Menstrual Cycle
Introduction
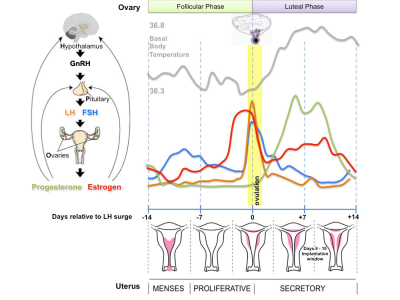
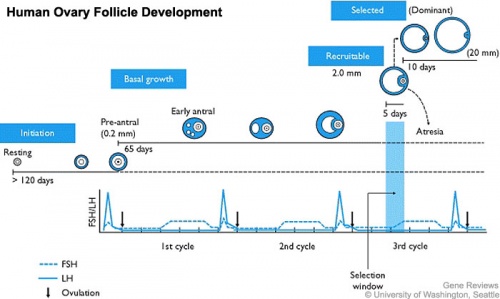
The human reproductive cycle, an cyclic endocrine regulated change in female anatomy and physiology that occur over 28 days (4 weeks, a lunar month) during reproductive life (between puberty and menopause). Endocrine changes during pregnancy block the menstrual cycle, which normally would shed the functional layer of the uterine lining each cycle. A common misunderstanding is that development of the follicles occurs within a single cycle, in fact humans require at least 3 menstrual cycles to occur in the development of an ovulating follicle.
This cycle differs from other non-primate female vertebrates (eg rats, mice, horses, pig) that have a reproductive cycle called the estrous cycle (oestrous, British spelling).
- The average menstrual cycle is 28 days with ovulation (egg release) occuring approximately the middle of the cycle.
- The last menstrual period (LMP) is used clinically in determining developmental ages. (More Birth Date)
- Menstruation phase (menses, period) is the loss of the uterus epithelial functional layer and occurs if fertilization and implantation have not occurred before the end of the current cycle.
Menstrual Parameters
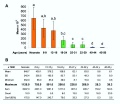
There is a broad variability in the parameters of the adult human menstrual cycle. The data below is based upon normal mid-reproductive years and using simplified terminology, Table IV from 2007 international agreement discussion.[1] The same group also recommended replacing confusing clinical terms such as amenorrhea, menorrhagia, metrorrhagia, hypermenorrhea and dysfunctional uterine bleeding.
| Clinical dimensions of menstruation and menstrual cycle | Descriptive terms | Normal limits (5th - 95th percentiles) |
| Frequency of menses (days) | Frequent | < 24 |
| Normal | 24 - 38 | |
| Infrequent | > 38 | |
| Regularity of menses (cycle to cycle variation over 12 months; in days) | Absent | - |
| Regular | Variation ± 2 to 20 days | |
| Irregular | Variation greater than 20 days | |
| Duration of flow (days) | Prolonged | > 8.0 |
| Normal | 4.5 - 8.0 | |
| Shortened | < 4.5 | |
| Volume of monthly blood loss (ml)[2] | Heavy | > 80 |
| Normal | 5 - 80 | |
| Light | < 5 |
Iron Depletion
See also the article on iron depletion by whole-blood donation harms menstruating females.[3] "The collection of 450 or 500 mL of whole blood, plus an additional 30 to 50 mL for blood tests, results in 480 to 550 mL of blood loss per whole-blood donation. These losses leads to a 60- to 88-g loss of hemoglobin (Hb) per whole-blood donation in women, based on a Hb range of 12.5 to 16.0 g per dL, and 204 to 299 mg of iron loss, based on 3.4 mg of iron per gram of Hb. This iron loss is 9 to 13 percent of the total body iron in an average woman (2300 mg), and it is 66 to 97 percent of the total stored iron in an average menstruating woman (309 mg). Therefore, whole-blood donation is an iron depletion event that causes significant iron loss in women."
- prevalence of iron deficiency in 20- to 49-year-old women before blood donation is 12 percent
- prevalence of iron deficiency in 16- to 69-year-old men is 2 percent
(based on data from the National Health and Nutrition Examination Survey (NHANES 1999-2000)
Environmental Effects
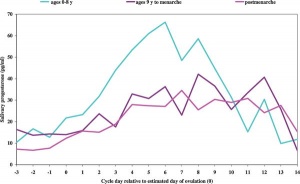
A recent paper has also demonstrated that the human menstral cycle can be modulated postnatally by environmental conditions as measured by changes in progesterone based upon the age of migration from a relatively poor environment (Bangladesh) to a relatively better environment (UnitedKingdom).[4]
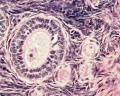
Menstrual Cycle Histology
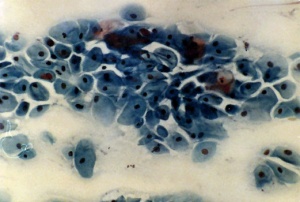
The different stages of the menstrual cycle can be monitored by the cellular appearance of vaginal smears Menstrual Cycle - Histology.
A more invasive technique is dilate and curettage (DnC), which allows sampling of the functional layer of the uterine endometrium Menstrual Cycle - Histology.
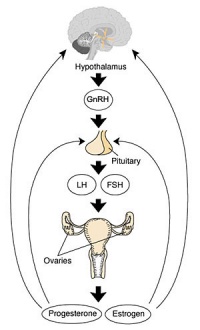
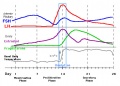
Ovulation (HPG Axis)
- Hypothalmus releases gonadotropin releasing hormone (GRH, luteinizing hormone–releasing hormone, LHRH) -> Pituitary releases follicle stimulating hormone (FSH) and lutenizing hormone (LH) -> ovary follicle development and ovulation.
- release of the secondary oocyte and formation of corpus luteum
- secondary oocyte encased in zona pellucida and corona radiata
- Ovulation associated with follicle rupture and ampulla movement
Ovulation Movies
Human Oocyte Numbers
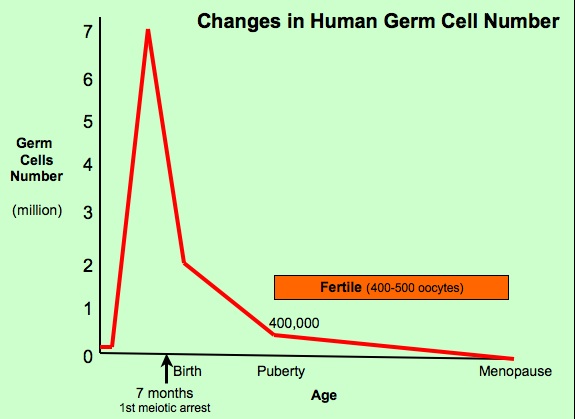
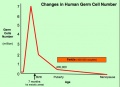
There is continuing debate as to whether the human ovary has the ability to generate, or continues to generate, new functional follicles and oocytes postnatally.[5] [6] (More? Ovary Development)
- The graph shows the changes in human germ cell numbers in the ovary with age, peaking at about 7 million (occuring in early fetal development) and then decreasing by apopotic cell death.
- At puberty there remain only about 400,000 and only about 10% of these will be released through reproductive life.
- Graph data based on article.[7]
Follicle Development
A common misunderstanding is that development of the follicle containing the oocyte occurs within a single cycle. In fact humans require at least 3 menstrual cycles to occur in the development of a single ovulating follicle. Most of the other follicles will degenerate in a process described as atresia.
Oocyte Development
Primary Oocyte
- arrested at early Meiosis 1
- diploid: 22 chromosome pairs + 1 pair X chromosomes (46, XX) autosomes and sex chromosome
- Oogenesis- pre-antral then antral follicle (Graafian follicle is mature antral follicle released)
Secondary Oocyte
- 1 Day before ovulation completes (stim by LH) Meiosis 1
- haploid: 22 chromosomes + 1 X chromosome (23, X)
- nondisjunction- abnormal chromosome segregation
- begins Meiosis 2 and arrests at metaphase
- note no interphase replication of DNA, only fertilization will complete Meiosis 2
Ovarian Stimulation
A variety of drug based techniques are used to stimulate maternal oocyte development, called ovarian stimulation, for many assisted reproductive technology (in vitro fertilization) procedures. The recommended for technique will vary for some procedures and also from clinic to clinic and between countries.
An example of ovarian stimulation
- Gonadotrophin releasing hormone agonist (GnRHa) triptorelin acetate (Decapeptyl (0.1 mg/day) was started on the 22nd day of the preceding menstrual cycle.
- Human menopausal gonadotrophin (HMG) and/or follicular stimulating hormone (FSH; Gonal-F, Serono) was carried out daily 12 to 15 days later.
- Dosage may vary dependent upon patient response and can be monitored by hourmone levels (oestradiol) and transvaginal ultrasound (follicular size).
- The resulting ovulatory wave generates large follicles (greater than 18 mm in diameter).
- Human chorionic gonadotrophin (HCG) is then administered (36 to 38 h later)
- Clinical transvaginal puncture is used to collect from these follicles cumulus-oocyte complexes.
- Links: In Vitro Fertilization
References
- ↑ <pubmed>17204526</pubmed> | Hum Reprod.
- ↑ <pubmed>5922481</pubmed>
- ↑ <pubmed>8654511</pubmed>
- ↑ <pubmed>17503960</pubmed> | PLoS Medicine
- ↑ <pubmed>15115550</pubmed>
- ↑ <pubmed>18596027</pubmed>
- ↑ <pubmed>8908177</pubmed>
Reviews
- The primordial pool of follicles and nest breakdown in mammalian ovaries. Tingen C, Kim A, Woodruff TK. Mol Hum Reprod. 2009 Dec;15(12):795-803. Epub 2009 Aug 26. Review. PMID: 19710243 | Mol Hum Reprod.
Articles
- Effect of rising hCG levels on the human corpus luteum during early pregnancy. Järvelä IY, Ruokonen A, Tekay A. Hum Reprod. 2008 Dec;23(12):2775-81. PMID: 18694877
Search Pubmed
Search Pubmed Now: Menstrual Cycle | corpus luteum
Additional Images
- Monkey-ovary x20he.jpg
Ovary - antral follicle
External Links
Women’s Health Queensland Wide - Understanding Your Menstrual Cycle
Glossary Links
- Glossary: A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | Numbers | Symbols | Term Link
Cite this page: Hill, M.A. (2024, May 6) Embryology Menstrual Cycle. Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/Menstrual_Cycle
- © Dr Mark Hill 2024, UNSW Embryology ISBN: 978 0 7334 2609 4 - UNSW CRICOS Provider Code No. 00098G