BGDA Practical Placenta - Cord Development
| Practical 14: Implantation and Early Placentation | Villi Development | Maternal Decidua | Cord Development | Placental Functions | Diagnostic Techniques | Abnormalities |
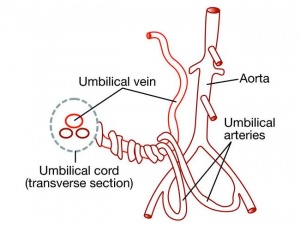
Placental/Umbilical Cord
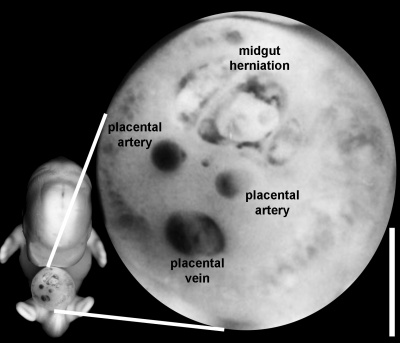
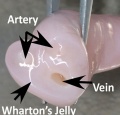
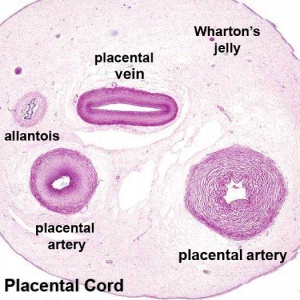
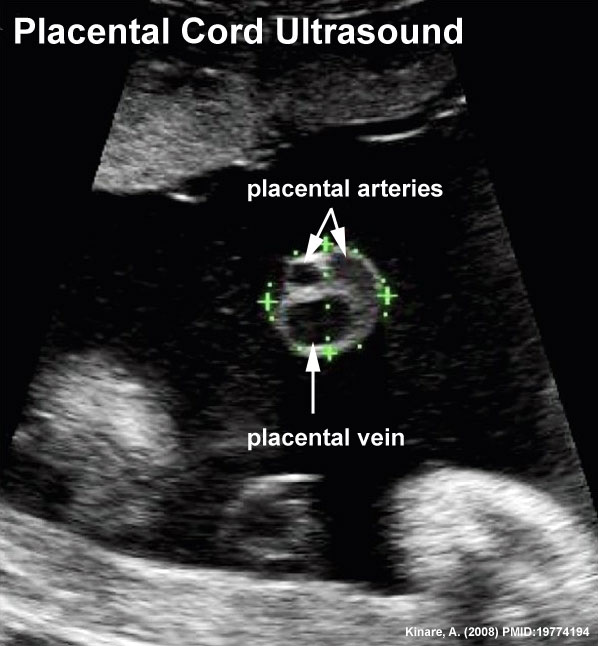
Placental Arteries and Vein
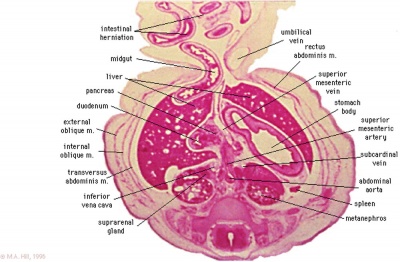
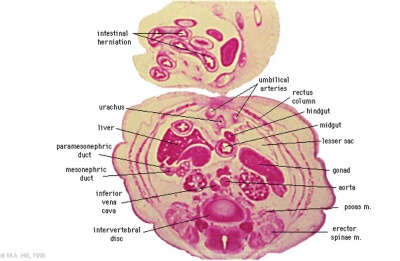
Week 8
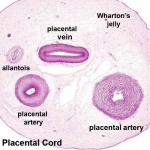
Placental Cord Histology
| Slide - Human Placental Cord |
Placental Cord Ultrasound
|
Ultrasound of transverse scan through the cord
|
Wharton's Jelly
Hofbauer Cells
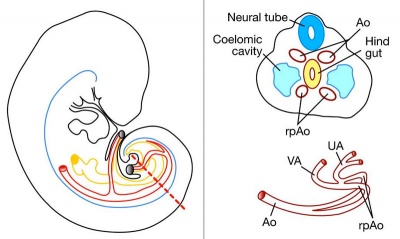
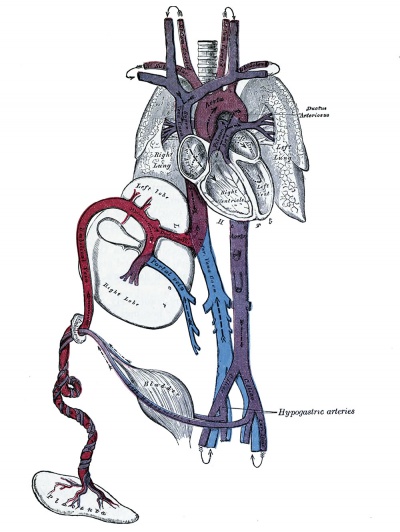
Fetal Circulation
|
|
|
Cord Features
Cord Length
The following are lengths and classifications at term.
- Normal range - 50 to 60 cm.
- Short cord - less than 35 cm.
- Long cord - over 70 cm can be associated with wrapping around the fetus and other abnormalities.
Cord Coiling
- Hypocoiling - associated with increased incidence of fetal demise, intrapartum fetal heart rate decelerations, operative delivery for fetal distress, anatomic-karyotypic abnormalities and chorio-amnionitis.
- Hypercoiling - associated with increased incidence of fetal growth restriction, intrapartum fetal heart rate decelerations, vascular thrombosis and cord stenosis.
Placental Cord Interactive Component
| Attempt the Quiz - Placental Cord | ||
|---|---|---|

Here are a few simple Quiz questions that relate to Placental Cord from the practical.
|
| Practical 14: Implantation and Early Placentation | Villi Development | Maternal Decidua | Cord Development | Placental Functions | Diagnostic Techniques | Abnormalities |
Additional Information
| Additional Information - Content shown under this heading is not part of the material covered in this class. It is provided for those students who would like to know about some concepts or current research in topics related to the current class page. |
Persistent Right Umbilical Vein
Persistent Right Umbilical Vein (PRUV)
Adiego-Calvo I, Saviron-Cornudella R, Martinez-Payo C, Rubio-Aranda E, Sancho-Sauco J, Cisneros-Gimeno AI, Perez-Perez P, Lerma-Puertas D & Whyte-Orozco J. (2016). Are congenital malformations more frequent in fetuses with intrahepatic persistent right umbilical vein? A comparative study. Taiwan J Obstet Gynecol , 55, 782-785. PMID: 28040119 DOI.
Kumar SV, Chandra V, Balakrishnan B, Batra M, Kuriakose R & Kannoly G. (2016). A retrospective single centre review of the incidence and prognostic significance of persistent foetal right umbilical vein. J Obstet Gynaecol , 36, 1050-1055. PMID: 27599270 DOI.
Canavan TP & Hill LM. (2016). Neonatal Outcomes in Fetuses With a Persistent Intrahepatic Right Umbilical Vein. J Ultrasound Med , 35, 2237-41. PMID: 27582531 DOI.
Hill LM, Mills A, Peterson C & Boyles D. (1994). Persistent right umbilical vein: sonographic detection and subsequent neonatal outcome. Obstet Gynecol , 84, 923-5. PMID: 7970470
- A study of 15,237 obstetric ultrasound examinations performed after 15 weeks' gestation identified only 33 cases of persistent right umbilical vein.
- Note that there can be also an intrahepatic portion of PRUV (I-PRUV)
Vessel Anomalies
- Fetal intra-abdominal umbilical vein varix is a focal dilatation of the intra-abdominal portion of the umbilical vein.
Nuchal Cord
Recent large study of tight nuchal cord, where the placental cord is completely wrapped around the fetal neck.[2]
The best practices for the care of a neonate born after a tight nuchal cord have not been defined. As a step toward this, we compared the outcomes of neonates born after a tight nuchal cord vs those born after a loose nuchal cord vs those born after no nuchal cord. This was a retrospective comparison using electronic data of all deliveries during a 6-year period (2005 to 2010) in a multihospital healthcare system in the western United States. At the time of delivery, each birth was recorded as having a tight nuchal cord, a loose nuchal cord or no nuchal cord. Nuchal cord was defined as a loop of umbilical cord ≥360° around the fetal neck. 'Tight' was defined as the inability to manually reduce the loop over the fetal head, and 'loose' as the ability to manually reduce the loop over the head.
Of 219,337 live births in this period, 6.6% had a tight nuchal cord and 21.6% had a loose nuchal cord. Owing to the very large number of subjects, several intergroup differences were statistically significant but all were judged as too small for clinical significance. For instance, those with a tight nuchal cord had a very slightly older gestational age, a very slightly lower birth weight, a preponderance of male fetuses, primagravid women, singleton pregnancies and shoulder dystocia (all P<0.001). Term neonates with a tight nuchal cord were slightly more likely to be admitted to a Neonatal Intensive Care Unit (6.6% vs 5.9% admission rate, P=0.000). Those with a tight nuchal cord were not more likely to have dopamine administered or blood hemoglobin measured on the first day, nor were they more likely to receive a transfusion or to die. The subset of very low birth weight neonates with a tight nuchal cord, compared with those with no nuchal cord, were of the same gestational age and birth weight, with the same Apgar scores, and were not more likely to have severe intraventrucular hemorrhage, retinopathy of prematurity or periventricular leukomalacia, or to die.
The presence of a tight nuchal cord is not uncommon, occurring in 6.6% of over 200,000 consecutive live births in a multihospital health system. No differences in demographics or outcomes, judged as clinically significant, were associated with a tight nuchal cord. Thus, we speculate that the best practices for neonatal care after a tight nuchal cord do not involve an obligation to conduct extra laboratory studies or extra monitoring solely on the basis of the report of a tight nuchal cord.
References
- ↑ Shwarzman P, Waintraub AY, Frieger M, Bashiri A, Mazor M & Hershkovitz R. (2013). Third-trimester abnormal uterine artery Doppler findings are associated with adverse pregnancy outcomes. J Ultrasound Med , 32, 2107-13. PMID: 24277892 DOI.
- ↑ Henry E, Andres RL & Christensen RD. (2013). Neonatal outcomes following a tight nuchal cord. J Perinatol , 33, 231-4. PMID: 22699359 DOI.
| Practical 14: Implantation and Early Placentation | Villi Development | Maternal Decidua | Cord Development | Placental Functions | Diagnostic Techniques | Abnormalities |