Note there are additional glossaries associated with spermatozoa, oocyte renal.
- androgens - male sex hormones, such as testosterone, or the more potent dihydrotestosterone (DHT, 5α-dihydrotestosterone, androstanolone, 5α-androstan-17β-ol-3-one), formed by the enzyme 5α-reductase. Dihydrotestosterone).
- androgen insensitivity syndrome - (AIS) Clinical term for a developmental abnormality affecting genital development, through a fetal tissue insensitivity to male hormones.
- anogenital distance - (AGD) A clinical measure of a parameter sexually dimorphic for genital development. This distance, from the posterior aspect of the scrotum to the anal verge, has been used as a marker for endocrine disruption in animal studies and may be shorter in infant males with genital anomalies. Recently been shown that infertile men possessed significantly shorter mean AGD.
- anorchia - (embryonic testicular regression, vanishing testis syndrome) Clinical term for the absence of testes in a 46,XY individual with a male phenotype. Rare abnormality with an incidence of about 1 in 20,000 male births, and occurs more frequently with cryptorchidism (1 in 177 cases).
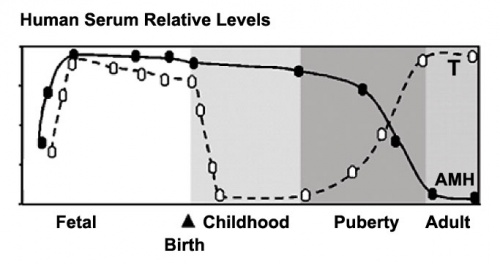
- Anti-Mullerian Hormone (AMH, Müllerian Inhibiting Substance, MIS, Müllerian Inhibiting Factor, MIF) A secreted glycoprotein factor (transforming growth factor-beta, TGF-beta superfamily) that regulates gonadal and genital tract development. In the male embryo, the Sertoli cell secrete AMH and inhibit paramesonephric (Mullerian) duct development. In postnatal males, AMH increases during the first month, reaching peak level at 6 months of age, and then slowly declines during childhood falling to low levels in puberty. In reproductive age women, AMH is produced in the ovary by the granulosa cells surrounding preantral and small antral follicles and serum levels may reflect the remaining follicle cohort and decrease with age. AMH | TGF-beta | OMIM - AMH
- ascending testis — (Undescended testis, cryptorchidism) postnatal male genital abnormality where a previously descended testis no longer lies within the scrotum. Peak incidence occurs around 10 years of age (affects 1-2%) and may also occur as a complication of inguinal hernia surgery in children.
- Bardet-Biedl syndrome - (BBS) is an abnormality with triallelic inheritance and is characterized by a rangne of multisystem abnormalities (cone-rod dystrophy, truncal obesity, postaxial polydactyly, cognitive impairment, neural development, male hypogonadotrophic hypogonadism, complex female genitourinary malformations, and renal dysfunction).
- Bartholin gland - (greater vestibular gland) A pair of female external genital tract glands which secretes mucus to lubricate the vagina. The equivalent male gland is the Bulbourethral gland or Cowper's gland.
- Template:Bicornuate uterus - ("heart-shaped" uterus) Female uterus (internal genital tract) abnormality, where the paramesonephric ducts (Müllerian ducts) fail to completely fuse forming two separate body parts that fuse close to the opening into the vagina.
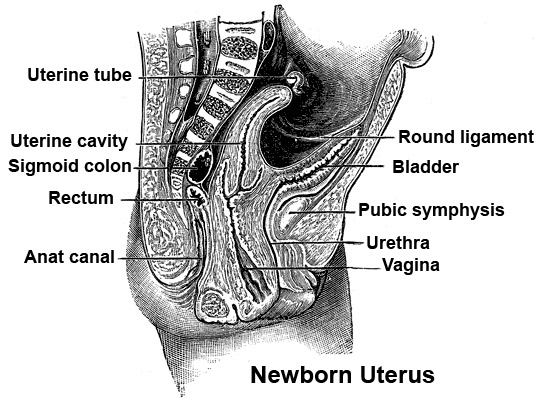
- broad ligament - Human female genital tract mesentery formed by a double fold of peritoneum that connects the uterus to the peritoneal floor and walls. Anatomically it has three parts: mesometrium (surrounding the uterus), mesosalpinx (surrounding the uterine tube) and mesovarium (surrounding the ovary).
- bulbourethral gland - (Cowper's gland) A male genital tract gland which secretes a small amount of a thick clear mucous fluid prior to ejaculation, the alkaline content apparently buffers acidity of the urethra. The equivalent female genital tract gland is the greater vestibular gland or Bartholin gland.
- chordee - abnormality of bending of the penis that may involve soft-tissue tethering. The second most common (8.6%) congenital penile anomaly and can be found associated with hypospadia.
- cloaca - (cloacal cavity) The term describing the common cavity into which the intestinal, genital, and urinary tracts open in vertebrates. Located at the caudal end of the embryo it is located on the surface by the cloacal membrane. In many species this common cavity is later divided into a ventral urogenital region (urogenital sinus) and a dorsal gastrointestinal (rectal) region.
- cloacal membrane - Forms the external lower membrane limit (caudal end) of the early gastrointestinal tract (GIT). This membrane is formed during gastrulation by ectoderm and endoderm without a middle (intervening) layer of mesoderm. The membrane breaks down to form the initial "anal opening" of the gastrointestinal tract. The upper end of the gastrointestinal tract has a similar embryonic membrane, the buccopharyngeal membrane.
- clomiphene citrate - (CC) A fertility drug taken orally to promote the process of follicle/egg maturation in superovulation therapy. (CC) an anti-estrogen (MRL-41) therapy for WHO group II (eu-oestrogenic) infertility associated with polycystic ovary syndrome. Used for more than 40 years it is a simple, cheap treatment, with low side effects and yields a 25% live birth rate. Alternative therapeutics being considered are metformin, aromatase inhibitors and low-dose FSH.
- congenital adrenal hyperplasia - (CAH, adrenal virilism) Abnormality of the fetal adrenal cortex, alters cortisol and androgens with different effects dependent upon sex: in females masculization of the external genitalia; in males, disorder often unnoticed until postnatally. In both sexes, accelerated skeletal growth and sexual maturation is seen in late childhood. Caused by a deficiency or absence of the enzyme 21-hydroxylase in the adrenal cortex. Grouped with the Disorders of Sex Development (DSD) and classified by Prader stages. (More? congenital adrenal hyperplasia | adrenal | genital abnormalities)
- 'Cowper's gland - (bulbourethral gland) A male genital tract gland which secretes a small amount of a thick clear mucous fluid prior to ejaculation, the alkaline content apparently buffers acidity of the urethra. The equivalent female genital tract gland is the greater vestibular gland or Bartholin gland.
- cryptorchid testes - (cryptorchidism) A male genital abnormality where the testes remain undescended in the abdominopelvic cavity or other non-scrotal locations. (More? cryptorchidism | Male)
- DAX1 - (NR0B1) Original gene acronym for "D"osage sensitive sex reversal (DSS), "A"drenal hypoplasia congenita (AHC) critical region on the "X" chromosome, gene "1". Current gene name is Nuclear Receptor Subfamily 0, Group B, Member 1 (NR0B1), a nuclear hormone receptor involved in female ovary development. (More? HGNC | OMIM)
- DAZL - Acronym for DAZ-like due to homology to DAZ (Deleted in AZoospermia), a gene on the long arm of the Y chromosome that is frequently deleted in infertile men with nonobstructive azoospermia. HGNC | OMIM)
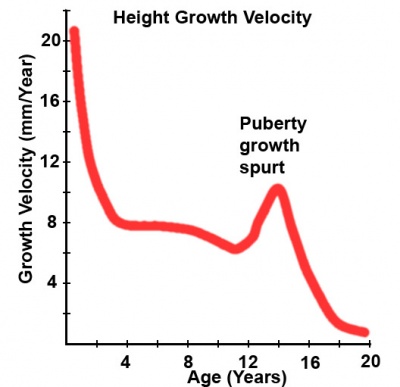
- delayed puberty - (Latin, pubertas = adulthood) An abnormal timing of puberty. Determined in boys by a lack of increase in testicular volume by the age of 14 years. In girls, no breast development by the age of 13.5 years and a lack of menstruation by the age of 16 years. There can also be a "pubertal arrest" where there is no progress in puberty over 2 year period.
- DES - Acronym for Diethyl stilbestrol or diethylstilbetrol, a drug prescribed to women from 1938-1971 to prevent miscarriage in high-risk pregnancies. Acts as a potent estrogen (mimics natural hormone) and therefore a potential endocrine disruptor. Female fetus, increased risk abnormal reproductive tract and cancer. Male fetus, abnormal genitalia. Banned by USA FDA in 1979 as a teratogen, previously used as livestock growth promoter.
- DHEA - (dehydroepiandrosterone, androstenolone) precursor of sex steroid hormones and is converted to testosterone and estradiol. Postnatally, an abundant circulating steroid produced in the adrenal gland. The fetal adrenal cortex produces dehydroepiandrosterone sulfate (DHEA-S) used by the placenta to produce estrogens. DHEA, androstenedione, and testosterone can be metabolized to epiandrosterone, and etiocholanolone. PMID 15635500
- dihydrotestosterone - (DHT) The hormonally active form of testosterone (male sex hormone) produced by enzyme (5-alpha reductase) conversion. In the male embryo, this can occur in the genital skin which then supports external genital development. In the adult, this conversion occurs in a number of different tissues. A known treatment for prostate cancer include 5-alpha reductase inhibitors.
- Disorder of Sex Development - (DSD) A new terminology to describe disorders of sex development. The previous human sex development terminology (intersex, true hermaphrodites, male pseudohermaphrodites and female pseudohermaphrodites) are considered outdated and stigmatising and have been replaced with this general term "Disorders of Sex Development" (DSD) established by the Consensus statement on management of intersex disorders. International Consensus Conference on Intersex. International Consensus Conference on Intersex organized by the Lawson Wilkins Pediatric Endocrine Society and the European Society for Paediatric Endocrinology. (More? PMID 16882788)
- ductuli efferentes - In the testis (male gonad) series of tubular structures which arise from the rete testis and conduct spermatazoa into the ductus epididymidis. Their columnar epithelium lining consisting of both absorptive and ciliated cells (giving rise to "cogwheel appearance) which removes much of the fluid associated with the spermatazoa leaving the testes (also by the upper epididymis) thereby increasing the spermatazoa concentration. (More? testis)
- ductus deferens - (vas deferens, Latin, deferens = carrying-away vessel) The excretory duct of the testis that is the continuation of the canal of the epididymis. Develops from the mesonephric duct. Anatomically beginning at the lower part of the tail of the epididymis it is at first very tortuous, but gradually becoming less twisted it ascends along the posterior border of the testis and medial side of the epididymis, and, as a constituent of the spermatic cord, traverses the inguinal canal to the abdominal inguinal ring. (More? ductus deferens | testis)
- ductus epididymidis - (epididymidis) male testes tubular structure which arise from the ductuli efferentes and conduct spermatazoa into the ductus deferens (vas deferens). The long duct is lined by a tall pseudostratified columnar epithelium. (More? testis)
- ectopic testis — (Undescended testis, cryptorchidism) male genital abnormality the testis is clinically palpated in a location outside the normal path of descent, such as the perineum or femoral area.
- epispadias - Uncommon abnormality associated with the penis, 1 in 30,000 infant males, external urethral opening on the dorsal surface of penis.
- epoophoron - (rete ovarii, broad ligament cyst) A group of epithelial tubules that can be located in the mesosalpinx possibly mesonephric duct in origin. Occurs when a segment of the mesonephric duct remains in the female, associated with either the ovary and broad ligament. This "male remnant" will appear as a cyst (broad ligament cyst, adnexal papillary cystadenoma of probable mesonephric origin, APMO) with an appearance that differs depending upon the state of differentiation when the original abnormality occurred.
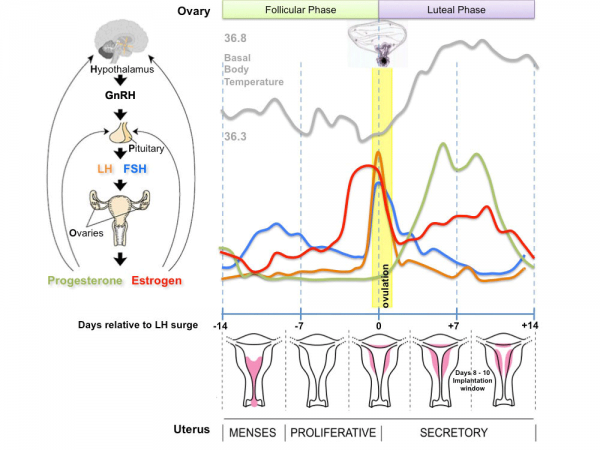
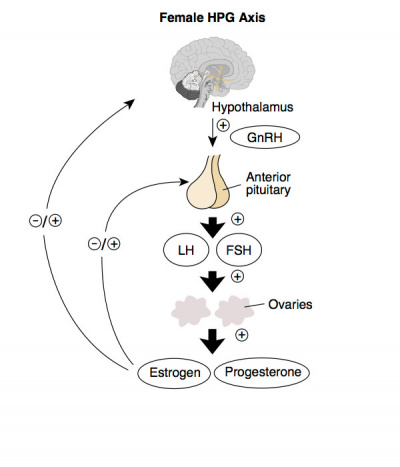
- estrogens - (oestrogens) Sex hormones found in both male and female. In the female, this hormone is produced by the ovaries and is responsible for development of secondary feminine sex characteristics. Together with progesterone these hormones also regulate changes that occur each menstrual cycle. In the male, Leydig cells produce estrogen into the rete testis fluid at variable levels in different species. During female development the fetal adrenal gland synthesises DHEA, an oestrogen precursor, converted by the placenta into estrogen (estradiol). During male embryonic development exposure to high levels of estrogen can lead to genital abnormalities.
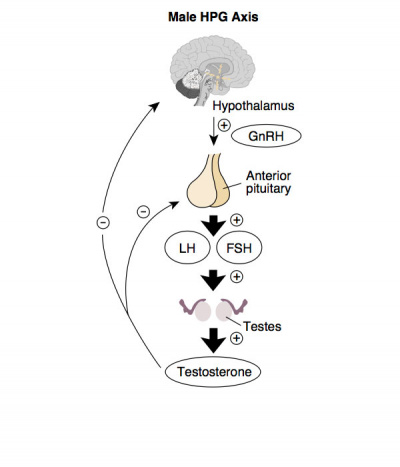
- follicle stimulating hormone - (FSH, gonadotropin) A glycoprotein hormone secreted by anterior pituitary (adenohypophysis gonadotrophs, a subgroup of basophilic cells) and acts on gametogenesis and other systems in both males and females. In females, FSH acts on the ovary to stimulate follicle development. Negative feedback by inhibin from the developing follicle decreases FSH secretion. In males, acts on the testis Sertoli cells to increase androgen-binding protein (ABP) that binds androgens and has a role in spermatogenesis.
- Fraser syndrome - (cryptophthalmos-syndactyly syndrome) An autosomal recessive congenital malformation syndrome characterized by cryptophthalmos, syndactyly, and urogenital defects (bicornuate uterus, imperforate anus, anal stenosis or renal malformations).
- Gartner's duct - A female developmental abnormality caused by the persistance of the mesonephric duct (normally lost in females) when the ureteric bud fails to separate from the mesonephric duct and can generate a broad ligament cyst or vaginal cyst. Named after Hermann Treschow Gartner (1785-1827) a Danish surgeon and anatomist.
- genitalia - Latin, genitalis = “of or belonging to generation”)) The term used to describe either the external or internal male and female sexual and reproductive organs.
- genital ridge - (gonadal ridge) The thickened epithelial/mesenchymal region adjacent and medial too the mesonephros. Primordial sex cells migrate into this region to form the indifferent gonad. These undifferentiated gonads have a cortex and a medulla. Female XX chromosome complex, cortex differentiates into an ovary, and medulla regresses. Male XY complex, medulla differentiates into a testis and cortex regresses.
- genital tubercle - (GT) A prominence or rounded protuberance extending ventrally at the inferior end of the body of the embryo. It has initially a sexually indifferent external genitalia structure and contributes to either male (glans penis) and female (clitoris) external genitalia. The endodermally derived urethral epithelium lies within the genital tubercle and functions as an organizer by expression of sonic hedgehog (Shh). This signaling is required for initial genital tubercle formation and for ectoderm induction for urethral tube closure.
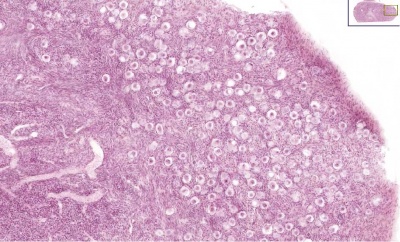
- germ cell - (primordial germ cell, gonocyte) Term used to describe the embryonic population of cells that will form either the spermatozoa (sperm) progenitor in the embryonic testes or oocyte (egg) progenitor present in the primordial follicle ovary from birth, located in the stroma of the ovary cortex beneath the tunica albuginea. In humans, these cells initially migrate during week 5-6 into the genital ridge which will later form the gonad.
- gonadotropin - (Greek, gonos = seed; gonadotrophin, Gn) Three separate endocrine factors form the gonadotropins. Two from the anterior pituitary, luteinizing hormone (LH) and follicle stimulating hormone (FSH). The third produced by the implanting conceptus trophoblast cells and the corpus leutum in primates chorionic gonadotropin (CG), the human form is human chorionic gonadotropin (hCG). Both luteinizing hormone and follicle stimulating hormone are stimulated for release by the hypothalamus gonadotropin releasing hormone.
- greater vestibular gland (Bartholin gland) A pair of female external genital tract glands which secretes mucus to lubricate the vagina. The equivalent male gland is the Bulbourethral Gland or Cowper's Gland.
- gubernaculum - A mesenchymal structure occurring associated with gonad development and involved in testes descent. Two factors, insulin-like peptide hormone 3 (INSL3) and androgen, have been shown to be involved with gubernaculum development. Insulin-like peptide 3 (INSL3) hormone receptor is RXFP20.
- Mayer-Rokitansky syndrome - (MRK anomaly, Rokitansky-Küster-Hauser syndrome, RKH syndrome, RKH) congenital absence of the vagina, dyspareunia, vaginal agenesis.
- Müllerian inhibiting substance - (MIS, anti-Müllerian hormone, AMH) A secreted glycoprotein factor (transforming growth factor-beta, TGF-beta superfamily) that regulates gonadal and genital tract development. In the male embryo, the Sertoli cell secrete AMH and inhibit paramesonephric (Müllerian) duct development. In postnatal males, AMH increases during the first month, reaching peak level at 6 months of age, and then slowly declines during childhood falling to low levels in puberty. In reproductive age women, AMH is produced in the ovary by the granulosa cells surrounding preantral and small antral follicles and serum levels may reflect the remaining follicle cohort and decrease with age.
- Ohno's law - A genetic evolutionary theory that suggests that the mammalian X chromosomes are conserved among species. Named after Susumu Ohno 大野 乾 (1928 – 2000) a Japanese-American geneticist and evolutionary biologist.
- perineal body - (central tendon of perineum) anatomical connection between muscles of the pelvic floor. In males, it is found between the bulb of penis and the anus. In females, provides support of the lower part of the vagina and the function of the anal canal.
- Prader stages - (Prader scale) Clinical term used to describe the congenital adrenal hyperplasia (CAH) virilization of female genitalia. Two normal (Stage 0 – Normal female genitalia; Stage 6 – Normal male genitalia) and five distinct abnormal stages (1 to 5 increasing virilisation).
- prepuce - external genital term describing in the male the penis foreskin, in the female the fold of skin surrounding the clitoris.
- primordial germ cell - (germ cell, gonocyte) Term used to describe the embryonic population of cells that will form either the spermatozoa (sperm) progenitor in the embryonic testes or oocyte (egg) progenitor present in the primordial follicle ovary from birth, located in the stroma of the ovary cortex beneath the tunica albuginea. In humans, these cells initially migrate during week 5-6 into the genital ridge which will later form the gonad.
- hermaphrodite - (Disorder of Sex Development, DSD) This historic terminology is no longer applied to abnormal sexual development and has been replaced with the term (Disorder of Sex Development (DSD). Humans having both male and female reproductive organs, occurs in both male and female forms and mixed ovotesticular DSD.
- hydrocele - (Greek, hydro = water, coele/koilia = cavity) a fluid-filled cavity of either testis or spermatic cord, where peritoneal fluid passes into a patent processus vaginalis.
- hydrocolpos - Clinical condition caused by accumulation of fluid in the vagina due to developmental obstruction by either an imperforate hymen or a transverse vaginal septum. Associated complications include: multiple urinary tract infections, hydrocolpos infection, sepsis, failure to thrive, ruptured hydrocolpos, and development of hydronephrosis in previously normal kidneys.
- hydrosalpinx - (Greek, hydro = water + salpinx = trumpet) Accumulation of interstitial fluid (edematous) in either one or both blocked uterine tubes or fallopian tubes due to a previous tubal infection. (Salpinx refers to the trumpet shape of the uterine tube. This blockage can impact upon maternal fertility and may require in vitro fertilization (IVF) techniques for reproduction.
- hypospadias - A male external genital abnormality resulting from a failure of male urogenital folds to fuse in various regions and are therefore classified by the location of the opening meatus). This is the most common penis abnormality (1 in 300) and one of the highest in the list of frequently reported birth defects. (More? hypospadias)
- infundibulum - The uterus funnel-shaped initial segment of uterine tube (oviduct or Fallopian tube) opening into peritoneal cavity and connected to the ampulla. The peritoneal opening sitting over the ovary.
- inguinal canal - The anatomical pathway for male testes descent from the abdominal cavity (fetal) into the scrotum.
- interstitial cell - (Leydig cell) Male gonad (testis) cell that secrete the androgen testosterone, beginning in the fetus. Required for internal and external male genital development.
- Leydig cell - (interstitial cell) Male gonad (testis) cell that secrete the androgen testosterone, beginning in the fetus. These cells are named after Franz von Leydig (1821 - 1908) a German scientist who histologically described these cells.
- ligamentum teres - (ligamentum teres uteri, Hunter's ligament) The round ligament of uterus which maintains the ventral uterine position.
- luteinizing hormone - (LH, gonadotropin, lutropin, Interstitial Cell Stimulating Hormone, ICSH) Glycoprotein hormone releasd from anterior pituitary hormone that acts on the gonad and has a role in male and female reproduction. In female, increase in concentration during the menstrual cycle triggers ovulation (release of the oocyte). In male, stimulates testis interstital cell (Leydig cell) production of testosterone. Gonadotrophins have been used clinically in humans for the treatment of female infertility.
- Mayer-Rokitansky-Kuster-Hauser syndrome - (MRKH) Abnormality of development of the female genital tract: partial or complete absence (agenesis) of the uterus; absent or hypoplastic vagina; normal fallopian tubes, ovaries, normal external genitalia and normal female chromosome pattern (46, XX). Has an incidence of approximately 1 in 4500 newborn girls and has been associated with a microdeletion at 17q12.
- mediastinum testis - (Latin, medialis = middle) A single conical mass of connective tissue within the testis (male gonad) which extends from the tunica albuginea (cortical thick capsule surrounding the testis) into the seminiferous tubule region (medullary). Embedded within this connective tissue are the rete testis component of the duct conduction system for spermatozoa.
- mesonephric duct - (Wollfian duct) An early developing urogenital paired duct system that initially runs the length of the embryo, that will differentiate and form the male reproductive duct system (ductus deferens). In females, this duct degenerates occasionally some remnants may remain associated in broad ligament.
- mesorchium - A peritoneal fold attaching the testes to the mesonephros during development.
- mesovarium - The mesentry of the ovary formed from a fold of the broad ligament that attaches the ovary through this structure pass the vessels and nerves to the ovary, entering at the hilus of the ovary.
- Müllerian duct - (paramesonephric duct) An embryonic paired duct system that will form the epithelial lining of female reproductive organs: utererine tube, uterus, upper vaginal canal. This duct system degenerate in male gonadal development. Named after Johannes Peter Müller (1801-1858) a German scientist.
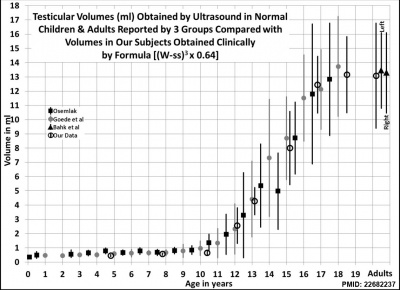
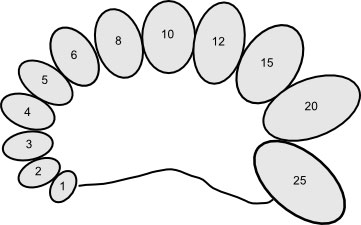
- orchidometer - (orchiometer) A clinical instrument used to measure postnatal testis volume using 12 beads ranging from 1 to 25 millilitres.
- ovarian reserve - (ovarian reserve markers) Clinical term describing the ability for follicular development in ovaries in response to gonadotropins. This reserve value is relevant for fertility and in vitro fertilization treatments and a number of different ovarian reserve serum and ovarian markers have been identified: baseline follicle stimulating hormone (FSH) levels, baseline anti-Müllerian hormone (AMH) levels, and antral follicle count (AFC). In addition, with reproductive aging there is seen both a quantitative and a qualitative reduction of the primordial follicle pool available.
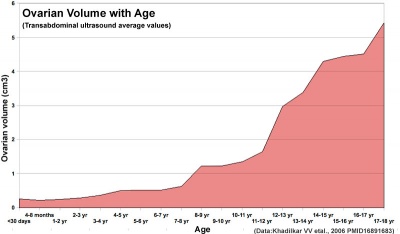
- ovary - The two female gonads where female germ cells (oocytes, eggs) are generated and also the source of estrogen and progesterone the female hormones regulating secondary sex characteristics and menstrual cycle uterine changes. The ovary is embryonically formed from primordial germ cells entering region of the paired mesonephric ducts (Wolffian ducts) which are lost in females.
- oviduct - (uterine horn, fallopian tube, oviduct, salpinx) see uterine tube. A pair of tubular structures designed to transport the oocyte (egg) from the ovary to the uterus body.
- paramesonephric duct - (Müllerian duct) (Greek, para = "beside") The paired ducts that lie beside the mesonephric ducts, that will differentiate in the female embryo to form the female internal genital tract (uterine tubes, uterus, upper vaginal canal). Paramesonephric duct differentiation in females requires Wnt (WNT7a, WNT5a) signaling through the intracellular β-catenin pathway.
- para-urethral gland - (Skene gland, Skene's gland, lesser vestibular glands, female prostate gland) Female genital glands on the anterior wall of the vagina and around the lower end of the urethra. Named in 1880 after Alexander Johnston Chalmers Skene (1838-1900) an American gynaecologist.
- raphe - Anatomical line of fusion of the urogenital folds lying along the urethra and scrotum in male external genitalia.
- rectouterine pouch - (Pouch of Douglas or rectovaginal) Anatomical description of the female peritoneal cavity lying between the back wall of the uterus and rectum.
- rete testis - (Latin, rete = "net", refers to a network) The duct (epithelial tubules) conduction system for spermatazoa embedded within the mediastinum (connective tissue) located in the center of the testis (male gonad) derived from the mesonephric duct, and allow spermatazoa to travel from the seminiferous tubules to the vasa efferentia.
- scrotoplasty - (oscheoplasty) Clinical surgical term for the repair or plastic surgery of the scrotum. This procedure is often associated with the repair of hypospadia.
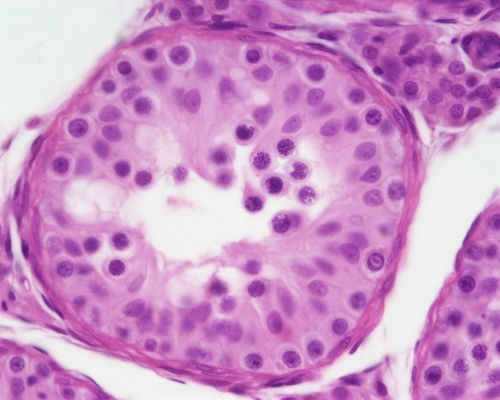
- seminiferous tubule - (spermatogenic epithelium) Male genital testis structure where spermatozoa develop within the wall. Consists of outer smooth muscle layer, spermatogonia, sertoli cells and maturing spermatozoa.
- sertoli cell - The supporting cells in the testes (male gonad) that induce primordial germ cells to commit to sperm development. Support is nutritional and mechanical, as well as forming a blood-testis barrier. In development, these cells secrete anti-Mullerian hormone (AMH), which causes the Mullerian duct (paramesonephric duct) to regress, and help to induce other somatic cells to differentiate into Leydig cells.
- sex chromosome - Term used to describe both the male Y chromosome and the female X chromosome. All other chromosomes that are not the sex chromosomes in the genome are described as autosomes. These terms are also used in describing the location or inheritance of genes and/or genetic disorders.
- sinovaginal bulbs - The caudal ends of the paired mesonephric ducts (Wolffian ducts) thought to be involved in vaginal development, they are under negative control by androgens.
- spermatogenesis - (Greek, genesis = origin, creation, generation) The term used to describe the process of diploid spermatagonia division and differentiation to form haploid spermatozoa within the testis (male gonad). The process includes the following cellular changes: meiosis, reoorganization of DNA, reduction in DNA content, reorganization of cellular organelles, morphological changes (cell shape). The process following meiosis is the change in cell shape and organization, called spermiogenesis.
- spermatogenic epithelium - Term used to describe the wall of the seminiferous tubule consisting of spermatogonia, developing spermatozoa stages and sertoli cells.
- spermatogonia - (spermatogonial stem cell) These cells form in the embryo from the primordial germ cell and are located in the seminiferous tubule adjacent to the basal membrane. The cells can either divide and separate to renew the stem cell population, or they divide and stay together as a pair (Apr spermatogonia) connected by an intercellular cytoplasmic bridge to begin to differentiate and eventually form spermatozoa.
- spermatozoa - (spermatozoon, singular term) The male haploid gamete cell produced by meiosis in the testis (male gonad) seminiferous tubule. In humans, produced from puberty onwards and develop from the diploid stem cell the spermatogonia. The developmental meiosis is called spermatogenesis and the final morphologiccal (shape) change is called spermeiogenesis. The mature human spermatozoon formed from the spermatid has a head, neck and tail and is about 60 µm long. At ejaculation these cells undergo capacitation (activation) and become motile.
- testis - (Latin testis = "witness", plural testes) Anatomically the male gonad where male germ cells (spermatozoa) are generated and also the source of testosterone (male hormone). Embryonically formed from primordial germ cells entering region of the paired mesonephric ducts (Wolffian ducts) which are preserved in male gonad development and lost in females.
- testis cord - (sex cord) The embryonic precursor of the seminiferous tubule. These form embryonically initially as a complex series of parallel transverse loops separated by interstitial cells. During fetal development these cords elongate and expand leading to the convoluted structure of the seminiferous epithelium.
- testis-determining factor - (TDF, Sry, Testis-Determining Factor on Y, TDY ) Protein name for the protein transcription factor product of the Sry gene on the Y chromosome responsible for maleness. This protein is a member of the high mobility group (HMG)-box family of DNA binding proteins. See also the transcription factor SRY-related protein, SOX9 (SRY-related high-mobility group (HMG) box 9)
- testosterone - A steroidal hormone secreted by the gonad (testis and ovary) and in males is the androgen which regulates genital (gonadal and tract), secondary sex characteristics and neural development. The steroid is converted to the active metabolite dihydrotestosterone (DHT) by the enzyme 5-alpha reductase for the genital effects and estradiol by the enzyme aromatase for the neural effects.
- true undescended testis — (Undescended testis, cryptorchidism) male genital abnormality the testis lies along the expected path of descent but has never been present in the scrotum.
- tubal factor - A structural or functional damage of one or both fallopian tubes that reduces fertility, described as tubal factor infertility (TFI).
- tunica albuginea - A dense mesenchymal connective tissue layer lying between germinal epithelium and cortical region of female ovary, or the equivilaent capsule of the male testis forming a thick fibrous capsule. Male forms the testicular septations and the mediastinal testis. Female lies under the surface epithelium of the ovary.
- tunica vaginalis - The serous membrane pouch covering the testis formed from the saccus vaginalis of the peritoneum.
- unicornuate uterus - An abnormality of uterine development where the paramesonephric ducts (Mullerian ducts) fail to fuse. A single paramesonephric duct can fuse with the vaginal plate and will opens into the vagina, while the other duct forms a diverticulum. There are a range of additional uterine abnormalities based upon the degree of initial duct fusion and regression. Uterus didelphys (double uterus) is a rare condition where the entire tract is separated.
- urogenital fold - (urogenital ridges, urethral folds) The ventral portion of the original cloacal folds, which contribute to the formation of the urethral groove on the ventral aspect of the genital tubercle. In females, these folds remain separate. In males, these folds will later fuse, failure of complete fusion leads to the male genital abnormality hypospadia.
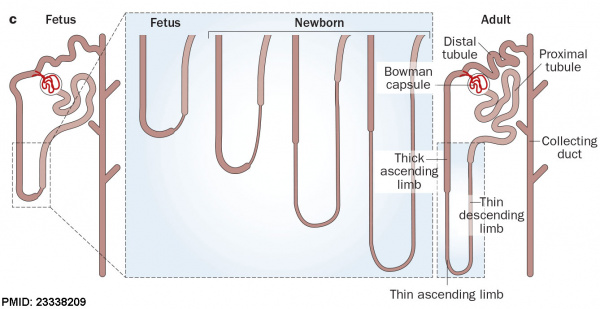
- uteric bud - Renal (kidney) development term for paired lateral diverticulum epithelial tubes arising from each mesonephric duct near its cloacal connection. This branch from the mesonephric duct extends into the intermediate mesoderm (metanephric mesenchyme) inducing the surrounding this mesoderm (metanephric blastema) to differentiate. The uteric bud gives rise to the renal collecting ducts, calyces, pelvis and developing ureters.
- uterine body - Anatomical term describing the region of the uterus above the uterine isthmus and below the opening of the uterine tubes.
- uterine duplication - (uterus didelphys, double uterus, uterus didelphis, bicorporeal uterus) Rare uterine developmental abnormality where the paramesonephric ducts (Mullerian ducts) completely fail to fuse generating two separate uterus parts each connected to the cervix and having an ovary each. Failure of fusion of lower paramesonephric ducts, with either double or single vagina. ESHRE/ESGE classification of uterine anomalies - U3.
- uterine isthmus - Anatomical term describing the region between the uterine body (corpus) and the cervix.
- uterine gland - (endometrial gland) The simple tubular glands formed by invagination of the uterine endometrium (a columnar epithelium of ciliated cells and secretory cells). The glands extend into the underlying thick vascular stromal layer. The glands line the uterus body and change in appearance and secretion during the menstrual cycle. The glands secretions function to provide the initial nutritional support of the conceptus and may have a role in maintaining adhesion.
- uterine tube - (uterine horn, oviduct, fallopian tube, salpinx) A pair of tubular structures that transport the oocyte (egg) from the ovary to the uterus body. They are located laterally on the upper uterus and consist medial to lateral of three main parts: isthmus (medial constricted third), ampulla (intermediate dilated portion) and infundibulum (containing the abdominal opening/ostium, surrounded by finger-like fimbriae). The tube has structurally several layers: a lining mucosa (mix of ciliated and secretory epithelium), a middle muscularis layer (inner circular muscle layer and an outer longitudinal layer) and outer serous layer (peritoneal).
- uterus - The female internal genital (reproductive) tract forming a hollow muscular walled organ, embryonically derived from the paramesonephric ducts. The human uterus has two uterine tubes (fallopian tubes, oviducts) where the first week of development occurs and a single hollow body where implantation of the blastocyst normally occurs. Following puberty, the non-pregnant uterus (epithelium and underlying stroma) undergoes cyclic changes under the influence of hormones, the menstrual cycle. This cycle of uterine changes ceases during pregnancy. In pregnancy, the uterus contributes the maternal component of the placenta.
- vagina - Part of female genitalia formed from the paramesonephric duct develops as a muscular tube between the uterus and vestibule.
- vulva - (Latin, volva or vulva = "female genitals"; vulvar vestibule) Term used to describe the external genital organs (genitalia) of the female.
- Wolffian duct - (mesonephric duct, preferred terminology), A developmental duct that runs from the mesonephros to cloaca. The duct in male differentiates to form the ductus deferens and in female the same structure regresses. Historically named after Caspar Friedrich Wolff (1733-1794), a German scientist and early embryology researcher and is said to have established the doctrine of germ layers.
- X chromosome - The female sex chromosome, which following sexual reproduction is inherited from each parent in females, and inherited from the mother in males. This inheritence pattern impacts upon the pattern of genetic disease. In females, a single X chromosome is inactivated in each cell. X chromosome
- X Inactivation - Process that occurs in all cells within females, each cell has 2 copies of the X chromosome (one from father and one from mother) one of copy of which is randomly inactivated throughout the entire body in order to maintain gene dosage. Recent studies have shown that this process starts in female human preimplantation-stage embryos, by accumulation of Xist RNA on one of the two X chromosomes starting around the 8-cell stage. X Inactivation
- Y chromosome - The male sex chromosome which contains the sry gene producing Testis-Determining Factor required for male phenotype and can only be inherited from father. In humans the chromosome contains 200+ genes and consists of 50 million base pairs. Testis-Determining Factor (TDF; Testis-Determining Factor on Y, TDY ) is a protein transcription factor and a member of the high mobility group (HMG)-box family of DNA binding proteins. See also the transcription factor SRY-related protein, SOX9 (SRY-related high-mobility group (HMG) box 9). Y Chromosome
|