Book - Extra-uterine pregnancy - 1921
| Embryology - 28 Apr 2024 |
|---|
| Google Translate - select your language from the list shown below (this will open a new external page) |
|
العربية | català | 中文 | 中國傳統的 | français | Deutsche | עִברִית | हिंदी | bahasa Indonesia | italiano | 日本語 | 한국어 | မြန်မာ | Pilipino | Polskie | português | ਪੰਜਾਬੀ ਦੇ | Română | русский | Español | Swahili | Svensk | ไทย | Türkçe | اردو | ייִדיש | Tiếng Việt These external translations are automated and may not be accurate. (More? About Translations) |
Schumann EA. Extra-uterine pregnancy (1921) D. Appleton And Company, New York London 1921.
| Online Editor | |||||
|---|---|---|---|---|---|
| This historic 1921 book by Schumann described the historic treatment of ectopic pregnancy.
|
| Historic Disclaimer - information about historic embryology pages |
|---|
| Pages where the terms "Historic" (textbooks, papers, people, recommendations) appear on this site, and sections within pages where this disclaimer appears, indicate that the content and scientific understanding are specific to the time of publication. This means that while some scientific descriptions are still accurate, the terminology and interpretation of the developmental mechanisms reflect the understanding at the time of original publication and those of the preceding periods, these terms, interpretations and recommendations may not reflect our current scientific understanding. (More? Embryology History | Historic Embryology Papers) |
Extra-Uterine Pregnancy
By
Edward A. Schumann, M.D. (Edward Armin), 1879-1970
Lecturer On Obstetrics, Jefferson Medical College; Gynecologist And Obstetrician To The Philadelphia General Hospital; Gynecologist To Frankford Hospital; Consulting Gynecologist To Rush Hospital; Assistant Obstetrician Jefferson Medical College Hospital; Fellow Of The American Gynecological Society, Obstetrical Society Of Philadelphia, Etc.
Gynecological and Obstetrical Monographs with Seventy-One Illustrations
D. Appleton And Company
New York
London
Printed In The United States Of America
Preface
Progress in surgery, both from the scientific side and from the purely practical clinical aspect, is perhaps as well summarized by a study of the advance in thought concerning extra-uterine pregnancy as may be possible.
Less than two generations ago, the woman to whom befell the calamity of a ruptured tubal pregnancy, was doomed to almost certain death, without benefit of any rational attempt being made to save her.
To-day the mortality of this formerly dreaded accident has been reduced to below five per cent.
This book has been prepared to emphasize the progress and to present modern thought concerning the several problems arising from a consideration of various phases of ectopic gestation.
Especial attention has been paid to the etiology and pathology with a view toward grouping and epitomizing rational explanations as to the cause of the condition.
American views have been particularly embodied in the work and the ideas presented may be said to reflect the general trend of opinion upon this subject, in this country at this time.
Illustrative case histories have been incorporated from time to time but no attempt has been made to reproduce in full, verbose and irrelevant anamneses.
The original material consists of cases occurring in the service of the writer at the Philadelphia General, Jefferson, Frankford and Gynecean Hospitals and the management of ectopic gestation as outlined is that practiced by him in these institutions.
The author is indebted to the publishers, Messrs, D. Appleton and Company, for many acts of kindness ; to Mrs. Gertrude V. Schwartz for her painstaking and careful illustrations, to Miss Marion E. Tighe for her faithful preparation of the text and to Dr. Charles P. Noble for his helpful criticism and suggestions.
Edward A. Schumann
PHILADELPHIA
Contents
I. Historical Considerations
- Development of modern methods of treatment, I — Extra-uterine pregnancy unknown to the ancients, i— First recorded case, i — Case reported by Cordseus, 3 — Essay of Dr. Campbell, 4 — Monograph of John S. Parry, 4 — Review of H. C. Kelly, 4 — Case of Cornax, 4 — Case of Jacob Nufer, 4 — Bain's operation, 5 — Case of Primrose, 6 — Case of Dr. Felix Platerus, 6 — Case reported by Calvo, 6 — Case of Riolanus, 7 — Mauriceau's case, 7 — 'Work of Pierre Dionis, 9 — First recorded case in America, 9 — Second recorded case, 10 — Monograph of Dezeimeris, 10 — Parry's Book, 11 — Work of Lawson Tait, 12 — Use of electricity advocated, 15 — History of treatment, 12 — Treatment of rupture of the cyst, 12 — Treatment suggested by Dr. Harbert, 14 — Treatment suggested by Stephen Rogers, 14 — Case of Dr. Charles Briddon, 15 — Experiments of Dr. Hunter Robb, 15.
II. Definition, Frequency, Causes
- Definition, 17 — Frequency, 17 — Race incidence, 19 — Age, 19 — The varieties of extra-uterine gestation, 19 — The relative frequency, 21 — The causes of extra-uterine pregnancy, 22^-Obstruction of the tubal lumen from without, 23 — Anomalies of the tubal lumen, accessory tubes, etc., into which the ovum falls, 25 — Decidual reaction of the tube, 26 — The external migration of the ovum, 27 — The cause of ovarian pregnancy, 31 — The cause of primary abdominal pregnancy, 31.
III. The Terminations of Ectopic Pregnancy
- Termination by resorption of the ovum, 34 — Death of the embryo with the formation of tubal mole, 34 — Tubal abortion, 34 — Rupture of the pregnant tube, 37 — Rupture between the folds of the broad ligament, 39 — The growth and development of the fetus to full term, while still confined within the tube, 41 — Interstitial pregnancy may terminate by the gradual growth of the fetus into the uterine cavity, 41 — Tubo-abdominal pregnancy, 42 — Secondary abdominal pregnancy, 42 — Tubo-ovarian pregnancy, 43 — Intraligamentary pregnancy, 43— Ovario-abdominal pregnancy, 44 — Abdominal pregnancy, secondary to primary ovarian pregnancy, 44 — Resorption and tubal mole, 44 — Hematocele, 44 — Solitary hematocele, 45 — Infected hematocele, 45 — The terminal changes, 46.
IV. The Anatomy and Pathology of Extra-Uterine Pregnancy
- The mode of implantation of the ovum in the tube, 47 — Placentation in tubal pregnancy, 55 — Changes in the uterus produced by ectopic pregnancy, 62 — The relation of uterine decidua and decidual casts to ectopic pregnancy, 63 — The cast of membranous dysmenorrhea, 67 — The pathology of interstitial or cornual pregnancy, 69 — The pathology of ovarian pregnancy, 73 — Placentation, 75— The pathology of pelvic hematocele, 77— The pathology of advanced ectopic pregnancy, 79— Changes in the tissues the result of ectopic pregnancy, 84 — Diagnosis of ectopic pregnancy, 85— The fate of the embryo in ectopic pregnancy, 87.
V. Recurrent Extra-Uterine Pregnancy
- Twin ectopic pregnancy, 104 — Combined intra- and extra-uterine pregnancy, 108— Complicated extra-uterine pregnancy, 109— Tubal pregnancy and fibroid tumors of the uterus, 109— Unique forms of ectopic pregnancy, in — Hemorrhage from ovary or tube simulating ruptured ectopic pregnancy, 113.
VI. The Diagnosis and Symptomatology of Extra-Uterine Pregnancy
- The previous history, 127— Absolute sterility, 127— Preexisting pelvic disease, 129— The general health and the medical history of the patient, 130 — The findings on general examination of the patient, 131— Blood pressure, 134— The diagnosis of ectopic pregnancy, 136— Diagnosis of long existing and untreated ectopic gestation, 141 — Diagnosis of ectopic pregnancy, other than tubal, 143— Ovarian pregnancy, I45 — Abdominal pregnancy, 146 — The diagnosis of lithopedion or adipocere, 147 — The diagnosis of complicated ectopic gestation, 147 —The differential diagnosis of ectopic pregnancy, 148— Differentiation of ectopic gestation from acute salpingitis, 151 — The histological diagnosis of extra-uterine pregnancy, 157.
VII. Treatment
- Treatment before rupture has occurred, 161— The treatment of the affected tube, 166— The treatment of the remaining tube, 167— The management of abdominal lesions, not connected with the ectopic pregnancy, 168— The closure of the incision, 168— The treatment of advanced extra-uterine pregnancy, 173— The treatment of advanced ectopic pregnancy when the fetus is known to be dead, 176 — The treatment of infected and suppurative ectopic pregnancy, 176— The treatment of hematocele, 176— Mortality and prognosis, 177.
Chapter I. Historical Considerations
Development of Modern Methods of Treatment — Extra-uterine Pregnancy Unknown to the Ancients — First Recorded Case — Case Reported by Cordaeus — Essay of Dr. Campbell — Monograph of John S. Parry — Review of H. C. Kelly — Case of Cornax — Case of Jacob Nufer — Bain's Operation — Case of Primerose — Case of Dr. Felix Platerus — Case Reported by Calvo — Case of Riolan — Mauriceau's Case — Work of Pierre Dionis— First Recorded Case in America — Second Recorded Case — Monograph of Dezeimeris — Parry's Book — Work of Lawson Tait — Use of Electricity Advocated — History of Treatment — Treatment of Rupture of the Cyst — Treatment Suggested by Dr. Harbert — Treatment Suggested by Dr. Stephen Rogers — Case of Dr. Chas. Briddon — Experiments of Dr. Hunter Robb — Bibliography.
The history of the recognition of pregnancy proceeding outside the cavity of the uterus, the gradual understanding of its gravity and the development of modern methods of its treatment, forms one of the most fascinating episodes in that epitome of human intellect, its brilliancies and its lamentable failures, the history of medicine.
Extra-uterine pregnancy was apparently unknown to the ancients, there being no allusion to the subject in the works on Greek or Roman medicine. The first recorded case is that of one Albucasis, an Arabian physician living in Spain and flourishing about the middle of the eleventh century. He reports a case wherein he saw parts of a fetal body escaping from the abdomen of a woman by the process of suppuration. An abstract of this case report is found in the very complete text book of gynecology and obstetrics, "Gynaecorum sive de Mulierum Affectibus Commentarii," edited by Caspar Bauhin and published in Basel in 1586. This work is a collection of essays by different authors; and in the lecture by Francisco Rousetti is found the reference to Albucasis' case, as shown by the reproduction of the text found on the next page.
The following accurate translation of this account of Rousetti was kindly furnished the writer by Professor W. B. McDaniel of the University of Pennsylvania :
"Fourth Account of the Same Subject. — If certain more fastidious readers, who are pleased only with what is ancient, should not be satisfied with these recent authors and cannot really be convinced of anything except with the utmost difficulty, still the authority of the learned and highly distinguished Arab surgeon and doctor Albucasis will, I hope, prove satisfactory. In the second book of his Treatise on Surgery he writes after this fashion. I have seen a woman who although a fetus in her womb had died, yet became pregnant again and had this second child also die in her. A long time afterwards a swelling arose at the navel itself. When this had been opened, matter flowed from it. I was called in to see the case, and although I treated her for a long time, the wound could not be healed. (Presumably he means T could not get the wound to close so that all was whole and firm again in the part affected'). And so I applied strong medicaments of the utmost drawing power, with the result that a great many bones came out one after another, the sight of which greatly frightened me, since I knew that there were no bones in the abdomen. Accordingly, after having carefully weighed all the facts and made a thorough investigation, I recognized that they were the bones of the dead fetus, and so when I had now extracted more of them, I restored her to her former health, excepting only that she was always discharging something through the ulcer. Up to this point we have the account of Albucasis. But if there are still some persons who are so difficult to satisfy that they cannot even in this way be persuaded, because they abominate everything that comes from the Arabs as so much barbarian ignorance, I refer them to Alexander Benedictus, who, in his treatise on the difficulties of childbirth, has a similar story from his own practice."
Fig. 1. Text of Albucasis' Case, from Caspar Bauhin, 1586.
This case of Albucasis was, of course, one of old, long retained secondary abdominal pregnancy, and indeed, all of the older cases were of this variety.
Another interesting example is that of the lithopedion of Sens reported by Cordaeus early in the sixteenth century. A cut of this lithopedion with its description is published by Rousetti in Bauhin's Gynecorum (q.v.) Speaking of this lithopedion, Rousetti says "We must subjoin to this treatise the monstrosity called the Lithopedion or petrified embryo from the city of Sens. Although indeed that may be had in its entirety in the commentaries of Cordaeus, we have inserted in this place a picture of it that was left out in Cordaeus, that we may not without reason fail to satisfy any desire of yours."
Fig. 2. The Lithopedion of Sens. From Bauhin's Commentarii, 1586.
This case led to the publication of an interesting epigram, by an unknown author, the translation of which has also been kindly given by Prof. McDaniel:
"Deucalion, hurling stones behind his back, fashioned from the hard marble our soft race : how does it happen that now, by a change of lot, the tender little body of a baby has limbs that are most like stone? Divine power used to bend the manners of the men of old, but nowadays our untamed necks bear no yoke."
Following these cases, others are recorded with increasing frequency. In compiling the history of the scattered, early records, the writer is greatly indebted to two works, one, a most scholarly and readable essay, entitled "A Memoir of Extra-uterine Gestation," by Wm. Campbell of Edinburgh and published in 1842; the other, the classic monograph of John S. Parry of Philadelphia, "Extra-uterine Pregnancy," Phila., 1876, one of the epoch making works on this subject. The excellent historical review by H. C. Kelly in a discussion before the Baltimore Gynecological Society in 1890, and the article of Bovee, 1 have also been of great service. Free use has been made of these excellent references in outlining the sequence of medical thought upon the matter of ectopic pregnancy.
After the lithopedion of Sens, there occurred a case in the early half of the sixteenth century, that of Cornax. 2 "In the early half of the sixteenth century Cornax dilated an ulcer which formed near the umbilicus, and extracted a semiputrid fetus, which had been retained for nearly five years. When the patient arrived at the termination of her pregnancy, pains resembling those of labor supervened, and were followed by an unusual sound in the abdomen, but the uneasiness did not subside. For four years the abdomen continued distended and painful; and at last, a fetid discharge issued per vaginam. First one abscess, and thereafter another, formed at the umbilicus : these were dilated by an incision eight inches in length, and the fetus removed. The woman recovered so well after the operation as to conceive again, and she had a natural delivery, but died some time thereafter. This case was considered by its narrator as one of rupture of the uterus ; but as the pains continued after the unusual sound in the abdomen was heard, and that there is no mention made of there having been any hemorrhage, it should rather be viewed as an instance of extra-uterine gestation."
In 1500 there is found the remarkable case of Jacob Nufer, which, however, is usually considered as the classical first case of cesarean section on the living woman, as no mention is made as to whether the fetus was intra- or extra-uterine. The details of Nufer's case, as recorded in Von Siebold's History of Obstetrics (Bovee), is as follows: "According to the relation of Caspar Bauhin, in his appendix to the Latin translation of Fr. Rousset's writings upon cesarean section, Jacob Nufer, a swine spayer, at Sigerhausen, in Switzerland, in the year 1 500, delivered his own wife by opening the abdomen, and the operation proved successful for both mother and child. The woman was pregnant for the first time, and when labor came on, and she had already suffered severely for several days, there had gradually assembled at her bedside thirteen midwives and several lithotomists. But all of them together were unable to relieve the poor woman of her child or to mitigate her suffering. Thereupon, the husband of the woman proposed to resort to the last means of saving her, and assured her that, if she would take his advice, he hoped, by the blessing of God, to bring the case to a successful issue. She gave her full consent, and Nufer persisted further in having the permission of the magistrate to his attempt. This, after some reluctance, was eventually obtained. Nufer next asked those of the midwives who had sufficient nerve for it to assist him in the delivery of his wife, while the more timid ones were requested to leave the room. Eleven of them chose the latter course, while two of them and all of the lithotomists remained to assist. The husband first besought the help of the Almighty, then closed the door, laid his wife upon a table and made an incision in her abdomen in the same way he was accustomed with the swine. He opened the abdomen so cleverly at the first incision that the child was safely extracted. When the eleven midwives outside the door heard the baby cry they desired admission, but this was refused until the baby was washed and the wound closed as in the swine. It healed rapidly. She was later confined four times and bore twins. The child delivered by the operation lived seventy-seven years."
Forty years later Bain's operation was performed for a long retained fetus. "In April, 1540, at Castrum Pomponii, commonly called Pomponischi, in the Province of the Lords of Gonzago, not far from the river Po, there lived a woman whose name was Lodovia; but from her great size termed LaCavalla. She had been pregnant and the fetus had died in the uterus, while the soft parts had sloughed through the vulva and the bony portions had been retained within her. She recovered and again became pregnant, followed by a rapid loss of flesh, and was reduced to a condition of great danger. Christopher Bain, a traveling surgeon, happened by and offered to attempt to restore her for ten golden pieces, if successful, and her body if she died. She and her relatives were very poor, and most of the money was raised by their good neighbors. The woman was tied up; he slowly cut through the abdominal wall, including the peritoneum, and at last opened the uterus and extracted the skeleton of a male child; he washed out the uterus with some warm wine and aromatics, and after cauterizing the edges of the wound, closed it with a suture. She recovered and in a short time had other children born in good condition. Later she had four in all. Witnesses : Dominus John Baptist Zorzonus, and Alexander Begher, Dominus Frederick de Filini, and Dominus Leonellus Zorzonus, and Antonius Maiochus or Mazzuchinus, and several others, present at the whole operation."
Bovee thinks this operation was probably done to relieve an ectopic, but as the description clearly states that "he opened the uterus and extracted the skeleton of a male child; he washed out the uterus with warm wine," etc., it would appear that the procedure was in reality a hysterotomy, and that the child must have been contained within the uterus.
The earliest absolutely definite case of surgical interference for the removal of the abdominal fetus, is that of Primerose 3 in 1594. "The history of this patient has become classical. She was twice pregnant with extra-uterine children — first in 1591, and again some time before 1594. The cyst of the first child opened spontaneously through the abdominal wall. The fistula was enlarged, and this child extracted by Jacob Noierus, a surgeon. This operation proving successful Primerose removed the second infant by gastrotomy two months later. It is easy to imagine how he was led to perform the second and more hazardous operation."
"A case that may, upon the whole, be considered very characteristic, is related by Felix Platerus, 1594, in which the concubine of one of the sacerdotal order, at the close of her third pregnancy, endured for eight days pains resembling those of labor, which then subsided without, however, being followed by delivery. After having for some time suffered from a variety of complaints, a small swelling, the size of an acorn, formed a little above the umbilicus ; it was laid open, and an entire but semiputrid fetus extracted from the abdomen; and the hand thereafter introduced into the cavity for the removal of any remaining portions of the decomposed mass. The patient was restored to health, and survived the operation a year."
Following the case just related, there is no record of any operations having been performed for this condition for more than a century. Calvo 4 reported a case in France in 1714. It will be noticed that all of the cases cited were examples of full term or long retained secondary abdominal pregnancies. The first record of tubal gestation with rupture and the classical symptoms of this accident is that of Riolan, reported in 1604. He relates the case of a lady aged thirty-one, who, with the exception of a hard, slightly painful tumor the size of an egg or clenched hand, situated above the right groin, experienced no unusual complaint until she was about four months pregnant of her eighth child. January 2, 1604, she was seized with violent pain about the pubes, extending from the pelvis to the upper part of the chest, with occasional syncope, which continued till five next morning, when she died. The right fallopian tube was found to have contained a fetus ; but the uterus was healthy and uninjured. The same writer relates a second example of this kind which occurred in 1638, when the patient was three months pregnant. She had such distressing pains for four months that she died in violent convulsions in the seventh month of pregnancy. On dividing the abdominal parietes, the left fallopian tube, much distended, and containing a fetus, presented itself.
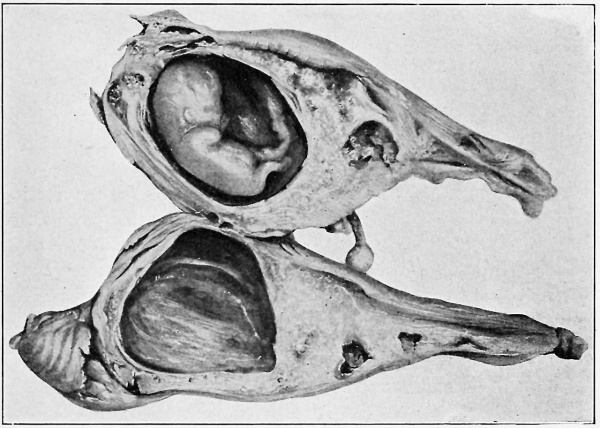
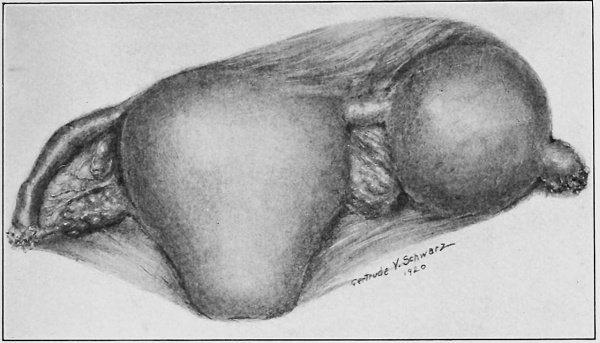
In 1669 that master of obstetrics, Mauriceau, reported a case of ruptured extra-uterine pregnancy, the text of his description being as follows : "History of a woman in whose abdomen there was found, after death, a small fetus about two and one half inches long, together with a great quantity of coagulated blood. The history of this case deserves to be carefully examined into, to decide whether the fetus (as believed by many) was generated in the ejaculatory vessel, called the tube of the womb. On the 6th of January, 1669, in the village Corrari, I saw in the hands of a chirurgus called Benedict Vassal, a uterus, the picture of which is shown at the end of this chapter, which the same chirurgus had a short time before removed from the body of a woman aged 32, who died after three whole days of torture with the most agonizing pains in the stomach, through which she had fallen into frequent fainting spells and the most violent convulsions. This woman had borne eleven children at term, but in her twelfth pregnancy, at about two and one half months, the womb dilated in the direction of the right horn, and, unable to stand distention, ruptured. The fetus was cast out at once and found among the intestines of the mother, with a great quantity of coagulated blood in the whole lower abdomen. Many physicians, chirurgi and other students of nature did as did we ourselves, betook themselves to this chirurgus to see this uterus (which he showed for a prodigy, persuading them that it was formed in the ejaculatory vessel, which Fallopius calls the trumpet of the womb). They believed at once, without any more investigation, that this was just as the said chirurgus told them, and that this case confirmed stories of a like nature narrated by Riolanus. However, I examined the parts of that uterus most carefully and attentively, and it was known to me that those who had fallen into this opinion were in the error whither the chirurgus was leading them, and for this reason, at that very time, I took a drawing of the womb as it then was, and this is the more faithful, true drawing than that which the chirurgus caused to be engraved on brass after an entire month, at a time when the uterus retained almost nothing of its primitive form, and was spoiled by the handling of a thousand men or more who had seen the uterus, pulled it, disturbed it, turned it inside out that they might examine it. Many have brought forward this case to prove to us that the testes (ovaries) of women are full of little ova which, at the moment of coitus, freeing themselves and emerging from the body proper of the testes (ovaries), are borne into the uterus through the tube, afterwards to serve for the generation of the fetus; and one of these so-called ova had by chance remained in the tube of this woman, instead of passing forward into the uterus, and that this was the cause of her death. Regnus Graaf among others holds this opinion, for the confirmation of which he brings forward the figure of this uterus, which he painted from this case which the chirurgus of whom I have spoken had already given to the public ; as one finds it on the 260th page of this book on the generative organs of women; but any who will, carefully and without prejudice, examine the following figure, which is most faithful and faultless, and at the same time examine into our reasons, will find that we have given another demonstration and that we believe that to be the true explanation."
Fig. 3. Mauriceau's Case of Ectopic Pregnancy (from Traite des maladies des femmes, Grones, Paris, 1675).
By studying the illustration, Fig. 3, it is easy to see why this case gave rise to the bitter controversy that followed its publication. It was Mauriceau's contention that generation in man was accomplished by the union of two liquid elements, the male and the female, and that accordingly these liquids only meet and cause fetal development in a large and suitable cavity, as that of the uterus. He held that tubal or ovarian gestation was impossible, and hence proved to his satisfaction that the case referred to was a pregnancy in the uterine horn. Study of the plate merely enhances the confusion, since, while the rupture seems to have taken place in the ampulla of the tube, the location of the right broad ligament makes it evident that the gestation sac must be an elongated uterine cornua. The question, therefore, must perforce remain unsettled.
The first evidence of a true understanding of the cause and the phenomena of extra-uterine pregnancy is found in the works of Pierre Dionis, 5 ' 6 published in 1718. Concerning the cause of tubal pregnancy Dionis says "If the egg be too big, or if the diameter of the tuba fallopiana is too small, the egg stops and can get no farther, but shoots forth and takes root there ; and having the same communication with the blood vessels of the tuba that it would have had with those of the womb, had it fallen into it, is nourished and grows big to such a degree that the membrane of the tuba, being capable of no such dilatation as that of the uterus, breaks at last, and the fetus falls into the cavity of the abdomen, where it sometimes lies dead for many years, and at other times occasions the death of the mothers by breaking open its prison."
Fig. 4. The Case of Pierrre Dionis. The First Case of True Tubal Pregnancy Ever Published (from the English translation of Dionis' Treatise on Midwifery, London, 1718).
This description includes essentially the present day idea of the causation of ectopic gestation, except that Dionis does not recognize the existence of salpingitis as the reason for an obstruction in the tube.
The first recorded case of operation for extra-uterine pregnancy in America is reported by Dr. John Bard, 7 a surgeon of New York, in a communication to the journal, "Medical Observations and Inquiries." Dr. Bard's letter is dated December 25th, 1759, and states in brief the history of a case, in which a Mrs. Stagg, 28 years of age, having had one child without any uncommon symptoms, became a second time pregnant. She was more disordered in this pregnancy than during the first, and at the end of nine months she had some labor pains but no flow of water or other discharge. The pains soon wore off and there remained a large, hard, indolent tumor inclining toward the right side. In five months she conceived again, and at term, after a short and easy labor, was delivered of a healthy child. Five days after delivery she was seized with a violent fever, purging, pain in the tumor and fetid sweats. At the end of the nine weeks, as the tumor developed fluctuation, Bard made an incision through the right rectus muscle, and delivered the suppurating body of a full term fetus. The wound was drained and the patient made a good recovery.
"On January 14th, 1791, this operation was performed upon this side of the Atlantic for the second time, the subject of it being a Mrs. Cocke, the wife of a Virginia planter. The operation, which was done by Dr. William Baynham, a country physician, was entirely successful. The same gentleman operated with the same happy result upon a negro slave on February 6th, 1799. This was the fourth American gastrotomy for the removal of an extra-uterine fetus. The third one was performed by McKnight, and communicated to the famous Dr. Lettsom, by Dr. Mease of Philadelphia, and published in 1795. Dr. Baynham's cases are well worth attentive study. They illustrate the intrepidity and good judgment so often displayed by the provincial surgeon, who, separated by long distances from his fellows, often has to act in the greatest emergencies without the counsel which he may earnestly desire. Almost a quarter of a century passed before the operation was repeated in this country. On the 6th day of October, 1823, it was again performed by Dr. Wishart, likewise a country practitioner. The sixth American operation was performed on February 7th, 1846, by Dr. A. H. Stevens of New York, a man who had all the advantages of a metropolitan experience." (Parry.)
From this time on interest in the subject grew, three varieties of extra-uterine pregnancy being generally admitted to occur, namely, tubal, ovarian, and abdominal. The matter rested here until 1824, when Breschet added what he supposed to be a new one, that which was afterward known as interstitial pregnancy, although Schmitt 8 is generally accredited with publishing the first authentic case of this variety.
In 1837 appeared the very important monograph of Dezeimeris, 9 in which he made a new and complex arrangement of the varieties of ectopic gestation, with a careful study of the pathology.
In 1S42 Campbell's Memoir, which has been so freely quoted here, was published, and since this time there has been a steady increase in the volume of the literature on this matter, most of the essays being valuable contributions, many of them confused and showing marked ignorance of the basic principles involved, and a few teeming with magnificent collections of gorgeous misstatements.
Parry's work, by far the best produced up to his time, and one which inspired much work along the lines of pathology and treatment of extrauterine pregnancy, was published in 1876. Of this book Tait says "It is at once remarkable for its scholarly research and fine critical sagacity. Where he has got astray, has chiefly been by the delusive use of statistics, a point which I shall deal with by and by."
No better appreciation of the amazing advance in the knowledge of intrapelvic pathology, as well as the marvels achieved by modern surgery, can be obtained than by a close reading of Parry's book, published only a little more than four decades ago. In the light of the routine hospital work of today, the facts brought out in this monograph seem to express the thought of 1476, rather than 1876; and to compare the results of treatment then and now must lead every reader to mentally add another star to the galaxy that crowns those two pioneers, to whose bold and scholarly efforts we owe all of the surgical wonders of our time, Pasteur and Lister.
For instance, in speaking of ruptured extra-uterine pregnancy, Parry says "The gravest accident that can happen to the victim of misplaced pregnancy is rupture of the gravid cyst. This is attended with the most alarming symptoms, and frequently terminates in death within a short time. The almost universal opinion of the profession is, that this accident is uniformly fatal, and, if not so, that we have no reliable means" of combating its dangers. True, some have raised their voices and used their pens to advocate surgical interference, but as yet no one has been bold enough to hazard an operation under the circumstances. Operative interference is condemned by the highest authorities upon the subject, and he who would subject a woman under these circumstances to the dangers of gastrotomy would have to possess the courage of McDowell and his immediate followers. The subject, however, is worthy of careful investigation; indeed, this is one of the most practical questions which the student of the clinical history and the results of extra-uterine pregnancy can investigate."
Parry was able to collect from the literature 500 cases of extra uterine pregnancy of all ages, among whom 366 died and 163 recovered, a mortality of 67.20 per cent. In the list of causes of death, rupture of the sac claimed 174 victims, or 53 per cent of the deaths. These figures should in themselves be sufficient to disprove the claims of those who, even today, advise expectant treatment in these cases.
After Parry, came what Bovee well terms the housecleaning work of Lawson Tait, 10 who so definitely established the pathology and treatment of this accident that, in the main, his views are still those accepted by the profession. Curiously enough Tait would not admit the possibility of primary ovarian pregnancy, considering the chance of its occurrence so remote that it might be "regarded as likely as the birth of a blue lion or a swan with two necks, like a heraldic monstrosity — a mere pathological curiosity." Tait's work has been followed by the modern literature, which is still too closely in focus to be regarded from the viewpoint of the historian ; although an account of the epoch making essays on extrauterine pregnancy cannot be closed without mention of the brilliant study of Werth in 1887, in which are laid down the principles followed to this time by every pathologist engaged in the study of specimens of this lesion.
Ovarian pregnancy has long excited the interest of obstetricians, and many amusing and interesting debates have arisen concerning its possibility and mechanism.
The first case so diagnosed was that of Dr. de S. Maurice, communicated by the Abbe de la Roque, and occurring in 1682. This was followed by another example reported in 1697. Velpeau in 1824 denied the possibility of this variety of ectopic gestation, though it was recognized by Dezeimeris.
Tait, as has been shown, waxed satirical regarding the matter, and not until the carefully studied case of Van Tussenbroek was published, did recognition of ovarian pregnancy become universal.
History of Treatment
Laparotomy for the removal of old abdominal fetuses dates from 1500 as has been described, but the treatment of early rupture of a tubal pregnancy is quite another story.
Here again the critical acumen of Parry leads him to conclusions far in advance of the trend of contemporary medical thought. Though himself not a surgeon, his summary of the appropriate treatment of cases of early rupture is masterly; he says "Treatment of Rupture of the Cyst in the early Stages of Pregnancy. In speaking of the result of this pitiless termination of extra-uterine gestation,, it was stated that so few recover from it, that all hope of such a happy result is to be dismissed in considering the treatment. No doubt, notwithstanding the statement of Rogers to the contrary, a few women have recovered, though the number is very small — so small that when one is called to a case of the kind, it is his duty to look upon his unhappy patient as inevitably doomed to die, unless he can by some active measures wrest her from the grave already yawning before her. The history of human injury and disease presents no condition parallel to this one. However fatal the disorder, science and art have found some means of prolonging life or 'smoothing the stormy passage to the grave.' A bleeding vessel, through which the red stream of life is rushing away, can be ligated. A gangrenous limb, which is destroying its possessor by sending its poisonous emanations to the remotest regions of his body, can be amputated. A cancerous breast, which is sapping the vitality of its victim hour by hour, can be removed with the prospect of temporary relief. An aneurism, that places life in constant jeopardy, can often be cured by proximal or distal ligation. The tumultuous action of a heart organically diseased may be quieted till nature restores the balance, after which the person may enjoy a long and even a useful life. Even phthisis now counts its many cures; but here is an accident which may happen to any wife in the most useful period of her existence, which good authorities have said is never cured, and for which, even in this age when science and art boast of such high attainments, no remedy, either medical or surgical, has been tried with a single success. From the middle of the eleventh century, when Albucasis described the first known case of extra-uterine pregnancy, men have doubtless watched the life ebb rapidly from the pale victim of this accident, as the torrent of blood is poured into the abdominal cavity, but have never raised a hand to help her. Surely this is an anomaly, and it has no parallel in the whole history of human injuries. The fact seems incredible, for if one life is saved by active interference, it may be triumphantly pointed to as the first and only instance of the kind on record. In the whole domain of surgery — for we cannot look to other than surgical measures under the circumstances — there is now left no field like this. In this accident, if in any, there is certain death. How often do we see persons recover from injuries which their surgeons tell them will be mortal, jtf they do not submit to a grave and terrible operation, and which with a dogged determination they refuse to have performed, preferring to perish rather than to suffer such grave bodily mutilation; or else, with a keener instinct, they foresee a happier result and get well, notwithstanding the evil prognostications of the surgeon, and in defiance of all the laws which, as man with his fallible knowledge supposes, govern human injuries. But in rupture of an extrauterine fetal sac, in the early stages of pregnancy, a whole lifetime — a whole century — is not enough to enable one person to make two' errors in regard to the prognosis of this accident. The only remedy that can be proposed to rescue a woman under these unfortunate circumstances is gastrotomy — to open the abdomen, tie the bleeding vessels, or to remove the sac entire. This treatment was suggested by Dr. W. W. Harbert, in 1849, an d again by Dr. Stephen Rogers, of New York, in a paper read before the American Medical Association in 1866. The first suggestion of performing gastrotomy to save a woman dying from early rupture of the cyst came, so far as we know, from our countryman, Dr. Harbert, while to Rogers belongs the credit of formulating the arguments in favor of this practice and bringing them prominently before the profession. Since he wrote the same plan of treatment has been advocated by Meadows, Heritt, Greenhalgh, and Playfair, in a discussion before the Obstetrical Society of London. Koberle, Behier, Schroder, and Atlee countenance the proceeding, but no person has yet performed gastrotomy for the relief of this accident. The great impediment to the adoption of this treatment is the uncertainty of diagnosis. It should be remembered that rupture usually occurs before the end of the fourth month, and that in many of these cases the contents of the cyst are discharged and float freely in the blood in the peritoneal cavity. It is also an established fact that in early rupture the most severe hemorrhage occurs in those cases in which the contents of the cyst do not escape, and the blood flows from an orifice, sometimes so minute that this is one of the most singular facts known in connection with extra-uterine pregnancy. This and the well established fatality of the accident warrant the conclusion that the woman's chances of life will not be lessened by enlarging the opening and removing the ovum."
Although abdominal section was first suggested in the treatment of ruptured tubal pregnancy by Dr. Harbert in 1849, the honor of performing the first operation for this emergency went to Lawson Tait in 1883. Deaver 10 describes the event, relating that Mr. Tait had been earnestly solicited to operate for this condition in 1881 by a physician who had correctly diagnosed a case of rupture with internal hemorrhage. He refused, and the patient died shortly after. Unfortunately the first patient operated on died also, but his change of heart was complete and, correctly attributing his failure in the first case to faulty technique, he altered his method and continued to operate upon all such cases. Of the next forty patients only one died. Truly a brilliant record, which was not long in converting the medical fraternity.
It is interesting to note, in this connection, that in 1882 two of America's foremost gynecologists, T. Gaillard Thomas and H. J. Garrigues, 12 in a paper read before the American Gynecological Society strongly advocated the use of electricity in cases of extra-uterine pregnancy, the principle being to destroy the life of the ovum by a strong galvanic current applied to the enlarged tube via the vagina. Both essayists deprecated operative interference in these cases until the period of the viability of the child, when cesarean section was permissible. In the discussion that followed the opinions of the fellows generally were in accord with the paper. Even so late as 1890 we find Howard A. Kelly 13 making the statement, "I have no fault to find with those who use electricity in the earlier months, while holding themselves in readiness to perform an abdominal section upon the appearance of the first untoward symptom. It is well adapted to those cases which have ruptured into the broad ligament, and are very difficult to enucleate. These are cases where we want to stop the growth of the fetus and where we need not be in haste to operate."
The first American operation for ruptured ectopic pregnancy was performed in October 1883 by Dr. Charles K. Briddon of New York. This case was seen in consultation by T. G. Thomas, 14 who describes it. The patient was a woman of twenty-eight, who had borne two children, the last one thirteen months before her present illness. She developed the signs of a ruptured ectopic pregnancy, and Dr. Briddon made a diagnosis and proved its correctness by performing laparotomy and removing the fetus and the ruptured tube. The patient rallied and for a time did well, but at the end of forty-seven hours succumbed to shock.
To illustrate the view of the leaders of gynecological thought at this time, a paragraph from this same paper of Thomas' may well be quoted. He says "The growing triumphs of abdominal surgery are apt to lead to the conviction that laparotomy should, as a rule, be the procedure of election in these cases. From this view I unqualifiedly dissent. In the electrical current we have an infanticide agent of reliable character."
From this time on operative interference in ectopic pregnancy has been the recognized treatment, although in 1907 the experiments of Hunter Robb and the work of his followers tended for a short time to delay surgical intervention. Robb severed the ovarian and uterine arteries in pregnant bitches and found that practically none of his experimental animals succumbed to hemorrhage. From this basis he reasoned that women did not bleed to death from ruptured tubal pregnancies, but did die from the attendant shock, and that, if the shock were properly combated, the patient would react and operation, if at all necessary, could safely be performed after reaction had taken place. These experimerits and the very definite statements of Robb and Simpson of Pittsburg had a profound effect on the profession at large, and the so-called hibernation treatment became common. It has not stood the test of time, however, many patients being lost from hemorrhage while the surgeon waited in vain for the expected reaction, and this plan for the management of these cases has been abandoned to a considerable extent.
Immediate laparotomy is the rule today, although some operators still prefer to observe their very ill patients as to whether they are gaining or losing ground, before resorting to surgical measures for relief.
Literature
1. Bovee, J. W. Ectopic Pregnancy. Am. Jour. Obst., 1910. 61 1583.
2. Cornax, M. Sur les accouchements. 2:61.
3. Primerose, J. De Mulierum Morbis et Symptomatis Libri Quartus, 1594. 4:316.
4. Calvo, P. B. Histoire de l'Academie Royale des Sciences, 1714. p. 29.
5. Dionis, P. Traite general des accouchemens. Paris, 1718. p. 91.
6. Ibid. A General Treatise on Midwifery. Translated by Bell et al. London, 1719.
7. Bard, J. Medical Observations and Inquiries. London, 1764. 2:36.
8. Schmitt. Beob. K.K. Med.-Chir. Akad. zu Wien. 1801. 1 :$.
9. Dezeimeris, J. E. Grossesses extra-uterines. Jr. de conn, med. chir. Jan., 1837.
10. Tait, R. L. Lectures on Ectopic Pregnancy and Pelvic Hematocele. Birmingham, 1888.
11. Deaver, J. B. Sajous' Analytic Cyclopedia of Practical Medicine. 1:184.
12. Thomas, T. G., and Garrigues, H. J. Tr. Am. Gyn. Soc. v. 7.
13. Kelly, H. A. Discussions Bait. Gyn. and Obst. Soc. 1890.
14. Thomas, T. G. Extra-uterine Pregnancy. Tr. Am. Gyn. Soc. 1884. 9:161.
Chapter II. Definition, Frequency, Causes
Definition — Frequency — Race Incidence — Age — The Varieties of Extra-Uterine Gestation — The Relative Frequency — The Causes of Extra-uterine Pregnancy — Obstruction of the Tubal Lumen from Without — Obstruction of the Tubal Lumen from Within — Anomalies of the Tubal Lumen, Accessory Tubes, etc., into which the Ovum Falls — Decidual Reaction of the Tube — The External Migration of the Ovum — The Cause of Ovarian Pregnancy — The Cause of Primary Abdominal Pregnancy — Bibliography.
Definition
Extra-uterine pregnancy or ectopic pregnancy or ecchyesis, may be defined as that condition which arises when a fecundated ovum lodges and imbeds itself in any situation outside the cavity of the uterus, nidation proceeding in the aberrant site for a variable period.
There are several well differentiated varieties of this lesion, as the ovum is arrested and develops in one or another site, the varieties being marked by differences in physical signs, in symptoms, in terminations and in results, as well as the varying reactions of the tissues, in which such abnormal implantation occurs, to the presence of trophoblastic activity.
Frequency
Statistics regarding extra-uterine pregnancy show a constantly increasing frequency of this condition. The older text books, those written before 1900, give a varying proportion of from one in five hundred to one in twelve hundred pregnancies. Winckel saw sixteen cases in twenty-two thousand births and Bandl of Vienna saw but three among sixty thousand births.
By contrast, Wynne reports 303 cases of ectopic pregnancy in 22,688 patients in the gynecological clinic of Johns Hopkins Hospital, an incidence of 1.3 per cent.
These statistics are all presumably valueless in estimating the actual frequency of ectopic gestation, because while some were compiled from the histories of obstetric clinics alone, others, as those of Wynne, show the incidence only in relation to gynecological cases.
In order to ascertain the true relation of the occurrence of extrauterine pregnancy to intra-uterine gestation, the writer obtained the total number of cases of the former variety admitted to the hospitals in the City of Philadelphia, during the year 19 18. If the total number be compared to the number of births registered by the Bureau of Vital Statistics for the same time and covering the same area, an absolute ratio is established, at least for one large city during one year, and for statistical purposes it is fair to assume that this ratio remains fairly constant from year to year. During 191 8 there were admitted to all the hospitals in the corporate limits of the City of Philadelphia 169 cases of ectopic gestation. During the same year there were registered by the Division of Vital Statistics 42,904 living births and 2,049 st iH births, a total of 45,153 and a ratio of ectopic gestation to full time intra-uterine pregnancy of 1 to 267 or .0038 per cent.
These figures are accurate and give the absolute relation of extra- to intra-uterine pregnancy, as reported to the hospitals and the Bureau of Health. In order to utilize them from the standpoint of scientific comparison, however, it is necessary to make certain corrections. Not all cases of extra-uterine pregnancy are admitted to hospitals, some dying at home under a mistaken diagnosis, and some recovering without hospital aid or surgical interference. Therefore it seems proper to arbitrarily add 10 per cent to the total of reported cases of ectopic pregnancy, to allow for the factor of error.
Furthermore, not all intra-uterine pregnancies go to term. In a careful analysis of this matter, Hirst 2 concludes that there is one abortion to every four full time pregnancies.
Abortion and miscarriage are not reported to the Division of Vital Statistics, and in order to reach the proper figures in this regard, it becomes necessary to add one fourth the total number of births, or in this instance, 11,288, to the recorded number, in order to include in the statistics of intra-uterine pregnancies those which terminate before the viability of the child.
The corrected figures for the City of Philadelphia in the year 19 18 would then read :
- Intra-uterine pregnancies 56,441
- Extra-uterine pregnancies 186
- Giving a ratio of 1 to 303 or .0033 per cent.
The increased frequency of ectopic gestation during the past two decades is explained, first, by the fact that, as more cases are constantly being accurately diagnosticated and subjected to operative relief, and fewer women die as a result of erroneous diagnosis, the increase is to a considerable degree a fictitious one and not absolute; second, that, as conservative gynecological operations become more popular, so will subsequent ectopic gestation become more common, since previous pelvic operation is so usual an event in the history of these cases. Such accession in number is, of course, an absolute increase in frequency of extrauterine pregnancy. De Lee states that the condition is more frequent in city than in country practice, but this may be due to the more accurate diagnostic method available in cities and the more general hospitalization of patients in urban communities.
Repetition of the accident in the same tube, and not uncommonly in the other tube in the same individual, has been reported, and intrauterine and extra-uterine gestation may coexist.
Race Incidence
In the United States, at least, race seems to be a negligible factor with regard to the occurrence of extra-uterine pregnancy. Statistics vary as to its prevalence among whites and negroes, according to the locality from which the figures are taken. In the south and along the Atlantic seaboard the lesion is frequently found in the colored race. (Wynne, in 303 cases studied at Johns Hopkins Hospital, found 202 to be among the white race and 10 1 occurred in negroes.) In the western portion of the country there are but few recorded cases among negroes, due, naturally, to the small element of this race among the population.
Age
Extra-uterine pregnancy being solely a disease of the child bearing period, its age incidence is necessarily limited.
Farrar's 3 statistics in a series of 262 cases showed that the ages ranged from seventeen to forty-two years and 63 per cent of the series were between the ages of twenty-four and thirty-three years inclusive.
Wynne 1 found in 303 cases 61 per cent occurring during the decade, twenty-four to thirty-three years inclusive. In the writer's series of cases, 70 per cent occurred in this decade.
The most frequent age for the development of ectopic gestation, then, is the decade between twenty-four and thirty-three years, and, as most American girls marry in their early twenties, it follows that the majority of these cases occur within the first ten years of married life.
This fact is significant, in view of the commonly repeated statement that extra-uterine pregnancy occurs most commonly after a prolonged period of sterility, or at least unfruitfulness.
The Varieties of Extra-uterine Gestation. — An ovum may be arrested anywhere in its passage from the ovary to the uterine cavity, and may imbed in any portion of the genital tract distal to this cavity; hence the several varieties of ectopic gestation are to be considered solely in relation to that portion of the genital tract in which the aberrantly situated ovum imbeds and develops.
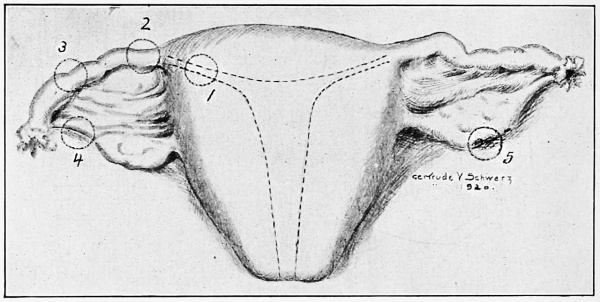
This classification is based upon the original point of implantation of the fertilized ovum. When nidation proceeds at the point of first arrest, it is designated as primary extra-uterine pregnancy ; when its position is changed by rupture or further development, it is designated as secondary. Beginning at the uterus, there may be a cornual, interstitial, or apical pregnancy when growth of the impregnated ovum proceeds within the thickness of the uterine wall in the tubal lumen; isthmial, when the arrest takes place in the constricted isthmus of the tube; ampullar, when embryological development goes on in the expanded, trumpet shaped ampulla of the tube ; tubo-ovarian when the abnormal site is at the fimbriated extremity of the tube, which is in these cases attached to the ovary by preexisting adhesions. Ovarian pregnancy, the rarest of the primary forms, occurs when the ovum is fertilized without having been extruded from the graafian follicle, the development continuing within the cortex of the ovary (Fig. 5).
Fig. 5. The Sites of Implantation of the Ovum in Extra-uterine Pregnancy. 1. Interstitial or Cornual; 2. Isthmial; 3. Ampullar; 4. Tubo-ovarian; 5. Ovarian.
Primary abdominal pregnancy, when the ovum is fecundated while free in the peritoneal cavity and implants itself upon any tissue with which it may come in contact, is a theoretical possibility. In the older literature this variety is commonly noted, but Werth demonstrated that the clinical cases reckoned as such were all tubal in their origin.
As a result of rupture or extrusion from the original site, the primary forms may undergo changes in site, development going on to greater or less degree in the secondary location. Thus an interstitial pregnancy may, by muscular action, be forced into the uterine cavity and grow as a secondary intra-uterine pregnancy, or, it may, in common with any of the tubal forms, become abdominal, that is, either the fetus alive, is extruded from a rupture in the sac, the placenta continuing to develop in its original site, or the entire ovum may escape into the abdominal cavity, the placenta becoming reimplanted on some vascular intra-abdominal tissue with continued growth of the embryo. The same change may take place in primary ovarian pregnancy.
Interstitial .... may become
Tubal ., . ;. . may become
The following table, taken from Kelly, 4 clearly shows the changes which each of the primary forms may undergo.
Primary Forms Secondary Forms
'Intra-uterine, Abdominal, Intraligamentary.
'Abortion, Tubo-abdominal, Tubo-ovarian, Abdominal,
Llntraligamentary.
Ovarian .... may become .... Abdominal.
The Relative Frequency of the various forms of ectopic pregnancy is somewhat, difficult to determine, as statistics are usually mute on this point. The interstitial variety appears to be the rarest of the tubal forms.
Rosenthal 5 found it to occur in 30 per cent of 1324 cases of ectopic pregnancy collected by him. This estimate seems very high. Weimbrenner 6 collected only 35 cases up to 1904. The old analysis of J J cases observed by A. Martin (quoted by Kelly 4 ) is as follows:
Ampullar 48
Isthmial . . 8
Interstitial 1
Intraligamentary 7
Tubo-ovarian 6
Tubo-abdominal 3
Ovarian 1
Undetermined 3
In a study of 106 cases, Oastler 7 found the following sites :
Inner half of tube (isthmial) 38
Outer half of tube (ampullar) 32
Interstitial 2
Ovarian 2
Not obtainable 32
A study of 1 17 cases by Foskett 8 shows the pregnancy to have been :
Ampullar in 52
Isthmial in 64
Interstitial in 1
These statistics show considerable variation; but a survey of them demonstrates the fact that isthmial pregnancy is slightly more common than ampullar, interstitial is rare, as is abdominal of the various types, while ovarian pregnancy is very seldom met with. The tubes are affected with almost equal relative frequency, though there is a widespread belief that the right is more commonly involved. This is in error, as shown by the following review of case groups :
Tube Affected
OASTLER
FARRAR
BOVEE
FRANK
FOSKETT
WILLIAMS
Total
Right
Left
54 46
2
I48
I4O
I
28 31
23 29
43 74
69
53 1
365
373
4
Both
The Causes of Extra-Uterine Pregnancy
The causative factors leading to the ectopic implantation of an ovum are of various natures, usually indeterminate in the individual case, and discussion and speculation upon these details has developed an enormous literature, but with no specific pathology as yet remaining unchallenged, applicable to the condition as a whole.
Out of the mass of theory and clinicopathological facts presented, a series of factors, any one of which, or a combination of several, when operative, may result in ectopic implantation of the ovum, have been generally accepted as true causative agents. The difficulties in arriving at the true cause lie largely in the fact that the pathologist is rarely able to make his observations until the condition has progressed so far that the original anatomical features have been obliterated, or so altered that the recognition of the factors predisposing to the starting or development of the tubal pregnancy are obscured or rendered imperceptible. The importance of careful study of all specimens with regard to the etiology is well brought out by Williams 9 when he says that, despite the existence of seemingly insuperable difficulties, it is our duty to continue our researches in this almost unknown field, for not until we clearly understand the predisposing factor, or factors, which bring about an ectopic gestation, can we hope to institute a more intelligent preventive treatment that will result in a lessened morbidity, or at least a lessened mortality. In general, however observers may differ as to the cause of ectopic pregnancy, it is universally held that this cause must lie in some interference with the passage of the ovum from the fimbriated extremity of the tube to the uterine cavity.
Such interferences may result from :
1. Obstruction of the tubal lumen from without.
2. Obstruction of the tubal lumen from within.
3. Anomalies of the tubal lumen, accessory tubes, etc., into which the ovum falls and can henceforward be propelled no further.
4. Decidual reaction in the tube.
5. The growth of a fertilized ovum outside the tube to such ex tent that, when the ovum does finally enter the tube, its size precludes its transit through the lumen (external emigration of ovum).
1. Obstruction of the Tubal Lumen from Without. — Taking up these primary causes in detail, the obstruction of the tubal lumen from without may originate in :
a. Peritubal adhesions, causing strictures or kink.
b. Constriction resulting from presence of a tumor of neighbor ing organs, as a cornual fibroma, ovarian or parovarian cysts, etc.
(a) Peritubal adhesions are of frequent occurrence, being the end result of a perisalpingitis, whose etiology may be either of intratubal origin or an inflammation by contiguity following appendicitis, diverticulitis or a general peritonitis from rupture of a gastric or intestinal ulcer.
A case of the writer's well illustrates this etiology. A woman of 36, who had previously suffered from a violent suppurative appendicitis with long continued abdominal drainage, developed an ectopic pregnancy in the right tube, which ruptured at about the fourth week of pregnancy. The tube was removed, the patient making an uneventful convalescence. On examination of the specimen, the pregnancy was found to be ampullar in type, the rupture having taken place on the superior aspect. The entire tube was bound down by dense adhesions, and just distal to the gestation sac there was found a sharp angulation of the tube, the kink being held securely in place by a broad, firm band of adhesion. On section there was nowhere apparent any evidence of endosalpingitis.
Conservative gynecological operations, performed for the relief of sterility or to cure a train of symptoms dependent on such peritubal adhesions, are in themselves strong predisposing factors to the subsequent development of ectopic pregnancy.
Thus Giles 10 reports 125 cases wherein conservative operations had previously been performed. Of these, 33 or 26 per cent became pregnant later, and of the pregnancies, eignt or 24 per cent were extra-uterine.
In Norris' 1X series of 68 cases, two were subsequently operated upon for ectopic pregnancy, and Norris pertinently remarks that, if tubal pregnancy is particularly prone to follow conservative operations, this factor must be taken into consideration in all conservative operations on married women of child bearing age.
(b) Constriction resulting from pressure of a tumor of neighboring structures, without inflammatory changes in the tube. Such purely mechanical obstruction of the lumen of the tubes is a well known cause of tubal pregnancy, although clinically uncommon. A typical case is reported by Gardner. 12 Gardner studied one case of tubal pregnancy, which was associated with a large uterine fibroid, and the pregnant tube was found crowded down in the pelvis, under the tumor. Microscopically as well as macroscopically there were no evidence of any present or past inflammatory change whatever.
2. Obstruction of the Tubal Lumen from Within seems in the last analysis to underlie the vast majority of all tubal pregnancies. It has been definitely learned that the direction of the ciliary current in the tube is toward the uterus, the function of the cilia being to assist the peristaltic action of the tubal musculature to promote the transit of the ovum to the uterine cavity. Recent observations render it almost a certainty that fertilization of the ovum normally occurs in the tube, and if, therefore, any marked diminution in the size of the tubal passageway has taken place, or if the cilia have been destroyed by inflammatory process, there may easily result a temporary arrest of the fecundated ovum at the point of greatest resistance to its passage. This arrest, acting for but a short time, will permit the rapidly growing embryo to attain such dimensions that under no circumstances could it penetrate the constricted area, even though tubal peristaltic contraction becomes very powerful.
The most common morbid process in the production of strictures in the tube or destructions of its epithelial coat is some form of salpingitis, notably gonorrhea, by reason of the prevalence of this infection.
Williams 9 states definitely that in all his specimens evidences of an inflammatory reaction, which had preceded the onset of the ectopic gestation, were demonstrable, and further, these inflammatory changes in all cases where both tubes were removed were shown microscopically to be bilateral, and diverticula were present, not only in the tube which lodged the ovum, but also in the opposite one.
Williams holds that in such cases of old salpingitis there are present epithelial lined, false diverticula, open at the distal and closed at the mesial end, these diverticula being formed by a coalescence and cohesion of the tubal mucosa. The complete or partial absence of cilia, or the infiltration and alteration of the tubal wall, resulting from inflammatory change, as a consequence of which peristalsis is impeded, are contributing factors, but are in themselves insufficient to produce an absolute barrier to the passage of the ovum. If, however, the ovum enters one of the false diverticula, closed at the mesial end, its progress is effectually checked.
This view as to causation is strongly upheld by Opitz, 13 who, on making serial sections of the tubes in 23 cases of ectopic pregnancy, found these canals or false passages present in every instance.
The severity of the inflammatory change in the tube and the progress made toward healing of the lesion are important with respect to the etiology of tubal pregnancy. In a well considered article Mall 14 points out that, if the ovum within the tube contains a normal embryo, there is but little adjacent inflammation; but if it. contains a pathological embryo, the changes in the tubal wall are usually marked, and when the ovum is well disintegrated, the changes are still more pronounced. Read in the other way, this would mean that, if the inflammatory condition is nearly healed, the ovum implants itself in the tube and grows normally; but if the results of infection are still pronounced, the ovum rapidly disintegrates. Such an inflammation is signalized, not only by an inflammatory reaction in the tubal wall, but also by very pronounced changes within the tube lumen, the most common of which is a hypertrophy and adhesion of the tubal folds, the so-called follicular salpingitis.
This observation is of clinical importance, in that it confirms the view that in the presence of acute or subacute salpingitis, ectopic pregnancy does not occur, while it does take place when the inflammatory process is subsiding; and it is fair to assume that, had the ectopic pregnancy not developed at this time, the tube would probably have become completely healed within a few years, thus permitting the fertilized ovum to reach the uterus.
3. Anomalies of the Tubal Lumen, Accessory Tubes, etc., into which the ovum falls. 4. Decidual Reaction in the Tube. — • Congenital, as distinguished from postinflammatory anomalies of the tube, are regarded by many investigators as being the chief cause of ectopic pregnancy, especially if the existence of rudimentary mullerian tissue in the tubal wall be considered as a congenital anomaly. Webster 15 first laid down the rule that the ovum always imbeds in mullerian tissue. When the hypothesis was first formulated he held that all ectopic pregnancies were primarily tubal, but when the indisputable fact, that primary ovarian pregnancy could and did occur, was brought to his notice, Webster amplified his theory to include such a happening by stating that mullerian rests could occur in the ovary, and that ovarian pregnancy must take place in such rest. This theory does not explain the development of primary abdominal pregnancy, but no really authentic case of this variety, which has withstood all criticism, has been recorded.
Hirst and Knipe 16 report a case which seems to meet all the requirements, but as the tube and ovaries were not removed at operation and hence not subjected to microscopical study, the case has been attacked. Therefore, inasmuch as primary peritoneal imbedding has not been satisfactorily demonstrated, Webster's theory is not weakened thereby.
This hypothesis, reduced to its lowest terms, is that under certain conditions an ovum may imbed in an aberrant site because, and only because, that site contains cells, originally derived from the mullerian ducts, which, having passed through a stage of evolution, later revert to their original type and reacquire their genetic function or the property of forming decidua.
This hypothesis has been modified and advanced again by Huffman, 17 who states as his theory that ectopic pregnancy is determined by an anomalous imbedding area. At present it is impossible to recognize the anatomical factors which are necessary to an imbedding area, but it may be assumed that the special tissue may become misplaced during the development of the tubes and uterus from the mullerian ducts. There is a mutual relationship of imbedding area and fecundated ovum.
In a later article 18 this author states that he has examined 68 specimens of tubal pregnancy, and, in spite of the difficulties of examining torn and sometimes incomplete material, he has found malformations in 54 per cent of them. This evidence, besides the negative findings in regard to any obstruction or inflammation, is sufficient to warrant the establishment of the anomalous imbedding area theory, in Huffman's opinion the most logical of all the explanations for ectopic pregnancy.
Both Webster's and Huffman's hypotheses are attractive, but unsatisfactory for certain cases, first, in that it has been shown, as pointed out by Williams, that the decidua does not play nearly so important a part in tubal pregnancy as was formerly supposed; second, that it does not account for the very many specimens, indeed in the opinion of the writer, the great majority, wherein marked evidence of preexisting tubal inflammation with destruction of mucosa, inflammatory diverticula, obstructions by exudate, etc., are associated with tubal pregnancy, with a total absence of any demonstrable anomalous imbedding area.
Concerning Huffman's views that malformation of the tubes, accessory ostia, congenital diverticula, etc., are responsible, it is not quite clear just why the presence of such malformation should predicate the existence of primitive miillerian tissue. Further, if this hypothesis were true, it should logically be expected that most cases of ectopic pregnancy should occur in primiparae, with whom decidual reaction is most intense, whereas the reverse is the fact.
Fig, 6. — Polypoid Chondrofibroma of the Fallopian Tube, Associated with Tubal Pregnancy. From Outerbridge.
5. The External Migration of the Ovum. — External migration of the impregnated ovum from its graafian follicle, across the peritoneal cavity, to enter the opposite tube, the tube on the same side being absent or impervious, has been advanced as a cause of tubal pregnancy % As an etiological factor this phenomenon does not seem to be of much importance.
Besides this group of usual causes, there are recorded occasional cases due to other factors. Tumors of the tube are found sometimes in definite relationship to this lesion. In a case of Outerbridge 19 there was found in a tube removed on account of an early tubal pregnancy, a small, somewhat papillary growth practically filling the lumen, just proximal to the placental area. Microscopic examination of the tumor showed it to be a somewhat degenerated chondrofibroma, which had been connected to the tubal wall by a narrow pedicle. (Figs. 6, 7, 8.)
A similar case, of a pedunculated, submucous fibroma, measuring about 4.5 x 3 inches, situated just at the tubo-uterine opening, which is partly occluded, is reported by Wettergren. 20 This tumor was associated with a tubal pregnancy, which the author considered in all probability due to the partial obstruction of the tube by the tumor.
Fig. 7. — Chondrofibroma of Fallopian Tube. From Outerbridge.
Tubal polyps were ascribed as common causal agents by the earlier writers, but subsequent investigations have proved them to be of infrequent occurrence. Cases have been reported by Beck, Breslau, Leopold (two cases) and Wydn, all of whom discuss the possibility of the tumor having formed a mechanical hindrance to the entrance of the ovum into the uterus. In several of these cases a distinct decidual reaction was present, and Ahlfeld indeed has advanced the contention that these polyps represent merely proliferations of tubal decidua, secondary to the pregnancy, and are therefore not to be considered a causative factor in the localization of this in the tube (Outerbridge 19 )-.
There are several other possible causal agencies, all of which are purely conjectural but of much interest, as, for example, the view that monstrous or deformed ova are themselves responsible for their abnormal imbedding, since they do not possess the required motility to progress along the tube. As the motility of the young ovum has not been demonstrated to exist, this view cannot as yet be supported. Again, it is thought by some observers that the ovum in transit through the tube derives its nutriment from some tubal secretion, and that, under certain conditions, the tube may secrete substances toxic to the ovum, which is thereby impaired as to its vitality and ability to progress toward the uterus.
Fig. 8. — Chondrofibroma of Fallopian Tube. From Outerbridge.
Schil 21 advances a new theory as to the causation of extra-uterine pregnancy, believing that the essential factor is a failure of the unstriped muscle fibers of the tube to contract, so that the ovum does not pass into the uterus. What the factors are that prevent the contraction is not stated, and the observation lacks confirmation.
In summing up the probable causes of ectopic gestation, it is true that no one or even several causative agents have been satisfactorily demonstrated. From his own observation, however, and from a study of the literature, it is the opinion of the writer that the usual cause is the widely accepted and simple one of some mechanical arrest of the fecundated ovum during its tubal journey, and that such arrest is most commonly brought about by the end results of tubal inflammation or by pressure from neighboring neoplasms.
The readiness of the young ovum to implant itself is shown by the rapidity with which secondary implantation takes place when a living ovum is extruded from a tube, either by rupture or tubal abortion. This is well illustrated by a recent case occurring in the writer's clinic. A woman of 32, who had borne one child, developed the usual signs of a ruptured ectopic pregnancy. She reacted from the initial traumatism
Fig. 9. — Secondary Implantation of an Ovum on a Knuckle of the Ileum, Ten Days after the Rupture of a Tubal Pregnancy (author's case).
and was kept at home for six days, when, symptoms of intestinal obstruction supervening, she was referred to the Frankford Hospital. On examination there was found a tympanitic abdomen, with obstruction to the passage of feces, though flatus was expelled. Douglas' pouch was bulging and doughy. On operation there was found a ruptured tubal pregnancy, isthmial in character, of the right tube. The ovum, 1 inch in diameter, had imbedded itself in the angle of a coil of ileum, and in six days had become so firmly attached that the bowel was angulated and obstructed, and the villi had so deeply entrenched themselves that, upon separation of the ovum from the intestine, the mucosa of the bowel was exposed, with free hemorrhage necessitating suture. (Fig. 9.) In general, then, the inflammatory theory of the causation of ectopic pregnancy should receive first consideration. Further observations along this line will be awaited with the greatest interest.
The Cause of Ovarian Pregnancy
This rare and interesting variety of ectopic gestation has not been reported in sufficient numbers to formulate any specific cause, histologically demonstrable. Leopold 22 has suggested that, in a certain proportion of cases, a centrally located follicle may rupture into a more superficially located one, the ovum in the former not being expelled, but being fertilized in its original location by a spermatozoon, which has gained access through the superficial follicle.
Hewetson and Lloyd 23 believe that, after fertilization, the phagocytic ovum may burrow into another or deeper portion of the ovary. Norris 24 holds the spermatozoon finds its way into a recently ruptured graafian follicle and fertilizes the ovum in situ. In connection with Webster's decidual reaction theory, as applied to ovarian pregnancy, Norris points out that, in the cases of this condition reported up to 1890, but few are found that record the presence of decidua-like cells, and in these the identification of the latter is somewhat doubtful. Having not had the opportunity of studying a specimen of ovarian pregnancy, the writer has no personal opinion as to its causation.
The Cause of Primary Abdominal Pregnancy, like its very existence, remains in obscurity and requires no further mention.
Literature
1. Wynne, H. M. N. Bui. J. Hopk. Hosp., 1919, 30:15.
2. Hirst, B. C. Textbook of Obstetrics. Philadelphia.
3. Farrar, L. K. P. An Analysis of 309 Cases of Ectopic Gestation. Am. Jr. Obst. 1919. 79 733 4. Kelly, H. A. Operative Gynecology. New York, 1902. 2 434.
5. Rosenthal. Ein Fall Intramuraler Schwangerschaft. Centrbl. f. Gyn. 1896. 20:1297.
6. Weimbrenner. Uber Interstitielle Schwangerschaft. Ztschr. f. Gebh. u. Gyn. 1904. 51:57.
7. Oastler, T. R. Ectopic Pregnancy. Surg. Gyn. Obst. 1917. 24:224.
8. Foskett, E. Am. Jr. Obst. 1916. 74:232.
9. Williams, C. D. Etiology of Ectopic Gestation. Surg. Gyn. Obst. 1908. 7:519.
10. Giles, A. E. A Study of the After Results of Abdominal Opera tions on the Pelvic Organs. Jr. Obst. Gyn. Brit. Emp. 1910.
17, 153 11. Norris, C. C. Gonorrhea in 'Women. Philadelphia, 1913. p. 307.
12. Gardner, W. S. The Cause of Tubal Pregnancy. West Virg. Med. Jr. 1918. 12 :37c
13. Opitz. Ztschr. f. Gebh. u. Gyn. 1903. b. 48.
14. Mall, F. P. The Cause of Tubal Pregnancy and the Fate of the Enclosed Ovum. Surg. Gyn. Obst. 1915. 21 1289.
15. Webster, J. C. Ectopic Pregnancy. Edinburgh, 1895.
16. Hirst, B. C, and Knipe, N. Primary Implantation in an Ovum in the Pelvic Peritoneum. Surg. Gyn. Obst. 1908. 7:456.
17. Huffman, O. V. Ectopic Pregnancy Associated with Anomalies of the Fallopian Tubes. Surg. Gyn. Obst. 1913. 16:548.
18. A Theory of the Cause of Ectopic Pregnancy. Jr. Am. Med. A. 1913. 61:2130.
19. Outerbridge, G. W. Polypoid Chondrofibroma of the Fallopian Tube Associated with Tubal Pregnancy. Am. Jr. Obst. 19 14. 70:173.
20. Wettergren. Gros polype fibromyomatique de la trompe, decou vert en cours d'une operation de grossesse tubale. Nord. Med. Ark. 1901. 34:1. Quoted by Outerbridge.
21. Schil, M. Jr. de Med. de Paris. 1914. No. 17.
22. Leopold. Arch. f. Gyn. 1882. 19:210. Quoted by Norris.
23. Hewetson and Lloyd. Brit. Med. Jr. 1906. 568.
24. Norris, C. C. Primary Ovarian Pregnancy. Surg. Gyn. Obst. 1909. 9:123.
Chapter III. The Terminations of Ectopic Pregnancy
Termination by Resorption of the Ovum — Death of the Embryo with the Formation of Tubal Mole — Tubal Abortion — Rupture of the Pregnant Tube — Rupture Between the Folds of the Broad Ligament — The Growth and Development of the Fetus to Full Term, While Still Confined Within the Tube — Interstitial Pregnancy May Terminate by Gradual Growth of the Fetus Into the Uterine Cavity — Tubo-Abdominal Pregnancy — Secondary Abdominal Pregnancy — Tubo-Ovarian Pregnancy — Intraligamentary Pregnancy — Ovario-Abdominal Pregnancy — Abdominal Pregnancy Secondary to Primary Ovarian Pregnancy — Resorption and Tubal Mole — Hematocele — Solitary Hematocele — Infected Hematocele — The Terminal Changes — Bibliography.
Tubal pregnancy may primarily eventuate in :
i. Early death of the ovum with complete resorption and a restoration of the tube to its prepregnant condition.
2. Death of the embryo with the formation of tubal mole.
3. Tubal abortion.
4. Rupture of the pregnant tube, either into the peritoneal cavity or between the folds of the broad ligament.
5. The growth and development of the embryo may proceed to term, when either the fetus dies as a result of nutritional failure, or is delivered by abdominal section.
6. If the pregnancy be interstitial, the fetus may gradually be extruded into the uterine cavity, the placenta remaining attached to the cornual wall, and the pregnancy may terminate by spontaneous vaginal delivery, as in normal intra-uterine gestation, the placenta being also spontaneously expelled.
These are the primary terminations of tubal pregnancy.
Secondarily, the embryo may be expelled from the tube and the placenta remain behind, the pregnancy going to term, with the fetus free m the abdominal cavity and the placenta implanted in the tube — the socalled tubo-ovarian pregnancy. Or, the entire living ovum may be expelled, the placenta reattaching itself to any tissue within the peritoneal cavity and pregnancy then going on to term — secondary abdominal pregnancy. In either of these instances the fetus, unless removed by laparotomy, dies, and proceeds to suppuration and necrosis, lithopedion formation, mummification, or adipocere. Practically speaking, unless terminated by surgical intervention, every case of ectopic pregnancy results fatally for the child, except the rare case of secondary uterine gestation following a primary interstitial implantation of the ovum. The terminations of ovarian pregnancy are: i. Rupture into the peritoneal cavity with hemorrhage and death of the fetus.
Fig. 10. — A Tubal Mole. All gross evidence of pregnancy has disappeared, the
distended tube being filled with organized clot. On microscopical examination,
distinct placental shadows could be seen in the tube wall (author's case).
2. Rupture of the sac with secondary ovario-abdominal pregnancy; the placenta remains attached to the ovarian parenchyma.
3. Rupture with secondary attachment of the ovum — abdominal pregnancy secondary to primary ovarian gestation.
I. Termination by Resorption of the Ovum takes place, in the opinion of the author, much more frequently than is commonly believed. In taking detailed histories of gynecological cases when some operation is contemplated for relief of pelvic symptoms, it is not uncommon to elicit an account of a train of symptoms' strongly suggestive of the existence of an ectopic pregnancy at some past period of the woman's life. When, upon subsequent laparotomy, no evidence whatever is found of any lesion of the tubes, or when a small, nodular area of fibrosis exists in one tube, the fact that resorption of an extra-uterine embryo has at some time taken place is at least suggestive.
Furthermore, the finding of small, absorbing tubal moles, upon the examination of certain excised tubes, lends additional plausibility to this form of termination of extra-uterine pregnancy. Nothing more definite than the foregoing facts is available, but it seems reasonable in the face of such evidence to consider death and resorption of the ovum as one mode of termination in these cases.
2. Death of the Embryo with the Formation of Tubal Mole. — A tubal mole results when the fetus dies in the intact tube, with marked hemorrhage about it and between its membranes. At the same time the liquor amnii is absorbed, the blood more or less organized, and a structure produced which is identical with the moles occurring in uterine pregnancy. Such moles may vary markedly in size, according to the age of the pregnancy and the amount of hemorrhage, and may be retained in the tube for an indefinite period (H. A. Kelly). (Fig. 10, Fig. 11.)
3. Tubal Abortion, one of the two most common terminations of extra-uterine pregnancy, occurs when the ovum becomes detached from its imbedding site in the tube and is expelled from the fimbriated extremity of the tube by tubal muscular contraction, the abortion being complete when the ovum and its envelopes are entirely extruded from the
Fig. 11. — A Tubal Mole, the Fetus Still Intact, but Undergoing Degeneration. Tube greatly distended, but not ruptured. A large blood clot separates the fetal envelope from the tube wall.
Fig. 12. — Section of a Tube Showing Incomplete Tubal Abortion. The embryo
in its sac, which is surrounded by a large clot, is seen partially extruded
from the enormously distended fimbriated extremity (a). The uterine end of
the tube is shown at b (case of Dr. J. M. Baldy).
Fig. 13. — A Tube Removed a Few Hours after Complete Tubal Abortion Had
Taken Place. Note the enormously hypertrophied and distended fimbriae at a.
tube and fall into the abdominal cavity, and incomplete when only a portion of the sac protrudes from the free end of the tube, the remainder being still confined within the tube walls. (Fig. 12.)
Tubal abortion is usually accompanied by severe hemorrhage, and clinically cannot be differentiated from rupture of the tube, although occasional cases are recorded where the hemorrhage was negligible in amount. The possibility of this termination of extra-uterine pregnancy was first expressed by Werth 1 and it has come to be believed that this is the most frequent outcome of tubal pregnancy (Fig. 13).* Opinions as to the relative frequency of abortion and tubal rupture vary within wide limits, as will be shown later in discussing this phase of the subject.
According to Martin 2 this termination is the general rule, spontaneous rupture occurring only in those cases in which occlusion of the abdominal end of the tube precludes the possibility of an abortion, or in which the ovum, being inserted in a hernia of mucosa, burrows directly through the tube wall.
4. Rupture of the Pregnant Tube. — (a) Into the Peritoneal Cavity. — According to many authorities rupture is the most usual mode of termination of a tubal pregnancy. Such accident happens usually before the twelfth week, most commonly, in the opinion of the writer, before the eighth week following conception. Naturally ruptures occur in almost a direct ratio to the site of implantation of the ovum. Ampullar pregnancies are far more prone to end by tubal abortion than by rupture; midtube pregnancies terminate almost equally by these two accidents, while in isthmial and interstitial pregnancies, the tube usually suffers a rupture of its wall. The tear in the tube is commonly over the site of the developing placenta, and, when intraperitoneal, takes place on the free aspect of the tube.
The older writers considered this accident to be due to a simple overdistention of the tube wall beyond the point of its elastic resistance. Close study of the pathology led to a change in thought, and it was held that the rupture was always due to perforation of the tube wall by proliferating syncytial cells.
My own view is that a combination of these factors brings about the lesion, an area of the tube wall becoming thinned out and weakened by the erosive action of the syncytium, and, being the point of least resistance, yielding to the pressure of the growing ovum, or more commonly to the accumulated mass of blood clot gathering in and about the oval sac.
Attention has been called to the divergent views held as to the relative frequency of tubal abortion and tubal rupture. In 1892 Schrenck found only six cases of abortion in 610 cases of tubal pregnancy, while the reports of Martin, Wormser, Fehling, Zletsch, and Mandle and Schmidt (quoted by J. W. Williams), comprising 289 cases, show that 78 per cent ended by abortion and only 22 per cent by rupture. Modern statistics also vary very greatly, as is shown by the following table :
No. OF
Tubal
Other
CASES
Ruptures
ABORTIONS
TERMINATIONS
1 06
21
55
30
117
49
64
4
59
20
25
14
76
42
20
16
309
169
81
59
Oastler, q. v . . Foskett, q. v. Williams, q. v Frank, q. v. . Farrar, q. v . .
To glance at these figures is to be convinced that the relative frequency of these two terminations of tubal pregnancy has by no means been determined. It is somewhat difficult to reconcile the wide difference in the statistics, all made by expert and painstaking observers, with abundant laboratory facilities for the verification of any doubtful specimens. The individual experience of various gynecologists differs greatly
Fig. 14. — Rupture of a Pregnant Tube Occurring Subsequently to the Development of Tubal Abortion. At a is seen a portion of the clot surrounding the
embryo, being extruded from the fimbriated extremity of the tube, while at b
is a secondary point of rupture, which was bleeding freely at operation (author's
case).
in this respect, and until very large groups of cases are collectively studied, no accurate estimation as to the relative frequency of tubal abortion and tubal rupture can be made.
So far as the writer's personal observation goes, rupture occurs with nearly double the frequency of tubal abortion.
Very many cases, which at first partake of the nature of an abortion, proceed to secondary rupture of the tube, as the blood accumulates about the ovum faster than the propulsive forces of the contracting tubal musculature and the vis a tergo of the blood behind the ovum can act to expel the latter through the fimbriated extremity; and rupture finally occurs by reason of overdistention of the tube, especially if the fimbriated end be occluded by old inflammatory processes and the extrusion of the embryo through the abdominal ostium is thereby impeded. Fig. 14.
Such cases, if seen early, soon after the development of symptoms, and immediately operated upon, will be listed as tubal abortion, whereas in clinics wherein immediate operation is not practiced, or in communities where, by reason of the attitude of the local practitioners, these cases are not promptly removed to hospitals, time is given for secondary rupture to take place and the cases are accordingly listed as tubal ruptures. This situation will serve to explain the variance of statistics in part, but is not sufficient to entirely reconcile the discrepancies that exist.
The amount of the hemorrhage, in cases of rupture of the tube, is in general greater than where tubal abortion has taken place, and varies with the location of the rupture. The nearer the uterus, the more severe the hemorrhage, is the rule. Inasmuch as most ruptures occur among isthmial or interstitial pregnancies, it follows that bleeding following this accident is generally profuse. The rupture of an interstitial pregnancy results almost always in excessive bleeding, sufficient to cause a fatal termination in most instances, unless checked by immediate surgical interference. On the other hand, there are on record cases of tubal rupture accompanied by but slight hemorrhage. This is especially true where the site of the laceration is on the posterior aspect of the tube at its middle third, where the blood supply is limited to the smaller arterioles.
(b) Rupture Between the Folds of the Broad Ligament. — In exceptional cases the tube may rupture along its inferior aspect, through the mesosalpinx, the hemorrhage thus taking place in the extraperitoneal portion of the tube, and dissecting between the layers of the broad ligament.
This type of rupture may eventuate in the death of the embryo and the formation of a broad ligament hematoma, or by the further development of the embryo as a secondary broad ligament pregnancy (exceedingly rare), or, if the tension created by the extravasated blood be sufficiently great, there may occur a secondary rupture of the broad ligament, the blood eventually escaping into the peritoneal cavity.
This variety of rupture is rarely attended by severe hemorrhage, and from the clinical standpoint is to be regarded as by far the most favorable type with regard to the welfare of the patient.
When the growth of the embryo continues after its escape into the broad ligament, the future course depends largely upon the degree of completeness with which the placenta has been separated from its tubal attachment, as pointed out by J. W. Williams, who states that, if the placenta remains attached to the tube on the side opposite the point of rupture, it generally becomes displaced upward as pregnancy advances, and comes to lie above the fetus; but when it is situated near the point of rupture, it gradually extends down between the folds of the broad ligament, being implanted partly upon the tube and partly upon the pelvic connective tissue.
In either event the fetal sac lies entirely outside the peritoneal cavity, and as it increases in size, the peritoneum is gradually dissected up from the pelvic walls. This condition is designated as extraperitoneal or broad ligament pregnancy, and was carefully studied by Dezeimeris 3 in 1836.
Lawson Tait laid great stress upon the importance of broad ligament rupture, holding that only such cases could go to term ; but the more careful pathologic work of later investigators has proven this contention to be erroneous.
Rupture of a tubal pregnancy into the broad ligament is uncommon. Williams, quoting the gathered statistics of Mandl and Schmidt, Kiistner, and Fehling, finds it noted in but 4 out of 276 cases, and out of 50 specimens examined by Williams this lesion had taken place only once. In Frank's study of 80 cases there was one intraligamentous rupture. P. F. Williams found 3 broad ligament ruptures in 132 cases, while, .strange to say, Foskett, reporting on Coe's cases, noted 8 intraligamentary ruptures out of 49 cases, a most unusually high percentage, so high as to raise some question as to the accuracy of the interpretation of the specimens.
Rupture of the tube, either into the peritoneal cavity or between the folds of the broad ligament, generally occurs spontaneously, but it may be a direct result of trauma, either by direct or indirect violence. Two such cases have been observed by the writer. In one of them a woman was kicked in the abdomen by a brutal husband, suffered violent pain and at once went into collapse. Diagnosis of some hemorrhagic form of intraperitoneal traumatism was made and immediate laparotomy performed, with the finding of a ruptured ampullar pregnancy of about 6 weeks' duration, which had not previously given rise to symptoms.
The other case was that of a lady who had suffered some slight pelvic pain for several days and who, while in the act of boarding a trolley car, found her foot slip off the car step, with a sudden contraction of the abdominal muscles. There immediately followed a tearing pain in the left side, with syncope and collapse. She was admitted to Frankford Hospital and operated upon within an hour of the accident. A ruptured isthmial pregnancy of the left tube, probably of four to six weeks' duration, was found, the abdomen containing a large amount of free blood. The tube and cornua were excised, the patient making an uneventful recovery. Vaginal examination has resulted in the rupture of an ectopic pregnancy, and this fact must be emphasized in order to avoid the error of vigorous bimanual examination in suspected cases. Coitus has been recorded as causing such accident.
5. The Growth and Development of the Fetus to Full Term, While Still Confined Within the Tube. — This rare and interesting termination of tubal pregnancy is occasionally recorded in the literature, though the writer has not had the good fortune to observe a case.
Dr. W. P. Conaway 4 reports a case in which, on opening the abdomen, he found an enormously distended right tube, which was very adherent on the right side to the parietal peritoneum and to the broad ligament, but perfectly free on the left side. There were no adhesions to the omentum or mesentery. The uterus was slightly enlarged and there was a marked lateral displacement to the left side. The left tube and ovary were apparently normal. The right ovary was enlarged, cystic and easily removed with the ovisac. After freeing the peritoneal adhesions the ovisac, which consisted of the right tube, was ligated and easily removed. There was little or no hemorrhage and no evidence of previous hemorrhage. This ovisac bore the same relation to the uterus, ovary and broad ligament as a hydrosalpinx. The contents of this tube were a perfectly formed dead fetus, which weighed six and three fourths pounds, a placenta which weighed three and one-half pounds, and about two quarts of thick slightly greenish fluid. The placenta was attached to the posterior surface of the sac, and between the layers of the broad ligament. The placental vessels were thrombosed. The ovisac was very thin and perfectly intact, until easily ruptured in freeing the adhesions. The abdominal cavity was flushed with normal saline solution, drainage inserted in the lower part of the wound, and the incision closed with through and through sutures of silkworm gut.
6. Interstitial Pregnancy May Terminate by the Gradual Growth of the Fetus Into the Uterine Cavity, the placenta remaining attached to its original cornual site, its growth taking place toward the uterus, rather than too greatly distending the uterine cornua. Fetal growth under these circumstances may continue to term, though this is rarely seen, or the embryo may die and be expelled as an intra-uterine abortion.
In this connection, Webster 5 reports a case wherein the patient expelled a complete uterine decidual cast, to which was attached, at one of the upper angles, an early ovum, which had evidently been situated in the interstitial portion of one of the tubes.
Secondary Terminations of Extra-uterine Pregnancy
In addition to the foregoing primary terminations of extra-uterine pregnancy, certain secondary end results may develop.
Tubal rupture or abortion, but far more commonly the former, may be succeeded by :
1. Tubo-abdominal pregnancy.
2. Secondary abdominal pregnancy.
3. Tubo-ovarian pregnancy.
4. Intraligamentous pregnancy.
Ovarian pregnancy may secondarily result in:
5. Ovario-abdominal pregnancy.
6. Secondary abdominal pregnancy.
1. Tubo-Abdominal Pregnancy is that condition which is found when, following a rupture of the tube wall on its free surface, the placenta remains attached to the tube wall either wholly or in part, fetal nutrition in the latter instance being derived from placental adhesions to contiguous structures. The fetus meanwhile has been expelled through the aperture in the tube wall and lies free in the abdomen, surrounded by its amniotic envelope, or is in some cases entirely devoid of covering.
Whether fetal life can continue or not, under these circumstances, depends naturally upon the traumatism inflicted upon the embryo by the act of tubal rupture, and upon the area of placenta remaining imbedded in the tube and maintaining unimpaired vascular connection with the tubal vessels. It will at once be seen that the possibilities of irreparable injury to the embryo from hemorrhage, as well as the tendency to complete or nearly complete separation of the immature placenta from its abnormal implantation site, are so great that the proportion of tuboabdominal pregnancy, in which development of the fetus continues to term, as compared with immediate fetal death following rupture, is extremely small. Tubo-abdominal pregnancy is, therefore, a rare condition though by no means unique, as a fairly large number of cases are recorded.
Webster 6 reported a case in which the child lay in a thin walled sac behind the omentum, while the placenta was still within the tube. He designated the condition as tuboperitoneal gestation, and supposed that it resulted from the early rupture of a tubal pregnancy, with the escape into the peritoneal cavity of the fetus surrounded by its amnion, and that the latter gradually became converted into the wall of the upper portion of the sac.
2. Secondary Abdominal Pregnancy is that condition found when, following tubal rupture or abortion (more commonly the latter), the entire ovum is expelled into the general peritoneal cavity and, the embryo continuing to live, the syncytia attach themselves to whatever tissue they may and reimbedding takes place in an entirely secondary location.
This possibility is denied by Williams, 7 who does not believe that the placenta can become directly attached to organs far removed from the pelvic cavity, such as the stomach and diaphragm, for instance; and when such conditions are observed, Williams thinks that one has to deal with a broad ligament pregnancy, in which the placenta is situated upon the upper portion of the fetal sac, which has become adherent to the organ in question.
Certain cases are recorded, however, which seem to definitely prove the existence of true secondary abdominal pregnancy, as, for example, that of Lane, 8 who describes a case of pregnancy at term at which abdominal section was begun on account of the patient's debilitated condition. The child was found free in the abdominal cavity and lived for twentyfour hours. Profuse hemorrhage followed delivery, and partial detachment of the placenta from its site in the left lumbar fossa anterior to the kidney was discovered. The uterus was apparently normal, save for being enlarged to the size of a ten weeks' pregnancy. No trace of rupture of tube, uterus or ovary was visible, nor was there any connection between the ovisac and the uterus, tubes or ovaries. Lane considers this case as one of primary abdominal pregnancy, but it is moreTikely that it was secondary to an early tubal abortion.
3. Tubo-Ovarian Pregnancy occurs when the fetal sac is composed partly of tubal and partly of ovarian tissue. It may originate in a tubo-ovarian cyst, or more commonly in a tube, the fimbriated extremity of which was previously adherent to the ovary.
Pathologically these cases are not distinct varieties, but begin as tubal or possibly rarely as ovarian, pregnancies, their subsequent course being due to the accidental attachment of the tubes to the ovary. A specimen is described by Paltauf 9 in which double tubo-ovarian cysts communicated with one another. Pregnancy occurred in the left cyst, and at autopsy a sound could be passed from the left cornu of the uterus, through both ovarian cysts, and back into the uterine cavity through the right tube.
A considerable series of this type of case is recorded in the literature.
4. Intraligamentary Pregnancy results when the tube ruptures
between the folds of the broad ligament and, the placenta remaining fast
to its tubal attachment, the fetus develops within the broad ligament.
As growth proceeds the parietal peritoneum is dissected away from the
tissues and the entire gestation sac continues to be extraperitoneal. The
term subperitoneopelvic pregnancy has been used to describe this variety,
and it was considered a common occurrence by the older writers. With
more careful study of the anatomy, however, intraligamentary pregnancy
has been found to be quite rare.
5. Ovario-Abdominal Pregnancy. — Should an ovarian pregnancy rupture and the embryo survive, there may develop an ovario-abdominal pregnancy, in which the placenta remains attached partly to the ovary and partly to the contiguous structures.
The case reported by Norris, 10 which fulfilled all the requirements for a justifiable diagnosis, presented a ruptured ovarian pregnancy, with the placenta implanted in the ovarian substances and a five months, macerated fetus partially within the gestation sac and partially in the abdominal cavity. Norris remarks that, in studying the doubtful cases of ovarian pregnancy in the literature, nearly half of them have reached full term. He thinks that many lithopedions are ovarian in origin.
6. Abdominal Pregnancy, Secondary to Primary Ovarian Pregnancy. — This condition is theoretically possible and differs in no way from abdominal pregnancy secondary to tubal rupture, save in the location of the primary embedding site.
The End Results of Extra-uterine Pregnancy
Untreated or long standing ectopic gestation may eventuate in :
1. Resorption of the products of gestation,
2. Tubal mole,
3. Hematocele, which may be
(a) Diffuse,
(b) Solitary,
(c) May become infected.
4. When fetal development continues the fetus may become:
(a) Lithopedion,
(b) Mummified,
(c) Adipocere,
(d) Skeletonized,
(e) May suppurate.
1 and 2. Resorption and Tubal Mole have been discussed in the section devoted to terminations and will not be further considered here.
3. Hematocele. — The older works on gynecology devote much space to a consideration of this subject, hematocele being considered as a distinct clinical entity. Veit, in 1884, first definitely stated the connection between hematocele and tubal pregnancy, but the great exponent of this origin was Tait. 11 This author, after painstaking investigation, laid down the rule that the presence of a pelvic hematocele afforded positive evidence of a preexisting extra-uterine pregnancy.
Tait's view has been proven incorrect, since a considerable number of cases of hemorrhage in the pelvis are secondary to rupture of a graafian follicle, or to bleeding into the ovarian stroma with subsequent rupture into the peritoneal cavity, without any evidence of pregnancy whatsoever.
The formation of a hematocele is one of the favorable terminations of ectopic pregnancy, in that the development of organized clot predicates the passage of sufficient time for active bleeding to have ceased, and the danger of death from hemorrhage to have passed. Hematocele is the result, necessarily, of slow hemorrhage, and it follows therefore that this termination occurs far more frequently where the initial lesion is tubal abortion, with its trickling of blood from the fimbriated extremity of the tube, rather than frank rupture of the tube wall, with its accompanying free bleeding.
The presence of blood in the peritoneal cavity sets up an irritative plastic, aseptic peritonitis, which invites adhesion formation, and in time the entire clot, occupying more or less of the whole pelvic cavity, becomes walled off by intestinal adhesions, the coils being firmly glued together and serving to form a sort of capsule for the clot. It has been held that the development of this so-called diffuse hematocele must have been preceded by adhesions between the pelvic organs, but the writer inclines to the view that the adhesions slowly form as a reaction of peritoneal surfaces to the irritation of free blood.
(b) Solitary Hematocele is a localized collection of organized blood clots, usually situated in close proximity to the fimbriated end of the tube. Its histogenesis is satisfactorily explained by Sanger, 12 who describes this phenomenon as being due to the very slow oozing of blood from the fimbriated end of a tube in which abortion had occurred, the periphery of the blood clot having had time to coagulate, while the center is steadily being increased by a slow accumulation within it. The irritating quality of blood on peritoneum causes such solitary hematoceles to be shortly surrounded by adhesions binding them to neighboring serous structures.
(c) Infected Hematocele. — Hematoceles, from their very nature, are excellent culture media for pyogenic bacteria, and infection of these collections is a frequent and dangerous sequel. The colon bacillus is naturally a common offender. The result of infection by this or other pyogenic organisms is to convert the hematocele into an abscess, which may point into the general peritoneal cavity, with subsequent peritonitis, may rupture into the rectum (a very fortunate termination for the patient), or into the bladder, or happily may sometimes drain into the vagina. Infected hematoceles are among the most serious and dangerous sequelae of ectopic pregnancy.
4. The Terminal Changes which may offset the fetal body, lithopedion, etc., are not of common occurrence and play but a small role in the medical history of ectopic pregnancy. Their chief interest lies in the classification and the genesis of their formation, discussion of which will be taken up in detail in the section of this book devoted to pathology.
LITERATURE
1. Werth. Beitrage zur Anatomic und zur Operativen Behandlung
der Extra-uterine Schwangerschaft. Stuttgart. 1887,
2. Martin, A. Zur Kenntniss der Tubar Schwangerschaft. Monschr.
f. Gebh. u. Gyn. 1897. 5 :I > 2 44- Quoted by Williams, J. W.
3. Dezeimeris, J. E. Grossesses Extra-uterines. Jr. de Conn. Med. Chir. Jan., 1837. Quoted by Williams, J. W.
4. Conaway, W. P. Tr. Phila. Obst. Soc. 1911-13.
5. Webster, J. C. Extra-uterine Pregnancy. 1895. p. 76.
6. Tubo-peritoneal Ectopic Gestation. Edinburgh, 1892.
p. 50. Quoted by Williams, J. W.
7. Williams, J. W. In Kelly and Noble's Gynecology and Abdominal
Surgery. Philadelphia, 1910. p. 155.
8. Lane, J. W. Bost. Med. Surg. Jr. 1911. 164:683.
9. Paltauf. Die Schwangerschaft in Tubo-ovarialcysten. Arch. f.
Gyn. 1887. 30:457. Quoted by Williams, J. W.
10. Norris, C. C. Primary Ovarian Pregnancy. Surg. Gyn. Obst.
1909. 9:123.
11. Tait, L. Lectures on Ectopic Pregnancy and Pelvic Hematocele.
Birmingham, 1888.
12. Sanger, tiber Solitare Hematocele und deren Organization.
Verhl. d. Deutsch. Gesch. f. Gyn. 1893. p. 281.
Chapter IV. The Anatomy and Pathology of Extra-Uterine Pregnancy
The Mode of Implantation of the Ovum in the Tubes — Placentation in Tubal Pregnancy — Changes in the Uterus Produced by Ectopic Pregnancy — The Relation of Uterine Decidua and Decidual Casts to Ectopic Pregnancy — The Cast of Membranous Dysmenorrhea — The Pathology of Interstitial or Cornual Pregnancy — The Pathology of Ovarian Pregnancy — Placentation — The Pathology of Pelvic Hematocele — The Pathology of Advanced Ectopic Pregnancy — Changes in the Tissues the Result of Ectopic Pregnancy — Diagnosis of Ectopic Pregnancy — The Fate of the Embryo in Ectopic Pregnancy — Bibliography.
A review of the normal morphology of the fallopian tubes will naturally precede a discussion of the implantation of the fecundated ovum in their walls. These structures, embryologically identical with the uterine body, being the upper prolongation of the mullerian ducts, are situated on the upper surface of the broad ligaments, to which they are attached by means of a thin fold of peritoneum, the mesosalpinx.
The tube is made up of three coats, an outer serous, an inner mucous with two layers between of muscular tissue, one in which the fibers are arranged in longitudinal bundles, externally, and one with its fibers dis^ posed in a circular direction, encircling the lumen of the tube, internally The mucous membrane, the lining of the tube, is covered with a single layer of epithelium, in the form of high, columnar, ciliated cells, which rest upon a thin basement membrane. There is no submucosa, the epithelium being separated from the underlying muscle by a layer of connective tissue of varying thickness, this arrangement corresponding with that of the uterus. The mucosa is thrown into folds, simple at the uterine end of the tube, and becoming more complex as the fimbriated end is approached. The appearance of the lumen varies according to the portion of the tube examined. In the uterine portion four elevations are seen, which together make a figure resembling a Maltese cross. In the isthmial portion of the tube a more complicated appearance can be noted ; while in the ampulla the lumen is almost completely occupied by the arborescent mucosa, which upon careful examination is seen to be made up of four very complicated, tree-like folds. (Figs. 15- 16-17.)
Fig. 15. — Section Through Uterine Portion of Tube.
The current produced by the cilia of the tube is directed toward the uterus, as was conclusively demonstrated by the experiments of Pinner, Jani, and Lode, who showed that foreign bodies injected into the abdominal cavity of animals made their way into the tubes and were gradually carried down into the uterus and thence into the vagina. (Description taken from J. W. Williams' Obstetrics.)
The muscular layers of the tube possess active peristaltic powers, which aid in the propulsion of the ovum towards the uterus, and in cases of tubal abortion or tubal pregnancy act to force the ovisac out through the fimbriated extremity. Developmental errors are common in the fallopian tubes. Accessory ostia and congenital diverticula are frequently noted and, as has been said, are considered an important etiological factor in the production of tubal pregnancy.
The morphology of the tubal mucosa renders it peculiarly susceptible to invasion and serious damage by infective processes. When the infection is severe and acute, with pus formation, the epithelium and, indeed, the entire mucosa of the tube may be destroyed and the fimbriated extremity closed. In this stage of salpingitis the ovum cannot enter the tube, and hence tubal pregnancy in the presence of pyosalpingitis is almost unknown. When, however, the inflammation is limited to the endosalpinx or when a more deep seated infection has undergone resolution, there results, not total destruction of the mucosa, but a glueing together of the arborescent folds, with the formation of false diverticula or canals by the adhesion of the ends of the regenerated plicae. Infection of the tube usually begins at the mucosa and progresses from within outward, through the muscularis and serosa, to invade the general peritoneal cavity.
Such infections leave in their train areas of small round cell infiltration and a fibrinous exudate scattered throughout the tubal musculature, and these areas of decreased elasticity play an important part in predisposing to tubal rupture, should pregnancy take place subsequent to such infective process.
Fig. 16. — Section Through Isthmic Portion of Tube.
The fibrinous exudate may replace all of the muscular elements of the tube, in which event no further peristalsis would be possible. So profound a destruction of the muscle is exceedingly rare and may be disregarded clinically, since a tube so damaged is not apt to admit an ovum into its lumen. Usually in a healing salpingitis the arborescent longitudinal folds of mucosa become adherent along their long edges, converting the lumen of the tube into one of many channels of varying length, and open at one or both ends, or closed sacs. The epithelium contained within these postinflammatory diverticula is in places destroyed, but quite generally is fairly well preserved or regenerated, although cilia are frequently absent. It is in such canals, open at the distal and closed at the mesial end, that the fecund ovum becomes obstructed as to its progress toward the uterus, and implants itself as a tubal pregnancy. It will be seen that the presence or absence of cilia is of but little importance from an etiological standpoint, if the foregoing explanation be accepted. Attention has been called to the frequent presence of diverticula and accessory ostia in tubes, never the seat of inflammation, and therefore congenital in their nature.
Fig. 17. — Section Through Ampullar Portion of Tube. From Williams.
Such writers as Huffman lay great stress upon the occurrence of such malformations as provocative of tubal pregnancy, and many cases undoubtedly result from this cause. As a general proposition, however, the inflammatory origin seems to satisfactorily account for the bulk of the cases.
True mechanical obstructions of the ovum by kinks, caused by adhesion bands and by pressure from adjacent neoplasms, do indubitably occur, but these are in a small minority. Tumors within the tube, polypi, etc., are found on occasions, but are accidental causes of tubal pregnancy only.
The theory that developmental arrest in the tube, with the retention of its primitive character as a producer of decidua, in common with the uterus, has been discussed under the caption of causes of extra-uterine
pregnancy. It is a most attractive theory, but not satisfactory, in that it does not ex pl am tne de cidua found in abdominal pregnancies of the true secondary type, nor does j it explain why so great a majority of the cases of Fig 18 — Tubal Pregnancy Caused by Diverticu la of Fallopian Tube. From Huffman. tubal pregnancy present incontrovertible evidences of preexisting inflammation on study of the tubes. Further, there are many specimens of tubal pregnancy in which no decidual formation can be demonstrated, and in many more the decidua is so indefinitely formed as to be practically negligible. Curiously enough, the theory of mechanical or postinflammatory obstruction to the progress of the ovum, as a cause for tubal pregnancy, has been held untenable by reason of a piece of experimental work performed by Mandl and Schmidt, 1 who ligated the genital tract at various levels in rabbits shortly after copulation. They found that when one or both uterine cornua were ligated, ova developed distal to the constriction produced by the ligature. When, however, the uterine end of the tube was ligated, tubal pregnancy did not develop, though they record the finding of dead ova distal to the tubal ligatures. These experiments are absolutely valueless, no true case of tubal pregnancy having been reported in the lower animals to my knowledge, save one case of Waldeyer's occurring in an ape and therefore not to be considered, since the uterus and tubes of the higher monkeys conform in all respects to the human type and have but distant resemblance to these organs in the lower forms possessing the bicornuate uterus. The writer has studied every specimen of female genitalia from the autopsies held at the Philadelphia Zoological Garden for the past twelve years and no case of tubal pregnancy has been noted. Bland-Sutton (quoted by Williams) states that in his large experience in the Zoological Gardens of London he never met with tubal pregnancy in animals and does not believe it to occur.
The reason is a very simple one. The uterine tubes in those orders of mammalia having bicornuate uteri are lined with a mucosa which, while it is thrown into folds, is exceedingly simple in construction as compared with that of the human female, as is well illustrated by Figs. 19 and 20. This tubal mucosa does not hypertrophy during pregnancy among the lower animals and, in fine, offers a very poor surface for imbedding of the ovum. Furthermore, the tube is very short and the writer entertains much doubt as to whether fertilization of the ovum takes place normally in the tube in these orders, or whether it does not usually occur in the long uterine cornua.
Fig. 19. — Cross Section of Fallopian Tube of the Coati. (From Wm. Pepper Laboratory of University of Pennsylvania.)
External migration of the ovum has been advanced as a cause of tubal gestation. It has been shown that the ovum given off by one ovary may enter the tube of the opposite side.
There are many cases recorded in which, one tube and the opposite ovary having been removed, the ovum passes across the peritoneal cavity and enters the remaining tube. Just why external migration should be considered as a cause for the development of tubal pregnancy is not so clear. Sippel 2 advanced the ingenious hypothesis that the ovum occasionally became impregnated while in the abdominal cavity, and that its transit toward the opposite tube was so' delayed that it attained a size so great as to preclude its passage through the tube to the uterus. Inasmuch as the work of Peters proved that no chorionic villi are present until the ovum has been nourished for a considerable time by the decidua in which it is embedded, it seems far more likely that an impregnated ovum, free in the peritoneal cavity, would die before it reached the tube.
Fig. 20. — Section of Fallopian Tube of Cervus Duvanceli, Showing Straight and Simple Rugae. (From Wm. Pepper Laboratory of University of Pennsylvania.)
On the whole, the theory of external migration of the ovum as an etiological factor in tubal pregnancy, is difficult to reconcile with the known facts.
The Mode of Implantation of the Ovum in the Tubes
Study of specimens of tubal pregnancy, based on the epoch-making work of von Spee and Peters upon the uterine implantations of the. ovum, demonstrates clearly the mechanism of this process in the tube. Prior to the researches of von Spee and Peters, it was held that, wherever an ovum embedded itself, there must develop a decidua, complete in its three divisions of vera, reflexa and serotina. The discovery and study of the Peters ovum disproved this theory and demonstrated that an ovum can develop only on a spot free from epithelium, sinking through the decidua to rest on the subepithelial layer of the muscularis, and producing by its presence such reaction as to provoke dilatation of the lymph spaces and edema of the myometrium and endometrium immediately surrounding the ovum. A decidua is not necessary for the imbedding of an ovum, Peters' specimen also showed the error of earlier conceptions with regard to the decidua reflexa. Instead of being an upward development of the vera, the reflexa was found to consist merely of the side wall of the cavity into which the ovum sinks, the upper edges of the side walls becoming soon united over the ovum by organized blood clot and fibrin.
With regard to the formation of decidua in the tube, while it undoubtedly occurs, there are cases in which no true decidua has been found, and such observers as Aschoff 3 and Kuhne 4 greatly doubt the very existence of tubal decidua. Aschoff found no decidua at the placental site in tubal pregnancy, while Kuhne describes only a pseudodecidua consisting of fibrin, connective tissue, and invading ectoderm cells. Though slight decidual changes may occur at the placental area, the cells which have been previously described as decidual are considered by Kuhne to be the cells of Langhans, and the same view is shared by Aschoff.
The place of meeting of spermatozoon and ovum, long the subject of spirited debate, has been definitely learned to be normally situated in the tube during the passage of the ovum through that channel toward the uterine cavity. It has been shown how, by inflammatory changes in the tubal mucosa, by the presence of congenital diverticula, or by constriction from external pressure, the transit of the fecundated ovum may be impeded and its implantation into any portion of the tube wall, where the arrest of its progress takes place, naturally follows. This implantation may occur in one of three mechanisms, the columnar, the intercolumnar, or the centrifugal.
With regard to the details of these mechanisms, Bandler well says that, with the exception of the absence of the decidua and an enveloping zone composed of compacta, the processes of gestation in the tube are the same as those in the uterus, modified only, as would naturally be expected, by the absence of the decidua and the thinness of the tube wall.
Returning to the mode of implantation, columnar imbedding, which is exceedingly rare, occurs when the ovum attaches itself to one of the treelike folds of the tubal mucosa, later becoming attached to other folds of the mucosa, but nowhere in contact with the tube wall itself. The ovum in such case derives its nourishment from the blood vessels of the mucosa for a short time, but presently the mucosa is eroded by the phagocytic action of the syncytial cells and the ovum comes to lie in the tube wall, the villi of the chorion penetrating the muscularis.
Intercolumnar implantation occurs when primary imbedding takes place in a cleft between the folds of the tubal mucosa, the ovum resting upon the surface of the tube wall, at once burrowing beneath it to lie in intimate contact with the musculature, and compressing and eroding the neighboring folds of mucosa. In such case the surrounding mucosal folds unite over the imbedded ovum, forming a sort of false decidua reflexa.
The centrifugal form of implantation, according to Bandler, 5 occurs when the ovum sinks into the wall of the tube, and an invasion of the wall and vessels by the villi may take place, even up to the serosa. The capsularis is formed by muscularis and mucosa. It may rupture at its summit. The invasion of the vessels entering the intervillous space may cause hemorrhage. The villi which extend up to the serosa may cause bleeding, though their penetration is so gradual that these points are usually covered with thrombi. Finally, a rupture may take place at the placental site through multiple perforations producing an erosion. Bandler thinks that the centrifugal form of imbedding furnishes the majority of tubal ruptures.
No matter what form of implantation is taken by the tubal ovum, one factor is constant; there is always an excessive amount of hemorrhage about the ovum. Otherwise, provided the embryo is a normal one, the attachment of the ovum to the tube wall is closely akin to that seen in normal intra-uterine implantation. As practically no true decidua is formed in the tube, there is always present about the ovum an excess of blood, since it is thought that the decidua is an important factor in preventing hemorrhage, the result of excessive erosive action of the trophoblast.
According to Mall the blood which is in immediate apposition to the trophoblast does not coagulate and is taken up by the syncytium, which is usually very markedly vacuolated and serves as pabulum for the ovum. The trophoblast also has a marked tendency to produce a peculiar necrosis of the maternal tissues with which it comes in contact, producing the so-called fibrinoid substance. In a later paper Mall G states that he has never found any tissues that could be considered as the decidua, nor has he found any specimens of early implantations. Whenever he encountered an ovum which was very small, it was invariably found separated from the tubal wall by a definite layer of blood.
Berkeley and Bonney, 7 in a careful study, define the formation of decidua in tubal pregnancy in three ways. The term decidua may be used :
- In the sense of a definite massive proliferation of a (supposed) subepithelial stroma, causing a decided hypertrophy of the tubal mucous membrane, analogous to that occurring in the uterine mucosa. Such conditions as described by Webster, J. W. Williams, and others were not found by them.
- In the sense of a "decidua capsularis" separating the ovum from the tube lumen, just as the decidua reflexa separates the intra-uterine ovum from the cavity of the uterus. They do not think the term should be used in this sense.
- In the sense of a proliferative reaction of the connective tissue cells of the wall of the tube, irrespective of their position. The term decidua appears to be used by most modern writers in this sense.
In their sections the absence of connective tissue reaction to the invading trophoblast is one of the most striking features. Here and there are patches of small cells with single rounded, deeply straining nuclei, whilst scattered irregularly about in the muscle tissue are certain cells with large oval vesicular looking nuclei, which stain faintly with hematoxylin. These cells are decidua-like, but with these exceptions the maternal tissue appears to be undergoing a passive destruction. (It is probable that the ovum travels toward that part of the tube where the nutritional vascular supply is most copious, and that in the majority of cases it is primarily implanted in the attached half of the tube wall.)
The gestation sac is everywhere bounded by a layer of tissue composed of trophoblast cells and masses of fibrin. The cells of the trophoblast present two main forms, the large mononuclear, epitheloid cell, and the multinuclear masses of protoplasm called syncytia. Of these the first is evidently, the primitive one, for, in addition to being much the more numerous, it is the only one which can be said to invade the maternal tissue. These trophoblast cells invade the tube wall by insinuating themselves between the muscle tissue in several strata, but always tending to a more or less concentric arrangement, while the layers of maternal tissue in contact with them appear to be undergoing a fibrinous degeneration (the fibrin of Nitabuch).
Placentation in Tubal Pregnancy
The tubal and the uterine placenta are identical in formation, with the difference that, as development proceeds, the thin tube wall, lacking the true decidua serotina, is. easily invaded by the trophoblast and syncytial cells, since there is no active connective tissue reaction set up in the tube by the presence of fetal cells. The villi rapidly penetrate the tube wall and are soon found just beneath the serous coat, which is in turn invaded, with resulting rupture. The tubal placenta also suffers from a lack of nutrition, the false sinuses formed by penetration of tubal vessels by the trophoblast being in no sense comparable to the rich blood supply developed in the uterine wall. This is a probable explanation for the great number of pathological embryos found in extra-uterine gestation. Microscopically the tubal and uterine placentas are identical in all respects. An interesting pathological feature in this connection is the finding of masses of syncytial cells or even bits of villi in the veins of the tube, remote from the seat of the pregnancy. This phenomenon has been aptly termed deportation by Veit, 8 who explains these findings by the fact that certain villi are not firmly attached to the gestation sac and, having entered a tubal vein, they are later cut off from their attachment to the ovum and carried by the blood stream to varying distances from this point of origin.
Fig. 21. — Trophoblast Cells Between Muscle Bundles of Tube Walls.
In addition to this cause of isolated masses of trophoblast being found in the tube, there is the inherited tendency of these cells to penetrate tissue, and they are frequently found between the muscle bundles of the tube walls (Fig. 21).
From the foregoing statements it will be seen that, so far as is now known, the implantation of an ovum in the tube wall, whatever its mechanism, very shortly results in :
First, the formation of a gestation sac bounded on all sides by a layer of trophoblastic cells and masses of fibrin. This capsular membrane or pseudodecidua is formed of trophoblastic elements and the products of degeneration of the tubal mucosa overlying the ovum.
Second, the trophoblastic cells, besides forming a portion of the sac wall, lie in masses between the muscular fibers of the tube and tend to separate muscle bundle from muscle bundle.
Third, there is rarely formed a true decidua, in the sense of a proliferation of maternal subepithelial stroma as in the uterus.
Fourth, these same cells directly invade the walls of the tubal vessels, especially near the site of implantation of the ovum. This invasion of vessel walls, according to Berkeley and Bonney, occurs either directly from without, so that the mass of trophoblast replacing the vessel wall is directly continuous with a similar mass lying outside the vessel, or they may invade the vessels along the line of the perivascular lymphatics. Fifth, there is but slight connective tissue reaction to the corrosion of the invading trophoblast, this explaining the lack of resistance of the tube wall to the distention of the growing embryo.
Fig. 22. Rupture of a Gestation Sac within the Tube Lumen, the Well Preserved Embryo Remaining in the Center of an Organizing Blood Clot. A beginning tubal mole. (Case of Dr. H. B. Ingle.)
Sixth, inasmuch as the decidua is supposedly an important factor in inhibiting the excessive corrosive action of the trophoblast cells, the absence of true decidua in the tube predicates an excess of blood surrounding the ovum, especially since the intervillous space in tubal pregnancy is always markedly vasculated and the vessels widely invaded by the masses of trophoblast.
The foregoing conditions favor early rupture of the gestation saq. When such rupture occurs, it may be followed by several events.
The rupture may first take place entirely within the lumen of the tube, the embryo be destroyed by presence of blood and separation of the nutritive villi from the tubal vessels into which they dip, the ovum subsequently being extruded from the fimbriated end of the tube by the combined vis a tergo of the accumulated blood and the peristaltic contraction of the tube walls, the whole process resulting in tubal abortion.
The sac may rupture and the blood find its way between the muscle fibers of the tube wall, these having been separated by masses of trophoblast, as has been seen. Such mechanism results in a hematoma of the tube, and may be compared to the condition that results when a saccular aneurism becomes diffuse. (Fig. 22.)
Whether a given case will result in tubal abortion or tubal mole, depends upon the completeness with which the sac separates from its tubal attachment and the amount of the hemorrhage, together with the degree of invasion of the tubal musculature by the trophoblast and its accordingly greater or less contractile power.
Fig. 23. — Beginning Rupture of an Isthmial Pregnancy on the Inner, Posterior Aspect of the Tube. The rupture is shown at a, a. few fronds of the chorionic villi having been forced through the minute opening (author's case).
The gestation sac may rupture directly through the tube wall, either along its free edge or into the mesosalpinx between the folds of the broad ligament. Whether such extratubal rupture takes place or not, depends upon the amount of erosion of the tube by the villi, and also upon the degree of degeneration of the muscle by preexisting inflammatory processes. (Fig. 23.)
The mechanism of tubal rupture is clearly described by Miki Kiutsi, 9 who distinguishes between acute tubal rupture and the chronic form. Acute tubal rupture, he thinks, is due to compression of the villous tufts, accompanied by apoplexy, ischemia, destruction of the coverings of the ovum, hemorrhage into the sac, dilated veins, hematoma, and hemorrhagic infiltration of the edematous connective tissue. The primary cause of the pressure the author finds to be a plugging of the large intervillous veins which carry the blood to the villi. The supplying arteries bring this blood with considerable force and this force ruptures the plugged veins, in which there is no outlet for the blood. Later the coverings of the ovum also rupture. Collateral circulation does not lessen the pressure. The rupture in sudden cases does not show a smooth opening, as in slow cases, but an irregular rent. The strongest compression is seen in the periphery of the tufts. Intracapsular rupture occurs from bleeding into the connective tissue. First comes pressure from sudden bleeding, killing the ovum. This results primarily from increased arterial pressure, secondarily from the rapidity of the blood stream. The death of the ovum comes from lack of nutrition, due to obstruction of the chorionic circulation; it is a secondary result of the intervillous pressure, as the determining causal factor of the rupture of the chorionic villi, which have a loose structure with large, dilated veins and large intervillous spaces; and this is due to the abnormal implantation of the ovum. Contributing factors may be contraction or torsion of the tube, and influences from without, such as jumping, lifting, or coitus. Rupture of the tube results from increased venous pressure in the intervillous spaces, and this from pressure on the veins supplying the villi.
Should none of these terminations occur early in pregnancy, the embryo continues to grow, and the reason why most tubal pregnancies terminate early, while a few go on to term, remains one of the unsolved problems of the pathology of this condition. Suffice it to say that some inherent phylogenetic action in certain tubes enables them to resist the erosive action- of the villi, and to accommodate themselves to the immense distention of the growing fetus. Perhaps the factor will be found in some primitive reversion of the tube to its uterine origin, thus permitting it to take on, to some extent, the morphology of the uterine cornu of the lower mammals.
In the advanced cases, the structure of the fetal sac is closely comparable to that of intra-uterine pregnancy. The wall of the tube becomes analogous to the uterine body. It is greatly thinned out, the muscular fibers rapidly undergo a metaplasia into connective tissue, though they may always be found unchanged in greater or less number. This variation in the muscular structures of the pregnant tube may bear some relation to the reversion changes suggested above. The muscular elements sometimes are very pronounced, Pinard 10 reporting a case in which the tubal wall was so dense, and its contractions so pronounced, as to make differentiation between it and the uterine body difficult. The fetal membranes and the placenta may develop normally, but the majority of extra-uterine embryos are pathological, as will be shown later. The serous surface of the tube becomes thickened by hypertrophy and usually undergoes some inflammatory change, and a layer of fibrinous exudate usually forms the external covering of the tubal gestation sac.
Advanced tubal pregnancy may terminate in rupture at any time, with or without embryonal life and growth continuing outside the tube/ or the fetus may develop to maturity within the tube (vide Conaway's case).
Fig. 24. — Late Rupturing Tubal Pregnancy.
Whether a given tubal pregnancy will terminate by rupture or by tubal abortion, depends on a series of considerations. The situation of the pregnancy is probably the most certain factor in determining the mode of termination. Both by reason of the smaller size of the tube as the uterus is approached, and by reason of the longer distance to be traversed by the ruptured ovum to the fimbriated extremity of the tube, those pregnancies situated in the uterine half of the tube are far more prone to early rupture than are the ampullar ones. The degree of invasion and degeneration of the tubal musculature and the separation of its muscle bundles by masses of trophoblast as well as the penetration, through the muscle, of the chorionic villi, also are active factors in producing rupture of the tube. Further, the degree of patulousness of the abdominal ostium of the tube has an important bearing on the terminatioiL Should the fimbriae be glued together by inflammatory exudate, the abortion of the ovum will be retarded, and even though an abortion has begun, the accumulation of blood behind and about the sac may cause a secondary rupture of the tube wall before the obstruction at the occluded fimbriated end is overcome. When this obstruction is not overcome, and the force of the hemorrhage does not cause sufficient pressure to rupture the tube, the dead ovum, surrounded by blood clot, remains in situ- to become organized, partially absorbed and result in a tubal mole.
Obviously, none of these terminations can be forecasted.
Fig. 25. — A Gestation Sac with Large Surrounding Blood Clot Found Lying Free in the Peritoneal Cavity, the Result of a Complete and Rapid Tubal Abortion. There was but little hemorrhage.
If the abortion be complete and rapid, hemorrhage is usually small in amount, since the empty tube may in a measure contract, and the blood spaces be sufficiently occluded to prevent free hemorrhage and permit clotting. When hemorrhage from the tube does continue under these conditions, it is due to the fact that contractions of the tubal muscle are feeble and ineffectual, and also that true decidua, with its inhibiting effect upon bleeding, is absent. On the other hand, when the dead ovum is partially extruded from the abdominal end of the tube, the latter, being still distended by the ovum, cannot contract, and the open blood spaces continue to pour out blood, which accumulates in the tube behind the ovum until sufficient pressure is reached to force it out between the tube wall and the sac, when the pressure is reduced, the process repeating itself indefinitely. It is this type of slow but continuing hemorrhage that so frequently results in hematocele formation, the blood lying in Douglas' pouch having ample opportunity to clot firmly and the clot being steadily augmented by fresh accretions of blood.
Changes in the Uterus Produced by Ectopic Pregnancy
The influence of an impregnated and imbedded ovum, wherever situated, always brings about an evolution of the uterus to some degree, together with the development of a decidua vera in that organ. This invariable reaction has been denied by certain observers, but no definite case appears to be recorded in the literature, and inasmuch as the decidua is not uncommonly expelled from the uterine cavity previous to a case of tubal pregnancy coming to operation, the absence of this tissue on examination of the excised uterus offers no proof that it has not been so expelled.
The uterus, while always enlarged in ectopic gestation, rarely reaches the same dimensions it would if the pregnancy were intra-uterine and of the same age, the stimulus being less pronounced. The increase in size of the uterus, according to Sampson, 11 is due to two evident factors, hyperemia and a thickening of the endometrium. Possibly the muscle fibers are also increased in size. The changes in the endometrium are quite similar to those found in the decidua vera of early uterine pregnancy and also vary with the age of the pregnancy.
Upon the death of the ovum and the termination of the ectopic pregnancy, whatever may be the variety of this process, the uterus always undergoes involution.
While the tubal pregnancy is being terminated, the tube undergoes a measure of intermittent contraction, endeavoring to expell its contents. These contractions are transmitted to the uterus, which in time contracts as in labor, or better, abortion, but in far less marked degree.
The clinical expression of such uterine contractions is bleeding from the endometrium, with the extrusion of portions of decidua. It may be concluded, therefore, that uterine bleeding and the passage of decidua in the presence of extra-uterine gestation invariably predicates hemorrhage about the aberrant ovum and the termination of the ectopic pregnancy. So long as the embryo is living and development is in progress, there is no uterine bleeding. The reason that uterine bleeding may continue for a considerable time after the attack of pelvic pain which apparently marks the destruction of the embryo, lies in the fact that the termination of the tubal pregnancy is not necessarily at once complete, chorionic villi remaining alive and exerting their stimulus upon the uterus.
In a series of cases wherein Sampson removed the uterus in the course of operation for extra-uterine pregnancy and subjected these uteri to close study by injection of their blood vessels, he found "that the uterine bleeding in all cases was of venous origin and arose from the endometrium, and in not a single instance did it escape from the tube into the uterine cavity."
Sampson further states that "following the complete termination of the tubal pregnancy, uterine involution takes place, which differs only in degree from that following uterine pregnancy. The uterus becomes smaller, due to decreased arterial and venous hyperemia and atrophy of the endometrium." This uterine involution is divided into two stages, a regressive and a reparative, the former being marked by an atrophied endometrium, the compact layer absent or thin, the arterioles few and difficult to detect and the venous spaces dilated.
In the reparative stage, the endometrium becomes thicker, its surface is thrown into folds, and there is a formation of a compact layer and glandular hyperplasia. Sampson holds "that where the process of involution is delayed by the influence of an incomplete termination of the tubal pregnancy, a condition arises apparently analogous to subinvolution of the uterus, due to retention of some of the products of uterine concept tion. As these cases are operated upon after the onset of the termination of the pregnancy, the uterus has already been influenced by three factors or forces: the first of these is pregnancy; the second is labor; and thirdly, with the onset of the termination of the pregnancy, i.e., labor, the involution of the uterus begins. The stimuli exerted on the uterus by pregnancy and involution are therefore antagonistic."
These changes in uterine blood supply are well shown by the Figures taken from Sampson. (Figs. 26, 27, 28.)
The Relation of Uterine Decidua and Decidual Casts to Ectopic Pregnancy. — It has been shown above that uterine bleeding in the presence of ectopic gestation follows the termination of the tubal pregnancy, and is literally an expression of sympathetic labor on the part of the uterus. Following the bleeding there is usually expelled from this organ either portions of its thickened endometrium, or the entire uterine decidua vera is separated en masse in the form of a decidual cast. Such casts are passed in nearly one half of the recorded cases of tubal pregnancy which have been subjected to close study.
In a considerable number of cases, where the first attack of pain and the termination of the pregnancy have taken place some time before operation, the decidua may have been entirely exfoliated and replaced by a normal uterine mucosa. Curettage and examination of the endometrium, after such an event would naturally lead to negative findings and the conclusion that uterine decidua is not necessarily present in ectopic pregnancy.
Fig. 26. — Uterine Changes Consequent on E* topic Pregnancy. From Sampson.
From a close examination of the literature and of his own cases, the writer is convinced that in every instance where a fecundated ovum has imbedded and developed, no matter to what extent, a uterine decidua is formed, completely or not, according to the extent of development of the ovum. The uterine decidua is in the main identical with that of normal intra-uterine pregnancy, although there may be some variation in the relative thickness and density of the several layers.
Fig. 27. — Uterine Changes Consequent on Ectopic Pregnancy. From Sampson.
The passage of a decidual cast has been considered as important in the diagnosis of extra-uterine pregnancy. This is true, but it must be remembered that such casts are simply , significant of pregnancy in some form, and may well be found in connection with the early abortion of an intra-uterine ovum. Only when a cast is passed, which microscopically presents the characteristic of decidua, i.e., a distinct division into a stratum compactum and a stratum spongiosum, and which fails to exhibit any evidences of chorionic villi, can a reasonable diagnosis of the existence of ectopic pregnancy be made from this evidence alone. In addition, allowances must be made for the alteration in the structure of the decidua brought about by hemorrhage into its substance,, decomposition changes, etc.
Fig. 28. — Uterine Changes Consequent on Ectopic Pregnancy. From Sampson.
An interesting example of the possible diagnostic error from an examination of decidual casts is that reported by Frank. 12 A woman of 27 had had amenorrhea for two months and believed herself pregnant (nausea, increase in size of the breasts). For two weeks she had bled slightly and on one occasion bled rather profusely and fainted. On examination there was a moderate amount of dark bloody flow, no clots. The uterus was slightly enlarged, no distinct Hegar's sign could be obtained, and the right adnexa were tender and appeared slightly enlarged. The symptoms continued for the next two days and on the third day the patient passed a typical triangular uterine cast, complete except for its extreme fundal portion. Immediate microscopical examination showed only a fully developed decidua, with absence of villi. On these findings a diagnosis of tubal gestation was made. Twenty-four hours later the woman passed a smaller elliptical mass, which proved to be a small degenerated ovum, surrounded by organized blood. The patient recovered without operation.
Frank believes that at the onset of symptoms the ovum had become separated from the decidua by slow and progressive hemorrhage. The blood had completely enclosed the ovum. Then, later, further bleeding had detached the decidua, which was expelled first, and lastly the ovum was extruded. As a rule it is to be expected, in such cases, that at least a few villi should adhere to the decidua, so that, in spite of this most unusual occurrence, vital importance should be attached to decidual casts in patients suspected to be suffering from ectopic pregnancy. (Fig. 29.)
Fig. 29. — Decidua of Uterus in Case of Tubal Pregnancy. From Frank.
An excellent description of the appearance and structure of decidual casts, as well as of those of membranous dysmenorrhea, which are sometimes confused with them, is contributed by Huffman 13 and is here reproduced in detail.
The Decidual Cast of Ectopic Pregnancy
The size of the decidual cast depends upon the duration of the pregnancy at the time it is cast off. It is usually somewhat fleshy, being several millimeters in thickness, and is of a pink color. If it is complete and its separation has been unaccompanied by hemorrhage, it forms a little sac, which may be slipped over the little finger. The inner surface is smooth and glistening. The outer surface is rough or shaggy and numerous shreds of blood clot are found scattered over it. In some cases, especially when the rupture of the ectopic growth has caused severe anemia, the cast presents a very striking pale, pinkish, mottled appearance. In cases of advanced gestation, that is of two or three months' duration, the cast may be eight by four centimeters. If the separation has occurred slowly and has been attended by hemorrhage, the cast may be very thick and bulky from the addition of blood clot. The microscopical appearances are those of decidua vera, the same as in normal pregnancy, being composed mostly of the compact layer and partly of the spongy layer. If hemorrhage has occurred into the decidua, if necrosis has supervened, or if leukocytic infiltration has taken place, the decidua will have been altered accordingly. These possibilities, as well as the postmortem changes, will occur during the exit from the uterus and the sojourn in the vagina, and are so variable that no two casts have exactly the same appearance, although, of course, the essential histological details are there. (Fig. 30.) "The Cast of Membranous Dysmenorrhea. — The size of menstrual casts, when entire, is never more than four centimeters by two and a half. The membrane is not so thick as decidua and is much more fragile. It cannot be handled in the same manner as a decidual cast and it does not have a cavity large enough to insert the finger. As a background for the microscopical appearances, one should have in mind the appearance of the premenstrual endometrium, with its elongated and tortuous glands and its swollen stroma cells. One sees that an excessive exudation of leukocytes has occurred, together with the formation of more or less fibrin. This process may have been so extensive and severe as to have caused the death of the involved mucosa, and it will be only here and there that the remains of an utricular gland or area of unaffected stroma may be seen. Here too one must consider the changes induced during the time of expulsion. Between the changes induced in the glands of the endometrium during the premenstrual period and the changes induced during pregnancy there is no distinct difference, except in size, and this is not sufficient in degree early in the course of pregnancy to be of any aid to diagnosis. We have, therefore, to resort to the recognition of the changes inducted in the stroma cells, which in pregnancy undergo a distinctive change, becoming very large with translucent cytoplasm and very dense nuclei. These cells, the so-called decidua cells, which form the decidua compacta, are so very characteristic that they are proof of pregnancy. When accurately compared with the so-called decidual reacting cell of menstruation, they are found to be very much larger, besides presenting dense, well defined nuclei and being packed closely together. The stroma cells of menstruation are much smaller, have pyknotic nuclei, and are not firmly packed together, except in small groups, the lymph spaces preventing this by being engorged. (Fig. 31.) "To resume then, we may say that the decidua compacta is the real criterion for determining pregnancy by an examination of casts. A decidual cast indicates pregnancy, not always ectopic pregnancy, because decidual casts may be passed from the non-gravid horn of a double uterus during pregnancy. We must keep in mind also the possibility of cases like those of Dakin and Griffith, where decidual casts were passed without finding any absolute evidence of ectopic pregnancy when operated upon later. In Dakin's case a peculiar layer of epithelial cells was found near the corpus luteum cyst, that were regarded by Dr. Rolleston as relics of the wolffian body. In Griffith's case there was no conclusive evidence of ectopic pregnancy, and he suggests that an impregnated ovum probably initiated the process and then died."
Fig. 30. — Microscopic Section of Decidual Cast. From Huffman.
Fig. 31. — Decidua Cells. From Huffman.
The Pathology of Interstitial or Cornual Pregnancy
Interstitial pregnancy is the rarest form of ectopic gestation, with the exception of ovarian, although modern literature contains the record of a fair number of cases. The relative frequency of this variety of extra-uterine gestation, according to Wynne, 14 who studied the literature on this subject, is 1.16 per cent, eighteen cases of interstitial pregnancy being recorded among a total of 1547 cases of ectopic pregnancy studied. In the records of the Johns Hopkins Hospital there were two such cases among 304 of extra-uterine gestation. (See Frequency, Chapter II.)
The etiology of interstitial pregnancy is practically that of ectopic gestation generally, inflammatory lesions of the tube in its interstitial portion being probably the most common cause. It has long been thought by -the writer that, since the differentiation of the miillerian duct into uterus and tube begins at the uterine cornu, this area would naturally be more apt to present some arrest of development, the uterine morphology continuing for some little distance into the tube. Such reversionary structure would predispose to embryonal imbedding in this location.
Interstitial pregnancy has been divided according to the location of the imbedding site into three groups (Klebs) :
- Utero-interstitial pregnancy, when the ovum occupies the uterine end of the cornual canal.
- Tubo-interstitial pregnancy, when the ovum occupies the tubal end of the cornual canal.
- Interstitial pregnancy proper, when the ovum is imbedded about the middle of the cornual canal.
The terminations of interstitial pregnancy are determine^ to' great degree by the locality of the imbedding site. In the utero-interstitial form the ovum may abort into the uterine cavity, may very rarely grow into the uterine cavity and then develop to maturity, the fetus occupying the cavum uteri, the placenta still fast in the cornua, or the uterine horn may rupture into the peritoneal cavity. In the interstitial form proper rupture of the cornua is the common termination, though abortion into the uterus may occur, and the death of the ovum with the formation of a cornual mole does occasionally take place.
In the tubo-interstitial form, rupture is the usual termination, although incomplete tubal abortion may occur.
If the pregnancy be utero-interstitial, there is a distinct diaphragm of tissue separating the fetal sac from the uterine cavity, the membrane being apparently formed by the endometrium and a portion of the muscular ring composing the cornua. This latter may present the appearance of a distinct os, rather resistant to dilatation, and through which the fetal membranes may be felt.
J. C. Webster, 15 in discussing interstitial pregnancy, mentions the possibility of the ovum extending into the uterus and thus developing partly in the tube and partly within the uterine cavity. In other cases Webster has seen communication between the uterus and the fetal sac closed by a wall formed by the decidua; and in still another group the communication may remain patent and be only closed off by the fetal membranes themselves.
Fig. 32. — Schematic Representation of an Interstitial Pregnancy of Four Months, Which Was Removed via the Uterine Cavity. (Author's case.)
It has been the good fortune of the writer to observe three cases of interstitial pregnancy, illustrating these terminations. One was of the utero-interstitial type, and will be reported in detail in the chapter on diagnosis. In this case the enlargement of the uterine horn could be distinctly felt in bimanual examination. At the right cornu a distinct ring of fairly firm tissue could be made out. This was penetrated with a dull curette and a placental forceps introduced through the opening, and a normal four months' fetus with its placenta and membranes was extracted. The myometrium was greatly thinned out. The placenta presented a characteristic appearance, being much flattened and having at one side a long finger-like prolongation, which had extended through the uterine cornu and had evidently been attached for a considerable distance along the lateral aspect of the tube. (Fig. 32.)
The second case was one in which there had been the ordinary evidence of extra-uterine pregnancy — amenorrhea, followed by spotting and, severe right sided pelvic pain. The symptoms subsided after a few weeks, but a dull pain in the right iliac fossa finally brought the patient to the writer. The uterus was found slightly enlarged and there was a smooth, tender, fixed mass in the right cul de sac. Diagnosis of terminated ectopic pregnancy was made and operation advised and accepted. The mass which had been palpated through the vagina was found to be an unilocular ovarian cyst, eight centimeters in diameter, which was densely adherent to the right tube and broad ligament. The right uterine cornu was bulged out in a rounded form, the swelling being inside the attachment of the round ligament. In the middle portion there was found a recent cornual mole, one centimeter in diameter. This was shelled out, the cornu curetted, and the opening closed. The ovarian cyst was removed. The cornual mole was found to consist of blod clot, decidual cells, and chorionic villi. No embryo was demonstrable. (Fig. 33-)
Fig. 33— A Mole Pregnancy in the Right Uterine Cornu. Incision through the uterine wall shows the ovum in situ. Pregnancy associated with an adherent ovarian cyst. (Author's case.)
The third case was that of a lady of 36, who, without previous history of ectopic pregnancy, with the exception of pelvic pain for two weeks, suddenly suffered a most violent attack of pain in the left side of the pelvis, with syncope and rapid collapse. A diagnosis of ruptured ectopic pregnancy was made upon the symptomatology alone, and the patient was subjected to immediate operation. There was an abundance of free blood in the peritoneal cavity, and upon exposing the uterus, the entire anterior surface of the left cornu was seen to be literally blown out. The cornu was represented by a jagged, stellate laceration, from the edges of which blood was flowing, and from which protruded bits of decidua. The cornu, with the attached tube, was excised, and the wound closed, the patient making an uneventful recovery. No embryo was found, but on examination of the excised tissue, the uterine cornu showed the presence of decidua and many chorionic villi. The tube was the seat of an old endosalpingitis, but presented no evidence of decidual reaction. (Fig. 34.)
In the three cases just reported, the rupture, contrary to usual reports, was on the anterior aspect. In the first, the thinning of the uterine wall, though not seen, was definitely felt to be most marked on the anterior aspect. In the second case, the cornual mole lay just beneath the surface on the anterior uterine wall. In the third case, the rupture took place entirely in the anterior wall of the cornu.
Fig. 34. — An Interstitial Pregnancy Which Had Ruptured, Literally Blowing the Anterior Uterine Wall into Fragments. Very profuse hemorrhage into the peritoneal cavity. (Author's case.)
The Pathology of Ovarian Pregnancy. — It has been stated that ovarian is the rarest form of ectopic pregnancy, except perhaps the cervical variety, which is almost unique. Norris 1Q in 1909 reported nineteen positive cases in the literature, when all those which did not comply with all the criteria of this form of gestation were excluded. Lockyer 17 has surveyed the literature from 1909 to 1917, and finds during this interval 22 genuine cases, making a total of 42; since 191 7 the only reported case in literature available to the writer is that of Wynne and Meyer, 18 who thus add one case.
It is the growing belief among students of this subject that ovarian pregnancy is not so rare as has been thought in the past, and that many specimens which have been dismissed with a diagnosis of ovarian hematoma, after a cursory microscopic examination, are in reality cases of ovarian pregnancy, in which the products of conception have been extruded from the follicle or have become degenerated. The earlier cases of ovarian pregnancy, those reported before the classic one of Van Tussenbroek, are usually excluded from modern statistics because of the paucity of the information regarding the nature of the specimen and because they do not fulfil all of the criteria demanded by the most meticulous pathologists. As early as 1878 Spiegelberg 10 established certain conditions which must be fulfilled, if the specimen in question is to be regarded as one of proven, primary ovarian gestation. Spiegelberg's conditions were that (1) the tube on the affected side must be intact; (2) the fetal sac must occupy the position of the ovary; (3) it must be connected with the uterus by the utero-ovarian ligament ; (4) definite ovarian tissue should be found in the sac wall.
To these criteria Williams 20 adds the very important condition that ovarian tissue must be present in several portions of the sac wall at some distance from one another. This requirement is necessary, for the reason that in certain cases of tubal or broad ligament pregnancy the ovary may become flattened out and to a certain extent become incorporated in the sac wall. Norris demands, in addition, that the tube on the affected side should not only be intact, but should be microscopically free from any evidence of gestation. More recent demands that an embryo must be found are not justifiable, since, in a large number of cases of ectopic pregnancy of all varieties, the embryo is lost in blood clot and is not demonstrable.
When it is considered that many of these specimens come to the pathologist at a time when the pregnancy is an advanced one, the anatomical relations distorted by the fetal sac, the tissues flattened and thinned out, and the entire mass surrounded by adhesions, it will be realized how difficult it is to find a case which complies with all the requirements deemed necessary to confirm its genesis.
When the operation has been performed days or weeks after rupture of the sac wall has taken place with the escape of the embryo, the involution changes in the sac wall themselves are sufficient to obliterate the evidence of ovarian origin of the pregnancy. For these reasons, it is probable that ovarian pregnancy is not nearly so uncommon as is stated in the literature, but in the light of our present knowledge of the condition, no case is to be accepted as positive which does not conform to all of the criteria as laid down.
Primary ovarian pregnancy is the result of the fecundation of an ovum while it is still confined within the graafian follicle. This statement, originally made by Van Tussenbroek, 21 has been confirmed by all subsequent investigators, Norris finding eleven of the nineteen cases regarded by him as being positive to have had this origin.
Leopold has suggested that in certain cases a centrally located follicle may rupture into a more superficially located one, the ovum in the former not being expelled, but being fertilized in its original location by a spermatozoon which gains access through the superficial follicle. Hewetson and Lloyd 22 believe that, after fertilization, the phagocytic ovum may burrow into another or deeper portion of the ovary. Both these hypotheses lack confirmation. The etiology of graafian follicle impregnation has been well expressed by Caturani, 23 who holds that the condition results from ovarian inflammation, especially peri-ovaritis. The resistance of ovarian tissue so affected to rupture by the ripening follicles and the subsequent formation of follicular cysts are well known.
Caturani thinks that it is quite possible that the opening in the mature follicle may be insufficient to allow the exit of the ovum, or incidental disease of the granulosa or of the theca folliculi may render the escape of the ovum impossible. When the ovum in the follicle has been fertilized, the latter immediately undergoes conversion into a true corpus luteum, being lined with lutein cells.
The corpus luteum is rarely perfectly formed, by reason, probably, of the early small hemorrhages about the ovum, as well as the erosive action of the trophoblast, whose cells rapidly penetrate the layer of lutein cells, in order to invade the surrounding vessel walls and open blood spaces, from which the developing chorionic villi may derive nutriment for the embryo. Between the ovum and the lining of the follicle there is always noted a layer of fibrin, degenerated cells, and blood.
The chorionic villi are found attached to the ovum, with their distal ends penetrating the layer of fibrin and blood clot, and in various areas entering blood spaces in the ovarian stroma, just as in tubal pregnancy.
Placentation in ovarian pregnancy probably follows the same course as in uterine or tubal pregnancy, except that the greater vascularity of the ovum permits of more complete placental attachment and a consequent more definite blood supply to the ovum. As to the formation of decidua in the ovary, while the question cannot be said to have been absolutely determined, the views of nearly all those who have recently studied this matter coincide in the belief that in the ovary, as in the tube, no true decidual reaction takes place, but that there is formed a tissue, consisting of fibrin, lutein cells and masses of trophoblast, which may be termed a pseudo decidua, and which is the expression of the reaction of the ovarian tissue to the irritation produced by the erosive action of the trophoblast.
Fig. 35.— Ovarian Pregnancy: Posterior View. From Mall and Cullen.
Fig. 36.— Ovarian Pregnancy: Macroscopic Section. From Mall and Cullen.
The duration of ovarian pregnancy is in the main longer than that of the tubal variety, by reason of the different nature of the tissues enclosing the embryonal sac. The ovary is far more elastic and resilient than the tube, as evidenced by its distention in cases of dermoid cysts. The substance of the ovary is also so much thicker than the tube wall that penetration of the former by chorionic villi is most improbable, while in the latter it is the rule. duration of ovarian pregnancies, many of them, indeed, going to term. The typical histological characteristics of ovarian pregnancy are well illustrated by accompanying drawings, taken from Mall and Cullen.
These facts will account for the longer
Fig. 37. — Ovarian Pregnancy: Microscopic Section. From Mall and Cullen.
When rupture of an ovarian pregnancy occurs, it is occasioned in the same way as in tubal pregnancy, and is well expressed by Rubin 25 as follows :
- The invasion of the syncytium into blood vessels may cause intracapsular or extracapsular bleeding.
- The sac may become thinner and no longer able to resist the increasing pressure of the growing ovum. The intraperitoneal bleeding may be very slight, or, as in ruptured tubal pregnancy, severe. In the former instance the process may go on to resolution or undergo inflammatory change.
The Pathology of Pelvic Hematocele
Collections of blood in the pelvis were treated as clinical entities until the work of Lawson Tait convinced the profession that such a condition merely represented a terminal pathology of ectopic pregnancy. This view was held until it was found that occasional pelvic hemorrhage resulted from ovarian and tubal hemorrhage not connected with pregnancy. Indeed Bovee 26 reports 19 cases, 1 5 tubal and 4 ovarian, of hemorrhage from the tube and ovary that could not be diagnosed as ectopic pregnancy at the time of operation. In 12 of these cases, microscopic reports were positive as to ectopic pregnancy in but 2. On the other hand, Caturani 27 analyzed one hundred cases of specimens of tubes and adnexa removed after clinical diagnosis of ectopic pregnancy, and only fifteen failed to produce positive microscopical evidence.
Fig. 38. — Ovarian Pregnancy: Microscopic Section. From Mall and Cullen.
When the literature of this interesting question is summed up, it appears that the vast majority of pelvic hemorrhages have their origin in some variety of ectopic pregnancy, but there remains a considerable number in which clinical and pathological evidence of pregnancy is absolutely lacking.
Hematocele has been defined as an organized collection of blood in the pelvis, and these collections have been divided into encapsulated, diffuse, and solitary hematocele, the encapsulated form being the one usually met with. Its genesis is that, following tubal abortion or tubal rupture, free blood enters the peritoneal cavity and sinks by gravity into the pouch of Douglas. By its presence the blood sets up an irritative peritonitis with peritoneal exudate and the formation of adhesions. Further hemorrhage from the tube augments the clot and adds to the exudate and the number of adhesions. The final result is a dense mass of coagulum, firmly bound together in layers by exudate and adhesions, the affected tube and its ovary together with coils of intestine being firmly atached to its surface.
Hematocele formation most commonly follows tubal abortion, by reason of the slowness of the accumulation of blood in these cases, but it may be associated with rupture of the tube in instances when the hemorrhage is not rapid and profuse.
If the collection of blood be small, the hematocele will be limited to Douglas' pouch, extending laterally only on the side of the affected tube: If the blood be abundant, the hematocele , may attain great size and fill the pelvis, leaving the uterus firmly fixed in its midst. As organization proceeds, the entire pelvic viscera may be involved in a dense firm mass of clot, fibrin and peritoneal adhesions. (Figs. 41 and 42.)
Fig. 39. — Ovarian Pregnancy: Microscopic Section. From Mall and Cullen.
The so-called solitary hematocele has been described (see page 45) and is comparatively uncommon.
Hematocele formation offers a favorable outcome for ectopic pregnancy, since eventual complete absorption of the clot frequently occurs.
Fig. 40. — Ovarian Pregnancy: Microscopic Section. From Mall and Cullen.
Secondary rupture of a rapidly growing hematocele may, however, lead to a repetition of the original hemorrhage into the peritoneal cavity, with disastrous consequences.
The real gravity of hematocele lies in its susceptibility to infection. Given a mass of blood mixed with fibrinous exudate and in intimate contact with the intestinal walls, infection by the ubiquitous colon bacillus is a natural sequence, and the conversion of the blood clot into a pelvic abscess is naturally a common occurrence.
In most cases, though, the infection is of such low grade that the tissues do not break down, but a parametritis develops, with extension of the inflammation to the pelvic connective tissue. This in time undergoes resolution and leaves in its train merely an adhesive pelvic peritonitis, the structures being firmly bound together by dense adhesions.
The Pathology of Advanced Ectopic Pregnancy
It has been previously stated that far advanced tubal pregnancy without rupture of the tube is a rare occurrence. Under these circumstances, the pathology is that of a marked distention of the tube wall, the thinning out of the muscular layer, and the wide distribution of connective tissue in and between the muscle bundles. The tube becomes involved in a reactive inflammation and is usually found more or less densely adherent to surrounding structures. Otherwise, there is no noteworthy change.
Fig. 41. — Pelvic Hematocele Following Tubal Abortion. From Crossen.
The common forms of advanced ectopic gestation (and these, too, are most infrequent) are either the secondary abdominal types, which follow rupture of the tube with the expulsion of the embryo into the peritoneal cavity, or the quite rare type which develops when the ovum entire is extruded from the tube and becomes secondarily implanted upon tissues possibly remote from the original site. Most cases of abdominal pregnancy seem to follow either rupture into the broad ligament, development continuing between the folds of this structure, or the rupture taking place on the posterior aspect of the tube, the placenta remaining partially attached to its original site within the tube lumen and partially becoming secondarily attached to the posterior surface of the broad ligament. In cases reported in the literature, the fetal sac is frequently described as ending in a pedicle, composed of the tube and the broad ligament on the affected side.
Fig. 42.— Blood Mass Surrounding Ruptured Tube. From Crossen.
There has been considerable discussion as to whether fetal development may go on uninterrupted, where the membranes have been destroyed at the time of primary rupture. An analysis of the literature leads to the conclusion that, while the fetus in these cases is usually enclosed in a sac which may be composed either of the fetal membranes, or of a fibrinous exudate, evidently of secondary formation, there may be no evidence of any embryonic covering whatever, with normal growth and development of the fetus. This is well shown by the case of Bland-Sutton, 28 in which the patient went to full term and on operation the child was found alive, having escaped from the amnion, and was disporting itself among the intestines. When a sac is present, it is usually found densely adherent to surrounding intestinal coils and to omentum, the adhesions being commonly very vascular.
Placental attachment in these cases is usually in the tube or along the border of the broad ligament, though occasionally the entire ovum may have been extruded from the tube and the ovum have become secondarily implanted at a point remote from its original site.
(See the case of Lane, page 43.)
Extraperitoneal abdominal pregnancy results when the ovum continues to develop after a rupture of the tube between the folds of the broad ligament. As the embryo grows, the leaflets of the broad ligament are dissected widely away from the pelvic walls, and the sac develops under the peritoneum and becomes what Hart has termed a subperitoneopelvic pregnancy, until, the pelvic brim having been passed by the steadily growing fetus, the gestation becomes subperitoneo-abdominal. These retroperitoneal pregnancies are uncommon, and, as pointed out by Williams, are in grave danger of infection and suppuration, by reason of their intimate contact with the rectum and bladder.
When abdominal pregnancy goes on to term, an attempt at labor usually occurs, the contractions of the uterus being more or less marked for several hours and then subsiding. After the subsidence of labor pains, fatty degeneration of the placenta takes place, resulting in the death of the fetus, which may then undergo various changes in its composition.
In this connection, it is interesting to note that abdominal pregnancy, terminated by operative interference, has in some instances resulted in the delivery of a living child. Horsley 29 has recently reviewed the literature on this point and presents the records of 105 cases with living children, up to 19 12. The majority of the children in these cases lived but a few hours after delivery and many of them were deformed. A few, however, survived. Horsley' s case is here quoted as an excellent illustration of this interesting outcome. "H. L., colored, aged 27 years, from Brunswick County, Virginia, was referred by Dr. B. W. Dameron. Family history of no importance. The patient had been married ten years and had menstruated regularly, except when pregnant. The first pregnancy resulted in a miscarriage at four months about nine years ago. The next child was born dead at full term, a year before admission to the hospital. The first menstruation missed since these pregnancies was in March, 191 1. There was some slight bleeding in April and May, but since that time there had been no sign of menstruation. There were no pains in the abdomen until the onset of labor, and the patient had no reason to believe that the pregnancy was abnormal until labor began. On the first of December she had cramp-like pains around the navel, which were very severe. There was no pain in the back. The feet were slightly swollen. These pains continued and Dr. Dameron was called in. He found the uterus empty, diagnosed abdominal pregnancy, and brought the patient to the hospital. A long incision was made a little to the left of the middle line. The intestines. and omentum tended to protrude. The anesthetic was given lightly, as the patient's condition was considered dangerous and she was not thoroughly relaxed. After packing away the intestines and omentum, the baby was found lying largely to the left of the middle line and floating among the intestines, covered only by a thin membrane, which also surrounded the placenta. In order to save the child, the delivery was accomplished as rapidly as possible. The head was towards the pelvis and was lifted up with the hand, at the same time rupturing the membrane. The cord was clamped and the child was given to Dr. M. L. Anderson for resuscitation. The baby was a boy weighing six pounds and had no deformity. There were a few adhesions of the intestines and omentum to the sac; these were separated and ligated where they were vascular. The placenta and the sac had a distinct pedicle from the left broad ligament. The pedicle was ligated and the placenta and membranes were removed. The condition resembled very much an ovarian tumor, in which the child and placenta might be said to constitute the contents of the tumor. The wound was closed in layers with catgut, and as there was some muddy fluid present, a drainage tube was placed in the cul de sac through a stab wound in the right flank. Mother and child were in excellent condition when discharged from the hospital on January 22, 191 2, and both are well now, December 17, 1912, more than a year after the operation."
Abdominal pregnancy may follow normal uterine implantation of the ovum, after rupture of the uterus, an accident usually brought about by instrumental attempts to induce abortion. As this condition is not strictly ectopic pregnancy, it is merely mentioned, and illustrated by the case of Bishkow, 30 which was as follows : "At about four weeks' pregnancy catheters introduced either perforated the fundus or caused a local necrosis, followed by perforation, with expulsion of the products of conception into the peritoneal cavity. A portion of the placenta sufficient to keep the fetus viable retained its attachment to the endometrium. The rest protruded from the perforation and, by partially filling up this opening, controlled to some extent the hemorrhage. There must have been a slow, continuous bleeding, for a large amount of blood was found in the peritoneal cavity and there was absence of any severe shock. The fetus and the greater part of the placenta lying extra-uterine became, in time, covered by a fibrinous deposit, which formed a false sac. The day preceding operation this sac ruptured and expelled the fetus into the peritoneal cavity. The size of the uterine cavity as compared with the size of the fetus shows that for a period of about four months the fetus remained viable in the peritoneal cavity."
Changes in the Tissues the Result of Ectopic Pregnancy. — Chorio-epithelioma may develop primarily in a tube which has been the site of a tubal pregnancy, the focus of the growth being at or near the placental site ; occasionally, indeed, such neoplasm may originate at some point remote from the tube, just as in similar instances, where these tumors succeed normal pregnancies.
Primary chorio-epithelioma of the tube is fairly common, Leipman 31 reporting 18 cases up to 1914. This condition has been studied by Hartz, 32 who reports a typical case: "A. S., 34 years of age, white, married. She began to menstruate at 13 years ; was regular and normal. The patient had been married for twenty years, had six normal pregnancies, and four abortions. The last pregnancy terminated in abortion four months prior to the onset of symptoms. For two weeks the patient complained of vaginal bleeding, accompanied by severe cramp-like pains in the lower abdomen. A diagnosis of ectopic gestation was made and operation advised. The operation was performed in December, 19 13. The abdomen was opened. The right tube showed a pregnancy of about six weeks. The tube and ovary were removed and the- abdomen was closed. The pathological report of the specimen is as follows : The mass consists of tube and ovary and gestation sac in collapsed condition. The tube measures five centimeters in length and four centimeters in diameter at its widest portion, which is situated near the fimbriated end. The lumen is filled with clotted blood and the walls of the tube are considerably thickened. Between the lower border of tubes and ovary there is an irregularly shaped sac in collapsed condition, measuring five centimeters in diameter and lined by a shaggy, dark red membrane. Adherent to these shaggy villous-like projections are masses of clotted blood. Under the microscope sections of the tubal wall show an attached placenta. At points the chorionic epithelium extends into the thin wall of the tube for some distance, and there are masses of these cells in the lumina of some of the veins. This involvement of the wall of the tube is more extensive than usual and justifies the term choriorepithelioma.
Diagnosis. — Primary chorio-epithelioma of tube following ruptured tubal gestation. The patient remained well after two years. (Fig. 43.)
In Risel's 33 statistics there were 3.5 per cent of primary tubal chorio-epitheliomata in approximately 300 cases in the literature.
Decidua formation in remote tissue occurs after extra-uterine gestation as well as in normal pregnancy. Outerbridge 34 reports a case in which portions of omentum, which had been excised with the placenta during an operation for full term abdominal pregnancy, showed distinct islands of decidual reaction scattered throughout their structure. Decidua formation has been reported in the appendix (Hirschberg, quoted by Outerbridge) and in a parovarian cyst (Taussig, quoted by Outerbridge), and in both of these cases it occurred in connection with tubal pregnancy. Outerbridge's specimen showed clearly defined groups of decidual cells scattered throughout the lower portion of the omentum. The cells were roundish, ovoid or polygonal elements, many times larger than the stroma cells of the surrounding connective tissue, having perfectly distinct cell boundaries, and arranged in many places in a beautifully tessellated manner. Each cell has a layer of pink staining, finely granular cell body; the tendency to vacuolation is not marked. The nuclei are regular in form, round or oval, very distinct, and show a fine chromatic network.
Outerbridge's discussion of the etiology of decidual masses in the omentum is well put. He says, "The question as to the etiology of the decidual masses in the omentum is of extreme interest. It can hardly be maintained that the decidua has been formed here in a physiologic sense, i.e., in order to give to the ovum opportunites for attachment and nourishment. No chorionic villi were found in direct attachment to this omental decidua, at least none sufficiently well preserved to be definitely diagnosed as such, and the history of the case indicates that the pregnancy was primarily tubal at any rate, the ovum reaching its final resting place in the abdominal cavity only after it had undergone several months of development; the attachments which it then formed to the omentum must therefore be considered purely secondary in character. Just what influence the presence of the developing ovum in immediate proximity to the omentum and ovary had in producing the extremely extensive decidual reaction in those structures is hard to state, though that this factor must have played a certain role seems clear. Loeb's interesting experiments have shown — at least for rabbits and guinea pigs — that the primary factor in the formation of uterine decidua is the presence in the circulating body fluids of a hormone developed in the corpora lutea; that the uterine mucosa, being "sensitized" by the presence of this substance, will respond by the formation of a decidua to any non-specific irritation — such as deep incisions into the uterine wall, the introduction of bits of glass tubing or other foreign substances into the uterine cavity — even though the ovum be entirely excluded from entrance into the uterus by ligation of both tubes. If this theory, that the sensitizing influence arises in the ovary, and not in the developing ovum, is correct, the seat of the fetal attachment would appear to exert no influence whatever on the formation of decidual cells, except by acting as a mere mechanical irritation to the fixed connective tissue cells of that region. Just how far this theory applies to the formation of extra-uterine decidua cannot be stated ; Loeb has not been able in his experiments to produce decidua outside the uterus, but the practically physiologic development of decidual nodules in the peritoneum and ovaries in normal pregnancies would seem to indicate that it may, in part at least, hold true for these situations as well. If the sensitizing hormone is the essential factor, and this arises in the corpus luteum, it would be natural to expect to find the ovarian stroma, at least that of the ovary containing the corpus luteum, and upon which its secretion must work in its fullest concentration, the seat of extensive decidual change. The fact that this change has been comparatively seldom observed in the omentum, however, would seem to indicate that under ordinary circumstances that organ either does not come extensively under the influence of the ovarian hormone, or that, if it does come under this influence, mechanical stimuli are wanting to call forth a decidual reaction. In such. a case as the one at present under consideration, where considerable portions of omental tissue have come into closest relationship both with the developing ovum and with the ovary containing the corpus luteum graviditatis, both these factors must certainly have been favored to the fullest degree, and this would seem to offer a satisfactory explanation for the extensive formation of omental decidua."
Fig. 43. — Microscopic Section of Primary Chorioepithelioma of Tube. From Hartz.
Fig. 44. — Decidual Tissue in the Appendix. From Outerbridge.
Fig. 45. — Decidual Tissue in a Parovarian Cyst. From Outerbridge.
The Fate of the Embryo in Ectopic Pregnancy
In the great majority of cases of extra-uterine gestation the embryo is destroyed during the early weeks of development. A careful study of the matter is that of Mall, 6 which will be freely quoted here : "In normal implantations in the tube most of the ova are destroyed in the early stages by the hemorrhage which is produced for their nourishment. If the dam built up by the trophoblast is sufficient to check the flood in part, enough villi will remain to nourish the ovum. When the tube ruptures into the broad ligament the space for the chorion becomes sufficiently large for new villi to grow and attach themselves."
In all cases an ovum within the tube is at a decided disadvantage, because it does not have a decidua to aid in producing a normal implantation. The importance of the decidua is probably greater during the early months of pregnancy than in the last half. "Rupture when it occurs on the free side of the tube, throws the embryo into the peritoneal cavity and usually terminates its career. Broad ligament ruptures offer the most hopeful outlook for the continuance of embryonic life. Whenever the degree of alteration in the tube wall is pronounced and accompanied by marked infection, the ovum does not implant itself well, and consequently the embryo does not develop normally, but becomes atrophied and degenerated. The more severe the inflammatory process, the more pronounced is the reaction upon the ovum."
It is noteworthy that, among the specimens studied by Mall, far more tubes ruptured, when they contained normal embryos, than among those in which the embryo was pathological ; showing that a live, normal, tubal embryo is probably far more dangerous to the mother than a pathological one. Pathological ova without embryos are very frequently encountered in examining series of specimens of tubal gestation. Mall found that 59 per cent of his specimens fell under this heading. Most of such pathological ova are collapsed and consequently small, less than 10 mm. in diameter. The pathological condition of these ova is that they are simply disintegrating and degenerating.
In 80 specimens studied by Mall there were 16 per cent of normal embryos, 25 per cent pathological embryos and 59 per cent pathological ova. It is probable that the pathological ova would have degenerated and undergone resorption, had they not been removed by operative measures. It is also probable that most of the pathological embryos would have been absorbed in the same manner. The normal embryos usually are destroyed by rupture or tubal abortion, but may survive, and it is thought that about 3.3 per cent of normal embryos go on to full term development, either within or without the tube; 10.5 per cent probably later become pathological and die, and 2.2 per cent become monsters. Von Winckel (quoted by Mall) thinks that fully one half the fetuses in ectopic pregnancy are deformed, the most common deformities being defects of the hands and feet. He collected 87 cases, and found that in 57 of them the fetuses were much deformed and in 12 were markedly monstrous. Among these were six cases of hydrocephalus and one each of hydromeningocele, encephalocele, anencephalus, omphalocele, spina bifida, and hypospadia. In addition, the head was found deformed in 57 specimens, the legs in 44, the arms in 35, in 12 there were club feet, and in 4 cases amniotic bands. The placenta was usually deformed, sometimes multiple, broad and thin, or short and thick, and often very hemorrhagic.
Cragin 35 reports a case of full term ectopic pregnancy, in which the living infant suffered from a small umbilical hernia, asymmetry of the head, and congenital dislocation of the hip. It was apparently mentally normal and was, as Cragin expresses it, "the pet of the ward."
The deformity so commonly noted among fetuses found in extrauterine pregnancy may also be due to pressure. "The walls of an ectopic gestation sac are more likely to exercise injurious pressure on the fetus than are the' uterine parietes. On the other hand, it may be that the cases in which the fetus has shown malformation have been those in which rupture of the sac had occurred, and the infant passed into the abdominal cavity, where it would be more subject to compression by the material structures."
Ballantyne 36 states that "In the event of the extra-uterine fetus surviving the effects of undue pressure plus the deficiencies in nutrition induced by faulty placentation, it may go on to normal development at full term and be removed from its aberrant antenatal situation by surgical measures." It has already been stated that 50 or more such cases have been recorded. When a correct diagnosis and indicated surgical treatment are not carried out, the fetus dies, or fetal death may occur from any one of the factors known to produce the accident in utero. When such fetal death does occur in advanced cases, certain terminal changes take place in the body of the child, provided, of course, it is not surgically removed.
These changes are suppuration, skeletonization, lithopedion, mummification, adipocere, or saponification.
Suppuration takes place in a considerable number of retained extrauterine fetuses, the septic process originating most frequently in the sac wall, thence spreading to the fetus, and the offending organism being probably usually the colon bacillus, which gains access to the sac wall by penetration of the intestinal wall along adhesion lines.
The inflammatory process is ordinarily of low grade type and eventuates either in the formation of a pelvic abscess, which points into the vagina or rectum, portions of the fetal body being discharged via these cloacae; or, the inflammation slowly subsides, the fetal soft parts undergo a liquefaction necrosis, and the skeleton remains to be carried as an inert foreign body, sometimes for a term of years. Occasionally the long bones of retained abdominal fetal skeletons penetrate viscera with resulting peritonitis of varying severity, according to the organ involved and the amount of trauma brought about by the irregular end of a fetal bone.
The following case of Cullen's 37 is typical of this termination. A colored woman of 33, whose previous history was uneventful, was admitted to Johns Hopkins Hospital, May 3, 1907. She had had one difficult full term pregnancy 13 years before, with a history of some puerperal infection. Three years previous to admission the patient was supposed to be pregnant, exhibiting the characteristic signs. She later developed severe abdominal pain, which was labor-like in character. This lasted for five minutes and then suddenly ceased, the patient passing only blood. Immediately after, she noticed a hard tender lump in the right lower abdomen. This lump has gradually become smaller, as has also the abdominal enlargement. There is burning on micturition, which is frequent and scanty, and the urine is at times mixed with blood. There is a profuse, odorless but irritating vaginal discharge.
On examination the abdomen was found distended on the right side by an irregular, nodular mass, which, on palpation, gave a feeling of crepitus, unusual to Cullen. The mass was irregular, but hard like a myoma. On pelvic examination the cervix was found to be firm, the uterus slightly enlarged and in retroposition. On the right side was a mass, which was apparently connected with the body of the uterus. The structure on the left side could not be palpated. From the history and examination the condition was diagnosed before operation as an abdominal pregnancy. The patient was catheterized when under ether, and a large quantity of thick tenacious urine was obtained. In the bladder the catheter also encountered something which felt very much like a stone. Operation May 4, 1907. A median abdominal incision was made. The peritoneum was opened and at once disclosed a large irregular mass in the right lower abdomen, with the omentum densely adherent to it. After the omentum had been doubly ligated and severed, the upper portion was pushed back out of the way and the parts were carefully walled off. The large and small bowel were found to be densely adherent to the sac. The small bowel was dissected away as carefully as possible, but the outer coat was torn about 12 inches above the ileocecal valve. This tear was immediately repaired with a continuous Pagenstecher suture. On opening the sac, it contained a large number of fetal bones. After removing the greater number of the bones, attempt was made to enucleate the sac. The left tube and ovary were now removed and the sac on the right side was gradually loosened up. The bladder was found densely adherent and connected with the extra-uterine mass. After being freed by blunt dissection, it was noted that one of the long bones projected into the bladder and that the portion within the bladder was covered with a thick deposit of urinary salts. The bladder opening was closed with catgut and with a continuous Pagenstecher suture. The enucleation of the sac was continued until it was delivered from the abdomen. The large bowel was then examined. There were two openings in the cecum, one at the junction of the ileocecal valve. The vermiform appendix was thickened and indurated. It was situated two centimeters from this hole in the cecum. The appendix was removed and the hole in the bowel closed in with two continuous Pagenstecher sutures. The second opening in the cecum was six centimeters from the ileocecal valve. This was drawn up into the wound and sutured in a similar manner with two continuous Pagenstecher sutures. The holes in the bowel had been made by the ends of the long bones, which had ulcerated through and were projecting into the lumen. Sections from the wall of the sac show that it consists partly of omentum, partly of granulation tissue, which is very edematous. The right ovary is edematous and cystic and measures 6.5 x 5.5 x 3 centimeters. In this case the uterus had evidently ruptured at the time of the patient's severe pain, and the fetus had escaped into the right lower abdomen. A slow inflammatory process had gradually developed, and eventually the ends of the long bones had been forced through into the bowel and bladder.
The interesting termination of abdominal pregnancy known as lithopedion occurs when the dead fetus of variable age becomes infiltrated with calcium salts and converted into a more or less completely calcified mass. The condition has been well known for many years, an interesting case being fully reported in 1586, to which reference has been made in the historical section of this book.
Fig. 46. — Fetal Bones Taken from Abdomen after Rupture of Pregnant Uterus. From Cullen.
These partially calcified, partially exsiccated fetuses may be carried by the mother for a long term of years, without marked evidence of their presence. Hayd's 38 case had been carried without inconvenience to the bearer for 33 years. Van der Veer and McCabe 39 removed at autopsy a lithopedion carried 35 years, the specimen lying entirely free in the abdominal cavity, except for a slight adhesion of intestine and peritoneum.
The frequency of lithopedion formation is difficult to determine, though it may be said that, as abdominal pregnancy itself is a rare condition, operators of wide experience, seeing but very few cases individually, it follows that this unusual termination of a process rare in itself must be quite uncommon.
Strauss 40 collected 38 cases from the literature from 1880 to 1900, and Bainbridge 41 added 36 cases, including one of his own, from 1900 to 1912, a total of 74 cases. The relative frequency of lithopedion formation in ectopic pregnancy is estimated by Schrenk 42 as 1.8 per cent, or 11 among 610 cases. Schauta (quoted by Bainbridge) found 9 lithopedions among 626 cases, or 1.5 per cent.
These figures, in the opinion of the writer, are too high, although no definite statistics can be offered to refute them. The case groups which have been gathered for analytical purposes in America during the past few years are of some value in estimating the relative frequency of such termination. In a summary of six case groups, compiled in recent years from various sections of the country, there were 866 studied cases of extra-uterine pregnancy, with no lithopedions. In the writer's series of 207 cases there was no lithopedion. It seems fair to assume, therefore, that a ratio of more than one per cent is entirely too high and gives a false estimate of the frequency of such pathological change.
This entire subject remained in confusion until cleared up by Kuchenmeister, 43 who in 1881 produced a masterly monograph originating the classification still in use. Kuchenmeister divided these tumors into three groups :
- Lithokelyphos, where the calcification is limited to the membranes or fetal sac.
- Lithokelyphopedion, when the membranes and the fetus are involved in the calcareous process.
- Lithopedion, when the fetal body alone is involved in the calcification.
Lithokelyphos follows usually the broad ligament pregnancies, or those in which intraperitoneal development of the ovum goes on for some time, the membranes being intact and the liquor amnii present. It is supposed that the presence of the gestation sac sets up a low grade, irritative peritonitis, which in turn gives rise to a fibrinous exudate, covering the walls of the sac and eventually undergoing calcareous degeneration, possibly as a terminal change following a fatty degeneration. In these cases the macerated fetus can sometimes be shelled out of the calcareous envelope.
In lithokelyphopedion both fetus and sac are involved in the calcareous process. The genesis of this condition is that either the fetus becomes adherent in some areas to its enveloping membrane during fetal life, or that the abdominal gestation sac becomes adherent to such viscera as have high absorptive power, such as the small intestine, the liquor amnii rapidly being absorbed, the sac wall coming into intimate contact with the fetus and joining with it in the stony change.
True lithopedion results when the fetus has escaped from its membranes before death and when there has not been developed about it the usual false sac wall, composed of fibrin and peritoneal adhesions. Of the three forms the first and third seem to be the most frequently observed, while the seconcl is uncommon, though far more frequent than formerly supposed. The age of lithopedions is difficult and almost impossible to determine, unless a history suggestive of the rupture of an ectopic pregnancy, followed by some evidence of false labor, is elicited, with the dates correctly noted.
These objects are much smaller than a living fetus of the same period of growth, owing, of course, to the exsiccation which they have undergone. The same factor will explain their comparative lightness, the weight steadily decreasing as moisture is abstracted, until the extreme low weight point is reached, after which the accretion of lime salts from without the structure may eventually materially increase its weight.
The ultimate result of lithopedion formation may be suppuration of the still moist fetal sac, with skeletonization of the fetus after a period of liquefaction necrosis of its soft parts ; or, the structure may remain, the low grade peritonitis excited by its presence soon subsiding, and the lithopedion being carried as a perfectly innocuous, and in many instances a totally unsuspected mass in the abdomen, until the death of the patient from some intercurrent disease. It is regarded as a favorable termination of abdominal pregnancy. Very rarely the fetus undergoes a saponification, the mechanism of which is obscure. Under the proper conditions (and no one knows what the proper conditions are) the fats of the fetal body, in contact with ammonia, evidently a decomposition product, become altered into a thick greasy, soapy substance, which entirely replaces the fetal tissues. This condition is called adipocere; its genesis is not understood and specimens are most uncommon.
A typical case of lithokelyphopedion is that of Hayd, 38 who operated upon a woman 67 years of age, who had gone through a false labor 32 years before and had remained in good health since until some weeks previous, when she developed steadily increasing abdominal pain, with ascites. A large, hard tumor could be felt rilling the whole of the pelvis, particularly on the left side. On operation there was removed a globular mass, weighing two pounds and four and a half ounces. It was surrounded by a dense, hard covering, which was about as thick as thin cardboard, and by letting the specimen drop upon the floor the noise made was as if a solid stone had fallen. After sawing through the outer envelope, the fetus was seen firmly bent upon itself; the arms and legs were flattened like bands. The calcified membrane was firmly adherent to the head and spine and back of the legs and arms. The abdomen, chest, side of head, arms, legs and fingers — and even finger nails — were in perfect preservation, the sex being determined by the little penis and scrotum. The placenta was present, the cord was thin and glistening in color, and was unusually well preserved. (Figs. 47-48.)
Fig. 47. — Lithokelyphopedion. From Hayd.
A case of true lithopedion, which illustrates the usual pathology and appropriate treatment, is that of Maier. 44 "A woman of 40 had two full term pregnancies, the labors of which were without incident. Her present trouble began twelve years ago. While six months pregnant, she fell down a well and injured her abdomen. Immediately afterward she suffered from severe abdominal pains and profuse hemorrhages from the vagina. These symptoms continued intermittently for two weeks, when they ceased. During this time no material was discharged that in any way resembled the products of conception. After the abdomen had again become normal in size, the patient noted a hard mass midway between the symphysis and the umbilicus. This mass was about the size of a large egg, freely movable, did not appear to increase in size, and only on strenuous exertion gave rise to distress. It was only within the past year that the patient had had symptoms sufficient to induce her to consult a physician. These were confined to the lower quadrant of the abdomen and of no definite character. In the presence of an enlarged irregularly nodulated uterus, a dense tumor to the left of it, and the hard movable mass floating above, a diagnosis of fibroids was made. Operation, hysterosalpingo-oophorectomy, at St. Joseph's Hospital, revealed the hard movable body to be a calcified fetus that floated fairly free in the abdominal cavity, just above the brim of the pelvis. The tip of the omentum and a few coils of the intestines were lightly adherent to its surface. It was attached by a short calcified pedicle, the remains of the umbilical cord, to a dense mass in the posterior surface of the left broad ligament, that consisted of a hard calcareous area, the former placenta, the tube, and the ovary." (Fig. 49.)
Fig. 48. — Lithopedion from Sac Shown in Fig. 47. From Hayd.
Fig. 49. — True Lithopedion. From Maier.
To summarize : The fetus in ectopic pregnancy usually perishes before the third month. Rarely, it may develop normally to term and be delivered alive by abdominal section, or it may grow to full maturity, die after false labor, and be retained for a variable length of time as a foreign body, undergoing generally some terminal change in its structure. (Figs. 50-5 1 -)
Fig. 50. — Lithopedion Lying Undisturbed in the Abdominal Cavity. From Kelly.
Fig. 51. — Lithopedion Removed from the Abdominal Cavity Four Years After a False Labor. From Kelly. 98
Literature
1. Mandl und Schmidt. Beitrage zur Atiologie und pathologischen Anatomie der Ei bei der Schwangerschaft. Arch. f. Gyn. 1898, p. 401.
2. Sippel. Uber Aussere Uberwanderung des Eies. Centrbl. £. Gyn. 1901, p. 289.
3. Aschoff. Die Beziehungen der Tubaren Placenta zur Tubenabort und zur Tubenrupture. Arch. f. Gyn. 1900. 60:523.
4. Kuhne. Beitrag zur Anatomie der Tubenschwangerschaft. Mar burg, 1899. Quoted by Bandler.
5. Bandler, S. W. Uterine and Tubal Gestation. New York, 1903. p. 136.
6. Mall, F. P. The Fate of the Human Embryo in Tubal Pregnancy. Carnegie Inst. Pub. No. 221.
7. Berkeley and Bonney. Tubal Gestation. Jr. Obst. Gyn. Brit. Emp. 1905. 7:77.
8. Veit. liber Deportation der Chorionzellen. Ztschr. f. Gebh. u. Gyn. 1 901, p. 466.
9. Miki, K. Arch. f. Gyn. 191 1. 95: No. 2.
10. Pinard. Ann. de gyn. et d'obst. 1892. v. 38.
11. Sampson, J. A. The Influence of Ectopic Pregnancy on the Uterus with Special Reference to Changes in its Blood Supply and Uterine Bleeding. Surg. Gyn. Obst. 1914. 18:587.
12. Frank, R. T. Am. Jr. Obst. 1912. 65 1466.
13. Huffman, O. V. Decidual Casts. Am. Jr. Obst. 1913. 68:704.
14. Wynne, H. W. N. Interstitial Pregnancy. Bull. J. Hopk. Hosp. 1918. 29:29.
15. Webster, J. C. Ectopic Pregnancy. Edinburgh, 1895. p. 76.
16. Norris, C. C. Primary Ovarian Pregnancy. Surg. Gyn. Obst. 1909.
17. Lockyer, C. Two Cases of Primary Ovarian Pregnancy. Proc. Roy. Soc. Med., Sec. Gyn. 1916-17. 102:158.
18. Meyer, A. W., and Wynne, H. W. N. Some Aspects of Ovarian Pregnancy. Bull. J. Hopk. Hosp. 1919 30:92.
19. Spiegelberg. Arch. f. Gyn. 1878. 13:73.
20. Williams, J. W. Obstetrics, New York, 1903. p. 537.
21. Van Tussenbroek. Un cas de grossesse ovarienne. Ann. de gyn. et d'obst. 1899. p. 211, 537.
22. Hewetson, J. T., and Lloyd, J. Brit. Med. Jr. 1906. p. 568. Quoted by Norris.
23. Caturani, M. Ovarian Pregnancy. Am. Jr. Obst. 19 14. 69:409.
24. Mall and Cullen. An Ovarian Pregnancy Located in the Graafian Follicle. Surg. Gyn. Obst. 1913. 17:698.
25. Rubin, I. C. A. Case of Primary Ovarian Pregnancy. Am. Jr. Obst. 191 1. 63:814.
26. Bovee, J. W. The Conflict of Clinical with Microscopical Evidences in the Diagnosis of Tubal and Ovarian Pregnancies. Am. Jr. Obst. 1918. 77:370.
27. Caturani, M. Clinical Diagnosis of Ectopic Pregnancy. Am. Jr. Obst. 19 19. 79:716.
28. Sutton, J. B. Tr. Obst. Soc. Lond. 1899. 40 :3o8.
29. Horsley, J. S. Abdominal Pregnancy with a Living Child. Surg. Gyn. Obst. 1913. 17:58.
30. Bishkow. Jr. Am. Med. A. 1919. 72:1668.
31. Leipman. Handbuch der Frauenheilkunde. 1914. v. 2:182.
32. Hartz, H. J. Primary Chorio-Epithelioma of Fallopian Tube Fol lowing Ruptured Ectopic Gestation. Surg. Gyn. Obst. 19 16. 23 :602.
33. Risel. Ztschr. f. Gebh. u. Gyn. 1905. 61 :i54. Quoted by Hartz.
34. Outerbridge, G. W. Decidual Formation in the Omentum in Sec ondary Abdominal Pregnancy. Am. Jr. Obst. 1912. 65:212.
35. Cragin, E. B. Am. Jr. Obst. 1900. 41 :74c
36. Ballantyne, J. W. Manual of Antenatal Pathology and Hygiene. Edinburgh, 1904. p. 144.
37. Cullen, T. S. Unusual Cases Illustrating Points in Diagnosis and Treatment. Surg. Gyn. Obst. 19 15. 20:260.
38. Hayd, H. E. Litho-Kelyphopedion. Am. Jr. Obst. 1907. 56:657 39. Van der Veer and McCabe. Alb. Med. Ann. 19 10. p. 4.
40. Strauss. Zur Kasuistik und Statistik des Lithopediona. Arch. f. Gyn. 1903. 68:3.
41. Bainbridge, W. S. Lithopedion. Am. Jr. Obst. 1912. 65:31.
42. Schrenk. Uber Ektopische Graviditas Inaug. Dis., 1893. Quoted by Bainbridge.
43. Kuchenmeister. Tiber Lithopedion. Arch. f. Gyn. 1881. 17: 153, 359
44. Maier, F. H. Extra-uterine Lithopedion. Am. Jr. Obst. 191 5. 72 :63c
Chapter V. Recurrent Extra-Uterine Pregnancy
Twin Ectopic Pregnancy — Combined Intra- and Extra-Uterine Pregnancy — Complicated Extra-Uterine Pregnancy — Tubal Pregnancy and Fibroid Tumors of the Uterus — Unique Forms of Ectopic Pregnancy — Hemorrhage from Ovary or Tubes Simulating Ruptured Ectopic Pregnancy.
The causes underlying tubal pregnancy are frequently identical in both tubes and, should one tube be removed for the relief of this condition, it is reasonable to suppose that the other tube may be similarly affected at some subsequent period. Indeed, this opinion is so definite that a number of gynecologists advocate the removal of the unaffected tube at the time of an operation for extra-uterine pregnancy, as a phophylactic measure against recurrence of the disease. An examination of the literature on this point brings out many illuminating details. Three authors have thoroughly investigated this phase of the subject, and the writer's views are based largely upon their work. They are Wassmer, 1 Smith, 2 and Giles, 3
First, as to the frequency of recurrence of extra-uterine pregnancy, versus the birth of full term children subsequent to an operation for tubal pregnancy. Giles found that, in 39 cases of ectopic pregnancy, whose history had been traced and where one tube or ovary was removed, five developed ectopic pregnancy in the remaining tube with operation (12.8 per cent).
Among the same 39 cases, six, or 15.4 per cent, developed some lesion of the remaining appendage, requiring operative relief. Of 38 cases, however, 13, or 34 per cent, later gave birth to living children. Incidentally, of 125 cases studied by Giles, in which unilateral salpingooophorectomy was performed for various lesions, including ectopic pregnancy, 33, or 26 per cent, became pregnant later, and of these, 8, or 24 per cent, were extra-uterine pregnancies.
Essen-Moller 4 collected 39 cases, in which subsequent pregnancy was possible. Of these, only two suffered from repeated tubal pregnancies, while 18, or 46 per cent, have had uterine pregnancies. He quotes Prochownik, 5 who had twenty-five normal pregnancies out of 57 women, or 43.8 per cent, and Engstrom, 6 who had twenty out of fortythree, or 46.5 per cent.
Smith 7 in a later paper collected 144 cases from the records of American operators. Of these 144, in all of which subsequent pregnancy was possible, 47 had uterine pregnancy with 64 children, and there were 21 instances of repeated ectopic pregnancy. The statistics of P. F. Williams show that among 58 cases of tubal pregnancies, 7 developed a subsequent pregnancy in the same series, a ratio of extra-uterine to intrauterine pregnancy of 1 :5-5 The thoughtful analysis of this subject by Smith reveals that, among 1608 cases of tubal pregnancy operated upon by members of the American Gynecological Society, there were 58 repetitions of the accident, or 3.6 per cent. From the literature Smith has collected 1390 authentic cases, with 55 repetitions, or 4 per cent. From the very nature of the case, it is difficult to obtain figures upon this point that are above criticism, since it involves a careful following up of patients over a considerable number of years, and this is rarely possible.
Obviously the cause of repeated ectopic pregnancy is usually identical with the cause of the original abnormal implantation, except in those cases where an inflammatory reaction following the laparotomy has damaged the remaining tube, which previously was healthy.
The practical point in this connection is, whether it is proper, in the interests of the patient, to uniformly remove the non-pregnant tube as a routine procedure in operation for tubal pregnancy. This question is best decided by a statistical comparison of repeated ectopics, as opposed to intra-uterine, since, should the former event supervene, it is obvious that the remaining tube is at least patulous and offers no obstruction to the passage of the ovum. If the statistics quoted above be grouped, it is found that among 280 patients, in whom future pregnancy of any variety was possible, 35, or 12.5 per cent, suffered from repeated ectopic gestation, while 134 intra-uterine pregnancies occurred, or 47.8 per cent, a ratio of about 1 to 4. It appears then that about one woman in eight who has had one extra-uterine pregnancy may expect another, whereas onehalf the total number have the possibility of future normal pregnancy.
These figures are overwhelmingly in favor of leaving a patient apt for future conception wherever possible, and they lead to the dictum laid down by the writer and practiced at his clinic, which is as follows : First, that the immediate recovery of the patient is the first consideration, and when a patient is in serious condition, no surgical procedure is performed, except the minimum one required to combat the pathology present. The remaining tube is therefore never removed under these circumstances, unless it be the seat of such grave disease as to possibly endanger the woman's life.
Second, when the patient is in good surgical condition, the nonpregnant tube is carefully inspected, and should it be apparently hopelessly damaged, it is removed. Indefinite signs of preexisting salpingitis, however, do not constitute an indication for such removal.
Third, inasmuch as ectopic pregnancy has recurred in the same tube and as conservative operations in the tube are ill advised in the opinion of the writer, the entire ectopic tube is invariably excised.
An interesting case of repeated extra-uterine pregnancy, which occurred in the service of the author, was that of a Polish woman of 26, who was admitted to Frankford Hospital with all the evidences of a ruptured tubal pregnancy. On section, the left tube was found the seat of the lesion, intraperitoneal rupture having taken place. The right tube presented no gross lesions and was not removed. The left one was excised, the patient making an uneventful recovery. Ten months later the woman was readmitted with the history of a self induced abortion with retained placenta. A four months' placenta was removed from the uterine cavity, with an afebrile convalescence. Six months following this operation the patient was admitted for the third time, with rather indefinite signs of ectopic pregnancy, and on laparotomy there was found an incomplete tubal abortion on the right side. The right tube was excised, with recovery.
There are instances on record where three ectopic pregnancies have developed in one patient, but a close examination of many of the histories leads to serious doubt as to their authenticity. Two cases, however, quoted by Smith, seem fairly definite, but even these will not stand scientific criticism. The histories were contributed by Peterson and Brettauer. Peterson's case is as follows:
Patient twenty-one years of age; has always been in good health. She was married December 26, 1908, and was always regular, but had had some dysmenorrhea. She had an attack of pain in the right side in May, 1909. She had skipped a period and began to flow, and was seized with pain in the right side. Her doctor felt a mass there, but she was not operated upon and gradually recovered. The appendix was removed six months later, November 23, 1909. The next attack was the first of May, 1 9 10. She skipped a period and was taken with pain in the right side. She went to bed, and after further pain a diagnosis of extrauterine pregnancy was made, and she was operated upon May 22, 1910 — a year after the first attack above mentioned. A ruptured ectopic pregnancy of six weeks was found. She skipped a period again in January, 191 1, had the same kind of pain in the left side, a bloody discharge from the uterus, and a distinct mass was felt in the left side. This absorbed without operation. Peterson says, "I know that the last two were attacks of extra-uterine fecundation. I cannot state positively about the first attack, but I am very sure that the right tube was affected at that time." Whereas operation did not verify the findings in each instance, considerable stress may be put upon its authenticity, since she came under the observation of a careful observer and the symptoms of ectopic pregnancy were clearly marked.
The case of Brettauer is still clearer. Brettauer says, "The patient referred to was operated upon at Beth Israel Hospital, New York, in April 1904, when, according to the records of that institution, the left appendage was removed for extra-uterine gestation. In February, 1905, she was admitted to the Mt. Sinai Hospital, and came under my care. She had missed two periods, had had a sudden attack of pain, and irregular uterine bleeding. Physical examination showed a large hematocele, occupying practically the entire pelvis. On top and toward the left was the uterus. A posterior vaginal section was done on February 25, and a large amount of fluid and coagulated blood were removed. There is a reference in the history to a fetus, but I am not positive about it and would rather leave this point in doubt. Convalescence was uneventful. On February 2, 1908 (three years later), she was again admitted to my service with a history of having missed two periods, severe abdominal pain, and a fainting spell two weeks before. Examination showed a retroflexed uterus low down in the pelvis. To the left of the uterus was a large irregular mass, the size of an orange, and closely adherent to it, and to the right a second somewhat larger mass was felt, movable, soft, and tender. On opening the abdomen the mass on the left was found to be a fibroid attached to the uterus by a broad pedicle. The one on the right consisted of a large, somewhat organized blood clot, adherent to the intestine, with one half still within the widely dilated end of the tube. Two thirds of the tube was amputated and the rest fixed to the ovary. No left appendage was present. After removing the fibroid the uterus was suspended and the patient discharged after an undisturbed convalescence. Microscopical examination showed decidua and chorionic villi."
Twin Ectopic Pregnancy
Twin tubal pregnancy may be unilateral, where one tube contains two embryos, or bilateral, where both tubes are simultaneously pregnant. To these classifications McCalla 8 would add two others, multiple tubal pregnancy, one tube containing one embryo and the other two or more, and multiple tubal pregnancy, one tube containing no embryo and the pregnant tube containing three or more.
Both unilateral and bilateral twin tubal pregnancies are rare, though some fifty cases are recorded in the literature. Many of these are not properly twin pregnancies, since it is frequently noted in the case reports that considerable intervals of time, sometimes years, have elapsed between the development of the pregnancies. Indeed a lithopedion in one tube, and a recently ruptured gestation sac in the other, have been reported as twin tubal pregnancy. Obviously, these are cases of repeated ectopic, and in no sense multiple f etations. McDonald and Krieger 9 point out the difficulties and the criteria of diagnosis of multiple tubal pregnancies.
Blood clot in a tube, when there is a fetus in the opposite tube, is no proof that gestation has occurred in both tubes. Even the presence of decidual cells in one tube, while the other tube has a gestation, is no proof that pregnancy has occurred in the tube with decidual cells and no fetus, since definite decidua has been found in the uninvolved tube by Kramer 10 and by Haultain. 11 McDonald and Krieger hold that, to definitely diagnose tubal pregnancy, a fetus or chorionic villi must be found. They have collected 25 proved Cases of double tubal pregnancy from the literature.
Proust and Buquet 12 reviewed the literature of bilateral simultaneous tubal pregnancy up to 19 14 and, after examining into the merits of 82 cases, accepted as genuine 33, which they believe to be true instances of simultaneous bilateral tubal gestation. Lockyer 13 adds one case of his own and accepts the case of Max Cheval, thus bringing the total up to 35, which Lockyer thinks is too high.
The diagnosis of simultaneity is somewhat difficult to reach. When the embryos are both preserved and of the same size, the diagnosis is assured. Lockyer thinks that, to establish definitely the diagnosis of simultaneity, "it should be based upon thorough macro- and microscopical investigation, and the pathological findings should harmonize with the clinical history of a single impregnation ending in a typical crisis or in two crises, more or less contemporaneous; and in some cases it will be possible to make out that the pain is bilateral in a single attack. When the onus of proof lies on the histological findings, the question of simultaneity is based on the character of the villi, i.e., on their relative size, development, and staining qualities. The villi in one tube should so closely correspond in all their features to the villi in the tube opposite, that the sections might be interchanged without detection."
A characteristic case of unilateral twin tubal pregnancy is that of Pool and Robin, 14 in which a woman of 27 gave the usual history of tubal pregnancy, and on laparotomy there was found a ruptured ampullar pregnancy of the left tube. There were two fetuses attached by separate cords to one placenta at the outer part of the tube. The fetuses were of the same size and development, their vertex-coccygeal measurement being 3.3 centimeters. (Fig. 52.)
Fig. 52. — Twin Ectopic Pregnancy. From Pool.
Triplet tubal pregnancy has been recorded by Sanger 15 and Krusen. 16 In Krusen's case a woman of 34 had a history of one full term pregnancy, followed by five miscarriages, again followed by a full term pregnancy. After one of the miscarriages she had suffered an illness apparently due to pelvic infection. After a period of amenorrhea lasting six weeks, the patient developed acute violent pelvic pain and other evidences pointing to the rupture of a tubal pregnancy. On operation there was found much blood in the abdomen, a ruptured and fragmented right tube containing three fetuses. The left tube was the seat of an old salpingitis. The patient was in desperate condition, succumbing to peritonitis three days later. The three fetuses were in the second month of gestation, were of the same size, and were apparently normal in all respects. (Fig. 53-)
Triplet tubal pregnancy is also recorded by Diament, 17 who found the signs of ectopic gestation present in a woman who had previously borne two children. On operation there was found a tubal pregnancy, and after freeing the adhesions and clots around the ampulla of the right tube, three embryos, each almost three centimeters long, were found in Douglas' cul de sac, having been aborted from the right tube.
Fig. 53. — Triplet Ectopic Pregnancy. From Krusen.
Bilateral twin tubal pregnancy offers some interesting problems in ovulation. It is impossible to imagine bilateral tubal pregnancy resulting from the development of twins from one ovum — i.e., the homologous or monochorionic variety. Furthermore, admitting that such twins are dichorionic ova, should both the ova arise from the same graafian follicle, one must reach the distal tube either by external or internal migration. Or it may be possible that all tubal twins are the result of the simultaneous impregnation of ova from each of the ovaries — a very rare condition, as shown by the great infrequency with which recently ruptured graafian follicles are found in both ovaries simultaneously.
When triple tubal pregnancies are considered, twins in one tube and a single embryo in the other, the case becomes more and more involved. In the present light of biological knowledge concerning ovulation, the whole subject may be well closed with the words of Ballantyne, writing upon a similarly involved theme, "Let us leave this subject: it is clear that it is obscure ; this alone is clear."
Combined Intra- and Extra-Uterine Pregnancy. — The fact that ectopic pregnancy may exist coincidently with normal intra-uterine gestation is well shown by many recorded cases.
In discussing the subject, it is understood that, by combined pregnancy is meant the presence of a fetus in the uterus and one of approximately the same period of development in the tube. Those cases of old, long since terminated tubal pregnancies, lithopedion, etc., in connection with an intra-uterine fetus, will not be considered.
Bichat 18 reviewed the older literature, reporting 48 collected cases, and adding one of his own. In 15 of Bichat's cases a tumor other than the gravid uterus was recognized, and occasionally fetal parts and a fetal heart were detected in the tumor. Rupture of the extra-uterine sac occurred 13 times, once 5 days after the birth of the intra-uterine fetus at term. In 15 cases the intra-uterine ovum was expelled prematurely, and in 12 cases both pregnancies continued uninterrupted to term.
An interesting feature of this complicated pregnancy is that, in common with other acute pelvic and abdominal lesions, the tubal pregnancy may be excised with safety, the intra-uterine gestation continuing to term. Such a case is recorded by Farrar, in which rupture of the tube occurred near the uterus at the second month of pregnancy. The patient was operated on while almost pulseless, but made a good recovery, and the intra-uterine pregnancy continued to term.
Simpson 19 divides these cases into four groups, as follows :
1. The woman becomes pregnant while carrying the dead products of an ectopic gestation.
2. The ectopic and intra-uterine products are both living at the same time. Such cases are naturally subdivided into three groups :
(a) Ectopic gestation precedes the uterine.
(b) Ectopic conception follows the uterine.
(c) Ectopic and uterine conception occur coincidentally.
Class 1 includes all the cases of lithopedion, and the end products of tubal gestation, in which the woman later becomes normally pregnant. Obviously such cases are in no sense combined pregnancy.
Class 2 (a), where the ectopic gestation precedes the intra-uterine, are rare instances. Simpson in 1904 found only three examples recorded.
Class 2 (b) includes the cases in which uterine pregnancy precedes the tubal conception. None of the recorded cases has withstood the test of critical analysis.
Class 2 (c) includes those cases in which the clinical course indicates fecundation of the two ova at or very near the same time, and in this group will be found the bulk of the cases of combined pregnancy.
(Note: Simpson's article contains a full bibliography of combined pregnancy to 1904.)
Complicated Extra-Uterine Pregnancy. — Ectopic gestation may complicate or may be complicated by the simultaneous existence of any form of disease process. Any attempt to consider possible coincident disease and the interrelation between the ectopic pregnancy and the added pathological condition would lead to a profitless narration of case records, interesting indeed, but in no sense usable either from a clinical or a purely theoretical standpoint.
For a clear understanding of the subject, though, there are to be discussed certain relationships which extra-uterine pregnancy bears to other clinical entities, since these relations are frequently met with.
First, the coincident existence of ectopic gestation and tumors of the pelvic organs. It may well be held that such relation is more than coincident, since the kinking and constriction of the tube, produced sometimes by a neoplasm of a neighboring organ, has been given as one important causal factor in the etiology of tubal gestation.
Tubal Pregnancy and Fibroid Tumors of the Uterus
In an analysis of 934 cases of myoma of the uterus, Cullen 20 found six cases of tubal pregnancy, all of which had been ruptured. In four of the cases the symptoms attributable to the myoma completely overshadowed those of the tubal pregnancy. Consequently the surgeon was totally unaware of the condition until the abdomen was opened. Ovarian cysts may complicate ectopic pregnancy and render the diagnosis most confusing. They also bear an etiological relationship to the condition by pressure upon the tube or by angulating their structures by means of bands of adhesions. A typical case of this sort is reported in an earlier chapter of this book (page 24).
Abdominal Inflammatory Disease is an infrequent accompaniment of extra-uterine pregnancy. An interesting case of appendicitis, in combination with an unruptured tubal pregnancy, is that of Vaughn. 21 "A colored girl fifteen years old was admitted to Georgetown University Hospital, Nov. 27, 191 1, suffering with severe pain in the abdomen. For two or three years, she says, she had suffered with abdominal pain, coming on at irregular times, worse in the right side in the region of the appendix. Has had several attacks this year, sometimes accompanied by vomiting. The attacks would usually subside in two or three days. Menstruation, she says, is usually regular and free from pain and lasts five days. Last menstruation was Nov. 6 and lasted only four days. The last attack of pain came on Nov. 2.7 , with griping pain in the abdomen all over, but worse on the right side, with nausea. Examination next day: pulse 80, temperature 99 , right side of abdomen tense but not tender or swollen. Diagnosis : catarrhal appendicitis. Operation advised and accepted. Gridiron incision on the right side permitted the delivery of the appendix, which was two and a half inches long, slightly swollen and congested, and bent on itself at an acute angle, owing to the peculiar attachment of the meso-appendix. It was removed and the pelvic organs were examined by palpation. The uterus could be felt, but the right ovary could not be recognized. In its place was a smooth mass, giving the sensation of an adherent cyst. While palpating, the mass suddenly ruptured and about an ounce of dark blood clots escaped, followed by a small quantity of red blood, which soon ceased. Two of the clots resembled membrane and were saved for further examination. Under the microscope chorionic villi were clearly seen, but the embryo was not found. The patient recovered without incident."
The Toxemias of Pregnancy are sometimes noted in connection with ectopic gestation and, when present, tend rather to clear up a doubtful diagnosis. The pernicious vomiting of early pregnancy is rarely met with, although a moderate degree of nausea and vomiting is not uncommon.
Eclampsia at times complicates secondary abdominal pregnancy at or near term. The disease is in no sense different in its manifestations, whether the pregnancy be intra- or extra-uterine, the important feature being the necessity for abdominal delivery in every case, if the fetus be extra-uterine, a necessity which naturally adds somewhat to the gravity of the condition.
An interesting case of this sort is contributed by Prof. E. P. Davis, in a personal communication. He says, "Some years ago I was asked to give a clinic at Harrisburg and the case selected for me was as follows : Primipara, aged about 30, previous history negative. Pregnancy had proceeded apparently normally until between the seventh and eighth month, when, after albuminuria of a week or ten days, the patient had several eclamptic convulsions. She recovered from this and, although she had some pains, labor did not occur. After her recovery, the abdomen grew smaller and fetal movements could not be felt, nor could heart sounds be heard. Her general health became good, but an abdominal tumor remained. On examination of the patient there was a central abdominal tumor closely connected with the uterus or part of it. Bimanual examination gave the phenomena usually seen in fibroid tumors of the uterus or abdominal pregnancy with retained fetus. This diagnosis was given to the physicians present at the clinic, and the abdomen was opened. A dead fetus of about eight months was in the abdominal cavity, its sac attached to the upper portion of the uterus. The fetus was not macerated, but the amniotic liquid had absorbed. The placenta was attached to the right broad ligament, the fetus was removed, the cord tied at the placenta and the greater part removed, the membranes stitched to the lower portion of the abdominal incision, and the cavity packed with gauze. The attending physician maintained drainage, the patient ultimately making a good recovery."
Much time might be devoted to a consideration of the coincidence of extra-uterine pregnancy and various disease processes from the diagnostic standpoint, but such relationship may occur in so many different phases, that a discussion of this subject could not result in more than an endless series of isolated case reports of no especial value in a categorical presentation of the subject, as is contemplated here.
Unique Forms of Ectopic Pregnancy
Cervical pregnancy is the condition which results when the ovum imbeds itself in the cervix uteri and there develops. It is doubtful whether such an implantation site should be classified as a variety of placenta previa, or whether it belongs in the category of ectopic gestation. Inasmuch as the cervical canal is not morphologically identical with the uterine cavity, it seems proper to include pregnancies in this area among the varieties of ectopic gestation.
The criteria of cervical pregnancy according to Rubin 22 are: (i) There must be cervical glands opposite placental attachment. (2) This attachment of placenta to cervix must be intimate. (3) The whole or a portion of the placenta must be situated either below the entrance of the uterine vessels or below the peritoneal reflection of the anterior and posterior surface of the uterus. (4) Fetal elements must not be present in the corpus uteri.
Cervical pregnancy is very rare, only a few cases being reported in the literature. It may be primary, when imbedding takes place originally in the cervical walls, or secondary, when a normally imbedded ovum becomes detached and reimplants itself in the cervix. The cervix does not usually participate in decidua formation, nor is this necessary for the development of an ovum, as shown by the pathology of tubal and ovarian pregnancy. The terminations of cervical pregnancy are either abortion, or more rarely rupture. In this latter case the rupture may take place in the infravaginal cervix, into the vagina or at the union of the peritoneal folds around the lower margin of the uterus, the hemorrhage thus being intraperitoneal. Cervical pregnancy usually terminates within the first three months, though the fetus may develop in the uterine cavity, the placenta remaining cervical. Rubin reports a case in which intraperitoneal rupture of a cervical pregnancy took place, with the signs of intraabdominal hemorrhage. On operation there was removed a uterus having the size of a pregnant organ at two and a half months. A fetus 23I/2 centimeters long was in the uterine cavity. On examination, the placental attachment was below the insertion of the uterine vessels and the lowermost points of reflection of the uterine serosa.
Fig. 54. — Cervical Pregnancy with Rupture into Abdomen. From Rubin.
Ectopic pregnancy in the gland spaces of an adenomyoma of the uterus has been reported by Doderlein and Herzog. 23 "There was present an adenomyoma in the left tubal angle or below it. The tumor contained glandular spaces, which were probably derived, not from any embryonic inclusions originating from the wolffian body, but from the uterine mucosa. The gland spaces may have been present in the tumor from the very beginning or they may have entered into its substance at a somewhat later period in consequence of inflammatory processes. Evidently there was a connection between the uterine mucosa and the gland spaces of the tumor. A fertilized ovum, by. some unexplainable coincidence, got into the gland spaces of the tumor and there developed. A fairly typical, though quite irregular, decidua was formed and the growing ovum stimulated the tumor to rapid growth and created for itself a cavity to accommodate the placenta. Pregnancy was interrupted, the embryo died, and was expelled in fragments. The latter were forced through the glandular canal connecting the tumor cavity with the uterine body."
Fig. 55. — Cervical Pregnancy. From Rubin.
Hemorrhage from Ovary or Tube Simulating Ruptured Ectopic Pregnancy. — Hemorrhage from the ovary or from the tube may occur entirely independent of the element of pregnancy, and the symptom complex, as well as the operative findings, may so closely simulate a ruptured ectopic gestation sac, that undoubtedly many such cases have been misinterpreted and have been recorded as instances of the latter condition, when painstaking microscopical examination of the tissues would have revealed the true state of affairs. Hemorrhage from the ovary may originate in a graafian follicle, or in the ovarian stroma.
Rupture of an apparently normal graafian follicle may lead to serious hemorrhage. Two such cases are reported by Primrose, 24 in which the excessive bleeding apparently followed some increase in intra-abdominal pressure from muscular effort. One of his cases followed the lifting of a heavy weight, while the second was superinduced by the vomiting attendant upon an acute appendicitis.
According to Bovee, 25 ovarian hematoma is a condition that has long been recognized. Peuch, in 1858, declared ovarian apoplexy actually exists and may cause death; it may form a hematoma and may or may not be absorbed. The condition has been so often encountered, as also have its, at times dangerous, associated conditions, that none should regard it as a myth or even a curiosity. Hemorrhage in the ovary occurs normally as it does in normal parturition. It may occur in graafian follicles or in an ovarian cyst when the venous circulation of its pedicle is obstructed by twisting of, or pressure exerted on, that structure. It may occur in the stroma, constituting a true hematoma. It may occur in toxic conditions, causing several accumulations of variable size, like those found in the kidney and other organs and which are noted in autopsies on patients dying of typhoid fever or other conditions having a local septic origin, such as puerperal sepsis or perforated gastric or duodenal ulcer (Wilson). Ovarian pregnancy is a rare cause. Hemorrhage into the stroma or into a follicle may occur in the newly born infant, fully developed, as in the case of Schultze, in quite young girls at or near the first menstrual period, and in early adult life or during the child bearing period, and may be accounted for in the noninfected cases by undue hyperemia, notable during the first few menstrual periods. Great sexual excitement is believed to be quite a common cause. Wilson states there is one case on record of a woman who died from shock on the eve of her marriage as the result of a profuse intraperitoneal hemorrhage from a ruptured corpus luteum. In early menstrual life profuse and prolonged uterine hemorrhage is far more common, and it is urged by some writers that this is from the irritation caused by continued bleeding from the ruptured graafian follicle.
Scanzoni reports a case of a girl dying from such profuse follicular hemorrhage during menstruation. At autopsy he found three liters of blood in the peritoneal cavity. A considerable number of cases have appeared in literature, like that of Fordyce, in which women, especially girls, exposed to cold and wet immediately preceding, or very early in, a menstrual period, have been the victims of ovarian hemorrhage so great in amount as to demand immediate abdominal section. In the inflammatory cases a quite well defined sclerosis of the ovary has taken place, giving rise to excessive formation of connective tissue in the ovary with fatty degeneration of the blood vessels, which rupture easily. It is probable in such a changed state, that expulsion of the ovum is retarded and the consequence, prolonged congestion, provokes hemorrhages into both the follicle and the stroma. When rupture of the bleeding ovary occurs, whether naturally from a graafian follicle or pathologically from overdistention due to blood accumulated in its stroma, free exit is given to escaping blood and hemorrhage is encouraged, more especially during ovular hyperemia. The rapidity of the flow of blood varies from a few drops to such large quantities as have been mentioned.
Schroder states that rupture of a graafian follicle may in exceptional cases be followed by so profuse a hemorrhage that it can ( i ) prove fatal; (2) cause peritonitis which may terminate fatally; (3) produce an encapsulated blood clot in the peritoneal cavity; or (4) produce a retrouterine hematocele. (Bovee.)
Tubal hemorrhage is not so well understood as is that from the ovary. While ectopic pregnancy is the active agent in its production in a preponderating proportion of cases, yet no one can doubt its occurrence quite frequently in postinfectional conditions, and in some instances reports have distinctly stated that neither inflammation nor pregnancy was evident. In the writer's judgment, the cases in which pregnancy, the result of infection, and traumatism, are all absent, must be extremely rare. The relation of ovarian and tubal hemorrhage to intraperitoneal hematocele needs no elucidation from the writer.
The difference between hemorrhage limited to the ovarian stroma and that in which there is peritoneal inundation from the same cause, appears to depend merely upon the amount of the bleeding and not upon any difference in mechanism.
Bovee feels that in the presence of hemorrhage of tubal or ovarian origin, where there is not positive clinical evidence of pregnancy as evidenced by the finding of a fetus or chorionic villi, one is not justified in making a diagnosis of extra-uterine pregnancy, unless proven by microscopical examination, and he supports his contention by a record of 29 cases of supposed ectopic gestation with free hemorrhage from ovary and tube, in which microscopical evidence supported the diagnosis in 17. This rather extreme view is counterbalanced by the work of Caturani, 26 who examined 100 specimens of suspected extra-uterine pregnancy, finding positive evidences of this lesion in 85, only 15 proving negative.
Fig. 56. A Hematoma of the Tube, Not Associated with Pregnancy of any Variety, but Strongly Simulating Tubal Gestation. (Author's case).
The pathology of ovarian hemorrhage, when it takes place into the stroma, is usually that of preexisting oophoritis, and peri-oophoritis, with the development of an excess of connective tissue, which impedes the rupture of the graafian follicle and causes the formation of a retention cyst. This is followed by a slow sclerosis with fatty degeneration of the stromal vessels, and these, being subjected to strain during the ovarian congestion incident to ovulation or intense sexual excitement, are unequal to resist the increased blood pressure and rupture, the blood escaping either into the parenchyma of the ovary or into a follicular cyst.
Follicular hemorrhage may result from the rupture of a normal well developed graafian follicle, as a result of sudden increase of intraabdominal pressure, or it may occur in follicles undergoing retrogression, and in which the unfertilized ovum has died, with the formation of a small retention cyst, having well marked vascular supply. These forms of ovarian and tubal hemorrhage possess no pathognomonic features and a diagnosis of the true origin of the hemorrhage is usually not possible until microscopic examination clears up the situation. The onset of the attack and the symptomatology is strikingly similar to that of a ruptured ectopic gestation.
The writer has had no personal experience with ovarian hemorrhage, but one typical case of bleeding from a tube, with evidence of pregnancy, may be cited. A spinster of 30 noted a sharp attack of left pelvic pain one year before admission. The pain gradually subsided, to recur at the menstrual period with increasing severity each month. There was pain on defecation and a slight loss of weight. On examination a distinct mass was palpated in the left vaginal vault. Operation revealed a greatly distended left tube, the enlargement measuring five centimeters in diameter, being globular in character and occupying the middle third of the tube. There was a small, organized pelvic hematocele. The right tube and both ovaries were normal. The left tube was excised, the patient making an uneventful recovery. On section of the tube, the mass was found to consist of organized blood clot. Microscopically there was considerable erosion of the mucosa by hemorrhage into the muscular coat, but no evidence whatever of decidual formation, villi or syncytial cells. (Fig. 56.)
Literature
1. Wassmer. Monschr. f. Gebh. u. Gyn. 1903. 17:88.
2. Smith, R. R. Repeated Ectopic Pregnancy. Am. Jr. Obst. 191 1. 64:401.
3. Giles, A. E. A Study of the After Results of Abdominal Operations
on the Pelvic Organs. Jr. Obst. Gyn. Brit. Emp. 1910. 17:153.
4. Essen-Moller. L'obstetrique. Paris, 191 1. 4:249. Quoted by Smith.
5. Prochowntk. Wien. Med. Woch. 1895. 14:1266, also Munch. Med. Woch. 1900. 64.
6. Engstrom. Mitth. a. d. Gyn. Klin, in Helsingfors. p. 327.
7. Smith, R. R. Ectopic Pregnancy and Repeated Ectopic Preg nancies. Surg. Gyn. Obst. 1914. 18:684.
8. McCalla, S. P. Twin Tubal Pregnancy and Bilateral Tubal Preg nancy. Surg. Gyn. Obst. 1909. 8:248.
9. McDonald, E., and Krieger, W. C. Multiple Ectopic Pregnancy. Jr. Am. Med. A. 1913. 60:1766.
10. Kramer. Arch. f. Gyn. 1903. 68:57.
n. Haultain. Jr. Obst. Gyn. Brit. Emp. 1906. 9:6.
12. Proust et Buquet. Rev. de gyn. et de chir. abd. 1914. 23 -.353.
13. Lockyer, C. Simultaneous Bilateral Tubal Pregnancy. Proc. Roy. Soc. Med. 1916-17. 10:88.
14. Pool, E. H., and Robin, F. Unilateral Twin Tubal Gestation. Am. Jr. Obst. 1910. 61 :6o6.
15. Sanger. tJber ein Fall von Ektopischer Drillings-Schwangerschaft. Centrbl. f. Gyn. 1893. P- : 48 16. Krusen, W. Triple Ectopic Gestation. Am. Med. Jr. 1902. p. 18.
17. Diament. Centrbl. f. Gyn. 1914. No. 3.
18. Bichat. Rev. de gyn. et de chir. abd. 1903. 7:412.
19. Simpson, F. F. A Consideration of Combined Ectopic and Intra uterine Pregnancy. Am. Jr. Obst. 1904. 49 :333
20. Cullen, T. S. Myomata of the Uterus. Philadelphia, 1909. p. 342.
21. Vaughn, G. T. Ectopic Pregnancy Complicating Appendicitis. Am. Jr. Obst. 1912. 66:829.
22. Rubin, I. C. Cervical Pregnancy. Surg. Gyn. Obst. 191 1. 13: 625. 2^. Doderlein, T. O., and Herzog, M. Surg. Gyn. Obst. 1913. 16: 14.
24. Primrose, A. Hemorrhage into the Peritoneal Cavity Caused by Accidental Rupture of the Ovary. Ann. Surg. 1912. p. 125.
25. Bovee, J. W. The Conflict of Clinical and Microscopical Evidence in the Diagnosis of Tubal and Ovarian Pregnancies. Am. Jr. Obst. 1918. 76:370.
26. Caturani, M. To What Extent Must We Depend Upon the Mi croscopical Examination to Support the Clinical Diagnosis of Ectopic Pregnancy? Am. Jr. Obst. 1919. 79:716.
Chapter VI. The Diagnosis and Symptomatology of Extra-Uterine Pregnancy
The Previous History— Absolute Sterility— Preexisting Pelvic Disease— The General Health and the Medical History of the Patient— The Findings on General Examination of the Patient— Blood Pressure— The Diagnosis of Ectopic Pregnancy— The Diagnosis of Long Existing and Untreated Ectopic Gestation— The Diagnosis of Ectopic Pregnancy, Other Than Tubal — Ovarian Pregnancy — Abdominal Pregnancy — The Diagnosis of Lithopedion and Adipocere — The Diagnosis of Complicated Ectopic Gestation — The Differential Diagnosis of Ectopic Pregnancy — Differentiation of Ectopic Gestation from Acute Salpingitis — The Histological Diagnosis of Extra-Uterine Pregnancy.
A discussion of the diagnosis and symptomatology of ectopic pregnancy opens a large and somewhat confused subject, the various phases of which must be grouped and the groups accurately correlated before any definitive statements are made.
The fact that pregnancy of some type exists must first be confirmed, after which a localization of the imbedded ovum may be attempted, first as to whether it be intra-uterine or extra-uterine and, if the latter, which structures are invaded by the aberrantly situated ovum. Diagnostic signs must also be differentiated into those present before rupture or tubal abortion has taken place, those noted immediately after such rupture or tubal abortion, and those apparent in later cases, where fetus and appendages, an old encapsulated blood clot, or both are present in the abdominal cavity.
A reader of text books upon gynecology and obstetrics must inevitably reach the conclusion that the diagnosis of unruptured ectopic pregnancy should be made in the majority of cases, and that recognition of the condition after rupture or tubal abortion is made simple by the development of a train of signs and symptoms unvarying in their course and apparent at a glance to a trained observer.
This happy situation, unfortunately, does not too often occur. Indeed, even in the hands of expert gynecologists, the diagnosis of unruptured extra-uterine gestation is more noteworthy by the high percentage of error than by the frequency with which correct conclusions are attained.
Furthermore, with respect to the cases in which rupture or tubal abortion has actually taken place, the clinical picture is often so obscure and the physical signs so parallel other acute abdominal lesions of widely divergent character, that even here experienced men often cannot form a clear conception as to the condition existent within the peritoneal cavity. Obviously, cases presenting the classical phenomena of extra-uterine pregnancy, either before or after rupture, are commonly seen, and here the diagnosis presents no difficulties ; but in studying a large series of case records, the writer believes it to be almost a rule that the signs and symptoms, which, if taken separately, would suggest ectopic gestation, lead to most conflicting conclusions when grouped, as they must be. The logical method of solution of the difficult problem of diagnosis is to categorically arrange the whole matter of ectopic gestation into its natural divisions, consider each division as a clinical entity, and then allow for biological variation of case from case and for the confusion of diagnostic evidence caused by the overlap of one phase of the condition over another.
The natural anatomicopathological groups into which ectopic gestation falls are :
1. The existence of tubal pregnancy, without any leakage of blood into the abdominal cavity whatever.
2. Tubal pregnancy with beginning tubal abortion or a minute rupture, permitting a minute quantity of free blood to come in contact with peritoneal surfaces.
3. Tubal pregnancy with frank rupture of the sac or tubal abortion.
4. Late abdominal lesions caused by a preexisting tubal pregnancy, where rupture or tubal abortion has been unrecognized or at least not surgically treated — hematocele, lithopedion formation, old traumatic salpingitis and the like.
5. Ectopic pregnancy other than tubal — ovarian, abdominal and cornual.
The foregoing completes the groups in which a direct diagnosis is necessary. The question of differential diagnosis also readily falls into certain great divisions, as follows :
1. Differential diagnosis of ectopic pregnancy from intra-uterine pregnancy, with or without threatened abortion.
2. Differential diagnosis of ectopic pregnancy from lesions of the reproductive tract not associated with pregnancy in any sense, but causing hemorrhage into the pelvic peritoneum — as ovarian apoplexy, unexplained hemorrhage of tubal origin, etc.
3. Differential diagnosis of ectopic pregnancy from other acute lesions of the abdomen.
The first group, that in which extra-uterine pregnancy exists, but the ovum and its envelopes are as yet entirely contained within the tube, is the one wherein lie those baffling obscurities and generally indefinite signs, whose very presence renders the diagnosis difficult.
A review of the facts as presented will prove the contention that the diagnosis of ectopic gestation, before the death and beginning separation of the ovum, or before rupture of the tubal wall has occurred, is a matter of so much doubt that its successful performance is almost to be considered a fortunate incident. The history is to some degree significant when taken as a whole. There will usually have been a period of amenorrhea, or at least a delayed period, in a woman usually regular. In the preruptured stage, there is scarcely, or never, any uterine bleeding. The associated history of a previous pelvic operation or attack of pelvic pain, due presumably to a low grade salpingitis, and the fact that the patient is the mother of a small family, or one child sterility, is of some presumptive value. There may be present the concomitant symptoms and signs of early pregnancy, though regrettably, these are usually conspicuous by their absence.
Vaginally there may be detected a slight degree of softening of the cervix, and perhaps a minor enlargement of the uterus. The tube will rarely be palpable. There is little or no pelvic pain, no leukocytosis, and no change in the urine.
Since the evidence of any pathological condition is so slight and vague, it will readily be seen that in this stage of the progress of ectopic gestation the patient rarely finds it necessary to consult a physician. The delayed or missed menstrual period is considered by the woman as evidence of a possible pregnancy. The subjective symptoms, when present, serve to confirm the opinion, and if a mild, dull pain develops in one or the other iliac fossa, it is ascribed to some ovarian condition incidental to the pregnancy. Only when the marked symptoms referable to rupture or tubal abortion make their appearance, does the woman become alarmed and invoke the aid of her physician, who, all too often, fails to be impressed by the significance of the grouped facts in the history of the patient, and considers the case one of intra-uterine pregnancy with some irritability of the uterus and possibly a threatened abortion. Furthermore, as Hunner 1 points out, there are undoubtedly many women with extra-uterine pregnancy who never even consult a physician and never have serious difficulties. The changes in the circulation may early rob the fetus of its blood supply, resulting in death and absorption.
The signs of early pregnancy, the breast changes, pigmentation, etc., are usually conspicuous by their absence. Upon vaginal examination, the enlarged and swollen fallopian tubes may be palpated, but only in a very small proportion of the cases. Boldt 2 says "I have never palpated a tubal pregnancy prior to the occurrence of symptoms due to the pathological implantation of the ovum, except in one instance — a double tubal gestation." He further well says that, though the statement not infrequently occurs in literature, that the diagnosis of uninterrupted ectopic gestation has been made by palpation, if the cases are carefully analyzed, it will almost invariably be found that bleeding into the tube had taken place, showing that the process of interruption of the gestation had been begun.
It must be remembered that the fallopian tube, when not the seat of inflammatory exudate, or when it has not been fixed in position by adhesions, is of a consistency about like that of intestinal coils, and its palpation through the vaginal vault is a matter of the utmost difficulty and uncertainty. Early tubal pregnancy, before separation of the ovum and bleeding into the tube takes place, does not appreciably alter the consistency of the tubal wall, nor does the tube increase markedly in size as a result of the presence of the imbedded ovum. Palpation of the affected tube is accordingly a matter of extreme technical difficulty and uncertainty.
Ectopic pregnancy, before bleeding takes place into the tubal wall or the peritoneal cavity, may be said to be a lesion incipient in all respects, provoking little or no reaction upon the physiology of the patient, and presenting only the most elusive details upon which a diagnosis may be based. In consequence, the diagnosis is made only in isolated cases, and then usually by accident.
The cases included in group two of the classification for diagnostic purposes are those in which beginning tubal abortion or a minute rupture of the tube permits a small quantity of free blood to come into contact with peritoneal surfaces, death of the embryo, or beginning separation of the decidua going on meanwhile. It is among the patients in this group that certain signs occur, which should clearly define the pathological process, and here it is that a correct diagnosis may and should be made in the vast majority of cases, provided the details of the history and the physical findings be carefully surveyed.
Speaking broadly, the evidences upon which a correct conclusion may be based are, first of all, the history; then the behavior of the menstrual flow; third, the indefinite signs of a pregnancy; fourth, the presence of pelvic pain, even though this be slight in character; and, lastly, the elicitation of a tender mass in one or the other vaginal fornix upon vaginal examination, together with the presence of certain gestational alterations in the uterus itself.
The history is by all odds the most important single feature in reaching a diagnosis, but in order to logically prove the importance of this factor, the other diagnostic features will be first considered, and then reviewed to demonstrate the importance of the history in correlating all the facts in the case.
In regard to the behavior of the menstrual flow, with few exceptions, there will have occurred a period of amenorrhea, varying from 'the missing of one or more periods with no bleeding whatever to a simple delay of one or two weeks, followed by a slight irregular "spotting" or a more frank bleeding, differing, according to the statement of various observers, from normal menstrual discharge, in that the blood is darker and more viscid.
In Farrar's 3 analysis the menstrual period was overdue in 34 per cent.
Foskett 4 says that the amenorrhea may be a relatively unimportant factor in the history, since only a little over 50 per cent of his patients had missed a period. He adds, however, that in general there is a history of irregularity. Crudely put, the history usually involves the statement that the patient was a few days or a week overdue, with some spotting or bleeding before the expected arrival of the next regular period.
Bandler 5 says that in early diagnosis the two symptoms of greatest value are atypical menstruation, or metrorrhagia and pain. The "atypical menstruation of ectopic gestation" is an expression used by Bandler to direct attention to the appearance of blood generally out of rhythm with the normal menstrual cycle of the individual. The amount of blood lost may be very much greater or very much less than the usual menstrual flow of the patient. It may be continuous or it may appear with interruptions. It may be darker, lighter or more brownish than the usual menstruation.
In MacKenzie's 6 careful study there was some degree of amenorrhea in 75 per cent of the 145 cases, and of the remaining 25 per cent, or 39 cases, thirteen were not subjected to operation and therefore not proven to be ectopic pregnancy, and nine were found, on operation, to be cases of pelvic hematocele, which might or might not have had their origin in an extra-uterine pregnancy.
Howard C. Taylor 7 states that in his series of 46 cases, 81 per cent gave a history of irregularity in the menstrual bleeding.
Rongy 8 found that in 75 cases the menstrual period was delayed in 53, or 71 per cent. The average period of amenorrhea was about eight weeks.
Summary: Analyzing the various statistics of a group of modern, trained observers, and averaging their opinions, it may be stated as a definite fact that mentrual irregularity, varying from the delay of an expected period for a few days, to profuse metrorrhagia, is a characteristic of at least three fourths of the case histories in tubal pregnancy. The irregular bleeding, which so uniformly occurs in the presence of ectopic pregnancy, possesses certain definite characteristics. So long as the life and growth of the ovum progresses without interference, there is no uterine bleeding, and the development of this sign invariably predicates death of the embryo, or at least its beginning separation from the false decidua into which it has imbedded.
This feature of the hemorrhage is excellently put by Taylor, 9 who says, "The hemorrhage is usually due to some separation of decidual membrane from the interior of the uterus and is moreover a sign that the vitality of the pregnancy is endangered or destroyed. So long as the pregnancy, although out of place, is growing and uninjured, there is, as a rule, no uterine bleeding. External hemorrhage, therefore, is not so much a sign of extra-uterine pregnancy as of some secondary disease or injury, which has affected the pregnancy; but as the great majority of cases suffer accidental changes during the earlier months, it becomes a sign of great importance.
The bleeding may occur without coincident pelvic pain, but such cases are in the minority. For example, in Oastler's 10 series of 106 cases, bleeding was closely associated with attacks of pain in all but eleven. In these the flow began some considerable time after the pain. Uterine hemorrhage was certainly absent in two cases, and bleeding continued intermittently for five months in two cases.
In Farrar's 3 series bleeding was present in 67.4 per cent of the cases. In this group bleeding occurred in five instances without pain, and Farrar thinks it probable that the contractions of the tube are not sufficiently forceful to cause severe pain until the supreme effort to rupture the tubal wall takes place.
In Polak's n large series of 227 cases 222 of the women presented some menstrual anomaly, as a period of amenorrhea, prolongation of the normal period, anomalous character of the bloody discharge, or an anticipated period, followed by an intermittent or continuous metrorrhagia. According to Polak, this vaginal discharge, which, is irregular in occurrence and amount, has presented definite characteristics; it is brownish red blood mixed with mucus which does not clot, and its quantity is increased from time to time, coincident with the painful paroxysms.
The bleeding of extra-uterine pregnancy is rarely large in amount, and herein lies an important point in the differential diagnosis of extrafrom intra-uterine pregnancy with threatened abortion. Hemorrhage from the uterus to the point of producing any demonstrable evidence of an acute anemia almost never occurs, and where a very profuse vaginal hemorrhage is associated with definite signs of an ectopic gestation, the case should at once arouse the suspicion that coincident extra-uterine and intra-uterine pregnancy are present.
Taking the combined experience of investigators along the foregoing lines, it may be said in summing up, that metrorrhagia of some degree is a very strong affirmative symptom of the existence of ectopic pregnancy, the strength of the sign as a factor in diagnosis increasing as the coordinating facts are developed in the study of the individual case.
Concomitant Signs of Pregnancy. — The third point in the diagnosis of the group of prehemorrhagic cases is the determination of the existence of pregnancy of some variety. The signs of pregnancy during the early weeks, both objective and subjective, may be detailed as :
Amenorrhea,
Morning nausea and vomiting,
Pain and tingling in the breasts, with the appearance of colostrum,
Increased pigmentation in various skin areas,
Softening of the cervix,
Enlargement of the uterus,
Cyanosis of the vaginal mucosa,
Increased anteflexion of the uterus,
Frequency of urination,
The Abderhalden reaction.
In general, it may be said that these signs and symptoms are almost invariably less marked when the fecundated ovum is aberrantly situated; only in rare instances are many of the signs present in any given case of extra-uterine gestation, and in the majority of instances they are so intangible as to be almost negligible in lending weight to a positive diagnosis of tubal pregnancy. On the other hand, if the usual evidences of early normal gestation be demonstrable in marked degree, they strongly negative the diagnosis of extra-uterine pregnancy and greatly increase the probability of the gestation sac being normally implanted within the uterine cavity.
Cessation of the menstrual flow and its characteristic irregular return have already been discussed.
The morning nausea seems to be present in some degree, although; in studying the analysis of large series of case histories in the literature, the point has received but little attention. Granting that the gastrointestinal phenomena represent some reflex irritation of sensory nerves, due to the presence of a new protein element in the metabolism, it is natural that this sign should accompany the development of an embryo, whatever its situation. If, however, the nausea be due to a direct referred irritation of the uterine nerve supply itself, as is held by a large number of obstetricians, there would seem to be but little reason for the occurrence of this symptom complex in extra-uterine gestation.
The fact remains that, in about one half of the cases careful amnesis will bring out the fact that morning nausea and occasional vomiting has been noted. This must not be confounded with the vomiting which so usually develops with beginning rupture, as a result of the irritation of the peritoneum by the presence of free blood.
As a diagnostic factor, this morning nausea and vomiting is of no positive importance, but must be regarded as rather of negative value. Pain and colostrum in the breasts are usually present in some degree. In Farrar's one hundred cases pain and colostrum were present in eighteen, 18 per cent. In Frank's 12 analysis he states that "pain and the presence of colostrum in the breasts were repeatedly noted in the histories." Bandler thinks it uncommon. Taylor found enlarged and tender breasts in 44 per cent of his cases.
The subject may be dismissed with the comment that breast changes are unimportant in so far as a diagnosis of ectopic pregnancy is concerned, but that their presence contributes to the knowledge that the patient is pregnant in some wise.
Increased pigmentation, the appearance of the linea nigra, and the darkened mammary areola, are signs so frequently absent or but vaguely present, even in intra-uterine pregnancy, that they must, of necessity, play but a small role in differentiating extra- from intra-uterine gestation.
The local signs of pregnancy, when present, and they usually are present in some degree, may easily confuse the diagnosis. Softening o£ the cervix and increase in the size of the uterus are the rule in these cases.
In Farrar's one hundred cases, the cervix was softened in twelve and the fundus enlarged in 32, 44 per cent, thus showing change in the size and consistency of the uterus.
Inasmuch as there is always a decidua formed in the uterus when an" ovum is impregnated, enlargement of the organ, even though small in degree, is always to be expected in cases of ectopic pregnancy.
The uterus is usually sharply anteflexed, as pointed out by Oastler, 10 who regards the anteflexion as an important fact in differentiating between ectopic pregnancy and old tubal disease, since in the latter the adhesions formed tend to pull back the uterus in retroposition, whereas in ectopic gestation the pathological condition does not exist long enough to cause any adhesions.
Frequency of urination is noted in something less than one half of the case records examined, though in one of the writer's cases it was the paramount symptom and the one which brought the patient to her physician for relief. It is not a sign of any diagnostic import, except that it may be regarded as slight affirmative evidence of the existence of pregnancy.
The Abderhalden reaction is mentioned merely to emphasize the fact that, as a diagnostic factor, it is of only the slightest value. When positive, it may be regarded as one more point in favor of a diagnosis of pregnancy, but the absence of the reaction by no means negatives the possibility of pregnancy having occurred, nor does it in any way assist in the diagnostic separation of extra- from intra-uterine gestation.
Pain in the pelvis, usually occurring in a more or less definite cycle, is the most important and constant sign of ectopic pregnancy, more noteworthy after rupture or tubal abortion has taken place, but a most significant symptom, even before any blood has escaped from the tubes.
In the analysis of Wynne 13 pain was the predominant symptom in 254 of 303 cases, or 84 per cent. In Farrar's 3 series of 186 cases, pain with or without bleeding was present in 96.6 per cent.
Out of Williams' series of 147 cases, pain was present as the chief symptom in no, or 80 per cent.
Ninety-five per cent of Frank's cases gave pain as an important symptom.
Such instances may be multiplied indefinitely, though in using these series of case. records as indicative of the predominance of pain as a symptom, it must be remembered that the cases are not usually classified as to the degree of rupture or the extent to which traumatism has advanced within the peritoneal cavity.
The etiology of the pain is threefold. First, when the ovum dies or separation of the embryonal envelopes from their abnormal decidua begins, the ovum becomes a foreign body and the tube makes efforts to expel it, via the fimbriated extremity, by means of vigorous peristaltic action on the part of its muscular coat. The clinical expression of this tubal muscular contraction is colicky pain, noted first in the region of the diseased tubes and later transmitted to the uterus, which in time begins to undergo contraction.
Second, under the circumstances present there is usually a variable amount of bleeding into the peritoneal cavity, and generalized dull, lower abdominal pain becomes a noteworthy symptom, as a result of the sensory reaction of the peritoneum to the irritative effect of blood in direct contact with it.
Third, as the blood accumulates within the pelvis, it gravitates to the most dependent portion and forms a clot or masses of clots in the cul de sac of Douglas, with the development of pain especially noted during defecation, as the fecal masses impinge upon the blood clot and force it against the sensitive peritoneal surface and the uterosacral ligaments. The importance of this symptom of painful defecation has been emphasized by Polak, who notes that on several occasions, it has been the first point, when taken in conjunction with a skipped or delayed menstrual period, to direct his attention to the possibility of ectopic pregnancy.
Lastly, if an effusion of blood takes place into the tubal wall, or between the folds of the broad ligament, then will follow a dull throbbing, pressure pain as the increasing amount of blood distends the tissues.
The types of pain which have just been described may be present in any combination in any case; but in order to elicit this phase of the symptomatology from the patient, it is obvious that very careful and patient questioning is necessary, and further, in developing the history, great care must be taken that too much insistence be not laid upon any one symptom, lest the woman be influenced by the suggestion and describe sensations she did not in reality experience.
The Previous History. — The older writers upon extra-uterine pregnancy laid great stress upon a history of sterility, a long period of marital life since the birth of the last child, evidence of preexisting pelvic inflammation, and a record of previous consecutive gynecological operations. Let us examine the very careful analysis of later writers who have observed long series of cases, and ascertain in how far their early opinions are correct.
Parry, in his classical work, says that "ectopic conception occurs most frequently in women showing previous inaptitude for conception," and these oft quoted words have been the keynote upon which later writers based their statements.
Absolute Sterility. — In Farrar's series of 186 cases, 31, or 16.6 per cent, were absolutely sterile, but of these 31 cases, 15 had been married less than five years, and therefore, in the light of present day ideas with respect to the prevention of conception among recently married couples, it would seem, at best, a matter of great doubt whether patients of less than five years marital experience should properly be listed as sterile. Frank 12 analyzes a series of eighty cases, and in these, even if the short and insufficient period of one year is regarded as an arbitrary criterion of sterility, only 7.5 per cent fall into this class.
In Rongy's series of 84 cases, 17 patients had not previously been pregnant (20 per cent), but, as Rongy does not mention the length of time these women had been married, it is fair to assume that a reasonable proportion had been living under marital conditions for so short a time that they were not true cases of sterility.
Foskett 4 found that 27 of his 117 patients had not previously been pregnant (21 per cent). Here, too, however, the length of time married is not mentioned, so that the percentage is in all probability much too high to regard as representative of the proportion of absolute sterility in the series.
Among Taylor's 9 patients, there were 4 cases of absolute sterility in 46 patients, or a percentage of 8.6 per cent.
Averaging the above figures, it is found that 15 per cent of patients in whom extra-uterine pregnancy exists have not previously been pregnant, but, as has been shown, the length of time married is not mentioned in a number of the statistics, and when it is recorded, this time is too short to properly constitute a true pathological sterility.
In the careful study of MacKenzie 6 there had been no previous pregnancy in 23 per cent of the 150 cases studied, or 15 per cent.
It is estimated that from 10 to 12 per cent of marriages among Caucasians are sterile, as a result of either male or female disability. If to this number there be added the marriages rendered unfruitful by deliberate intent, and such are by no means uncommon, it will be seen that, inasmuch as sterility, using the term in its most loose sense, only occurs in from 7 to 15 per cent of all women suffering from ectopic gestation, this factor, as a casual lesion, plays but a minor role.
When, however, the comparatively unfruitful marriages are considered, the so-called one child sterility, or those cases in which the offspring have been limited either as a result of some pathological process in husband or wife, or by methods designed to prevent conception, the proportion of extra-uterine gestation rises to a marked extent.
For example, MacKenzie 6 found, in his study of ectopic pregnancy, that 30 per cent of his patients had borne but one child, and 26 per cent had two previous pregnancies recorded. This leads him to remark that the greatest liability attaches to one pregnancy, and extra-uterine gestation is more likely to occur in the mother of a small family, since in 80 per cent of his cases there was a history of three or less previous pregnancies.
Farrar's series shows 32.2 per cent of cases occurring in relation to one child sterility, and in Rongy's eighty-four patients, forty-six had had three or less previous pregnancies, while among Williams' records of 121 histories, 64 patients were the mothers of less than three children.
Summary. — The conclusion to be reached in the matter of sterility as an etiological factor is that absolute sterility is an indefinite and unimportant point in the development of the diagnosis, while the fact that one or two children have been born over a period of years, is a diagnostic point of considerable value, when taken in connection with the other significant details of the history and physical examination.
The birth of many children in rapid succession has been held to be a factor in the etiology of ectopic pregnancy. Polak X1 says that the condition arises frequently among women who are the subjects of rapidly recurring and repeated pregnancies, as may be found among our foreign population, particularly the Jews, Italians and Irish. This observation is not generally borne out by a survey of other statistics.
Only 10 per cent of MacKenzie's patients had borne five or more children, and 2 per cent had borne seven or more. Frequent fecundation is not therefore to be considered as important in studying a case history.
The passage of a considerable interval of time between the last, pregnancy and the extra-uterine, is usually regarded as significant in an etiological sense.
MacKenzie found that 42 per cent of his cases occurred within two years of a previous pregnancy, and 59 per cent followed within 5 years of childbirth.
In one hundred cases of Farrar's 68 had borne a child or suffered a miscarriage five years or less previous to the development of the ectopic condition.
The average time elapsing in Williams's 79 cases, where the date of this preceding normal pregnancy or miscarriage was given, before the ectopic gestation developed, was three years and nine months.
In Rongy's series the last pregnancy occurred less than five years prior to the ectopic in 31 of a total of 45 cases.
If the foregoing figures be surveyed, it must be agreed that the length of the intergravid period is not a constant nor valuable detail in arriving at a diagnosis.
Pre-existing Pelvic Disease must of necessity be of prime importance as a causative agent; but unfortunately, the clinical signs of a pelvic lesion may be slight and indefinite, and a pathological condition well able to cause peritubal adhesions with kinking or strictures of the tubal lumen, may have not greatly disturbed the patient during its acute stage and, in consequence, is frequently forgotten by her when giving a history of past complaints, especially during the stress of hospital residence with a prospective abdominal operation in view. Farrar shows an incidence of 10 per cent of histories of infection. Oastler's series contained 22 cases of pelvic infection in a total of 106, or 20 per cent.
It is probable that, were it possible to obtain these details, a very high percentage of all causes of ectopic pregnancy would be found to have suffered from preexisting pelvic infection of some type. As the facts in these relations cannot be obtained, it must suffice that a history of previous pelvic disease is to be considered a strong affirmative point in a diagnosis of extra-uterine gestation, but the absence of such history cannot be regarded as of any negative value.
Previous operations on pelvic viscera or upon those organs occupying the inferior portion of the abdominal cavity, often leave such alterations in the normal anatomy of these parts as to predispose strongly to the subsequent development of extra-uterine pregnancy. This feature of the history, however, as a diagnostic point is greatly weakened, should the patient have experienced a normal pregnancy in the interval between the operative procedure and the development of a suspected ectopic gestation.
Oastler found that 13 of his 106 cases had been subjected to previous abdominal operations; Farrar, 16 in 186 cases, including four previous ectopics; and Foskett found histories of 6 women previously operated upon in a total of 117 cases.
Considering the comparatively small proportion of women who have been subjected to laparotomy, in relation to the feminine population as a whole, it is clear that, inasmuch as nearly 9 per cent of a large series of cases of ectopic pregnancy have had previous abdominal sections performed, this feature of the history is of prime importance as a positive factor in reaching a diagnosis, and great stress should accordingly be laid upon it.
The General Health and the Medical History of the Patient. — In a broad sense, tendency to infectious diseases, traumatism, and the like seem to have no etiological bearing on the development of extrauterine pregnancy.
A review of the anamnesis, then, from the "diagnostic standpoint would lead to the following conclusions :
1. Previous general health, and family history is of no diagnostic value.
2. Absolute sterility is not definitely associated with the occurrence of ectopic pregnancy.
3. Relative sterility, especially the one child type, on the contrary, is a significant point, and should be regarded as moderately affirmative.
4. The passage of a considerable interval of time between the last
intra-uterine pregnancy and the present suspected ectopic one is unimportant in diagnosis, and may be disregarded.
5. A history of preexisting pelvic disease is of great importance
when obtainable, but the absence of such history should not be an influence against a positive diagnosis of ectopic fecundation.
6. Previous abdominal operations indubitably render the patient
more liable to aberrant imbedding of the fecund ovum.
The Findings on General Examination of the Patient. — Where a tubal pregnancy is present, before rupture or tubal abortion has taken place, the physical signs are in general negative, as to a diagnosis. The blood and urine usually show no change referable to the condition, the blood picture especially being in striking contrast to that noted after rupture has occurred.
The physical findings in cases of beginning rupture or tubal abortion in tubal pregnancy are quite frequently definite enough to be considered pathognomonic. They consist of the presence of a tender mass occupying the site of one or the other tube, with or without a doughy fullness in the posterior vaginal fornix and the palpatory evidence of a blood clot in the cut de sac of Douglas.
Farrar's series revealed a pelvic mass or a definite enlargement of adnexa on one side in 96 of 100 cases, or 96 per cent. Frank found a palpable mass in one of the fornices or in the cul de sac in 86 per cent of his cases. The mass was usually described as "boggy," and was regularly tender on pressure. As a rule, vascular pulsation over or in the neighborhood of the mass was exaggerated. This sign of vascular pulsation has been emphasized by several observers, but in the opinion of the writer is of but slight value, being frequently noted in cases of normal pregnancy, as well as those of acute or subacute salpingitis.
Among Oastler's records of 106 cases, pelvic masses were noted in 86 per cent. The masses are not usually large, nor are they dense in consistency, but are soft and not too easily demonstrable. It is noteworthy that the tenderness on vaginal examination is usually out of all proportion to the size and density of the mass palpated, and to the experienced gynecologist the disproportionate tenderness is highly suggestive of the presence of an ectopic gestation, as against acute salpingitis. Traction on the cervix or active manipulation of the uterus greatly aggravates the pain and tenderness.
The uterus is generally in anteflexion, since, as pointed out by Oastler, the adhesions formed in inflammatory conditions tend to pull back the uterus in retroversion, whereas in ectopic pregnancy the pathological condition does not exist long enough to cause this position. Oastler found, in 106 cases, anteposition in 87 and retroversion in 19.
Size of the Uterus. — The uterus, when ectopic pregnancy exists, is usually enlarged, though the enlargement does not bear the proper relation to the duration of the pregnancy, as determined by the history, being in general less than would be the case, did intra-uterine pregnancy exist.
For practical purposes, the enlargement of the uterine body is of but little value, since, as most tubal pregnancies are terminated by rupture or tubal abortion before the tenth week, the uterine enlargement is so slight as not to be demonstrable, especially in cases when previous pregnancies have occurred and a relative increase in the size of the uterus is physiological.
Cyanosis of the vaginal mucosa has already been discussed.
Hegar's sign is not to be elicited, no matter what the size of the uterus, and is therefore of considerable negative value in determining a diagnosis. Should Hegar's sign be present, together with the other signs, intra-uterine pregnancy is almost a certainty, though it may well be complicated by a coexisting tubal gestation.
The passage of masses of decidua or complete decidual casts from the uterus is of great value positively, but of no great negative importance, since the decidua may well have been passed previous to the patient's coming under observation. Should a decidual cast be passed, it does not offer definite proof of the presence of extra-uterine pregnancy, since such structures are found sometimes in early intra-uterine pregnancy, with death of the embryo.
Microscopical examination will settle the diagnosis in such instances, the finding of chorionic villi in the decidual tissue establishing the diagnosis of intra-uterine abortion, while the presence of decidual cells without villi predicates the existence of extra-uterine pregnancy (see Decidua, in section on pathology).
It is most important that extreme gentleness be employed in the conduct of bimanual examination in a case of suspected ectopic gestation.
All too often has the tube been ruptured in the physician's office and the patient placed in deadly peril of her life, by a neglect of this precaution.
On no account should a uterine sound be used.
The abdomen in these cases is usually rigid to some degree, the rigidity naturally affecting more definitely the rectus muscle on the side of the affected tube.
The abdomen is generally tender on palpation, though a marked difference is usually noted between the degree of abdominal tenderness and that elicited by the vaginal finger in the course of a bimanual examination. There is frequently present a moderate degree of abdominal distention, rarely excessive. The attacks of pain are accompanied by nausea and vomiting in about one half the recorded cases, while at this stage syncope is rare. In general, when beginning tubal abortion or minute rupture of an ectopic gestate sac has occurred, the condition of the patient is strongly suggestive of an "acute abdomen" of moderate severity, without any localizing or pathognomonic symptoms to be detected outside the genital tract.
The pulse is usually slightly elevated, running between 86 and 92 in the writer's experience. The temperature is almost always slightly elevated, as an expression of the peritoneal reaction to the presence of free blood, and secondarily to the very common development of a mild pelvic peritonitis about the extravasated blood and the tube itself. This point was well brought out by Brickner in his study of cases from Mt. Sinai Hospital.
The temperature is usually not high, ranging from 99 to 102 R, rarely above the latter figure.
The blood picture reveals a commonly present leukocytosis of low degree, usually about 10,000 or 12,000, again an expression of peritoneal irritation by extravasated blood. The leukocytosis in these cases behaves in a characteristic manner which, when doubt exists, forms a valuable adjunct to the formulation of a correct diagnosis.
If the hemorrhage be inconsiderable in amount, the leukocyte count rises slightly within a few hours after the bleeding begins, while the red cells show no appreciable diminution in number, nor is the hemoglobin percentage affected.
The leukocytosis in these instances is due entirely to the peritoneal irritation set up by the contact of free blood with its -cells. In twentyfour or forty-eight hours this slight leukocytosis disappears and the entire blood picture is a normal one. Now if, as usually is the case, repeated small hemorrhage occurs, the leukocyte count will rise with each fresh outpouring of blood, until, after several such hemorrhages have taken place, the white count may reach 11,000 or 12,000 and remain at this figure for several days.
By this time the red cells will generally be found slightly decreased in number and the hemoglobin is slightly lowered.
When a sudden and profuse hemorrhage develops, the red cells and hemoglobin are sharply diminished, while a few hours after the hemorrhage the white count becomes fairly high — 20,000 to 25,000.
In cases of severe, sudden hemorrhage, the writer regards a high leukocyte count as fairly direct indication of the amount of blood lost, the white cells rising in direct ratio to the severity of the hemorrhage. The polynuclear cells also rise rapidly in percentage under the condition of large intraperitoneal hemorrhage.
The hemoglobin count is not of great value in ectopic pregnancy, since there is no immediate drop, and the lowest point is not reached until forty-eight to seventy-two hours after the involved vessel has undergone rupture.
The highest leukocyte count noted by Taylor in his series of cases was 46,000, with a polynuclear cell percentage of 95. In Farrar's series only one case had a leukocyte count above 25,000, while Foskett in 117 cases found a white count of 20,000 or over in 17, with a corresponding increase in the polynuclear cells.
There is a considerable factor of error in statistics concerning blood counts in ectopic gestation, since the writers do not specify the nature of the lesion in detail, and do not separate the cases of slight rupture or beginning tubal abortion, such as are under discussion here, from those of violent and profuse hemorrhage.
To sum up the condition of the blood in this group, it may be said that the existence of a mild leukocytosis, not above 12,000 cells, which develops within a few hours of an attack of pelvic pain, subsides in 48 hours, and rises again coincident with another attack of pain, is suggestive of the presence of an ectopic pregnancy, with small and repeated hemorrhage into the peritoneal cavity, especially if the red cell count and the hemoglobin proportion show no reduction from the normal.
Blood Pressure usually is unchanged, and variations of pressure are of no diagnostic import, unless the hemorrhage is of the profuse type, which will be considered elsewhere. A most important fact in the semiology of ectopic pregnancy is that the symptomatology is generally that of a subacute disease, rather than one of fulminant type.
Sudden onset of the so-called tragic type, without previous warning of the presence of pelvic pathology, is the exception rather than the rule. The usual type is that in which, after the menstrual disturbances, as described, have been noted by the patient, there is a short, but not overwhelming attack of abdominal pain, followed by uterine bleeding. The pain may, and frequently does, entirely disappear for a period of days or even weeks, to recur in repeated exacerbations until the case terminates in one of these ways — either a sudden violent attack of pain, with massive intraperitoneal hemorrhages, shock, syncope and collapse, with death or recovery upon operative interference, or a continuance of attacks of pain, with slow hemorrhage, gradual severe anemia, infection of the hematocele and death from exhaustion or sepsis, unless recovery results from successful surgery.
A third termination occurs much more commonly than is generally supposed. That is, the ovum dies, either as a result of rupture of the tubal wall or by tubal abortion, the hemorrhage ceases spontaneously, and the clot remains uninfected, to be gradually resorbed, with the complete recovery of the patient, who may have been entirely ignorant of her condition, supposing her illness to have been due to an early abortion, a view frequently shared by the medical attendant.
Recovery is rarely complete, however, since adhesions usually form about the affected tube, drawing it into contact with the area occupied by the hematocele in the cut de sac of Douglas, and leaving a condition strongly suggestive of an old low grade unilateral salpingitis, for the relief of which the patient sooner or later comes to operation. On exposing the internal genitalia there are found the evidences of a damaged tube, with no evidence of purulent change, but with fairly dense adhesions, causing the tube and ovary to lie fixed, behind the uterus.
The writer has noted this condition in several instances, and in one case, at least, there were found, on careful examination, syncytial shadows in the tubal wall, which were evidently the remains of old chorion formation.
The diagnosis of ectopic gestation, if properly made, at the stage of beginning tubal abortion or minute rupture, will obviously result in the institution of operative procedure before any great damage is done by severe hemorrhage, and when such operative interference is practiced at this time, the mortality will be surprisingly low. The diagnosis should be easily determined, provided careful study of each case be carried out, and if all the facts be collected and logically scrutinized. The whole matter has been excellently epitomized by Philander Harris, who, writing in 1907, says, "When any woman after puberty and before menopause, who has menstruated regularly and painlessly, goes four, five, six, eight, ten, fifteen to eighteen days over the time at which menstruation is due, see? blood from the vagina differing in quality, color, quantity or continuance from her usual menstrual flow, and has pains, generally severe, in one side of the pelvis or the other, or possibly in the hypogastric region, ectopic pregnancy may be presumed."
The Diagnosis of Ectopic Pregnancy when frank rupture of the tube or rapid tubal abortion has taken place, with massive hemorrhage into the peritoneal cavity.
In entering into the consideration of this group of cases, one is struck with the repetition of the word tragic in the literature. Indeed, so apt is that designation, that certain writers divide cases into those of the pretragic and those of the tragic stage. Here it is that the early mortality was appalling, and herein lies one of the signal triumphs of gynecology, that with the multiplication of competent operators, the widespread development of the hospital idea, and the diagnostic knowledge of the condition, so generally possessed by the medical profession, and to some degree, even by the laity, the mortality, even at a time when the tides of life are at their lowest ebb, and when each feeble cardiac contraction seems certain to be the last, has been reduced from 75 and 85 per cent to 6 or 10 per cent at the most.
The classical description of the symptomatology of sudden tubal rupture, with violent hemorrhage, has been quoted and taught so extensively, that any serious medical student, if confronted with the symptom complex as presented in textbook descriptions, can hardly fail of a diagnosis.
Unfortunately, the sudden rupture of a pregnant tube very frequently is followed by a train of events far removed from that so generally thought to be connected with the accident.
It has been the habit of the writer to divide these cases into two great divisions, which, for lack of a more accurately descriptive terminology, have been termed asthenic and sthenic. The two are found fairly equally divided, the former somewhat in the majority.
The asthenic group of cases includes those women in whom rupture of a pregnant tube produces a reaction of which depression is the dominant factor. These are the women who, while engaged in household duties or while walking about, are suddenly and without premonitory symptoms seized with an agonizing and lancinating pain in the lower abdomen, which is usually accompanied by extreme nausea and vomiting, to be rapidly followed by syncope, collapses and shock. The pulse is of a steadily increasing rate and equally decreasing volume, with cold, clammy, leaking skin, subnormal temperature, pallid features, the skin frequently of a lemon tint by reason of the extreme anemia, rapid and shallow respirations, with frequent sighing, contracted pupils, a facies of extreme anxiety, intense restlessness, thirst, air hunger, and with mentality unimpaired, indeed often too sharply acute.
Examination reveals an abdomen possibly slightly distended, rigid on the affected side, and often exquisitely tender to palpation. On vaginal examination, the posterior vaginal fornix is bulged with clots, and presents a doughy feel to the ringer. The ruptured tube is not usually to be palpated, since it is imbedded in recent clot and its outlines are obscure.
The urine is scant, but otherwise unchanged. The blood shows no great disturbance of its red cells during the first few hours, though later profound anemia is demonstrated by the hemoglobin estimation. The leukocytes rise rapidly in number, with a corresponding preponderance of polynuclear cells. For example, in one fatal case occurring in the writer's experience, the leukocyte count registered 24,600 with 92 per cent polynuclear cells, a hemoglobin of 70 per cent, and erythrocytes to the number of 2,680,000, the count being made six hours after the sudden onset of symptoms. The blood pressure is usually low, 90 to no systolic, but the pulse tension remains constant, and herein lies a most important diagnostic feature, for which we are indebted to Polak, who pointed out that pulse pressure remains fairly constant in cases of intraperitoneal hemorrhage, i.e., the ratio between systolic and diastolic pressure does not markedly change, both rising or falling together. In cases of shock, on the other hand, there is usually a marked irregularity in the pulse pressure, the ratio between systolic and diastolic pressure varying sharply from time to time.
Needless to say, the history of patients presenting such train of symptoms will usually coincide with that typical of ectopic gestation as previously outlined, and careful questioning will generally bring out the fact that there have been one or more attacks of pelvic pain, not necessarily of sufficient severity to cause the woman to suspect any serious pelvic lesion, but characteristic in behavior.
There are two local signs, which, when demonstrable, are of diagnostic value.
Pallor of the cervix uteri on inspection has been described as a sign of value. In one case in the practice of the writer the blanched, white appearance of the cervix, when distended by the speculum, was in sharp contrast to the deep and congested vaginal mucosa, and when the fundus uteri was exposed upon opening the abdomen, the entire uterine body was seen to be pallid and bloodless.
Another sign only occasionally noted, but of value when present, is a bluish black discoloration about the umbilical region. This was demonstrated by Cullen, 14 who reports the following case: A woman thirtyeight years of age suddenly developed abdominal pain and distention. Dr. Cullen saw her three weeks later. The umbilical region was bluish black, although she gave no evidence of injury. Vaginal examination yielded nothing, on account of the abdominal distention. Under ether, however, a mass eight by six centimeters was clearly felt to the right of the uterus. Extra-uterine pregnancy was at once diagnosed, although the patient had missed no period and there was no uterine bleeding. On opening the abdomen he found a right sided extra-uterine pregnancy and about one and one half quarts of free blood in the abdomen.
Hematinemia and jaundice as diagnostic signs have been described by Schottmuller, 15 who found that "in cases of jaundice of obscure origin the discovery of hematin in the blood serum served to confirm the suspicion of a ruptured extra-uterine pregnancy in one of the cases he relates. The spectroscope revealing the hematin indicated the necessity for an immediate operation, which was followed by speedy recovery ; the history and palpation findings had suggested a benign ovarian cyst. In two other cases the small proportion of hematin, while confirming the diagnosis of extra-uterine pregnancy, yet showed that there could not have been much extravasation of blood, and both the patients recovered without complications or operation. He has encountered four cases of jaundice with extra-uterine pregnancy in the last year; the tendency to jaundice was evident only in the conjunctivae, but this was enough to suggest hematinemia, and the spectroscope confirmed it. Urobilin was evident in the urine in some, but not all of the cases." The writer has had no experience with this phenomenon.
Dullness in the flanks on percussion has been described, but has not been noted by the writer, nor has DeLee seen this phenomenon.
Retention of urine occasionally occurs, Farrar recording it in four of her 1 86 cases.
The diagnosis of this asthenic type of case usually presents no difficulties, the sudden onset, the intensity of the symptoms, and the profound depression of the vital activities being so marked as to at once direct attention to the fact that rupture of a large intra-abdominal vessel has occurred. Differentiation must be made between ectopic pregnancy, a ruptured intestinal ulcer, and tubal or ovarian hemorrhage, the result of lesions not connected with an aberrant pregnancy. These differential points will be discussed at the appropriate place.
The sthenic type of reaction of the organism to. such an event as the rupture of an extra-uterine pregnancy is not found in descriptions of this accident, and the writer has not seen this very common clinical picture discussed at any length in the literature devoted to the subject.
In certain robust, florid women the rupture of a tubal pregnancy with intraperitoneal hemorrhage gives rise to a reaction, in which all of the physiological activities are stimulated rather than depressed, as in the classical or asthenic group.
Such a patient will present the characteristic previous history, which marks her as predisposed to ectopic gestation, and has had the usual amenorrhea, followed by attacks of pelvic pain more or less severe and attended by uterine bleeding. The frank rupture occurs with sudden violent pain in one or the other iliac fossa, possibly with nausea, vomiting or syncope, from which the patient rallies in a short time, after which the abdominal pain becomes generalized and acute, the temperature rises to 101 to 103 degrees, the pulse remaining full and strong, of excellent volume and rarely above no in rate. There is a sharp leukocytosis, averaging above 12,000, no marked hemoglobin alteration, and no especial diminution of the number of erythrocytes. Blood pressure is usually slightly above normal, pulse tension remaining constant.
On physical examination, the face is anxious, though usually not pallid and the mucous membranes retain their healthy tint. The abdomen is distended, moderately tympanitic, and extremely tender to pressure. Marked rectus rigidity is the rule, usually most intense on the affected side. Vaginal examination may or may not disclose the presence of a tubal mass, though usually there is the vague sensation of a doughy fullness in the cul de sac. A diagnostic point of value here, as in the other type of case, is the extreme tenderness elicited upon bimanual examination. There is usually some slight bleeding from the softened cervix, though this feature may be entirely absent. Obviously, the resemblance of the above symptom complex to that of an acute inflammatory process, acting in the lower abdomen, is so clear, the physical findings so parallel each other in the two conditions, and in both the clinical course of the patient is so similar, that diagnosis presents the greatest difficulties. It is common to find such cases diagnosticated as acute salpingitis and treated expectantly, until the temperature falls to normal and all evidence of acute pathological process has subsided, when, on the performance of a laparotomy, and not until then, is the true existence of the lesion recognized.
Happily such diagnostic error does not result in any harm being done the patient. Inasmuch as the life of the embryo is destroyed at the time of rupture and the hemorrhage ceases spontaneously, there remains an aseptic hematocele, which, on operation, is usually found to be undergoing absorption or contraction. Its removal is accomplished without undue difficulty and uneventful recovery is the rule. The only significant diagnostic points in this type of case are the characteristic ectopic history, the enlargement of the uterus with bleeding, and the extreme tenderness of the palpated tube. Amenorrhea followed by bleeding, however, is a common incident of acute salpingitis, so that for practical purposes there remains but the history and the excessive tenderness as definite points on which to base a diagnosis.
A typical case of this variety is the following, which occurred in the practice of the writer. A strong, healthy woman of 34 years, who had borne four children normally, had had one miscarriage with some fever following, two years before coming under observation. She had missed one period and after three weeks complained of some pain in the right side. There was no uterine bleeding nor was the pain severe enough to lead the patient to consult a physician. While engaged in household duties, the woman began to complain of a sharp pain in the right iliac fossa, which rapidly grew intense and forced her to lie down. She was seen by Dr. Wm. G. Shields, Jr., and by him referred to the writer's service at Frankford Hospital.
On admission her condition was as follows : Temperature 102. 4 R, pulse 96, respiration 20, leukocytes 13,000, hemoglobin 85 per cent, red cells 4,600,000. Blood pressure 130-75. The face was flushed, the chest was negative, the abdomen tympanitic and very rigid, the right rectus muscle being board-like in consistency. The entire abdomen was extremely tender.
On vaginal examination, the uterus was fairly large and movable, though pressure and manipulation of the slightly softened cervix occasioned great pain. There were none of the general or local signs of early pregnancy. An exquisitely tender, small mass was palpable in the region of the cut de sac. A provisional diagnosis of acute salpingitis with pelvic peritonitis was made, and the patient placed upon expectant treatment. In considering the case with the house staff, after the examination had been concluded, the intensity of the pelvic pain on pressure drew the writer's attention to one case he had previously seen, and, on the strength of this point and the history above, the diagnosis was altered to that of a ruptured tubal pregnancy and immediate operation was performed. The right tube was the seat of an early tubal pregnancy, which had undergone rupture, and the abdomen was literally full of liquid and clotted blood. The rupture in the isthmus of the tube was one millimeter in diameter, and a portion of the oval sac was protruding from the rent. There was no evidence of any inflammatory process whatever. The tube was excised, the incision closed, and the patient made an eventless recovery. Although a massive intraperitoneal hemorrhage had taken place in this case, there were absolutely no clinical data upon which to base a diagnosis of such accident, and, as has been said, the history and the inordinate tenderness were the sole points upon which a diagnosis of ectopic pregnancy could be formulated.
The Diagnosis of Long Existing and Untreated Ectopic Gestation (hematocele, tubal mole, lithopedion formation, etc.).
The older literature is replete with discussions anent the recognition and treatment of encapsulated masses of blood clot, occupying the pelvic cavity, and usually of long standing, the condition termed hematocele. As time went on, the space devoted to consideration of the hematocele and its treatment became steadily smaller, until, in the most recent works along these lines, the subject is dismissed with but a scant paragraph or two.
The reason for the change in thought is, of course, that following the generally disseminated knowledge concerning ectopic gestation and its almost universal treatment by immediate operation, the occurrence of hematocele, like that of vesicovaginal fistula, has so diminished as to be an almost negligible factor in either diagnosis or treatment. Hematocele has previously been defined as an encapsulated mass of blood clot, usually filling the pouch of Douglas, and occasionally extending laterally to the uterus.
It results from the rupture of a vessel in the peritoneal cavity, with consequent intraperitoneal hemorrhage, which later undergoes partial absorption, fibrinization, and forms a dense, elastic mass closely applied to the posterior surface of the uterus and molded into the cul de sac.
Not uncommonly the hematocele has been the seat of an infection, which on subsiding has left a tissue of peritubal and peri-ovarian adhesions in its wake. The symptomatology of this condition is vague and obscure. There is usually long continued dull pelvic pain, periodically more or less severe, according to the general condition of the patient and the amount of exhausting physical effort performed by her. Dyspareunia is commonly noted. On physical examination, there are no blood or urinary changes, except the hematocele be undergoing an acute or subacute suppuration, when leukocytosis is the rule, together with some elevation of temperature.
Rigidity of the rectus muscles is not present, nor is there apparent any special tenderness when the abdomen is lightly palpated. On vaginal examination, there will be found a firm, elastic mass in the pouch of Douglas, with the uterus riding upon it anteriorly. The latter organ is generally fixed and immovable. Both adnexa are adherent and the parametrium fixed and dense.
Diagnosis between such conditions and old chronic salpingitis is not to be made from the physical findings, and is only rendered possible by the development of a history of a previous train of symptoms, pointing to the rupture of a tubal pregnancy.
Puncture of the cul de sac with an aspirating needle has been advocated, the withdrawal of blood confirming the diagnosis of hematocele. This procedure is but of doubtful value, since, if the clot be sufficiently organized, no blood will escape through the needle, and in addition there is a certain danger of infection in this process, which is entirely unnecessary, since the operative measures indicated in the treatment of both hematocele and old salpingitis are identical. A most interesting case of this type occurred in the practice of the writer : A woman of 34, who had borne no children and had no record of miscarriage, had been complaining for two years of general pelvic pain, worse on exertion and at the menstrual period. The pain was always dull, though at times quite severe. There were associated dyspareunia and leukorrhea. On examination, the temperature and pulse were normal, leukocytes were 8,500, hemoglobin 85 per cent, and there was nothing suggestive in the general physical condition of the patient.
On vaginal examination, the uterus was found fixed, a dense hard mass filling the cul de sac and extending along the inferior border of both broad ligaments, with both tubes and ovaries fixed, enlarged and adherent. Provisional diagnosis of chronic salpingitis and parametritis was made and the patient admitted to Frankford Hospital for operation. When the usual detailed hospital history was studied, it was noted that the patient stated she had had a period of amenorrhea four years previously, which was followed by a sudden severe pelvic pain, with syncope and confinement to bed for three weeks, after which she recovered, menstruation reappeared, and she resumed her usual life. On the basis of this history alone the diagnosis was changed to that of old ruptured ectopic pregnancy with pelvic hematocele.
On exposing the pelvic region by laparotomy, there was found a large, old, encapsulated blood clot, which had evidently undergone inflammatory change, since the tubes and ovaries were closely adherent to, it. The case eventuated in a difficult hysterectomy, from which the patient made a good recovery.
Microscopical examination of the tissues removed, disclosed an old tubal mole in the right tube, with distinct evidence of a large rupture on the superior surface. This case is cited to again, emphasize the immense importance of a careful history in the diagnosis of ectopic pregnancy in all its phases.
The Diagnosis of Ectopic Pregnancy Other Than Tubal. — Interstitial, or, as the writer prefers to term it, cornual pregnancy, was formerly regarded as extremely rare, Tait finding only six specimens in English museums up to 1890. At the present time, with the growth of accurate diagnostic methods and prompt surgical intervention, this lesion is known to be comparatively common.
The diagnosis is difficult before rupture and usually impossible after this accident, since the phenomena are identical with those of a ruptured tubal pregnancy. In this connection the differential diagnosis is of no import, since clinically the two conditions are identical and the same treatment is indicated for both.
Rupture of an interstitial pregnancy is a grave lesion, owing to the tension under which the distended uterine muscle labors, and to the very rich blood supply of this portion of the uterine body. The diagnosis before rupture depends upon the usual ectopic history, the variable presence of the associated signs of pregnancy, and particularly the detection, upon vaginal examination, of an irregular enlargement extending around one uterine horn and merging completely with the general contour of that organ. There is never a pedicle or any area of differentiation between the enlarged horn and the uterus proper. The enlarged area may present a sense of great tension and very firm distention, and the tube and ovary may be of normal outline.
In the diagnosis of cornual pregnancy, the following mistakes are commonly made, according to Kustner; 16 on the one hand they are thought to be cases of normal pregnancy, with marked hypertrophy of the cervix, the true uterine cavity being mistaken for the cervical canal, and on the other hand they have been considered as incomplete abortions, the muscular diaphragm next the uterine cavity being mistaken for an extremely well marked contraction ring.
Pain is early and, in contradistinction to that of tubal pregnancy, usually develops before bleeding or death of the ovum occurs, this being due to the fact that the uterine horns withstand distention badly and pain begins shortly after even slight distention takes place.
An excellent illustrative case is one reported by the writer. 17 The patient was a lady of thirty-four years, the wife of a physician. Her previous history was uneventful, menses regular and normal, no illness of note. She had previously borne two healthy children, the first labor a slow instrumental one, the second easy and spontaneous. She had had two early miscarriages in the first years of her married life. In February, 1911, she noticed some delay and irregularity in the menses. This condition persisted until May, when there developed absolute amenorrhea with the subjective symptoms of pregnancy. The patient then began to complain of a steady dull pain in the right iliac fossa, which was at times aggravated by severe lancinating attacks of great violence. On at least two occasions there was a slight bloody discharge, simulating a scant menstruation.
When examined by the writer, the patient presented the usual signs of pregnancy, blueness of the vaginal mucous membrane, engorgement of the breasts, nausea, etc. Upon vaginal examination the uterus was found irregularly enlarged to the size of a grapefruit. The main enlargement was on the right side of the fundus uteri, a large, fairly dense mass, of smooth contour and apparently continuous with the body of the uterus, which was itself hypertrophied and boggy in consistency. A tentative diagnosis of some form of ectopic pregnancy was made, and the patient referred to Dr. B. C. Hirst for his counsel. Dr. Hirst considered the case one of cornual pregnancy and advised expectant treatment, in the hope that the gestation might be converted into an intrauterine one and go normally to term. Treatment by rest and careful avoidance of exertion were accordingly instituted, but after a trial of three weeks, the pain and discomfort became so marked that the patient demanded relief and operation was determined upon.
On June 24, after a thorough preparation for abdominal section, the cervical canal was dilated, under ether anesthesia, and the uterus digitally explored. The organ was enlarged and flaccid, with a large, dense mass occupying the right cornual region and bulging into the cavum uteri. A distinct septum of thick, soft but resistant tissue separated the cornual mass from the general uterine cavity. This septum presented a small central opening, which was readily dilatable with the finger, giving admittance to the fetal sac. There was found a normal four months' fetus with its membranes and placenta intact, the entire ovum lying within the thinned out uterine horn and extending into the uterine extremity of the tube. The myometrium was thinned out to a barely palpable tissue, and gave a tactile impression of marked attenuation. By means of a placental forceps the fetus and placenta were easily removed. The latter organ presented a characteristic appearance, being much flattened and having at one side a long, finger-like prolongation, which had extended through the uterine cornu and had been attached for a considerable distance along the lateral aspect of the tube. There was noted a general development of decidual tissue throughout the entire uterine cavity, which was curetted. The patient made an uneventful recovery and was discharged from the hospital in two weeks.
After rupture, the various varieties of ectopic gestation cannot be separated from a diagnostic standpoint, though, as has been said, the symptoms are usually grave by reason of the rich blood supply and the consequent rapidity of the hemorrhage.
A case of this type was that of a woman of 36 years, who had been married ten years and had never become pregnant. She had noted an amenorrhea for two months preceding her illness, and had suffered from a constant rather severe pain in the left iliac fossa, almost in the midline, but, inasmuch as she was aware of the existence of an old salpingitis, she laid no special stress on the presence of pelvic pain. Suddenly, while on a street car, she was seized with a most excruciating attack of leftsided pain, fainted, and fell into profound collapse. She was admitted to the Frankford Hospital and seen by the writer two hours after the initial attack.
Examination revealed a woman apparently moribund, pulseless, facies lemon yellow in hue, there were present extreme restlessness and anxiety, shallow respiration and a cold clammy skin. The systolic blood pressure was 80, diastolic 55. Hemoglobin was 70, red cells, 3,200,000 and leukocytes 10,000. The abdomen was rigid, but not tender, the patient's condition being almost beyond pain sensation. Vaginal examination was not made, a diagnosis of ruptured ectopic gestation being reached without this procedure.
Following the policy of the writer's clinic, immediate laparotomy was done, venoclysis with a solution of sodium bicarbonate being performed synchronously with the administration of the anesthetic, which was scarcely necessary.
On opening the peritoneum, an immense amount of blood was found in the cavity and the left uterine cornu was seen to have literally exploded, the rupture being a stellate one, several of the lines of laceration extending well into the fundus uteri. The cornu was excised with the tube, the uterus closed, and the abdominal incision united with hasty suture. The patient reacted promptly and made an uneventful convalescence, leaving the hospital on the fourteenth day. No embryo was found nor was any careful search instituted.
Ovarian Pregnancy. — This rare and interesting variety of extrauterine gestation has been considered at length in another part of this book and presents no features which permit of its diagnosis before rupture of the gestation sac, nor are there any distinctive signs after rupture which serve to differentiate it from other forms of ectopic pregnancy.
Diagnosis is only to be reached, after removal of the specimen, by the most thorough and painstaking microscopic examination.
Abdominal Pregnancy. — It has previously been stated that primary abdominal pregnancy, while a theoretical possibility, is not clinically demonstrable, and therefore all cases of this type are to be regarded as secondary to tubal rupture or abortion. The diagnosis of abdominal pregnancy depends first upon the history of an acute attack of illness, which corresponds to the rupture of an ectopic pregnancy.
Should the ovum not be destroyed by the rupture, development may continue and the fetus grow and live to maturity. Such a pregnancy is abnormal in that the fetal movements are far more vigorous and demonstrable than where the uterine wall lies between the fetus and the abdominal parietes. Vague abdominal pain is also a common symptom, this being due in part to the aberrant location of the placenta, whose villi may encroach upon and imbed themselves in any of the abdominal viscera, and in part to the irritative effect of the fetus and its envelopes upon the visceral and parietal peritoneum.
On palpation of the abdomen, the observer is struck with the nearness of the fetus to the examining hand, as though the child lay just under the skin. Usually the fetus is excessively movable, it being possible to displace it from one abdominal quadrant to another.
On vaginal examination, there is always found the comparatively small uterus, which may or may not be displaced as the fetus lies on one or the other side or above the fundus. The cervix is soft, but there is no evidence of Hegar's sign, nor can ballottement be demonstrated.
The fetal extremities are usually to be easily felt through the vaginal vault, a matter of the utmost difficulty in intra-uterine pregnancy. The symptoms of peritoneal irritation are usually well marked, nausea, vomiting, alternating constipation and diarrhea with occasional intestinal hemorrhage, and frequent and painful micturition.
Should the fetus die, it becomes at first macerated, giving rise to a low grade infection with subfebrile temperature and rather profound toxemia, these symptoms later subsiding as the fetus becomes converted into a lithopedion or an adipocere.
Should the fetus live to maturity, there supervenes, at term, what is known as false labor, to be recognized by the increased activity of the fetal movements, painful uterine contraction, and usually some vaginal bleeding. These signs continue for a short time, when,, by reason of fetal death, the movements cease, as do the uterine contractions and the hemorrhages. Mild toxemia follows and the case is eventually converted into one of lithopedion or other final change in the composition of the fetal tissues.
The Diagnosis of Lithopedion or Adipocere. — Terminal changes in the abdominal fetus convert it into what is a pedunculated benign tumor of the abdominal cavity, usually connected with contiguous viscera by fairly dense adhesion formation. Such lesions have been borne without symptoms for many years and give rise to no clinical signs, which might render a diagnosis positive. When symptoms referable to these growths do arise, and the tumor is discovered, it is usually mistaken for a pedunculated fibroid, unless a clear history of an unfruitful pregnancy with false labor be obtained ; or possibly X-Ray examination may disclose the nature of the growth.
The diagnosis of abdominal pregnancy, then, is to be made, during the life of the fetus, by the history of an attack of acute illness, which corresponds to tubal rupture or tubal abortion, by the fact that the uterus is small and not in direct relation to the fetal body, by the generally atypical subsequent course of the pregnancy and by the position of the fetus, which rarely occupies the midline and which may be much more easily palpated when lying free among the intestinal coils than when intra-uterine. The X-Ray may be of service, as brought out by Zurhille, 18 who says it has been claimed by other observers that the differential diagnosis of advanced extra-uterine pregnancy may be confirmed by the position of the fetus, which is asymmetrical as regards the mid plane of the pelvis. In Zurhiile's case the fetal shadow was present in this position, and he suggests than a sound be carefully introduced into the uterus before the exposure is made, so that the relation of the uterine cavity to the shadow of the fetal skeleton may be established. If this is carefully done and a living intra-uterine pregnancy excluded, no harm can result to the patient.
The Diagnosis of Complicated Ectopic Gestation. — Extrauterine pregnancy may be coincident with an intra-uterine gestation. Diagnosis under these circumstances usually presents marked difficulties and is not often made until the marked sign of a massive mtra-peritoneal hemorrhage clarifies the situation.
If the signs of a normal intra-uterine pregnancy, the history, vaginal cyanosis, uterine enlargement, etc., be associated with pain in one or the other iliac fossa, and should any evidence of the occurrence of intraperitoneal hemorrhage supervene, the question of a coincident tubal pregnancy must be considered. In such cases the vaginal bleeding, so characteristic of ectopic pregnancy, is usually absent. There may be found, on examination, a tender mass in one or the other of the vaginal fornices, but such findings are rarely significant, since pyosalpinx, small ovarian cysts and the like, give strikingly similar impressions. Usually, the plan to be followed in such a case is immediate hospitalization of the patient and a careful observance of temperature, blood pressure, and blood changes and other evidence of continuing hemorrhage.
Exploratory laparotomy should be performed as soon as there is a reasonable belief that ectopic gestation may exist. Absolute diagnosis before frank rupture is usually impossible.
The Differential Diagnosis of Ectopic Pregnancy. — Extra-uterine gestation, after partial or complete rupture of the sac, closely simulates a number of intra-abdominal lesions, so closely in many instances as to render differentiation a matter of extreme difficulty.
In this order of their frequency, the conditions most likely to be confounded with extra-uterine pregnancy are :
Intra-uterine pregnancy with threatened abortion,
Hemorrhage from the tube or ovary, not in relation to pregnancy,
Acute salpingitis,
Acute appendicitis,
Ovarian cyst with twisted pedicle,
Rupture of a gastric or duodenal ulcer,
Ureteral or renal colic.
By all odds the most common error in diagnosis is the confusion between ectopic pregnancy and early abortion of a normally implanted ovum. Indeed, in studying case histories, it is surprising to note how large a number of the patients have been subjected to curettage, in the belief that they were suffering from an early intra-uterine abortion.
Furthermore, it is a fairly common occurrence that these women, believing themselves pregnant, seek to terminate the gestation by selfinduced or criminal abortion. In Foskett's series, 12 of the 117 patients thought themselves pregnant, and seven attempted to induce abortion by instrumentation or drug taking, or both.
In Farrar's series of 186 cases, curettage was done before entrance into the hospital, in the belief that intra-uterine abortion existed, in 16 instances, 8.6 per cent. Owing to the close parallelism of the symptoms and physical findings, the differentiation between these two conditions usually presents marked difficulty, and in certain cases a definite diagnosis is almost impossible, except by direct inspection of the tubes by means of an exploratory laparotomy. Close study, however, will clear up the question in the great bulk of the cases, the diagnosis resting upon the following points of difference :
The pain of ectopic pregnancy is usually severe at its onset, changing in a few hours from a lancinating, stabbing sensation to a severe, dull, generalized abdominal distress. In intra-uterine abortion the pain is cramp-like, intermittent, and steadily grows more severe as the uterine contractions increase in frequency and force.
The pain of extra-uterine pregnancy is almost always, at first, localized distinctly in one or the other iliac fossa, while in intra-uterine abortion it is central, over the region occupied by the fundus uteri.
The presence of free blood in the cut de sac of Douglas causes usually very intense pain on defecation, together with considerable rectal tenderness. This symptom is wanting in intra-uterine abortion.
The bleeding varies to some degree in the two conditions. In intrauterine abortion the hemorrhage is generally profuse and the blood is bright red in color.
In ectopic pregnancy, the hemorrhage is apt to be small, and the blood is brownish and has been described as slimy in consistency. Vaginal examination is rarely productive of definite findings, but in general it may be said that the cervix is softer and shows more dilatation when the abortion is intra-uterine than when small rupture or beginning tubal abortion of a tubal pregnancy has taken place.
The discovery of a mass occupying the site of a fallopian tube and exquisitely tender to palpation inclines the diagnosis toward tubal pregnancy, the conviction being strengthened by the elicitation of a boggy, soft, indefinite mass in the cut de sac. The general physical examination reveals certain differences. Temperature is, as a rule, higher in ectopic pregnancy than in abortion, unless the latter be of the induced type, or if the uterus has become infected. The temperature in tubal pregnancy, after small hemorrhage, usually reaches 100 to 101 degrees, while in aseptic intra-uterine abortion, it rarely rises above 99 , unless and until infection supervenes.
Leukocytosis of low degree is common in extra-uterine pregnancy, uncommon in uterine abortion. Hemoglobin change occurs only late, if at all, in both conditions, and is therefore valueless as an aid to diagnosis. The extrusion from the uterus of any portion of an embryo, or fragments of chorion, shown by a miscroscopic examination, render the diagnosis of uterine abortion conclusive.
A blanched appearance of the cervix has been described as a diagnostic sign of rupture in ectopic pregnancy, but such phenomenon is to be expected only after profuse hemorrhage, in which case more definite characteristic symptoms should be present.
A strongly positive Wassermann reaction should incline one toward a diagnosis of uterine abortion, although the fact that a woman is infected with syphilis does not militate in any way against her developing extrauterine pregnancy.
The history presents few points of difference, though the essential facts which point to the patient being apt for pathological conception must be given due weight; one child sterility, previous pelvic infection, conservative gynecological operation, or ectopic pregnancy should predispose the observer to a diagnosis of ectopic gestation.
In the absence of any conclusive evidence, resort is sometimes had to posterior colpotomy, depending on the presence or absence of free blood in the abdominal cavity to determine the diagnosis.
The writer is not at all in accord with this practice, feeling that should a ruptured tubal pregnancy be discovered, operation for the relief of the condition must be performed via the vagina, the worst possible route for the excision of the pregnant tube, and the one most prone to be followed by infection of the pelvic cavity.
A sign of some value is the persistence of uterine bleeding of mild degree after curettage has been practiced. This sign is ordinarily negatived by the fact that but few of these cases are subjected to curettage, and that even among these free rupture with massive intraperitoneal hemorrhage takes place before enough time has elapsed to regard the continuing uterine hemorrhage as significant.
Summing up, thus, the essential features of a differential diagnosis between ectopic pregnancy with beginning rupture and uterine abortion, it may be said that the conditions present striking similarity, but that in uterine abortion the bleeding is more free, the blood bright red, the cervix is more widely dilated, the pain is markedly less, is spasmodic in type, located in the region of the uterus and steadily grows worse as the abortion proceeds, while in ectopic pregnancy the pain, usually localized over one or the other tube, begins suddenly with great violence, not unfrequently attended by nausea and syncope, and steadily grows less in severity, to be replaced within a few hours by a dull, generalized, abdominal ache. Abdominal rigidity is more marked in ectopic pregnancy, the temperature is higher, and moderate leukocytosis is present. In uterine abortion the uterus is apt to be large, and there is no palpable mass in either tubal region, except in those extremely puzzling cases where a subacute or chronic salpingitis is coincident with a uterine abortion.
An interesting and illustrative case, presenting the difficulties sometimes encountered in reaching a correct conclusion in this connection, is one reported by Oastler. 19 "Mrs. S. W., age twenty-eight years, with a negative previous history. Her first labor was normal and regular menstruation was resumed six weeks after weaning. The patient went two weeks beyond term and, thinking she was pregnant, tried to induce an abortion. Bleeding commenced in twenty-four hours and a dull pain in the lower abdomen was noted about forty-eight hours later. The bleeding continued for five days, when the patient came under Dr. Oastler's care. At that time she complained of discomfort in the lower abdomen and stated that, since the effort to induce abortion, she had become constipated, a condition from which she had never before suffered. There was no nausea and no increased frequency of micturition. Examination of the abdomen was negative, and no tenderness could be elicited. Vaginal examination showed the uterus somewhat enlarged and soft, with the cervix normal. Ovaries and tubes were apparently normal, and a diagnosis of incomplete abortion was made. The patient was curetted, but nothing was found, and she continued to flow, but had no pain. Not having bled for five days, the patient was again examined, and the results differed from the preceding one in only a single respect ; a small mass was felt in the right lateral fornix, which was hard, movable, and appeared like an ordinary cystic ovary. With the history of a missed period, negative curettage, sudden onset of constipation, slight general pain, continued bleeding notwithstanding curettage, and a small mass not found on first examination, a diagnosis of incomplete ectopic gestation was made. The operation revealed this condition in the right tube, with a small amount of blood around the fimbriated extremity. There were no adhesions present, and the corpus luteum was not found in the left ovary. The right ovary was very small and apparently atrophied. The interesting feature in this case was the misleading history and physical signs."
Differentiation of Ectopic Gestation from Acute Salpingitis. — A ruptured tubal pregnancy of the sthenic type sometimes so closely simulates acute inflammatory processes in the tube that a correct diagnosis is a matter of the utmost difficulty. The problem is to be attacked first by the securing of an accurate and detailed history, and, as has been repeatedly stated, the matter of the history in cases of suspected extrauterine pregnancy cannot be too greatly stressed. There is usually a known or demonstrable cause for the development of salpingitis, especially if the patient comes under observation during the acute stage of the disease.
A recent abortion, followed by a period of febrile reaction, an attack of appendicitis, recent gonorrhea, easily to be demonstrated by vaginal and cervical smears, will all serve to point to the existence of tubal inflammation. The manner of onset of the attack is a valuable point in differentiation. In salpingitis, the symptoms usually come on gradually, a steadily increasing pelvic pain being usually associated with leukorrhea, the maximum intensity of the pain generally not reached for several days after its being first noted. Whereas in extra-uterine pregnancy the pain begins suddenly and undergoes marked amelioration for a day or more, to be followed by renewed attacks.
Physical examination generally results in a rather confusing combination of signs and symptoms, often so misleading as to make a definite diagnosis almost impossible. Both conditions are associated with febrile reaction, though the fever resulting from pyogenic inflammation is usually higher than that produced by the mere irritative action of blood upon the peritoneal nerve endings. Leukocytosis is present in both conditions, but is generally higher where salpingitis exists than when the lesion is a ruptured pregnant tube. The exception to this is in those cases of extra-uterine pregnancy wherein very large intraperitoneal hemorrhage has taken place, in which instances the white count may reach from 2.5,000 to 30,000. In this type of case, however, the associated clinical evidences of massive hemorrhage are usually so pronounced that determination of the lesion should offer no untoward difficulties. On vaginal examination, there is rarely any special enlargement of the uterus with salpingitis, while only in unusual instances is there any considerable softness of the cervix. Uterine bleeding is uncommon, but may occur. The mass palpated in tubal inflammatory disease is generally much more definitely outlined and circumscribed than in tubal pregnancy, and the tenderness is not nearly so marked on pressure by the examining finger as in the latter condition. In salpingitis, there is commonly present a parametritis, demonstrable by a dense firm consistency of the vaginal vault with fixation of the uterus, such findings being rare in ectopic pregnancy. The concomitant signs of pregnancy are wanting in cases of inflammatory disease, while they are generally present in some degree in the presence of tubal pregnancy.
In summing up the features of variation of salpingitis from ectopic pregnancy, the history is to be regarded as of the first importance, followed by the nature of the onset of the attack, the fact that pulse, temperature and leukocytosis are usually higher in salpingitis, the swollen tube more easily outlined, and the tenderness and pain on examination markedly less.
The Diagnostic Separation of Ruptured Extra-Uterine Pregnancy from Ovarian Cysts, either with or without torsion of the pedicle, is not usually a matter of any great difficulty, but an occasional case will appear in which the sign and symptoms are confusing.
Ordinarily there are not present the characteristic extra-uterine history, the amenorrhea, or irregular bleeding. When torsion of the cyst pedicle takes place, there may be violent pelvic pain, with syncope and collapse. Slight elevation of temperature and a moderate leukocytosis may shortly follow the accident. On vaginal examination, the ovarian cyst is generally much larger than an ectopic pregnancy, the uterus is not enlarged, nor is the cervix softened. Small retention cysts of the ovary, with their attendant delayed menstruation and the dull pelvic pain which sometimes goes with them, closely simulate extra-uterine pregnancy, and, indeed, occasionally such cysts rupture during the course of a vaginal examination, this accident making the suspicion of ectopic pregnancy more pronounced. Many cases of this nature have been promptly operated upon, in the belief that a ruptured tubal gestation was being dealt with, only to discover a small and apparently insignificant follicular ovarian cyst. The history is the only means of differentiation in these instances, which are among the most difficult of correct interpretation.
The differentiation of extra-uterine pregnancy from retroversion of the normally pregnant uterus is sometimes a matter of the greatest uncertainty. Both conditions are attended by a train of signs and symptoms strikingly similar. In both there is bleeding from the vagina, pelvic pain, perhaps retention of urine; the concomitant signs of pregnancy are present in both, as is amenorrhea, a softening of the cervix, and a boggy, tender mass present in the cul de sac.
In a retroverted gravid uterus, however, the cervix is tilted upward and forward, pointing even sometimes toward the symphysis, whereas, if the uterus be pushed forward by a hematosalpinx or by a collection of blood in the cul de sac, the cervix points backward and toward the perineum.
The pain of a retroverted, congested pregnant tube is apt to be dull in character, constant, and located over the body of the uterus radiating to the back. The pain of ectopic gestation has been described as short and spasmodic in character, followed by an increasing general abdominal ache as the free intraperitoneal blood sets up peritoneal irritation. If the uterus be sharply retroflexed, the angle made by the junction of cervix with fundus may be clearly felt, but the abdominal hand feels no fundus, this portion of the organ having disappeared in the hollow of the sacrum. The diagnosis of a combination of retroversion of the uterus plus ectopic pregnancy, is extraordinarily difficult and is to be reached only after a most painstaking survey of the history.
When, following rupture of a pregnant tube with secondary abdominal development of the fetus, the uterus is crowded down below the gestation sac, the diagnosis offers great difficulty. De Lee 20 reports such a case, which was at first diagnosed as retroversion of the pregnant uterus
F IG . 57.— Uterus Crowded Down Below Gestation Sac. From De Lee.
Fig. 58. — Uterus Pushed Down by Gestation Sac. From De Lee.
with retention of the urine, but when the abdominal tumor did not subside on catheterization and the fetus was felt above the left Poupart's ligament, the correct condition was discovered, with operation and recovery. (Figs. 57 and 58.)
Fig. 59.— Section Through Attachment of Villi to Tube Wall. From Mall.
Differentiation of ectopic pregnancy from ruptured gastric ulcer, renal colic, cholecystitis, etc., should be made after a consideration of the history of the case, the absence of uterine bleeding, and the location and character of the pain, and will not be discussed in detail here.
In closing the question of diagnosis in extra-uterine pregnancy, attention is again called to the importance of most careful study of the case
Fig. 6o. — Section through Veins in Tube Wall. From Mall.
Fig. 6i. — Section Through Vacuolated Syncytium. From Mall.
Fig. 62.— Syncytium Covering a Typical Villus. From Mall.
history, as the paramount factor in a correct interpretation of the symptoms and signs of this lesion.
The Histological Diagnosis of Extra-Uterine Pregnancy. — It frequently becomes necessary to ascertain whether hemorrhage from a fallopian tube or an ovary is a result of the rupture of a gestation sac, or is due to other causes.
Microscopic examination should always determine the diagnosis, but un- Fig. 63.— Villus Undergoing Fibrous fortunately for the purposes of detailed Degeneration. From Mall.
study, most specimens of tubal or ovarian pregnancy are so damaged by the rupture of their walls and the subsequent operative manipulation that the tissues are distorted in their relations and so greatly altered by traumatism as to make orderly study difficult.
Fig. 64. — Section Through Ovum Adjoining Tube Wall. From Mall.
A positive histologic diagnosis of extra-uterine pregnancy is only to be made by finding chorionic villi or syncytial cells in the suspected tissue.
Fig. 65. — Tip of a Fibrous Villus. From Mall.
So-called decidual cells, when found, do not in themselves constitute the evidence for an affirmative diagnosis, as they may be present in the tube walls during intra-uterine pregnancy, and, indeed, when no pregnancy whatever exists.
The microscopic picture of a pregnant tube is well shown in Figs. 59 to' 69.
The chorionic villi frequently penetrate the muscular coat and may be seen terminating just under the serosa.
Syncytial cells are abundant and there is always noted an attempt at reaction to the invading blastodermic cells on the part of the tubal tissues, as evidenced by round cell infiltrations and the presence of fibrinous exudate.
Fig. 66. — Section Through a lus. From Mall.
Fig. 67. — Section of Vacuolated Syncytium Filled with Leukocytes. From Mall.
When the ovum has been dead for some time, areas of organized hemorrhage are the principal constituents of the tube. There are always
to be recognized, however, the characteristic chorionic villi, though perhaps in an advanced stage of degeneration.
The finding of an embryo is not a necessary criterion of the existence of ectopic pregnancy, since the fruit of the gestation is not uncommonly lost among coils of intestine, following the rupture of the tube or a tubal abortion; or the embryo, if very young, may have undergone absorption.
Evidence of villus formation is, however, an absolute necessity, if the diagnosis is to be substantiated.
The criteria necessary for the establishment of a diagnosis of ovarian pregnancy have already been enunciated.
-Extreme Degeneration of the Syncytium. From Mall.
Fig. 69. — Group of Villus Cells Growing into Mesenchyme. From Mall.
Histologically, ovarian pregnancy will always present syncytium, even though distinct villi be absent, although in most of the recorded cases, placentation was easily demonstrable.
Literature
i. Hunner, G. L. Ectopic Gestation from the Standpoint of the General Practitioner. Am. Jr. Obst. 19 10. 62:409.
2. Boldt, H. J. The Diagnosis of Extra-Uterine Pregnancy. Arch.
Diag. Jan., 1908. p. 32.
3. Farrar, L. K. P. Am. Jr. Obst. 1919. 79:733.
4. Foskett, E. A Study of 117 Cases of Ectopic Gestation. Am.
Jr. Obst. 1913. 67:27.
5. Bandler, S. W. Medical Gynecology. Philadelphia, 1908. p. 645.
6. Mackenzie, S. N. The Clinical Aspects of Extra-Uterine Gesta tion. Jr. Obst. Gyn. Brit. Emp. 191 1. 20:277.
7. Taylor, H. C. Med. Surg. Rep. Roosev. Hosp. 1915. p. 147.
8. Rongy, A. J. The Treatment of Ectopic Gestation, Based on a
Study of 100 Cases. Am. Jr. Obst. 1918. 77:86.
9. Taylor, J. W. Extra-Uterine Pregnancy, p. 102.
10. Oastler, F. R. Ectopic Pregnancy. Surg. Gyn. Obst. 191 7.
24 :224.
11. Polar, J. O. Observations in 227 Cases of Ectopic Pregnancy.
Am. Jr. Obst. 19 15. 71:946.
12. Frank, R. T. An Analysis of Eighty Consecutive Cases of Ectopic
Gestation. Am. Jr. Obst. 1909. 59:211.
13. Wynne, H. M. N. Bull. J. Hopk. Hosp. 1919. 30:15.
14. Cullen, T. S. Tr. Am. Gyn. Soc. 1918.
15. Schottmuller. Munch, med. Woch. Feb. 3, 1914.
16. Kustner. Ektopik Schwangerschaft. p. 118.
17. Schumann, E. A. Am. Jr. Obst. 1912. 65.
18. Zurhille. Zentbl. f. Gyn. Sept. 27, 1912.
19. Oastler, F. R. Am. Jr. Obst. 1914. 69:127.
20. De Lee, J. B. Obstetrics. Philadelphia, 191 5. p. 402.
Chapter VII. Treatment
Treatment Before Rupture Has Occurred— The Treatment of the Affected Tube — The Treatment of the Remaining Tube — The Management of Abdominal Lesions, Not Connected with the Ectopic Pregnancy — The Closure of the Incision— The Treatment of Advanced Extra-Uterine Pregnancy — The Treatment of Advanced Ectopic Pregnancy When the Fetus Is Known to Be Dead— The Treatment of Infected and Suppurative Ectopic Pregnancy — The Treatment of Hematocele — Mortality and Prognosis.
The greater portion of this book consists of the accumulated data compiled by many investigators and students in the field of extra-uterine pregnancy. This is necessary, since no one operator can hope to se or 52.88 per cent, perished from hemorrhage following rupture. Of these the period during which life was prolonged is mentioned in 113. Of the whole 113, 81 had died at the end of twenty-four hours after rupture was supposed to have occurred, while at the end of forty-eight hours only 15 or a little more than 13 per cent of the whole number were alive. Truly a curious combination, these accurate statistics, and the assertion of Robb that hemorrhage is not per se a cause of death in ruptured extrauterine pregnancy!
The expectant plan of treatment was soon abandoned, however, but the effect produced by it has not yet entirely disappeared, many .gynecologists of wide experience preferring not to operate in the so-called "tragic stage," but to await a reaction from the initial shock and a recovery in blood pressure and a lowering of pulse rate, before resorting to laparotomy. With such viewpoint the author is in no way in accord.
It is not within the ken of human minds to foretell the result of an internal hemorrhage, and to sit quietly by, counting the pulse and estimating the blood pressure changes, hour by weary hour, while the life blood drips slowly but surely from the severed ends of the torn vessels, hidden from sight in the abdominal cavity, to put off operative interference until the patient, exsanguinated, is at last moribund, to wait in vain for the reaction which does not take place, is a procedure repugnant alike to surgical experience and surgical courage.
The writer holds firmly with that master of the subject, Mr. Lawson Tait, when he says, "For surgical hemorrhage, cut down and tie the bleeding point; if a big branch of the femoral artery were bleeding, my colleagues, who deal in such cases, would cut down and tie it. Why should Poupart's ligament be a line of demarcation, within which this surgical writ will not run? Why should my friend, Mr. Bryant, be allowed to do to the external iliac artery what I am prohibited from doing to the internal division?" Why, indeed!
There is a deplorable laxity with regard to the terms used in describing the effects of the rupture of a gravid tube, and, as pointed out by John B. Deaver, one of the worst of these practices has been the use of the word shock, to define the symptom complex following such rupture. The picture, after the first few moments, is not at all one of shock, but corresponds in every detail to that of severe and continuing intraperitoneal hemorrhage.
Furthermore, it is the opinion of all operators of large experience that the condition of the patient, pulse rate, temperature, respiration, hemoglobin count, etc., bears a direct relation to the amount of blood lost. The greater the hemorrhage, the worse the patient, and vice versa. It follows, then, that the use of such "vicious, catch phrases" as "adding shock to shock" is not only misleading, but affords in no sense true statements, since the real fact is that, by immediate operation, one adds shock (or rather the possibility of shock) to preexisting hemorrhage, a result always to be anticipated when dealing with any surgical hemorrhage wherever situated.
The plan of awaiting reaction from the primary depression of hemorrhage in patients in extremis when admitted to hospital, has something in its favor. It is indubitably true that many, indeed, a majority of such patients do react, and may be operated upon with comparative safety twenty-four or forty-eight hours after reaction. It is equally true, however, that no man can foretell whether reaction will take place, or whether the patient will slip momentarily further and further beyond surgical aid, until the opportunity for interference has passed and death ends the scene, without any attempt having been made to save the life of the woman.
It is argued that one should closely watch the two indices of the patient's condition— pulse rate and blood pressure — and if she is seen to be losing ground, operate immediately; if she be gaining and reaction is beginning, await a more opportune time.
Theoretically this argument is good, but practically speaking, if these moribund women are watched until they grow worse, they will have perished before the bleeding vessel can be exposed and ligatured. The fact is that, given a woman exsanguinated from internal hemorrhage, with imperceptible pulse, rapid shallow respiration, cold leaking skin and very low blood pressure, her chances for recovery are far greater by offering her a combination of simultaneous abdominal section and bold stimulation than by any other plan of treatment yet devised.
The attitude of the writer in this matter, then, is that he would operate upon every woman suffering from a ruptured ectopic gestation as soon as the conditions for rapid and aseptic laparotomy are available, without regard to the condition of the patient. If any evidences of life are manifest, the patient is given the opportunity for recovery that is offered by the control of the hemorrhage and free stimulation.
While it is true that the resources of surgery are rarely successful when practiced on the dying, yet of all surgical conditions, ruptured ectopic pregnancy is the one wherein even patients operated upon almost in articulo mortis recover with the most surprising rapidity.
The treatment followed in the author's service is as follows : Immediately upon a diagnosis of ruptured ectopic pregnancy being made, the patient is given a subcutaneous injection of morphiae sulph., grs. %. The head of the bed is lowered and bodily warmth maintained by the use of external heat. So soon as the operating room can be made ready and the staff assembled, laparotomy is performed.
Before beginning an operation of this character, the steps to be followed should be clearly outlined in the mind of the surgeon, and his management of the varying conditions which may be found should be definitely determined, in order that no valuable time may be lost in arriving at a decision, after the abdomen is opened, which should have been reached before the patient entered the operating room.
There are always present in these cases a definite series of conditions whose management must be decided :
The management of free blood and clots in the abdominal cavity.
The treatment of the affected tube.
The treatment of the remaining tube.
The management of abdominal lesions not connected with the ectopic pregnancy. The closure of the incision.
Free blood and clots within the abdominal cavity are to be removed only in so far as their presence obscures the field of operation.
When the diseased tube has been brought into view and secured for excision, no further effort is made to remove blood and clots. Furthermore, it is important that the tube be exposed as soon as possible, else much valuable time may be wasted in sponging away blood which has already been lost to the patient, while the severed vessel is still bleeding unchecked.
It is the custom of the writer to scoop out with the hands the masses of clot that usually present as soon as the peritoneum is incised, and to make no further attempt at toilet of the peritoneal cavity until the operation is completed, when, depending upon the condition of the patient, either the residue of blood is left behind, or a more or less thorough sponging of the abdominal cavity is practiced.
The Treatment of the Affected Tube
In the treatment of the ruptured tube, one of three plans may be followed. The tube may be amputated just proximal to the gestation sac, leaving the stump as a possible factor in future uterine pregnancy. It may be split at the point of rupture, and the remains of the sac removed, after which the incision in the tube wall may be sutured or left open at the option of the operator. The tube may be excised down to the uterine cornu.
Inasmuch as a damaged tube offers great opportunity for a repetition of the accident of ectopic gestation, as shown by the cases of Coe, Taylor, Gottschalk, Stahl and others, and since a tube so' traumatized presents but a faint possibility of furnishing an unobstructed passageway for the ovum in the future, the first two plans of treatment are not advised nor practiced by the writer, who holds with Cragin x that the frequency of this repeated accident has been great enough to convince one of the danger of leaving behind a tube which has once been the site of an ectopic gestation. As regards the question of whether a tube, once the seat of a tubal rupture or abortion, will ever allow a normal intra-uterine pregnancy, the writer can only say that the proof of this result would require the previous removal or closure of the opposite tube, and he has been unable to find in the literature any record of a case of normal pregnancy in which the only patent fallopian tube possessed by the woman had previously been the site of an ectopic gestation. He would, therefore, state the proposition that a tube once the site of an ectopic gestation should be removed, as likely to be a source of danger if left behind, and not likely to be of value in future child bearing.
The affected tube, then, is to be excised down to the uterine cornua.
The Treatment of the Remaining Tube. — Authorities differ greatly in their views upon this phase of the question, some advocating the routine removal of both tubes, by reason of the likelihood of a later ectopic pregnancy developing in the tube left behind, while others would never remove the unaffected side. The rational view seems to rest somewhere between these two extremes.
The value of the unaffected tube lies in its offering possibilities for subsequent child bearing on the part of the patient; the danger of leaving it behind rests upon the probability of its becoming the seat of a future tubal pregnancy, since the causes underlying this condition are frequently identical in both tubes.
This question has been fully discussed in the section of the book devoted to Recurrent Extra-uterine Pregnancy, but a brief review of the facts is here set down, since the accumulated experience of gynecologists forms the basis of a rational treatment.
In a grouped study of the histories of 280 patients, the victims of ectopic pregnancy and in whom there existed the possibility of future pregnancy of any variety, 35, or 12.5 per cent, suffered from repeated ectopic gestations, while 134 intra-uterine pregnancies occurred, or 47.8 per cent, a ratio of extra- to intra-uterine pregnancy of about 1 14.
It appears then that about one woman in eight, who has had one extra-uterine pregnancy may expect another, whereas one half the total number have the prospect of future normal childbirth.
These figures are so overwhelmingly in favor of the retention of the unaffected tube, that there seems no valid argument left for its removal, provided, of course, that the organ shows no evidence of gross disease upon inspection.
It is the practice of the author always to leave one tube, unless its retention would seem to invite further pelvic pathology, to the detriment of the future health of the patient.
The Management of Abdominal Lesions, Not Connected with the Ectopic Pregnancy. — In approaching this phase of the subject, it should be remembered that the rupture or abortion of a tubal gestation sac is a lesion distinctly traumatic in its nature, that the patient is suffering from an acute injury, and that the surgical axiom that a minimum of operative trauma insures a maximum of success in treatment applies to the management of ruptured ectopic gestation as well as to that of any other accident involving hemorrhage.
Therefore a general rule may be advanced that no more surgery should be practiced upon a victim of such rupture than is absolutely necessary to insure primary postoperative recovery.
Practically applied, the rule means that, when dealing with a patient in serious condition from hemorrhage plus shock, the hemorrhage is to be controlled and the tube removed in the shortest time possible, and the operation terminated without regard to any other pathological condition observed in the abdomen, save one only and that one of very rare occurrence, namely, the presence of a pregnancy in the opposite tube which may be expected to rupture at any time. In this event, it obviously becomes necessary to excise both tubes.
The practice of systematic abdominal exploration, the removal of the appendix, uterine suspension and the like during the course of an operation for ruptured ectopic pregnancy, when there has been a considerable blood loss and the natural resistance of the patient greatly impaired thereby, is to be unqualifiedly condemned. Where there has been but little bleeding, as in certain cases of tubal abortion, and when the patient iz not in serious condition, the procedure may be modified, and attention to the coexistent lesions is not only justifiable but proper. In a general sense, however, the author is inclined to minimize intra-abdominal manipulation, in cases of ectopic gestation, to the lowest possible degree, and it is his firm belief that every unnecessary minute added to the operation time imperils the recovery of the patient in direct ratio. The shorter and less traumatic the operation, the less eventful the convalescence.
The Closure of the Incision
The abdominal incision in the type of case under discussion should uniformly be closed without drainage, it being presumed that no active infective process is present within the abdomen. Drainage has no place here, and if practiced, only tends to an infection of a sterile substance, which, however, is an excellent culture medium, the clot and free blood remaining within the peritoneal cavity.
Technic
The technic of laparotomy for ruptured ectopic pregnancy requires but brief description. Ether is the anesthetic of choice, by reason of its stimulant properties, and the anesthesia is begun with the patient in a moderate Trendelenburg position. This practice keeps the head lowered, a desideratum in the case of severe blood loss, and seems to greatly stabilize the respiratory excursion, obviating the straining and excessive contraction of the abdominal muscles sometimes noted when a patient already partially anesthetized is placed in the Trendelenburg position.
Immediately after the stage of excitement has passed, the arm of the patient opposite the side on which the operator is to stand is exposed, the cubital space prepared, and the median cephalic or basilic vein opened and the intravenous injection of either normal saline solution or, better still, a six per cent solution of gelatin in water, is begun. The amount introduced should be not less than one quart and not more than three pints, in case of severe hemorrhage. The intravenous replacement of fluid may continue until the required amount has been introduced, the apparatus being moved with the patient from the operating room to her bed, if necessary.
At the same time, if the pulse be rapid and small, a hypodermic injection of strych. sulph. gr. 1/20 and atrop. sulph. gr. 1/50 is exhibited.
While this is going on, the abdomen is being prepared according to the routine of the individual surgeon, either by iodin, alcohol and ether, or a combination of phenol, acetone and alcohol, a modification of McDonald's solution, which is used exclusively in the author's service.*
This mixture is used to saturate wash cloths, with which the entire operative field is vigorously scrubbed for three minutes, the solution being poured on from a wash bottle.
The abdomen is then appropriately draped and a median incision is made, generous in size, so that no time may be lost in gaining access to the pelvic viscera. The diagnosis is usually confirmed by the purplish hue of the peritoneum, caused by the presence of blood in the abdominal cavity. When the peritoneum is incised, blood is not infrequently ejected with considerable force, owing to the increase in intra-abdominal pressure brought about by the presence of a considerable volume of blood.
The formula used in Frankford Hospital consists of
- Phenoco 2 parts
- Acetone 40 parts
- Alcohol (95 per cent) to make 100 parts
The presenting clots are scooped out with the hands, the intestines isolated by means of gauze or crepe de chine pads if necessary, which is rarely the case, and the uterus grasped and brought into view. The affected tube is grasped with forceps and, if a bleeding point is detected, the hemorrhage is controlled by a clamp on the uterine end of the tube, while another grasps the mesosalpinx.
Fig. 70. — Blood Supply of Fallopian Tube. From Norris.
The manner of excision of the tube varies with the condition of the patient. If the case be a desperate one, the mesosalpinx is simply ligated en masse as a pedicle and the tube cut off. Usually, however, a greater refinement of technic is permissible, and the blood supply of the tube is controlled by three ligatures, preferably of No. 1 chromicized catgut, which are placed along the upper border of the broad ligament, one to secure the outer branch of the artery to the tube, just internal to the fimbriated extremity, one about the middle of the tube, and one well into the uterine cornu. The tube is then cut free from the mesosalpinx and its uterine end excised by a wedge shaped incision in the uterine cornu. The open upper border of the broad ligament is now approximated with a continuous suture of No. O chromic gut, and the operation is completed. The blood supply of the tube is shown by Fig. 70, taken from Norris, and the operative technic is well illustrated by Fig. 71. The abdominal incision is closed by layer suture.
The postoperative treatment of cases of ruptured ectopic pregnancy, in which there has been severe hemorrhage, is conducted with a view to the correction of three factors of danger to the patient; that is, shock, acute anemia, and cardiac dilatation and failure, resulting from a combination of the first two factors.
Shock is controlled by the generous use of external heat, electric heating pads being excellently adapted for the purpose, the retention of all blood possible in the great vessels of the head and trunk by means of the low head position of the bed and firm bandaging of the extremities.
Fig. 71. — The Details of Salpingectomy for the Removal of a Tubal Pregnancy. Note the location of the ligatures which control the tubal blood supply.
The acute anemia is best overcome by direct blood transfusion, whenever this is possible, at least 500 c.cm. of blood and more, if circumstances permit, being transfused. The blood should be typed before transfusion is attempted, and the method of choice is that of the simple large glass syringe, although the Kempton-Brown tubes may be utilized.
In the opinion of the writer, blood transfusion is by all odds the most important measure in the treatment of a desperate case, its importance bearing a direct ratio to the time elapsing between the onset of the hemorrhage and the replacement of the blood. For this reason, the ideal time for transfusion is during the course of the operative procedure and, when the requisite clinic and assistants are available, this is the method of choice. Transfusion may be practiced with benefit at any time during the convalescence, but after the first forty-eight hours it is not usually required. Failing the requisites for blood transfusion, saline or gelatin solution is to be introduced by vein as described. The surgeon should bear in mind that too much fluid per vein is almost as productive of harm as too little, since inundation of the vascular system readily leads to acute cardiac dilatation and edema of the lungs, with probably fatal results. As a general rule of practice, not less than one quart nor more than three pints of saline solution should be added to the circulation at one time.
Inasmuch as the fluid is absorbed by the tissues in a short time, it is proper to supplement this by the use of saline solution by the bowel, the institution to be begun about four hours after the completion of the operation and continued by the drop method so long as absorption takes place.
So soon as the patient has reacted from the operation and anesthetic, anemia is treated by the systematic administration of iron and arsenic in the combination favored by the individual operator. A capsule of Blaud's mass gr. v with arsenious acid gr. 1/24, exhibited three times daily, is the routine practiced by the writer.
Cardiac failure is anticipated and controlled in these cases by the free use of cardiovascular stimulants, strychnia, digitalis, and atropin by hypodermic injection being needful to some degree in most cases. Abundant feeding, and the stimulating effect of fresh air and sunshine are important factors in the treatment, most of the writer's cases being moved to the hospital sun porch on the day following operation. Pain and restlessness are controlled by the free use of morphin. Laxatives play no. part in the postoperative routine, the bowels being evacuated by means of daily enemata.
Such, in general, is the outline of the treatment of these desperate cases. The steps of the procedure vary, naturally, with the gravity of the case. When hemorrhage is slight and no constitutional signs of blood loss are apparent, transfusion and venoclysis are usually unnecessary, nor is postoperative stimulation required in so drastic a form.
When the pregnancy is interstitial, the hemorrhage has usually been profuse, and the trauma inflicted upon the uterine horn is excessive. In some instances, it is possible to excise and close the uterine cornu, but where this offers difficulty and appears to be a time consuming procedure, a quick supravaginal hysterectomy is the operation of choice. In this event, the unaffected tube and ovary are to be left in situ in most cases.
Ovarian pregnancy is treated by ovariotomy, the tube being also removed in most cases. The preoperative and postoperative treatment is essentially that of tubal rupture.
The question naturally arises, whether the plan of immediate radical treatment is absolutely requisite in all cases of extra-uterine pregnancy, or whether perhaps there are not some situations in which a policy of watchful waiting is not more conducive to the well being of the patient.
It has been stated previously that there are undoubtedly a number of cases of ruptured tubal pregnancy, in which the true state of affairs is never recognized and from which the women recover without any surgical aid.
There is another and considerable group of cases, in which rupture between the folds of the broad ligament or complete tubal abortion has taken place, the hemorrhage ceasing and the ultimate result being either a broad ligament hematoma or a pelvic hematocele, either condition not only presenting no indication for immediate operation, but, indeed, productive of a somewhat better end result, if the surgical intervention be delayed until the clot has become completely organized.
The difficulty in these cases centers about the diagnosis. If one is willing to assume full responsibility for the termination, and can be assured that hemorrhage has ceased and will not recur, a waiting plan may be adopted. The writer feels that, so far as his own experience is concerned, he can never be certain as to these essential facts, and in the absence of that certainty he feels it incumbent upon him, in the best interests of the patient, to ascertain, by direct inspection, the true state of affairs and to secure torn blood vessels against any possibility of recurring hemorrhage.
The Treatment of Advanced Extra-Uterine Pregnancy. — By advanced extra-uterine pregnancy is meant those cases not seen until after the fifth month, the fetus being alive or having perished, as may be. Here the management of the placenta becomes the factor of first importance, together with the fact that a possible infant life is to be considered, as well as that of the mother.
The placenta may occupy any position within the abdominal cavity, although it is most commonly found firmly attached to the posterior fold of the broad ligament and the floor and lateral walls of the pelvis, the villi dipping deep into the pelvic vessels. In other instances, however, the placenta may be found attached to the omentum, the intestines or indeed to any of the intraperitoneal viscera. In such case, where the fetus is alive and the placental circulation active, the removal of this organ may be attended by absolutely uncontrollable hemorrhage.
No definite technic for the performance of an operation for advanced ectopic pregnancy can be formulated, since each case is a law unto itself, but certain general directions will be found valuable.
The incision is preferably to be made along the outer border of the rectus muscle overlying the gestation sac, since so many of these placentas are found under and between the folds of the broad ligament that the removal of the fetus and placenta may be accomplished without entering the peritoneal cavity, a matter greatly to be desired, especially if the placenta cannot be removed at the time of operation.
Having reached the sac, it should be incised, the child extracted and the cord ligated as in cesarean section. The sac should then be examined in great detail, in order to ascertain whether it be feasible to attempt ligation of its blood supply and excision, or whether the attachment to great vessels or to vascular viscera is so intimate that attempt at enucleation will result in disaster.
In the former alternative, careful ligation of the vessels supplying the placenta should be performed, before attempts at its removal are instituted. The ligations accomplished, the placenta may be manually pulled off its attachment, bleeding being controlled by ligatures and pressure by gauze wrung out in hot saline solution, and the wound closed without drainage.
Should the location of the placenta be such that control of its blood supply seems impracticable, there are two methods for its management. First, the time honored plan of marsupialization, stitching the edges of the gestation sac to the abdominal wound and lightly packing the cavity with gauze. The gauze packing is changed at forty-eight hour intervals and the separation of the placenta aided by gentle traction. In the course of a few weeks the tissue has sloughed out and there remains a sinus of varying size, which usually closes spontaneously, although a second operation for the repair of the abdominal wall may be required.
The second plan, recently advocated by Beck, 2 is to simply leave the placenta in situ and close the abdominal wound without drainage, depending upon the absorption power of the peritoneum for the subsequent removal of the lesions. To test this principle, Beck placed three fifths of a 500 grain placenta, removed by cesarean section, in the abdomen of a dog. The animal promptly recovered. Two months later its abdomen was reopened and no trace of the placenta could be found. In Beck's statistics, there were twelve cases in which this procedure was adopted, from 1890 to 1919, of which four died, a mortality of 33.3 per cent during the same period, marsupialization was practiced in 52 women, 22 of whom died, or 38.7 per cent.
While these figures are greatly in favor of leaving the placenta for absorption, they are subject to the usual destructive criticism, since it is not stated in how large a proportion of the patient's fruitless attempts at enucleation had been made before it was decided to leave the placenta, which had been found impossible of removal, with the consequent infection and hemorrhage.
While he has never left a placenta for absorption, and is therefore not qualified to criticize this treatment, the writer confesses to a decided repugnance to leaving so large a mass of foreign tissue within the undrained peritoneal cavity.
In a consideration of the treatment of advanced ectopic pregnancy from the standpoint of the child, two questions present themselves : first, whether the fetus is apt to have suffered some arrest of development which renders. its postnatal life doubtful or impossible; second, whether or not the maternal risk is greatly increased by permitting the pregnancy to continue until term or thereabouts.
Briefly put, the question is, what is the best time to interfere in the interests of the child, what the best in the interests of the mother, and is there a time during the gestation when these divergent interests may both be protected. Beck 2 has approached this problem by carefully collecting case reports from the literature, as well as from the replies to a questionnaire sent to over 200 obstetricians. From his study of these cases, Beck concludes that:
- The best time to operate is during the sixth or the seventh month.
- The added risk in waiting for a well developed child is slight up to the thirty-ninth week.
- The danger of a catastrophe is sufficiently great in the last two weeks to warrant interference before this period is reached.
In the interests of the child it is found that the best time to operate is the thirty-eighth week, more infants having survived at this period than at any other. This may be explained to mean that, as interference is practiced before term, the child, as well as the mother, is spared the danger of spurious labor, and further, that the fetus is subjected to greatly increased pressure during the last two weeks of pregnancy, by reason of the diminution in the amount of the liquor amnii at this time.
Since the risk in waiting for the thirty-eighth week is slight for the mother, and since this is the time of election for the child, it follows that the thirty-eighth week of pregnancy is the best period for surgical intervention from the standpoint of both mother and child.
That these abdominal children are worth saving is beyond a doubt, Cragin finding two normal living infants in his four cases, while Horsley's statistics, previously quoted, amply confirm this.
The Treatment of Advanced Ectopic Pregnancy When the Fetus is Known to Be Dead
Should the fetus have been dead for a considerable time, immediate removal of the placenta is usually possible, its vascularity having markedly decreased and a partial separation of the villi from their site of implantation having taken place. If the fetus is known to have been dead but a short time, it is advisable to defer operation until some obliteration of the maternal blood spaces about the villi has occurred, since the enucleation of the placenta is greatly facilitated thereby. During the month or six weeks of waiting for the separation to take place, the patient should be under constant observation in a hospital, in order that immediate operation may be performed in the event of any infection of the gestation sac supervening, as evinced by an elevation of temperature and pulse rate and an increasing leukocytosis.
The Treatment of Infected and Suppurative Ectopic Pregnancy
Where infection is present, the ideal method of treatment is vaginal incision, the extraction of such of the products of gestation as are within reach, and the establishment and maintenance of free drainage. Suppuration is the only condition arising in connection with extra-uterine pregnancy, in which the vaginal route of operation is indicated, in the opinion of the writer, who feels that the time involved and the trauma inflicted are far less and the completeness of the operation is best attained by abdominal attack in all cases, save those complicated by pus formation.
The technic of vaginal incision is so well understood that any detailed description would be out of place here. Suffice it to say that the posterior vaginal fornix is the point of attack, and the incision into the abscess cavity is to be of sufficient size to admit of thorough digital exploration, in order to extract any large portions of the fetal body, if such be present.
Drainage is best maintained by the suturing into the cavity of a large sized rubber drainage tube, through which the abscess cavity may be flushed with Carrel-Dakin solution, or other antiseptic agent, at the option of the operator.
The Treatment of Hematocele. — The same general views obtain in the management of old organized blood in the pelvis as are held with regard to the treatment of advanced ectopic pregnancy. So long as no infection is present, the abdominal route is advised, since intestinal adhesions, usually so marked in other cases, can best be dealt with under the eye, the mass can be much more thoroughly enucleated, and the danger of traumatism to adjacent structures is reduced to a minimum. When complicated by suppuration, however, hematocele is best treated by simple vaginal incision and drainage, as described above.
The first American operation for the relief of advanced ectopic pregnancy by the vaginal route was performed by Dr. John King 3 of Edisto Island, S. C, in 18 16, when a full term child was removed after cutting through the posterior vaginal wall.
Mortality and Prognosis
The hope for recovery of a woman afflicted with ectopic pregnancy is yearly growing greater, and the gynecologist who reviews the history of this remarkable lesion must complete his surveys with intense pride and gratification that the labors of his predecessors in this field have wrought such vast improvement in results. Consider Parry's statistics of 1876, when among 500 cases 386 perished of this lesion.
In 1918 in Philadelphia, there were 169 such patients admitted to hospitals, of whom thirteen died, or y.j per cent. These figures contemplate all cases — those admitted to hospital when already moribund, as well as the more favorable types.
In Farrar's series of 309 cases, there were three deaths, or .97 per cent. In P. F. Williams' series of 147 cases, death occurred four times, a mortality of 2.J per cent. Of Oastler's 106 cases, seven died, or 6.5 per cent. The writer has studied 307 cases with eight deaths, or 2.6 per cent.
On the whole, then, it may be concluded that the average mortality in a well conducted clinic will be 4 per cent or under, and it is the firm belief of the writer that if every woman brought to a hospital with a correct diagnosis of ruptured ectopic pregnancy be subjected to immediate operation, without regard to her condition, the mortality will be still further reduced. Two of the writer's eight deaths were a direct result of his lack of courage in operating upon moribund women, and since this time, now four years ago, not one case has perished.
It has been said in high places that there is no excuse for the existence of gynecology as a surgical specialty, but to him who has read this book, the question is left, as to whether or not a branch of medicine which has within a half century reduced the mortality of so dreadful an accident as the rupture of a gravid tube, from 80 per cent to 4 per cent, has not justified its existence in full.
Literature
1. Cragin, E. B. The Treatment of Ectopic Gestation. Surg. Gyn. Obst. 1912. 14:276.
2. Beck, A. C. Treatment of Extra-Uterine Pregnancy After, the Fifth Month. Jr. Am. Med. A. 1919. 73 1962.
3. King, J. Am. Analysis of the Subject of Extra-Uterine Gestation. Munich, 18 18. p. 176. Quoted by J. W. Williams.
| Historic Disclaimer - information about historic embryology pages |
|---|
| Pages where the terms "Historic" (textbooks, papers, people, recommendations) appear on this site, and sections within pages where this disclaimer appears, indicate that the content and scientific understanding are specific to the time of publication. This means that while some scientific descriptions are still accurate, the terminology and interpretation of the developmental mechanisms reflect the understanding at the time of original publication and those of the preceding periods, these terms, interpretations and recommendations may not reflect our current scientific understanding. (More? Embryology History | Historic Embryology Papers) |
Figures
Cite this page: Hill, M.A. (2024, April 28) Embryology Book - Extra-uterine pregnancy - 1921. Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/Book_-_Extra-uterine_pregnancy_-_1921
- © Dr Mark Hill 2024, UNSW Embryology ISBN: 978 0 7334 2609 4 - UNSW CRICOS Provider Code No. 00098G