ANAT2341 Lab 4 - Decidua and Cord
| ANAT2341 Lab 4: Introduction | Implantation and Villi | Decidua and Cord | Abnormal Placenta | Cardiovascular | Online Assessment | Group Project |
Uterus
Human placenta classified as Haemochorial where the chorion comes in direct contact with maternal blood.
Menstrual Changes
- Endometrium - 3 layers in secretory phase of menstrual cycle: compact, spongy, basal
- Myometrium - muscular layer outside endometrium, contracts in parturition
- Perimetrium - tunica serosa of the uterus continuous with the peritoneal wall
Endometrial Layers
- Compact - implantation occurs in this layer, dense stromal cells, uterine gland necks, capillaries of spiral arteries.
- Spongy - swollen stromal cells, uterine gland bodies, spiral arteries.
- Basal - not lost during menstruation or childbirth, own blood supply.
Uterine glands
- still well-developed and highly active at 6 weeks (GA).
- gradually regress in length and epithelium height as the first trimester advances.
Decidual Reaction
Process (decidualization) of endometrial stromal cells (fibroblast-like) change in morphology (polygonal cells) and protein expression and secretion.
- occurs initially at site of implantation and includes both cellular and matrix changes
- reaction spreads throughout entire uterus, not at cervix
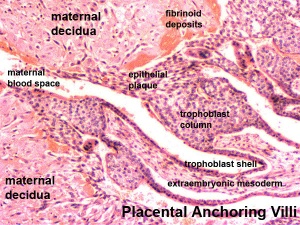
- deposition of fibrinoid and glycogen and epithelial plaque formation (at anchoring villi)
- presence of decidual cells are indicative of pregnancy
Fibrinoid layer - (Nitabuch's layer) is thought to act to prevent excessively deep implantation.
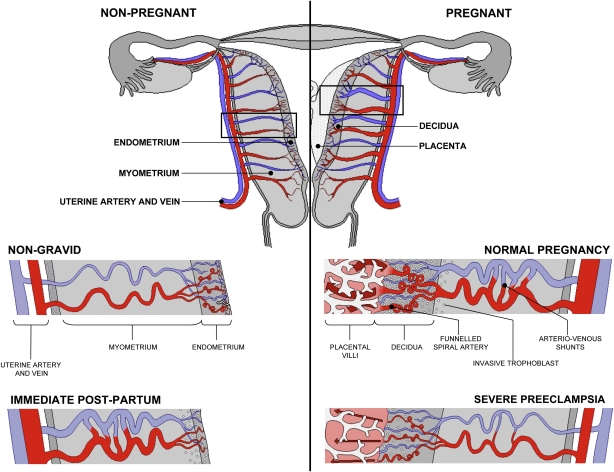
Artery Dilatation - due to extravillous trophoblast cells invading uterine wall and maternal spiral arteries replacing both smooth muscle with fibrinoid material and part of vessel endothelium. There is also a proliferation of maternal blood vessels.
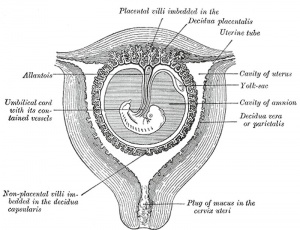
Cervix - at mouth of uterus, secretes mucus (CMP), forms a plug/barrier, mechanical and antibacterial.
Decidua
The endometrium becomes the decidua and forms 3 distinct anatomical regions (at approx 3 weeks)
- Decidua Basalis at implantation site
- Decidua Capsularis enclosing the conceptus
- Decidua Parietalis the remainder of uterus
- Decidua Capsularis and Parietalis fuse eventually fuse and uterine cavity is lost by 12 weeks
- decidua capsularis then degenerates
Fibrinoid
Exist as 2 forms of extracellular matrix:
- Fibrin-type fibrinoid is a maternal blood-clot product which replaces degenerative syncytiotrophoblast
- Matrix-type fibrinoid is secreted by invasive extravillous trophoblast cells.
Fibrinoid layer (Nitabuch's layer) is thought to act to prevent excessively deep implantation.
Decidualization
Process of endometrial stromal cells (fibroblast-like) change in morphology (polygonal cells) and protein expression and secretion (specific decidual proteins: prolactin, insulin-like growth factor binding protein-1, tissue factor, interleukin-15, and VEGF).
- Estrogen and progesterone - receptive phase, luminal and glandular epithelial cells change in preparation for blastocyst adplantation.
- Human Chorionic gonadotropin - luminal epithelium endoreplication leading to epithelial plaque formation.
- Human Chorionic gonadotropin - trophoblast invasion and decidualization of human stromal fibroblasts.
Maternal Blood Vessels
Artery Dilatation - Due to extravillous trophoblast cells invading uterine wall and maternal spiral arteries replacing both smooth muscle with fibrinoid material and part of vessel endothelium. There is also a proliferation of maternal blood vessels.
Uterine and Placental Vasculature in Non-pregnant, Pregnant and immediate Post-partum State
Diagrammatic representation of uterine and placental vasculature (red shading = arterial; blue shading = venous) in the non-pregnant, pregnant and immediate post-partum state.
- Normal pregnancy is characterized by the formation of large arterio-venous shunts that persist in the immediate post-partum period.
- Extravillous cytotrophoblast invasion in normal pregnancy (diamonds) extends beyond the decidua into the inner myometrium resulting in the formation of funnels at the discharging tips of the spiral arteries.
- Pregnancies complicated by severe preeclampsia are characterized by minimal arterio-venous shunts, and thus narrower uterine arteries.
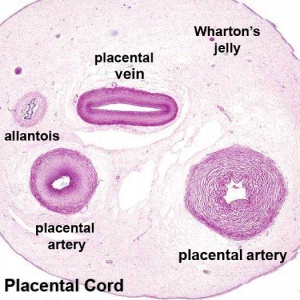
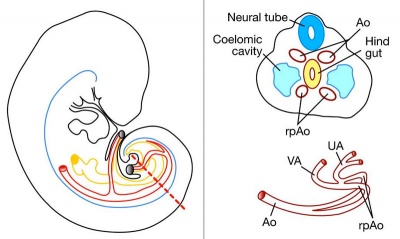
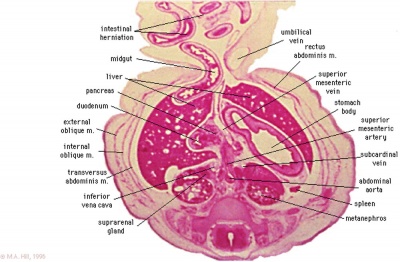
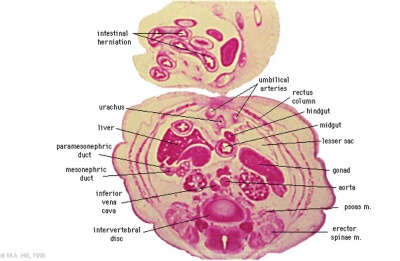
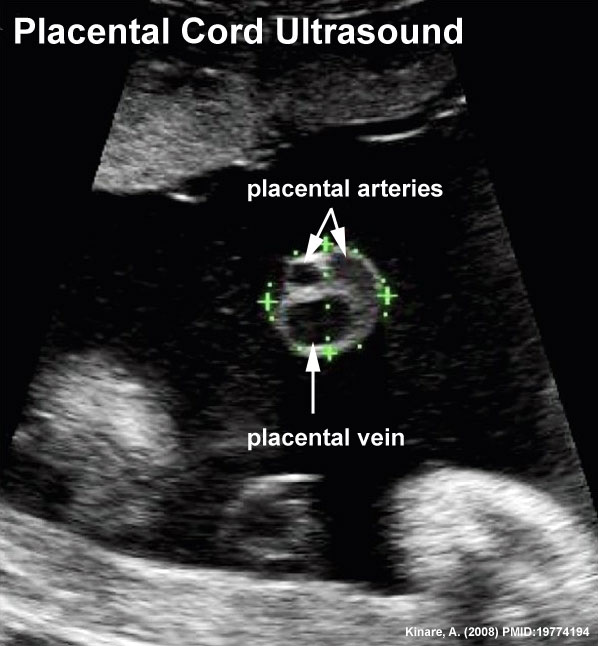
Placental Cord
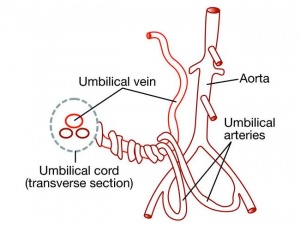
The placental cord (umbilical cord) is the connecting region between the functional placenta and the embryo/fetal umbilical region. The human cord varies physically in overall length, increasing to about 60 to 70 cm at term, degree of coiling, number of vessels and insertion site on the placenta. This extraembryonic structure contains the placental blood vessels and allantois.
Normally a pair of placental arteries are wrapped around a single (left) placental vein. A persistent right umbilical vein is thought to be a rare anomaly.
Placental Arteries and Vein
Week 8
Cord Histology
Virtual Slide - Virtual Slides - Placenta Please note that there are additional slides listed in the current set, only the first placenta slide and the cord cross-section will be covered in detail in the practical class.
Ultrasound image of transverse scan through the cord show the method of estimation of the cross-sectional area.
Wharton's Jelly
- placental cord connective tissue (substantia gelatinea funiculi umbilicalis)
- amorphous substance containing glycosaminoglycans, proteoglycans and hyaluronic acid.
- cells similar to smooth muscle that allows a contractile function.
- network of collagen that form canaliculi and perivascular spaces.
- maintain blood flow to the fetus during placental cord compression during pregnancy or delivery.
First described and named after Thomas Wharton (1614–1673) an English physician and anatomist.
Hofbauer Cells
- located the core of placental villi
- macrophages with micropinocytotic activity and phagocytosis ability
- possible paracrine role for early stages of placental vasculogenesis
- express angiogenic growth factors (VEGF)
Cord Length
The following are lengths and classifications at term.
- Normal range - 50 to 60 cm.
- Short cord - less than 35 cm.
- Long cords - over 70 cm can be associated with wrapping around the fetus and other abnormalities.
| ANAT2341 Lab 4: Introduction | Implantation and Villi | Decidua and Cord | Abnormal Placenta | Cardiovascular | Online Assessment | Group Project |
Additional Information
Other changes
- Endoreplication - rounds of nuclear DNA replication without intervening cell or nuclear division (mitosis).
- Cytokines - of maternal origin also act on placental development.
- Natural Killer (NK) cells - 30% of all the decidual cells towards the end of the first trimester of pregnancy. These lymphocytes are present in the maternal decidua in large numbers (70%, normal circulating blood lymphocytes 15%) close to the extravillous trophoblast cells. Have a cytolytic potential against virus-infected and tumor-transformed cells.
Historic Drawings
Placental Classification
Classification of placenta is on the basis of histological (microscopic) structural organization and layers between fetal and maternal circulation.
Three main groups:
- Haemochorial - placenta where the chorion comes in direct contact with maternal blood (human).
- Endotheliochorial - maternal endometrial blood vessels are bare to their endothelium and these comes in contact with the chorion (dogs, cats).
- Epitheliochorial - maternal epithelium of the uterus comes in contact with the chorion, considered as primitive (pigs, cows).
The presence of these three differing types of placenta have also been used to describe the pattern mammalian evolution.
Preeclampsia
- Preeclampsia - describes maternal high blood pressure and protein in the urine after the 20th week (GA) late 2nd or 3rd trimester of pregnancy. This may be due to factors from the placenta.
- Eclampsia - seizures (convulsions) in a pregnant woman that are not related to a preexisting brain condition.
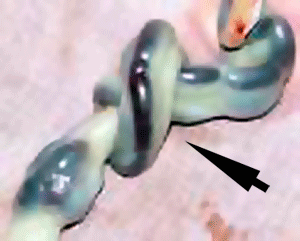
Cord Coiling
- Hypocoiling - associated with increased incidence of fetal demise, intrapartum fetal heart rate decelerations, operative delivery for fetal distress, anatomic-karyotypic abnormalities and chorio-amnionitis.
- Hypercoiling - associated with increased incidence of fetal growth restriction, intrapartum fetal heart rate decelerations, vascular thrombosis and cord stenosis.
Vessel Anomalies
- Fetal intra-abdominal umbilical vein varix is a focal dilatation of the intra-abdominal portion of the umbilical vein.
Persistent Right Umbilical Vein
A study of 15,237 obstetric ultrasound examinations performed after 15 weeks' gestation identified only 33 cases of persistent right umbilical vein.
<pubmed>7970470</pubmed>
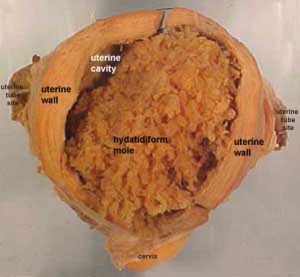
Hydatidiform Mole
Another type of abnormality is when only the conceptus trophoblast layers proliferates and not the embryoblast, no embryo develops, this is called a "hydatidiform mole" (HM), which is due to the continuing presence of the trophoblastic layer, this abnormal conceptus can also implant in the uterus. The trophoblast cells will secrete human chorionic gonadotropin (hCG), as in a normal pregnancy, and may appear maternally and by pregnancy test to be "normal". Prenatal diagnosis by ultrasound analysis demonstrates the absence of a embryo.
There are several forms of hydatidiform mole: partial mole, complete mole and persistent gestational trophoblastic tumor.
- Complete Mole - Only paternal chromosomes, chromosomal genetic material from the ovum (egg) is lost, by an unknown process.
- Partial Mole - Ultrasound of partial mole confirmed by triploidy, chromosomal (genetic) material from the ovum (egg) is retained and the egg is fertilized by one or two sperm.
On ultrasound the tumour has a "grape-like" placental appearance without enclosed embryo formation. Following a first molar pregnancy, there is approximately a 1% risk of a second molar pregnancy.
- The incidence of hydatidiform mole varies between ethnic groups, and typically occurs in 1 in every 1500 pregnancies.
- All hydatidiform mole cases are sporadic, except for extremely rare familial cases.
- Links: Hydatidiform Mole | Week 2 - Abnormalities
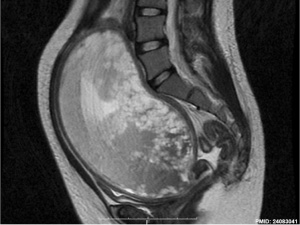
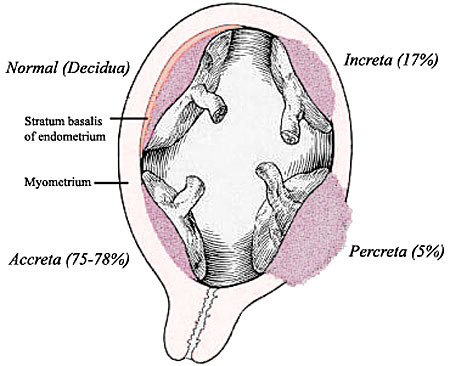
Implantation Abnormalities
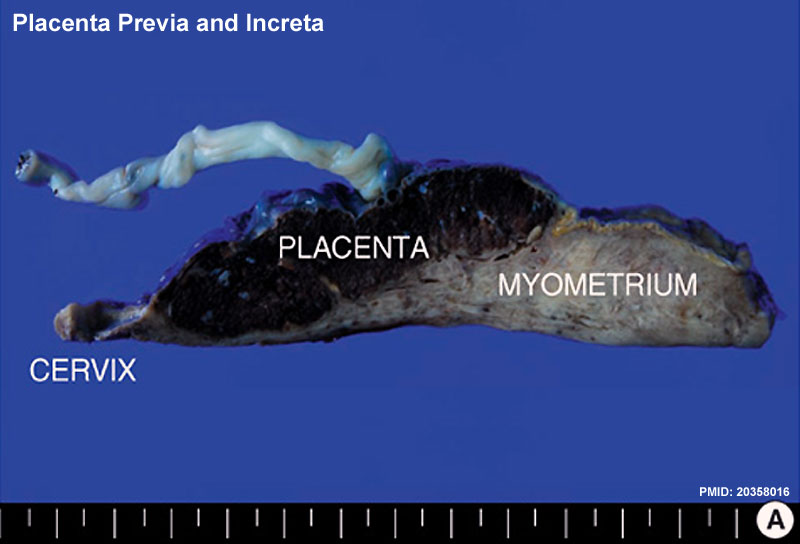
Placenta previa and increta
The placenta is a mateno-fetal organ which begins developing at implantation of the blastocyst and is delivered with the fetus at birth. As the fetus relies on the placenta for not only nutrition, but many other developmentally essential functions, the correct development of the placenta is important to correct embryonic and fetal development.
Abnormalities can range from anatomical associated with degree or site of inplantation, structure (as with twinning), to placental function, placento-maternal effects (pre-eclampsia, fetal erythroblastosis) and finally mechanical abnormalities associated with the placental (umbilical) cord.
- Placenta Accreta - abnormal adherence, with absence of decidua basalis. The incidence of placenta accreta also significantly increases in women with previous cesarean section compared to those without a prior surgical delivery.
- Placenta Increta - occurs when the placenta attaches deep into the uterine wall and penetrates into the uterine muscle, but does not penetrate the uterine serosa. Placenta increta accounts for approximately 15-17% of all cases.
- Placenta Percreta - placental villi penetrate myometrium and through to uterine serosa.
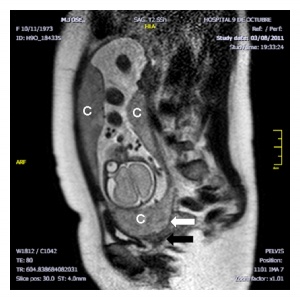
- Placenta Previa - In this placenatal abnormality, the placenta overlies internal os of uterus, essentially covering the birth canal. This condition occurs in approximately 1 in 200 to 250 pregnancies. In the third trimester and at term, abnormal bleeding can require cesarian delivery and can also lead to Abruptio Placenta. Ultrasound screening programs during 1st and early 2nd trimester pregnancies now include placental localization. Diagnosis can also be made by transvaginal ultrasound.
- Vasa Previa - (vasa praevia) placental abnormality where the fetal vessels lie within the membranes close too or crossing the inner cervical os (opening). Two main associations; 1. velamentous insertions (25–62%) and 2. vessels crossing between lobes in succenturiate or bilobate placentas (33–75%)
- Multilobed Placenta Succenturiata - an accessory portion attached to the main placenta by an artery or vein.
- Abruptio Placenta - a retroplacental blood clot formation, abnormal haemorrhage prior to delivery.
- Chronic Intervillositis - (massive chronicintervillositis, chronic histiocytic intervillositis) Rare placental abnormality and pathology defined by inflammatory placental lesions, mainly in the intervillous space (IVS), with a maternal infiltrate of mononuclear cells (monocytes, lymphocytes, histiocytes) and intervillous fibrinoid deposition.
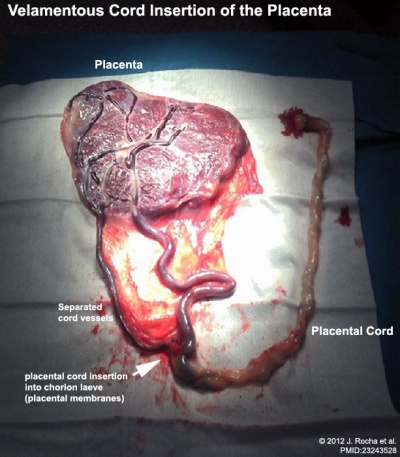
Cord Abnormalities
|
Velamentous Cord Insertion of the PlacentaThe placental cord inserts into the chorion laeve (placental membranes) away from the edge of the placenta.[1]
The placental vessels are therefore unprotected by Wharton's jelly where they traverse the membranes before they come together into the umbilical cord.
This can also be associated with vasa previa (see above) or haemorrhage caused if the vessels are damaged when the membranes are ruptured prior to birth. The condition is more common in monozygotic twins (15%) and triplets. |
Cord Length
Excessively short or long cords (see additional information on cord page). Abnormally long cords may wrap around either extremities or neck of the fetus.
Cord Vessel Number
Cord with only one artery and one vein.
Cord Knotting
Cord knotting can occur (1%) in most cases these knots have no effect, in some cases of severe knotting this can prevents the passage of placental blood.
Umbilical cord torsion
Rare umbilical cord torsion, even without knot formation can also affect placental blood flow, even leading to fetal demise.
| ANAT2341 Lab 4: Introduction | Implantation and Villi | Decidua and Cord | Abnormal Placenta | Cardiovascular | Online Assessment | Group Project |
- 2014 Course: Week 2 Lecture 1 Lecture 2 Lab 1 | Week 3 Lecture 3 Lecture 4 Lab 2 | Week 4 Lecture 5 Lecture 6 Lab 3 | Week 5 Lecture 7 Lecture 8 Lab 4 | Week 6 Lecture 9 Lecture 10 Lab 5 | Week 7 Lecture 11 Lecture 12 Lab 6 | Week 8 Lecture 13 Lecture 14 Lab 7 | Week 9 Lecture 15 Lecture 16 Lab 8 | Week 10 Lecture 17 Lecture 18 Lab 9 | Week 11 Lecture 19 Lecture 20 Lab 10 | Week 12 Lecture 21 Lecture 22 Lab 11 | Week 13 Lecture 23 Lecture 24 Lab 12
Student Projects - Group 1 | Group 2 | Group 3 | Group 4 | Group 5 | Group 6 | Group 7 | Group 8 | Moodle
- ↑ <pubmed>23243528 </pubmed>| PMC3517836 | Case Rep Obstet Gynecol.