Trisomy 13
| Embryology - 27 Apr 2024 |
|---|
| Google Translate - select your language from the list shown below (this will open a new external page) |
|
العربية | català | 中文 | 中國傳統的 | français | Deutsche | עִברִית | हिंदी | bahasa Indonesia | italiano | 日本語 | 한국어 | မြန်မာ | Pilipino | Polskie | português | ਪੰਜਾਬੀ ਦੇ | Română | русский | Español | Swahili | Svensk | ไทย | Türkçe | اردو | ייִדיש | Tiếng Việt These external translations are automated and may not be accurate. (More? About Translations) |
ICD-11 - LD40.1 Complete trisomy 13
|
Introduction
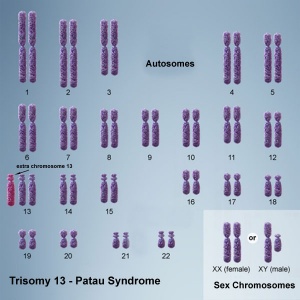
International Classification of Diseases Trisomy 13 (Patau syndrome) is a rare (1 in 10,000 newborns) developmental genetic abnormality (aneuploidy) with three copies of chromosome 13, instead of the usual two copies, there can also be a chromosomal translocation. Infant may have a single placental artery at birth.
Both trisomy 13 and trisomy 18 are generally considered fatal anomalies, with a majority of infants dying in the first year after birth.[1]
Patau syndrome is named after Klaus Pätau (1908–1975) an American geneticist who in 1960[2] was the first to attribute the syndrome of trisomy to chromosome 13.
Some Recent Findings
|
| More recent papers |
|---|
|
This table allows an automated computer search of the external PubMed database using the listed "Search term" text link.
More? References | Discussion Page | Journal Searches | 2019 References | 2020 References Search term: Trisomy 13 | Patau syndrome |
| Older papers |
|---|
| These papers originally appeared in the Some Recent Findings table, but as that list grew in length have now been shuffled down to this collapsible table.
See also the Discussion Page for other references listed by year and References on this current page.
|
Aneuploidy
- Euploidy normal, means having the complete chromosome sets (n, 2n, 3n). Aneuploidy is one of the three main classes of numerical chromosomal abnormalities:
- Aneuploidy are chromosome mutations in which chromosome number is abnormal (increased or reduced), nondisjunction in meiosis or mitosis (anaphase of meiosis I, sister chromatids fail to disjoin at either meiosis II or at mitosis) is the cause of most aneuploids.
- Polyploidy includes triploidy, usually due to two sperm fertilizing a single egg.
- Mixoploidy includes mosaicism, where there are two or more genetically different cell lines in an individual.
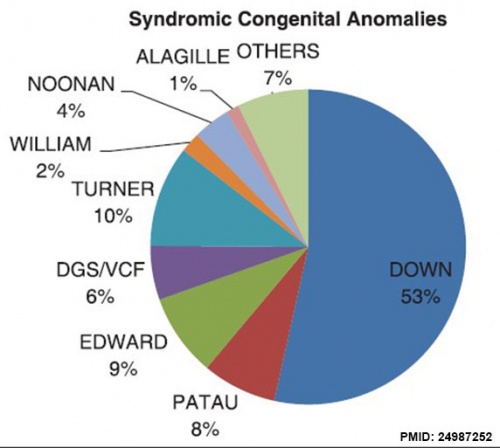
Prevalence
Abnormalities from USA Nationwide Inpatient Sample database (1998 to 2008)[8]
Cardiac Abnormalities
- Atrial septal defect
- Patent ductus arteriosus
- Ventricular septal defect
A study of Japanese cardiac surgery in patients with trisomy 18 and trisomy 13 in Japan[9]</ref>
- clinical data from 134 patients with T18 and 27 patients with T13
- patients with T13, 5 (19%) of 27 patients were alive during study period.
- Twenty-three (85%) of 27 patients had CHD and 13 (57%) of 27 patients had PH.
- Atrial septal defect was the most common form of CHD (22%).
- Cardiac surgery was done in 6 (26%) of 23 patients.
Cyclopedia Abnormality
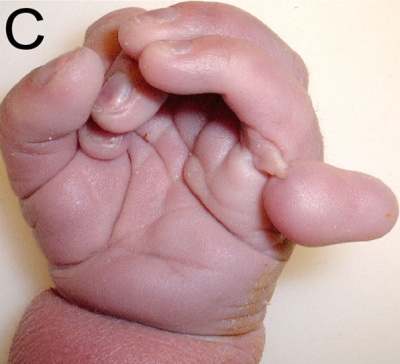
Digit Abnormality
Trisomy 13 polydactyly[10]
Neural Tube Abnormality
Additional Images
References
- ↑ Nelson KE, Hexem KR & Feudtner C. (2012). Inpatient hospital care of children with trisomy 13 and trisomy 18 in the United States. Pediatrics , 129, 869-76. PMID: 22492767 DOI.
- ↑ PATAU K, SMITH DW, THERMAN E, INHORN SL & WAGNER HP. (1960). Multiple congenital anomaly caused by an extra autosome. Lancet , 1, 790-3. PMID: 14430807
- ↑ Goel N, Morris JK, Tucker D, de Walle HEK, Bakker MK, Kancherla V, Marengo L, Canfield MA, Kallen K, Lelong N, Camelo JL, Stallings EB, Jones AM, Nance A, Huynh MP, Martínez-Fernández ML, Sipek A, Pierini A, Nembhard WN, Goetz D, Rissmann A, Groisman B, Luna-Muñoz L, Szabova E, Lapchenko S, Zarante I, Hurtado-Villa P, Martinez LE, Tagliabue G, Landau D, Gatt M, Dastgiri S & Morgan M. (2019). Trisomy 13 and 18-Prevalence and mortality-A multi-registry population based analysis. Am. J. Med. Genet. A , 179, 2382-2392. PMID: 31566869 DOI.
- ↑ Huang T, Meschino WS, Rashid S, Dennis A, Mak-Tam E & Cuckle H. (2018). Enhanced First Trimester Aneuploidy Screening with Placental Growth Factor and Alpha Feto-Protein: Detection of Trisomies 18 and 13. J Obstet Gynaecol Can , , . PMID: 30025867 DOI.
- ↑ Pyle AK, Fleischman AR, Hardart G & Mercurio MR. (2018). Management options and parental voice in the treatment of trisomy 13 and 18. J Perinatol , , . PMID: 29977011 DOI.
- ↑ Alberman E, Mutton D & Morris JK. (2012). Cytological and epidemiological findings in trisomies 13, 18, and 21: England and Wales 2004-2009. Am. J. Med. Genet. A , 158A, 1145-50. PMID: 22495937 DOI.
- ↑ Miller DT, Adam MP, Aradhya S, Biesecker LG, Brothman AR, Carter NP, Church DM, Crolla JA, Eichler EE, Epstein CJ, Faucett WA, Feuk L, Friedman JM, Hamosh A, Jackson L, Kaminsky EB, Kok K, Krantz ID, Kuhn RM, Lee C, Ostell JM, Rosenberg C, Scherer SW, Spinner NB, Stavropoulos DJ, Tepperberg JH, Thorland EC, Vermeesch JR, Waggoner DJ, Watson MS, Martin CL & Ledbetter DH. (2010). Consensus statement: chromosomal microarray is a first-tier clinical diagnostic test for individuals with developmental disabilities or congenital anomalies. Am. J. Hum. Genet. , 86, 749-64. PMID: 20466091 DOI.
- ↑ Egbe A, Lee S, Ho D, Uppu S & Srivastava S. (2014). Prevalence of congenital anomalies in newborns with congenital heart disease diagnosis. Ann Pediatr Cardiol , 7, 86-91. PMID: 24987252 DOI.
- ↑ Maeda J, Yamagishi H, Furutani Y, Kamisago M, Waragai T, Oana S, Kajino H, Matsuura H, Mori K, Matsuoka R & Nakanishi T. (2011). The impact of cardiac surgery in patients with trisomy 18 and trisomy 13 in Japan. Am. J. Med. Genet. A , 155A, 2641-6. PMID: 21990245 DOI.
- ↑ Chan A, Lakshminrusimha S, Heffner R & Gonzalez-Fernandez F. (2007). Histogenesis of retinal dysplasia in trisomy 13. Diagn Pathol , 2, 48. PMID: 18088410 DOI.
Reviews
Chen CP. (2010). Prenatal diagnosis and genetic counseling for mosaic trisomy 13. Taiwan J Obstet Gynecol , 49, 13-22. PMID: 20466287 DOI.
Solomon BD, Rosenbaum KN, Meck JM & Muenke M. (2010). Holoprosencephaly due to numeric chromosome abnormalities. Am J Med Genet C Semin Med Genet , 154C, 146-8. PMID: 20104610 DOI.
Spencer K. (2007). Aneuploidy screening in the first trimester. Am J Med Genet C Semin Med Genet , 145C, 18-32. PMID: 17290444 DOI.
Bugge M, deLozier-Blanchet C, Bak M, Brandt CA, Hertz JM, Nielsen JB, Duprez L & Petersen MB. (2005). Trisomy 13 due to rea(13q;13q) is caused by i(13) and not rob(13;13)(q10;q10) in the majority of cases. Am. J. Med. Genet. A , 132A, 310-3. PMID: 15690377 DOI.
Oyler M, Long BW & Cox LA. (2004). Sonographic markers used to detect frequent trisomies. Radiol Technol , 76, 13-8. PMID: 15503716
Shipp TD & Benacerraf BR. (2002). Second trimester ultrasound screening for chromosomal abnormalities. Prenat. Diagn. , 22, 296-307. PMID: 11981910 DOI.
Rodríguez JI, García M, Morales C, Morillo A & Delicado A. (1990). Trisomy 13 syndrome and neural tube defects. Am. J. Med. Genet. , 36, 513-6. PMID: 2202219 DOI.
Huang CY, Chiang JH, Yeh GP, Chou PH, Shiau HJ, Lai YS & Li SY. (1987). Cyclopia with trisomy 13. Aust N Z J Obstet Gynaecol , 27, 251-5. PMID: 3325020
Articles
Carey JC. (2020). Emerging evidence that medical and surgical interventions improve the survival and outcome in the trisomy 13 and 18 syndromes. Am. J. Med. Genet. A , 182, 13-14. PMID: 31609083 DOI.
Lakovschek IC, Streubel B & Ulm B. (2011). Natural outcome of trisomy 13, trisomy 18, and triploidy after prenatal diagnosis. Am. J. Med. Genet. A , 155A, 2626-33. PMID: 21990236 DOI.
Search Pubmed
Search Pubmed Nov 2010 "Trisomy 13" - All (3649) Review (283) Free Full Text (452)
Search Pubmed: Trisomy 13 | Patau Syndrome
External Links
External Links Notice - The dynamic nature of the internet may mean that some of these listed links may no longer function. If the link no longer works search the web with the link text or name. Links to any external commercial sites are provided for information purposes only and should never be considered an endorsement. UNSW Embryology is provided as an educational resource with no clinical information or commercial affiliation.
- NSW Centre for Genetics Education Fact Sheet - Trisomy 13
- PubMed Health Trisomy 13
Glossary Links
- Glossary: A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | Numbers | Symbols | Term Link
Cite this page: Hill, M.A. (2024, April 27) Embryology Trisomy 13. Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/Trisomy_13
- © Dr Mark Hill 2024, UNSW Embryology ISBN: 978 0 7334 2609 4 - UNSW CRICOS Provider Code No. 00098G