2010 BGD Tutorial - Applied Embryology and Teratology: Difference between revisions
| Line 78: | Line 78: | ||
====Gestational age==== | ====Gestational age==== | ||
* '''90.9%''' term (37–41 weeks gestation) | * '''90.9%''' term (37–41 weeks gestation) | ||
* 8.1% were preterm | * 8.1% were preterm and '''33.2 weeks''' was the mean gestational age for all preterm births | ||
** Preterm births were classified groups of 20–27 weeks, 28–31 weeks and 32–36 weeks | ** Preterm births were classified groups of 20–27 weeks, 28–31 weeks and 32–36 weeks | ||
Revision as of 12:49, 25 January 2010
Introduction
This Medicine Phase 2 tutorial introduces the topics of Applied Embryology and Teratology. This one and a half hour presentation uses your existing knowledge of normal human development in an applied clinical manner in relation to our existing knowledge of teratogens. In addition, you should begin considering the variables that will not change and those that will in future medical practice.
Due to time limitations, only a brief coverage can be given of any one topic. You should return here and later work through the linked online resources for a more detailed description and understanding of these issues.
The same content is covered in the previous online 2008 Tutorial - Applied Embryology and Teratology (Royal Hospital for Women)
Objectives
Applied Embryology: timeline of development, birth statistics, abnormalities statistics, unintended pregnancies, trophoblastic disease, embryonic development, placenta, fetal development, folic acid, multiple pregnancies.
Teratology: definitions, critical periods, medications, chromosomal abnormalities, environmental factors and infections.
Textbook Reading: Human Embryology, WJ. Larsen; The Developing Human: Clinically Oriented Embryology. Moore & Persaud
Original Tutorial Handout: Tutorial Applied Embryology and Teratogenicity (8 pages, PDF document)
Applied Embryology
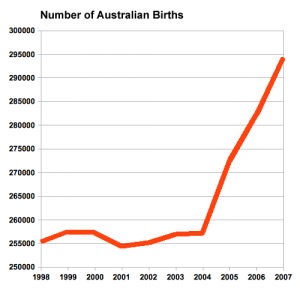
This data Australia's mothers and babies 2007 summarised below is provided to help you as a clinician or researcher understand the current trends in reproductive medicine within Australia.
The information is based upon data from the publication Laws P & Sullivan EA 2009. Australia’s mothers and babies 2007. Perinatal statistics series no. 23. Cat. no. PER 48. Sydney: AIHW National Perinatal Statistics Unit and is provided for educational purposes only. The original full publication is available online from AIHW Perinatal statistics series no. 23.
Mothers
- 289,496 women gave birth resulting in a total of 294,205 births
- increase of 4.3% from 2006, and 14.4% increase since 2004
- 2,177 were fetal deaths
- 29.9 years was the maternal mean age in 2007
- compared with 28.9 years in 1998
- 41.6% of mothers had their first baby and 33.5% had their second baby
- 10,883 women were Aboriginal or Torres Strait Islander (3.8% of all women who gave birth)
- 39.5% of all mothers in the Northern Territory
- 25.2 years was the average age of women who gave birth
Assisted reproduction technology
- 3.1% women received ART treatment
- ranging from 1.4% in the Australian Capital Territory to 3.7% in Tasmania
- 34.1 years was the average age of women who received ART
- 62.7% of mothers who received ART treatment were having their first baby and 37.3% had given birth previously
Smoking during pregnancy
- 16.6% of women smoked during pregnancy (similar proportion over the previous five years)
Preterm birth
- 7.4% of all mothers (less than 37 completed weeks of gestation)
- 38.8 weeks is the average duration of pregnancy
Multiple pregnancy
- 4,634 multiple pregnancies (1.6% of all mothers) increasing due to the increased use of ART
- 4,558 twin pregnancies, 76 triplet pregnancies and no quadruplet pregnancies
Presentation at birth
- 94.6% cephalic (any part vertex, face, or brow of the fetal head)
- 4.0% breech (buttocks or feet)
Method of birth
- 57.9% vaginal births
- 11.2% had an instrumental vaginal delivery (forceps or vacuum extraction)
- 30.9% caesarean section births
- 21.1% in 1998, 30.8% in 2006, rate recently stable
- 83.3% of these were repeat caesarean sections
- epilepsy, diabetes mellitus and hypertension, antepartum haemorrhage, gestational diabetes, cord prolapse and retained placenta, pregnancy-induced hypertension, fetal distress in labour and post-partum haemorrhage rates
Postnatal length of stay
- 2.0 days non-instrumental vaginal birth
- 3.0 days vacuum extraction delivery
- 4.0 days caesarean section or forceps delivery
Babies
- 292,027 live births and 2,177 fetal deaths
- stillbirth rate of 7.4 per 1,000 births
- most births occurred in March, August and October
- 105.6 sex ratio (number of male per 100 female liveborn babies)
Gestational age
- 90.9% term (37–41 weeks gestation)
- 8.1% were preterm and 33.2 weeks was the mean gestational age for all preterm births
- Preterm births were classified groups of 20–27 weeks, 28–31 weeks and 32–36 weeks
Birthweight
- 92.1% of liveborn babies had a birthweight in the range 2,500–4,499 grams
- average birthweight was 3,374 grams
- 17,976 (6.2%) low birthweight (weighing less than 2,500 grams)
- 2,956 (1.0%) very low birthweight (weighing less than 1,500 grams)
- 1,288 (0.4%) extremely low birthweight (weighing less than 1,000 grams)
Apgar scores - 1.4% of liveborn babies had a low Apgar score (between 0 and 6) at 5 minutes
Special care nurseries or neonatal intensive care units - 14.5% of liveborn babies were admitted to an SCN or NICU
Perinatal mortality
- 2,177 fetal deaths (7.4 per 1,000 births)
- fetal deaths are if the birthweight is at least 400 grams or the gestational age is 20 weeks or more
- 846 neonatal deaths (2.9 per 1,000 live births)
- neonatal deaths are those occurring in live births up to 28 completed days after birth
- 3,024 perinatal deaths
- perinatal death includes birthweight of at least 400 grams or, where birthweight is unknown, a gestational age of at least 20 weeks
- 23.5% congenital abnormalities (anomalies)
- 13.8% maternal conditions
- 12.6% unexplained antepartum death
Applied Embryology Links: Normal Development- Statistics | Normal Development- Australian Statistics | World Infant Health Statistics | Abnormal Development - Australian Congenital Malformations Classifications
Unintended Pregnancy
1995 USA National Survey of Family Growth (NSFG)
- 49% of pregnancies in the USA (excluding miscarriages)
- 31% of pregnancies resulting in a live birth are unintended
Unintended pregnancy is either
- mistimed (woman wanted to be pregnant later)
- unwanted (did not want to ever be pregnant)
(Reference: Pregnancy Risk Assessment Monitoring System USA)
Assisted Reproduction Technology
Assisted Reproduction Technology (ART) may include more techniques than, but is sometimes also used to identify, In vitro Fertilization (IVF) (More? In Vitro Fertilization).
- 51,017 treatment cycles reported to ANZARD in Australia and New Zealand in 2005.
- 91.1% were from Australian fertility centres
- 8.9% from New Zealand’s centres
- an increase of 13.7% of ART treatment cycles from 2004.
- 35.5 years average age of women (35.2 years in 2002).
- Women aged older than 40 years has increased from 14.3% in 2002 to 15.3% in 2005.
Single Embryo Transfers (SET)
- Significant increase in the number of SET embryos transfer cycles
- 2002 28.4%
- 2005 48.3%
- increase of SET cycles resulted more singleton deliveries (singleton deliveries 2005 was 85.9%)
- single-embryo transfer babies had better outcomes compared to babies born to women who had a double-embryo transfer (DET).
- 2005 3,681 SET babies and 5,589 DET babies.
- Singletons babies
- 96.1% SET
- 61.6% DET
- Preterm babies
- 11.7% SET
- 30.6% DET
- Low birthweight liveborn babies
- 8.0% SET
- 25.0% DET
Perinatal mortality rate is a measure of perinatal outcomes.
- 2005, for all babies born following ART treatment
- perinatal mortality rate was 14.7 deaths per 1,000 births
- 23.8% decrease from 19.3 deaths per 1,000 births in 2004
- Perinatal mortality rate was the lowest among singletons born following SET (7.3 deaths per 1,000 births) in 2005.
(Reference: AIHW National Perinatal Statistics Unit Assisted Reproduction Technology in Australia and New Zealand 2005)
Australian Birth Anomalies System
"The national collation and reporting of birth anomalies data has been suspended in recent years due to concerns about data quality and comparability."
- Variability among states and territories in scope of birth anomalies data collections
- sources of birth anomalies notifications
- definitions and classifications used
- method of data collection
- available resources
- Variability among the states and territories in the timing and method of the provision of birth anomalies data to the AIHW National Perinatal Statistics Unit (NPSU) for national collation and reporting.
- New Australian Birth Anomalies System should be data for birth anomalies detected up to 1 year of age
- including data on terminations of pregnancies with birth anomalies
- regardless of gestational age (i.e. including less than 20 weeks gestation)
- System will initially be based on data from the states able to detect birth anomalies at least up to 1 year of age
- NSW, VIC, WA and SA
- further extending the period of detection in the future
(Reference: modified from AIHW Website)
Ten most frequently reported birth Defects
- (Data from the Victorian Perinatal Data Collection Unit in Victoria between 2003-2004)
- Hypospadias (More? Genital Abnormalities - Hypospadia)
- Obstructive Defects of the Renal Pelvis (More? Urogenital Abnormalities)
- Ventricular Septal Defect (More? Cardiovascular Abnormalities - Ventricular Septal Defect)
- Congenital Dislocated Hip (More? Musculoskelal Abnormalities - Congenital Dislocation of the Hip (CDH))
- Trisomy 21 or Down syndrome - (More? Abnormal Development - Trisomy 21)
- Hydrocephalus (More? Neural Abnormalities - Hydrocephalus)
- Cleft Palate (More? Head Abnormalities)
- Trisomy 18 or Edward Syndrome - multiple abnormalities of the heart, diaphragm, lungs, kidneys, ureters and palate 86% discontinued (More? Abnormal Development - Trisomy 18)
- Renal Agenesis/Dysgenesis - reduction in neonatal death and stillbirth since 1993 may be due to the more severe cases being identified in utero and being represented amongst the increased proportion of terminations (approximately 31%). (More? Kidney Abnormalities - Renal Agenesis)
- Cleft Lip and Palate - occur with another defect in 33.7% of cases. (More? Head Abnormalities)
Links: Australian Birth Anomalies | Australian Anomalies Classification | Abnormal Development - Australian Statistics - Victoria |
Abnormal Development
There are many different ways that developmental abnormalities can occur the 3 major types are Genetic (inherited), Environmental (maternal) derived and Unknown (not determined or known) abnormalities. Often not considered, is that pregnancy itself can also expose abnormalities in the mother (congenital heart disease, diabetes, reproductive disorders) that until pregnancy had gone undetected.
Teratology Links: Abnormal | [images/hcriticaldev.gif Critical Periods of Development]
Teratology
Now consider how different environmental effects during the pregnancy may influence outcomes.
Teratogen (Greek, teraton = monster) any agent that causes a structural abnormality (congenital abnormalities) following fetal exposure during pregnancy. The overall effect depends on dosage and time of exposure. (More? [images/hcriticaldev.gif Critical Periods of Development])
Absolute risk the rate of occurrence of an abnormal phenotype among individuals exposed to the agent. (e.g. fetal alcohol syndrome)
Relative risk the ratio of the rate of the condition among the exposed and the nonexposed. (e.g. smokers risk of having a low birth weight baby compared to non-smokers) A high relative risk may indicate a low absolute risk if the condition is rare.
Mutagen a chemical or agent that can cause permanent damage to the deoxyribonucleic acid (DNA) in a cell. DNA damage in the human egg or sperm may lead to reduced fertility, spontaneous abortion (miscarriage), birth defects and heritable diseases.
Fetotoxicant is a chemical that adversely affects the developing fetus, resulting in low birth weight, symptoms of poisoning at birth or stillbirth (fetus dies before it is born).
Synergism when the combined effect of exposure to more than one chemical at one time, or to a chemical in combination with other hazards (heat, radiation, infection) results in effects of such exposure to be greater than the sum of the individual effects of each hazard by itself.
Toxicogenomics the interaction between the genome, chemicals in the environment, and disease. Cells exposed to a stress, drug or toxicant respond by altering the pattern of expression of genes within their chromosomes. Based on new genetic and microarray technologies.
Teratology Links: Abnormal Development | Genetic Abnormalities | Maternal Factors | [images/hcriticaldev.gif Critical Periods of Development] | Abnormal Development - Maternal | Abnormal Development - Fetal Alcohol Syndrome | Abnormal Development - Viral Infection | Rubella Virus | Abnormal Development - Hyperthermia | Abnormal Development - Drugs | Genetic Abnormalities | Abnormal Development - Trisomy 21 (Down Syndrome)
Australian Drug Categories
Legal drugs are classified, usually by each country's appropriate regulatory body, on the safety of drugs during pregnancy. In Australia, the Therapeutic Goods Authority has classes (A, B1, B2, B3, C, D and X) to define their safety. In the USA, drugs are classified by the Food and Drug Administration (FDA) into classes (A, B, C, D, and X) to define their safety.
Pregnancy Category A
Have been taken by a large number of pregnant women and women of childbearing age without an increase in the frequency of malformations or other direct or indirect harmful effects on the fetus having been observed.
Pregnancy Category B1
Drugs which have been taken by only a limited number of pregnant women and women of childbearing age, without an increase in the frequency of malformation or other direct or indirect harmful effects on the human fetus having been observed. Studies in animals have not shown evidence of an increased occurrence of fetal damage.
Pregnancy Category B2
Have been taken by only a limited number of pregnant women and women of childbearing age, without an increase in the frequency of malformation or other direct or indirect harmful effects on the human fetus having been observed. Studies in animals are inadequate or may be lacking, but available data show no evidence of an increased occurrence of fetal damage.
Pregnancy Category B3
Have been taken by only a limited number of pregnant women and women of childbearing age, without an increase in the frequency of malformation or other direct or indirect harmful effects on the human fetus having been observed. Studies in animals have shown evidence of an increased occurrence of fetal damage, the significance of which is considered uncertain in humans.
Pregnancy Category C
Have caused or may be suspected of causing, harmful effects on the human fetus or neonate without causing malformations. These effects may be reversible.
Pregnancy Category D
Have caused, are suspected to have caused or may be expected to cause, an increased incidence of human fetal malformations or irreversible damage. These drugs may also have adverse pharmacological effects.
Pregnancy Category X
Have such a high risk of causing permanent damage to the fetus that they should NOT be used in pregnancy or when there is a possibility of pregnancy.
Links: Abnormal Development - Drugs | Australian Fetal Risk Categories | USA FDA Fetal Risk Categories | Therapeutic Goods Authority | Australian Drug Evaluation Committee (ADEC) | Prescribing Medicines in Pregnancy | Appendix A: Therapeutic goods exempted from pregnancy classification |
Applied Embryology Links
The following are links to relevant notes pages that cover the key embryology concepts in this tutorial. These pages and their links will provide further detailed information.
Week 2 Abnormalities - Trophoblastic Disease | Placenta
Neural Abnormalities | Abnormal Development - Folic Acid and Neural Tube Defects | Week 3 - Neuralation
Week 1 Blastocyst | [BGDlab3_5.htm BGD - Early Cell Division] | Molecular Development
Teratology Links
The following are links to relevant notes pages that cover the key teratology concepts in this tutorial. Links from these pages will provide further detailed information.
Abnormal Development | Genetic Abnormalities | Maternal Factors
Critical Periods of Development
Abnormal Development- Australian Statistics | Normal Development- Australian Statistics
Genetic Abnormalities | Abnormal Development - Trisomy 21 (Down Syndrome)
Abnormal Development - Maternal
Abnormal Development - Fetal Alcohol Syndrome
Abnormal Development - Viral Infection | Rubella Virus
Abnormal Development - Hyperthermia
Additional Abnormal Development Links
Australian Statistics | Normal Development- Birth - Stillbirth and Perinatal Death | Abnormalities by SystemsPrenatal DiagnosisFetal Origins Hypothesis | Intrauterine Growth RetardationTwinningGenetic Abnormalities | Down Syndrome | Edwards SyndromeMaternal FactorsNeural Tube DefectsFetal Alcohol SyndromeSmokingChemicalDrugsRadiationHeavy MetalIodine DeficiencyViral Infection | Rubella | Parvovirus | Databases | NINDS Factsheets
External Abnormal Development Links
AIHW National Perinatal Statistics Unit Congenital malformations, Australia 1997
Victorian Birth Defects Register (VBDR) | VBDR brochure Food and Drug Administration (USA) Evaluating the Risks of Drug Exposure in Human Pregnancies
Centers for Disease Control and Prevention (CDC, USA) Pregnancy Risk Assessment Monitoring System (PRAMS) collects state-specific, population-based data on maternal attitudes and experiences before, during, and shortly after pregnancy.
Motherisk (Canada) Drugs, chemicals, radiation and herbal products in pregnancyOffice of Children's Health Protection (USA) Critical Periods in Development OCHP Paper Series on Children's Health and the Environment (2003) (PDF document)International Society for the Study of Trophoblastic Diseases Trophoblastic Diseases
Glossary Links
- Glossary: A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | Numbers | Symbols | Term Link
Cite this page: Hill, M.A. (2024, May 4) Embryology 2010 BGD Tutorial - Applied Embryology and Teratology. Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/2010_BGD_Tutorial_-_Applied_Embryology_and_Teratology
- © Dr Mark Hill 2024, UNSW Embryology ISBN: 978 0 7334 2609 4 - UNSW CRICOS Provider Code No. 00098G