Birth - Caesarean Delivery
Introduction
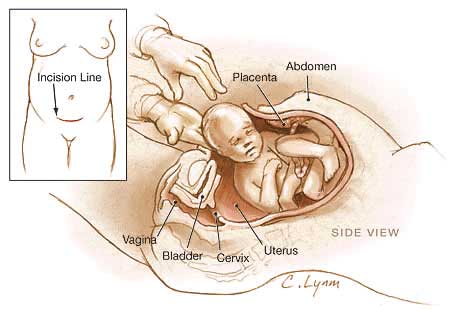
The term "caesarean" comes from the historic description of Julius Ceasar's birth, though probably ficticious as his mother Aurelia survived his birth. The procedure involves surgically cutting skin, abdominal wall and uterus to allow abdominal delivery.
The rate of caesarean delivery compared to normal vaginal birth is variable between countries (12-25%, 20% of all births in Australia) and increasing, particularly in older women. There are a number of different explanations as to why this is occuring, including maternal or fetal complications of either development or delivery.
Importantly this is a maternal surgical procedure which requires time for recovery and there are several studies that have looked also into the effects of caesarean delivery on potential future normal vaginal births.
Please note the UK/Australian "Caesarean" versus USA "Cesarean" spelling differences. Clinically, cesarean section may also be abbreviated to c-section or C/S.
Video Webcast: Hartford Hospital Cesarean Childbirth (September 23rd, 2005)
Some Recent Findings
|
| More recent papers |
|---|
|
This table allows an automated computer search of the external PubMed database using the listed "Search term" text link.
More? References | Discussion Page | Journal Searches | 2019 References | 2020 References Search term: Caesarean Birth | Caesarean Delivery |
| Older papers |
|---|
| These papers originally appeared in the Some Recent Findings table, but as that list grew in length have now been shuffled down to this collapsible table.
See also the Discussion Page for other references listed by year and References on this current page.
|
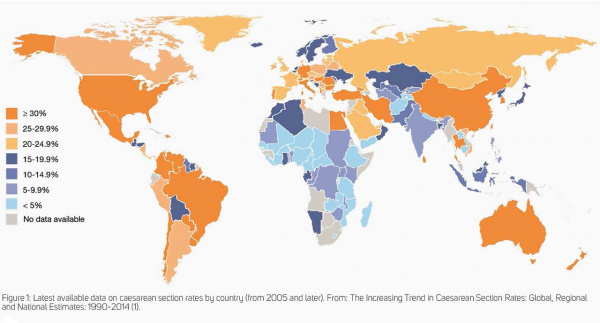
Caesarean Rates by Country
Caesarean rates by country (1990-2014)[8]
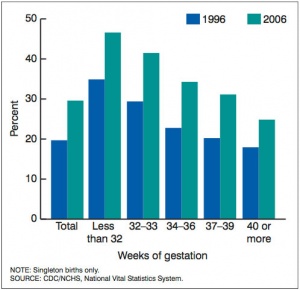
USA Caesarean Rate by Gestational Age
Latest 2013 data[9]

|
|
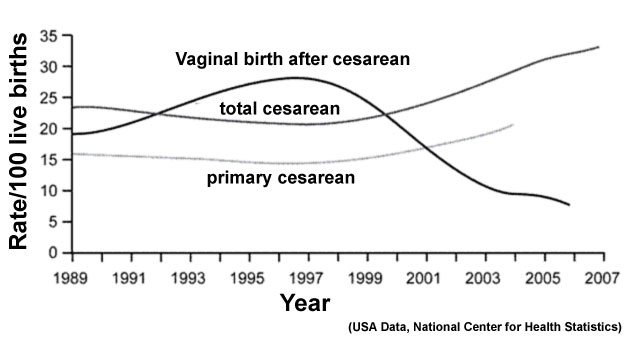
Trial of Labor
Trial of Labor (TOL) or trial of labor after cesarean (TOLAC) is a term used in relation to the offer for a normal vaginal delivery after a previous cesarean delivery. The resulting birth is described as vaginal birth after cesarean (VBAC), in recent years this option has been decreasing while the general caesarian rate increases.
Positive Factors
(increased likelihood of successful VBAC)
- Maternal age <40 years
- Prior vaginal delivery (particularly prior successful VBAC)
- Favorable cervical factors
- Presence of spontaneous labor
- Nonrecurrent indication that was present for prior cesarean delivery
Negative Factors
(decreased likelihood of successful VBAC)
- Increased number of prior cesarean deliveries
- Gestational age >40 weeks
- Birth weight >4,000 g
- Induction or augmentation of labor
Links: USA Guideline (2005) | NIH Consensus - Vaginal Birth After Cesarean (2010)
Robson Classification
The Robson classification[10] (10 group classification) is based on several simple obstetrical parameters; parity, previous CS, gestational age, onset of labour, fetal presentation and the number of foetuses. The classification categories are totally inclusive and also mutually exclusive.

There is no standard clinical classification system for caesarean delivery, with at least 27 classifications identified.[12] Recent studies of data from several countries[11] suggests that the 10 group classification system (Robson Classification[10]), or a modification of this system, may be the current best applied system.
Robson 10 Groups
- Nulliparous women with a single cephalic pregnancy, 237 weeks gestation in spontaneous labour
- Nulliparous women with a single cephalic pregnancy, 237 weeks gestation who either had labour induced or were delivered by caesarean Section before labour
- Multiparous women without a previous uterine soar, with a single cephalic pregnancy, 237 weeks gestation in spontaneous labour
- Multiparous women without a previous uterine soar, with a single cephalic pregnancy, 237 weeks gestation who either had labour induced or were delivered by caesarean Section before labour
- All multiparous women with at least one previous uterine soar, with a single cephalic pregnancy,
- All nulliparous women with a single breeoh pregnancy
- All multiparous women with a single breeoh pregnancy, including women with previous uterine scars
- All women with multiple pregnan- cies, including women with previous uterine scars
- All women with a single pregnancy with a transverse or oblique lie, ihcluding women with previous uterine scars
- All women with a single cephalic pregnancy (37weeks gestation, including women with previous scars
- Links: WHO Robson Classification
References
- ↑ Stark M, Mynbaev O, Vassilevski Y & Rozenberg P. (2016). Could Revision of the Embryology Influence Our Cesarean Delivery Technique: Towards an Optimized Cesarean Delivery for Universal Use. AJP Rep , 6, e352-e354. PMID: 28078171 DOI.
- ↑ Naji O, Wynants L, Smith A, Abdallah Y, Saso S, Stalder C, Van Huffel S, Ghaem-Maghami S, Van Calster B, Timmerman D & Bourne T. (2013). Does the presence of a Caesarean section scar affect implantation site and early pregnancy outcome in women attending an early pregnancy assessment unit?. Hum. Reprod. , 28, 1489-96. PMID: 23585560 DOI.
- ↑ Cunningham FG, Bangdiwala SI, Brown SS, Dean TM, Frederiksen M, Rowland Hogue CJ, King T, Spencer Lukacz E, McCullough LB, Nicholson W, Petit NF, Probstfield JL, Viguera AC, Wong CA & Zimmet SC. (2010). NIH consensus development conference draft statement on vaginal birth after cesarean: new insights. NIH Consens State Sci Statements , 27, 1-42. PMID: 20228855
- ↑ Betrán AP, Gulmezoglu AM, Robson M, Merialdi M, Souza JP, Wojdyla D, Widmer M, Carroli G, Torloni MR, Langer A, Narváez A, Velasco A, Faúndes A, Acosta A, Valladares E, Romero M, Zavaleta N, Reynoso S & Bataglia V. (2009). WHO global survey on maternal and perinatal health in Latin America: classifying caesarean sections. Reprod Health , 6, 18. PMID: 19874598 DOI.
- ↑ Lumbiganon P, Laopaiboon M, Gülmezoglu AM, Souza JP, Taneepanichskul S, Ruyan P, Attygalle DE, Shrestha N, Mori R, Nguyen DH, Hoang TB, Rathavy T, Chuyun K, Cheang K, Festin M, Udomprasertgul V, Germar MJ, Yanqiu G, Roy M, Carroli G, Ba-Thike K, Filatova E & Villar J. (2010). Method of delivery and pregnancy outcomes in Asia: the WHO global survey on maternal and perinatal health 2007-08. Lancet , 375, 490-9. PMID: 20071021 DOI.
- ↑ Howell S, Johnston T & Macleod SL. (2009). Trends and determinants of caesarean sections births in Queensland, 1997-2006. Aust N Z J Obstet Gynaecol , 49, 606-11. PMID: 20070708 DOI.
- ↑ Clark EA & Silver RM. (2011). Long-term maternal morbidity associated with repeat cesarean delivery. Am. J. Obstet. Gynecol. , 205, S2-10. PMID: 22114995 DOI.
- ↑ Betrán AP, Ye J, Moller AB, Zhang J, Gülmezoglu AM & Torloni MR. (2016). The Increasing Trend in Caesarean Section Rates: Global, Regional and National Estimates: 1990-2014. PLoS ONE , 11, e0148343. PMID: 26849801 DOI.
- ↑ Martin JA, Hamilton BE, Osterman MJK, et al. Births: Final data for 2013. National vital statistics reports; vol 64 no 1. Hyattsville, MD: National Center for Health Statistics. 2015. http://www.cdc.gov/nchs/data/nvsr/nvsr64/nvsr64_01.pdf
- ↑ 10.0 10.1 Robson MS. (2001). Can we reduce the caesarean section rate?. Best Pract Res Clin Obstet Gynaecol , 15, 179-94. PMID: 11359322 DOI.
- ↑ 11.0 11.1 Betrán AP, Vindevoghel N, Souza JP, Gülmezoglu AM & Torloni MR. (2014). A systematic review of the Robson classification for caesarean section: what works, doesn't work and how to improve it. PLoS ONE , 9, e97769. PMID: 24892928 DOI.
- ↑ Torloni MR, Betran AP, Souza JP, Widmer M, Allen T, Gulmezoglu M & Merialdi M. (2011). Classifications for cesarean section: a systematic review. PLoS ONE , 6, e14566. PMID: 21283801 DOI.
Books
Caesarean Section NICE Clinical Guidelines, No. 13 National Collaborating Centre for Women's and Children's Health (UK). London: RCOG Press; 2004 Apr. ISBN-10: 1-904752-02-0 Bookshelf
Reviews
Horey D, Weaver J & Russell H. (2004). Information for pregnant women about caesarean birth. Cochrane Database Syst Rev , , CD003858. PMID: 14974041 DOI.
- Journal of American Medical Association JAMA Patient Page: Cesarean Delivery (USA) - one page Caesarean delivery information sheet (PDF)
- electronic Med J Aust Caesarean section: a matter of choice? by de Costa, C.M. MJA 1999; 170: 572-573
Articles
Milne J, Gafni A, Lu D, Wood S, Sauve R & Ross S. (2009). Developing and pre-testing a decision board to facilitate informed choice about delivery approach in uncomplicated pregnancy. BMC Pregnancy Childbirth , 9, 50. PMID: 19874628 DOI.
Search PubMed
Search Pubmed: Caesarean Delivery | Cesarean Delivery
External Links
External Links Notice - The dynamic nature of the internet may mean that some of these listed links may no longer function. If the link no longer works search the web with the link text or name. Links to any external commercial sites are provided for information purposes only and should never be considered an endorsement. UNSW Embryology is provided as an educational resource with no clinical information or commercial affiliation.
Glossary Links
- Glossary: A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | Numbers | Symbols | Term Link
Cite this page: Hill, M.A. (2024, April 28) Embryology Birth - Caesarean Delivery. Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/Birth_-_Caesarean_Delivery
- © Dr Mark Hill 2024, UNSW Embryology ISBN: 978 0 7334 2609 4 - UNSW CRICOS Provider Code No. 00098G