomerular number shown to level at 36 weeks, increasing from about 15,000 at 15 weeks to 740,000 at 40 weeks.
Nephron Development
- disorganised mesenchymal cells become a highly organised epithelial tubule
- Condensation - groups of about 100 cells condense tightly together to form a distinct mass
- Epithelialisation - condensed cells lose their mesenchymal character and gain epithelial
- At end of this period formed a small epithelial cyst complete with a basement membrane, cell-cell junctions and a defined cellular apico-basal polarity.
Early morphogenesis
- cyst invaginates twice to form a comma
- then a S-shaped body one invagination site later becomes the glomerular cleft
- At about this time blood vessel progenitors invade cleft to begin construction of vascular component of glomerulus
- Tubule maturation specialised transporting segments of nephron differentiate complex of convoluted tubules is created
Endocrine Kidney
Covered also in Endocrine Development lecture
- Renin - Increase Angiotensin-aldosterone system
- Prostaglandins - decrease Na+ reabsorption
- Erythropoietin - Increase Erythrocyte (rbc) production
- 1,25 (OH)2 vitamin D - Calcium homeostasis
- Prekallikreins - (plasma protein inactive precursor of kallikrein) Increase kinin production (altered vascular permeability)
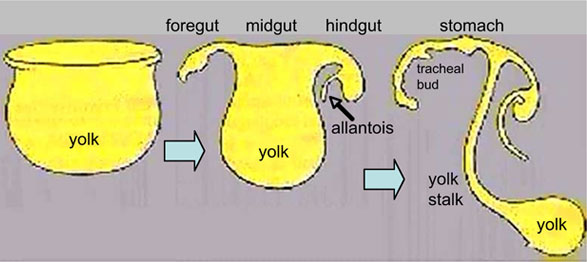
Cloaca
- hindgut region ending at the cloacal membrane
- divided (ventro-dorsally) by the urogenital septum
- ventral - common urogenital sinus
- dorsal - rectum
Common urogenital sinus
- superior end continuous with allantois
- common urogenital sinus and mesonephric duct fuse (connect)
- differentiates to form the bladder
- inferior end forms urethra
- this will be different in male and female development
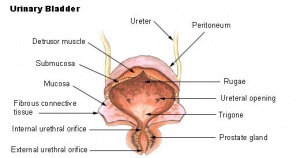
Urinary Bladder
- early origins of the bladder at the superior end of the common urogenital sinus
- 8 open inferiorly to the cloaca and superiorly to the allantois
- Septation of the claoca - divides the anterior region to the primordial bladder component from the posterior rectal component.
- associated ureters and urethra
Dorsal view of developing bladder
Trigone formation animation | small animation
- Ultrasound measurement of the bladder size can be used as a diagnostic tool for developmental abnormalities.
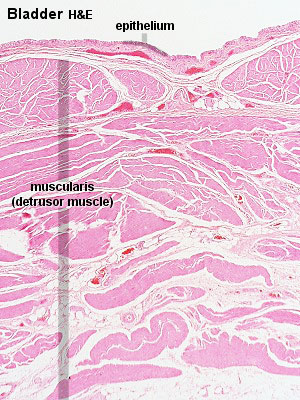
Bladder Structure
Can be described anatomically by its 4 layers from outside inward:
- Serous - the superior or abdominal surfaces and the lateral" surfaces of the bladder are covered by visceral peritoneum, the serous membrane (serosa) of the abdominal cavity, consisting of mesthelium and elastic fibrous connective tissue.
- Muscular - the detrusor muscle is the muscle of the urinary bladder wall.
- Submucosa - connects the muscular layer with the mucous layer.
- Mucosa - (mucus layer) a transitional epithelium layer formed into folds (rugae).
Detrusor Muscle
- The adult detrusor muscle consists of three layers of smooth (involuntary) muscle fibres.
- external layer - fibres arranged longitudinally
- middle layer - fibres arranged circularly
- internal layer - fibres arranged longitudinally
Ureter Development
- The adult ureter is a thick-walled muscular tube, 25 - 30 cm in length, running from the kidney to the urinary bladder.
- Anatomically can be described in two parts the abdominal part (pars abdominalis) and pelvic part (pars pelvina).
- The ureter is composed of three layers: outer fibrous layer (tunica adventitia), muscular layer (tunica muscularis) and mucous layer (tunica mucosa).
- The muscular layer can also be subdivided into 3 fibre layers: an external longitudinal, a middle circular, and an internal longitudinal.
Trigone Development
Kidney Ascent
- Pro-, Meso-, Meta- Early development descending
- Metanephros - initially pelvic, beside aorta
- Growth and straightening of body - Kidneys in abdomen and displace laterally
Renal Arteries
- Arise with ascent and inferior branches lost
- Sequential, 25% population have 2 or more renal arteries
- branch of abdominal aorta, divides into 4-5 branches
- each gives off small branches to suprarenal glands, ureter, surrounding cellular tissue and muscles
Note: Frequently a second renal artery (inferior renal) from abdominal aorta at a lower level, supplies lower portion of kidney
Abnormalities
Horseshoe Kidney
- fusion of the lower poles of the kidney.
- During migration from the sacral region the two metanephric blastemas can come into contact, mainly at the lower pole.
- The ureters pass in front of the zone of fusion of the kidneys.
- The kidneys and ureters usually function adequately but there is an increased incidence of upper urinary tract obstruction or infection.
- Some horseshoe variations have been described as having associated ureter abnormalities including duplications.
Urorectal Septum Malformation
- thought to be a deficiency in caudal mesoderm which in turn leads to the malformation of the urorectal septum and other structures in the pelvic region.
- Recent research has also identified the potential presence of a persistent urachus prior to septation of the cloaca (common urogenital sinus).
Bladder
- absent or small bladder -
associated with renal agenesis.
Bladder Exstrophy
- developmental abnormality associated with bladder development.
- origins appear to occur not just by abnormal bladder development, but by a congenital malformation of the ventral wall of abdomen (between umbilicus and pubic symphysis).
- There may also be other anomolies associated with failure of closure of abdominal wall and bladder (epispadias, pubic bone anomolies).
Ureter and Urethra
- Ureter - Duplex Ureter
- Urethra- Urethral Obstruction and Hypospadias
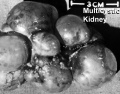
Polycystic Kidney Disease
- diffuse cystic malformation of both kidneys
- cystic malformations of liver and lung often associated, Often familial disposition
- Two types
- Infantile (inconsistent with prolonged survival)
- Adult (less severe and allows survival)
- Autosomal dominant PKD disease - recently identified at mutations in 2 different human genes encoding membrane proteins (possibly channels)
Wilms' Tumor
- (nephroblastoma) Named after Max Wilms, a German doctor who wrote first medical articles 1899
- most common type of kidney cancer children
- WT1 gene - encodes a zinc finger protein
- Both constitutional and somatic mutations disrupting the DNA-binding domain of WT1 result in a potentially dominant-negative phenotype
- some blastema cells (mass of undifferentiated cells) persist to form a ‘nephrogenic rest’
- Most rests become dormant or regress but others proliferate to form hyperplastic rests
- any type of rest can then undergo a genetic or epigenetic change to become a neoplastic rest
- can proliferate further to produce a benign lesion (adenomatous rest) or a malignant Wilms’ tumour
Prune Belly Syndrome
- lower urinary tract obstruction
- mainly male
- fetal urinary system ruptures leading to collapse and "prune belly" appearance.
Online Links
- UNSW Embryology Introduction | Nephron Development | Abnormalities | References | Stage13/14 | Stage 22 | Selected Human highpower | Genital | Genital Abnormalities | Urogenital Movies} | [http://embryology.med.unsw.edu.au/Notes/urogenlink.htm WWW Links
- UNSW Embryology Movies: Cervical Nephrotomes, Mesonephros and Metanephros (553Kb) | Development of the Renal Collecting System (298Kb) | Development of the Primitive Urogenital Sinus (476Kb) | Trigone (187Kb) | Male Gonadal Development (434 Kb) | Femal Gonadal Development (315Kb) | Formation of Uterus and Vagina (706Kb) | Male Genitalia Development (434 Kb) | Female Genitalia Development (357Kb) | Descent of the Testes (221Kb) | Movies
Movies
| Urogenital Sinus | Urogenital Septum | Trigone | Urogenital | Renal Nephron |
| Uterus | Female External | Male External | Testis Descent |
Images
References
Textbooks
- The Developing Human: Clinically Oriented Embryology (8th Edition) by Keith L. Moore and T.V.N Persaud - Moore & Persaud Chapter 13 p303-346
- Larsen’s Human Embryology by GC. Schoenwolf, SB. Bleyl, PR. Brauer and PH. Francis-West - Chapter 10 p261-306
- Before We Are Born (5th ed.) Moore and Persaud Chapter14 p289-326
- Essentials of Human Embryology, Larson Chapter 10 p173-205
- Human Embryology, Fitzgerald and Fitzgerald Chapter 21-22 p134-152
Online Textbooks
- Developmental Biology by Gilbert, Scott F. Sunderland (MA): Sinauer Associates, Inc.; c2000 Chapter 14 Intermediate Mesoderm | Figure 14.18. General scheme of development in the vertebrate kidney | Figure 23-23. Mechanism of mesenchymal inductive effect on the ureteric bud | Figure 14.21. Ureteric bud growth is dependent on GDNF and its receptor
- Molecular Cell Biology by Lodish, Harvey; Berk, Arnold; Zipursky, S. Lawrence; Matsudaira, Paul; Baltimore, David; Darnell, James E. New York: W. H. Freeman & Co.; c1999 Reciprocal Epithelial-Mesenchymal Interactions Regulate Kidney Development | Figure 23-21. Embryonic development of the kidney
Reviews
- Quaggin SE, Kreidberg JA. Development of the renal glomerulus: good neighbors and good fences. Development. 2008 Feb;135(4):609-20. PMID: 18184729
- Brenner-Anantharam A, Cebrian C, Guillaume R, Hurtado R, Sun TT, Herzlinger D. Tailbud-derived mesenchyme promotes urinary tract segmentation via BMP4 signaling. Development. 2007 May;134(10):1967-75. PMID: 17442697
- Forefronts Symposium on Nephrogenetics: from development to physiology March 8-11, 2007 Danvers, MA A meeting to synthesize an integrated view of the normal development and function of the kidney from the genetic standpoint.
- Costantini F. Renal branching morphogenesis: concepts, questions, and recent advances. Differentiation. 2006 Sep;74(7):402-21. PMID: 16916378
Search
- Bookshelf intermediate mesoderm | kidney development | renal development | ureteric bud | nephron development | bladder development
- Pubmed intermediate mesoderm | kidney development | renal development | ureteric bud | nephron development | bladder development
Terms
bladder exstrophy - A congenital malformation with bladder open to ventral wall of abdomen (between umbilicus and pubic symphysis) and may have other anomolies associated with failure of closure of abdominal wall and bladder (epispadias, pubic bone anomolies).
blastema - Term used to describe a mass of undifferentiated cells. (More? [#Wilms_tumour Wilm's tumour])
diabetes insipidus - The disorder is related to the hormone antidiuretic hormone (ADH, also called vasopressin) its synthesis, secretion, receptors and signaling pathway. In diabetes insipidus there is an excretion of large amounts (up to 30 litres/day) of a watery urine and an unremitting thirst (More? [urogen2.htm#Diabetes_Insipidus Kidney Abnormalities - Diabetes Insipidus])
hydronephrosis - (congenital hydronephrosis, Greek, hydro = water) A kidney abnormality due to partial or complete obstruction at the pelvi-ureteric junction. This leads to a grossly dilated renal pelvis causing extensive renal damage before birth.
hyperplastic rests - In kidney development, embryonic blastema cells can persist and proliferate to form a pool of cells, which under either genetic or epigenetic influence can then change to become a neoplastic rest. Normally the majority of nephrogenic rests either regress or become dormant.
mesonephros - The second temporary stage of kidney development (pro-, meso-, meta-). The intermediate mesonephros develops and disappears with the exception of its duct, the mesonephric duct, which will form the male reproductive duct system. In males, the mesonephric tubules go on to form the ducts of the testis. In females, these degenerate. A few mesonephric tubules remain as efferent ductules in the male and vestigial remnants in the female.
mesonephric duct - (= Wollfian duct) An early developing urogenital duct running the length of the embryo that will differentiate and form the male reproductive duct system. In females this duct degenerates (some remnants may remain associated in broad ligament).
metanephros - The adult kidney, third stage of mammalian kidney (pro-, meso-, meta-) development within the intermediate mesoderm.
metanephric cap - In kidney development, the intermediate mesoderm which surrounds the ureteric bud and will develop into nephrons.
Multicystic Kidney - There is no functional kidney tissue present in the kidney and it is replaced by a multilocular cyst. This is non-familial and is produced by atresia of a ureter and is always unilateral.
neoplastic rest - In kidney development, a neoplastic rest can develop under either genetic or epigenetic influence from a hyperplastic rest, originating from an embryonic blastema cell. Normally the majority of nephrogenic rests either regress or become dormant.
nephrogenic rest - A kidney term used to describe the embryonic blastema cells which persist and under either genetic or epigenetic can change to become a neoplastic rest. These neoplastic rests can develop postnatally as a benign form (adenomatous rest) or a malignant [W.htm#Wilms_tumour Wilm's tumour] form. The rests are further characterised by the time of generation leading to different anatomical kidney locations: early intralobar nephrogenic rests (within the renal lobe) and late pelilobar nephrogenic rests (periphery of the renal lobe) (More? [#Wilms_tumour Wilm's tumour] | [urogen2.htm Urogenital Abnormalities])
nephron - (Greek, nephros = kidney) The functional unit of the kidney.
nephros - (Greek, nephros = kidney) Term used to describe features associated with the kidney. (pronephros, mesonephros, metanephros, nephric, nephron, nephroblastoma).
podocyte - (visceral epithelial cell) kidney glomerulus cell forming the main component of the glomerular filtration barrier.
podocyte specific proteins - podocalyxin, glomerular epithelial protein-1, podocin, nephrin, synaptopodin, and alpha-actinin-4), podocyte synthesized proteins (vascular endothelial growth factor and novH), transcription factors (WT1 and PAX2).
pronephros - (Greek, pro = before) The first temporary stage of kidney development (pro-, meso-, meta-). This forms the kidney of primitive fish and lower vertebrates. Kidney development occurs within the intermediate mesoderm interacting with endoderm. In humans, this very rudimentary kidney forms very early at the level of the neck. It is rapidly replaced by the mesonephros, intermediate stage kidney, differentiating in mesoderm beneath.
proteinuria - The abnormal presence of protein in the urine and an indicator of diesease including diabetic kidney disease (DKD, diabetic nephropathy).
renal - (Latin, renes = kidney) Term used in relation to the kidney and associated structures (renal pelvis, renal artery)
ureter - The two ureters are hollow tubes that link and carries urine from kidney to the bladder. The tubes have a muscular wall lined with transitional epithelium.
urethra - The single muscular tube that links and carries urine from the bladder to the exterior. In humans, the urethral length differs between the sexes (male longer, female shorter).
urinary - Term used to describe all components of the kidney system including the bladder, ureters and urethra.
urine - Term used to describe the liquid waste produced by the kidney, stored in the bladder and excreted from teh body through the urethra.
urorectal septum - (URS) The structure which develops to separate the cloaca (common urogenital sinus) into an anterior urinary part and a posterior rectal part.
Wilms' tumour - A form of kidney/renal cancer (nephroblastoma) named after Dr Max Wilms who first described the tumor. This childhood kidney cancer is caused by the inactivation of a tumour suppressor gene (BRCA2) or Wilms tumor-1 gene (Wt1) and is one of the most common solid tumors of childhood, occurring in 1 in 10,000 children and accounting for 8% of childhood cancers. Wt1 also required at early stages of gonadal development. (More? [urogen2.htm Kidney Abnormal Development] | OMIM - Wilm's tumour | Dr Max Wilms)
Wilms' tumor 1-associating protein - (WTAP) protein expressed in extraembryonic tissues and required for the formation of embryonic mesoderm and endoderm.
Wolffian duct - (= mesonephric duct, preferred terminology), runs from the mesonephros to cloaca, differentiates to form the male vas deferens and in the female regresses. Named after Caspar Friedrich Wolff (1733-1794), a German scientist and early embryology researcher and is said to have established the doctrine of germ layers. (More? Caspar Friedrich Wolff)
Glossary Links
- Glossary: A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | Numbers | Symbols | Term Link
Course Content 2009
Embryology Introduction | Cell Division/Fertilization | Cell Division/Fertilization | Week 1&2 Development | Week 3 Development | Lab 2 | Mesoderm Development | Ectoderm, Early Neural, Neural Crest | Lab 3 | Early Vascular Development | Placenta | Lab 4 | Endoderm, Early Gastrointestinal | Respiratory Development | Lab 5 | Head Development | Neural Crest Development | Lab 6 | Musculoskeletal Development | Limb Development | Lab 7 | Kidney | Genital | Lab 8 | Sensory - Ear | Integumentary | Lab 9 | Sensory - Eye | Endocrine | Lab 10 | Late Vascular Development | Fetal | Lab 11 | Birth, Postnatal | Revision | Lab 12 | Lecture Audio | Course Timetable
Cite this page: Hill, M.A. (2026, February 27) Embryology 2009 Lecture 15. Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/2009_Lecture_15
- © Dr Mark Hill 2026, UNSW Embryology ISBN: 978 0 7334 2609 4 - UNSW CRICOS Provider Code No. 00098G