Talk:Placenta - Abnormalities: Difference between revisions
No edit summary |
No edit summary |
||
| Line 1: | Line 1: | ||
{{Talk Page}} | |||
==2010== | |||
===Recurrent hydatidiform moles=== | |||
Eur J Obstet Gynecol Reprod Biol. 2010 May;150(1):3-7. Epub 2010 Feb 19. | |||
Williams D, Hodgetts V, Gupta J. | |||
Source | |||
Department of Clinical Genetics, Birmingham Women's Hospital, Edgbaston, Birmingham B15 2TG, United Kingdom. | |||
Abstract | |||
Hydatidiform moles (HMs) are abnormal conceptions of excessive trophoblast development resulting in abnormal human pregnancies with no embryo and cystic degeneration of the chorionic villi. Prompt diagnosis, treatment and follow-up of patients using assays for betahCG from centres that specialise in this condition enable early diagnosis of potential malignant change. Hydatidiform moles occur quite frequently and although recurrence is rare, women who have experienced one molar pregnancy should be aware that they are at an increased risk of a further molar pregnancy in comparison to other women in the general population. For some women multiple molar pregnancies occur. In these women the recurrent molar pregnancies may be non-familial, referred to as recurrent molar hydatidiform moles in this article, or may result from an inherited predisposition, which we refer to as familial recurrent hydatidiform moles. We use the term familial biparental hydatidiform moles (FBHMs) for cases in which the parental contribution to the moles has been investigated and found to be biparental. It is important to recognise, however, that in some apparently non-familial cases, the absence of female siblings, or the absence of female siblings who have tried to conceive, may not allow the inherited nature of the molar pregnancies to manifest in more than one woman and be obviously familial. This review considers our current understanding about the aetiology of HMs and explores the mechanisms of both types of recurrent hydatidiform moles. It highlights the role that genetics can play in determining the origin of multiple molar pregnancies, which should be considered essential in providing women with accurate advice about their risk of recurrence, so allowing them to make appropriate reproductive choices. | |||
Copyright (c) 2010 Elsevier Ireland Ltd. All rights reserved. | |||
PMID 20171777 | |||
==2007== | |||
===The Black-White disparity in pregnancy-related mortality from 5 conditions: differences in prevalence and case-fatality rates=== | ===The Black-White disparity in pregnancy-related mortality from 5 conditions: differences in prevalence and case-fatality rates=== | ||
Revision as of 13:21, 16 January 2012
| About Discussion Pages |
|---|
On this website the Discussion Tab or "talk pages" for a topic has been used for several purposes:
Glossary Links
Cite this page: Hill, M.A. (2024, May 2) Embryology Placenta - Abnormalities. Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/Talk:Placenta_-_Abnormalities |
2010
Recurrent hydatidiform moles
Eur J Obstet Gynecol Reprod Biol. 2010 May;150(1):3-7. Epub 2010 Feb 19.
Williams D, Hodgetts V, Gupta J. Source Department of Clinical Genetics, Birmingham Women's Hospital, Edgbaston, Birmingham B15 2TG, United Kingdom. Abstract Hydatidiform moles (HMs) are abnormal conceptions of excessive trophoblast development resulting in abnormal human pregnancies with no embryo and cystic degeneration of the chorionic villi. Prompt diagnosis, treatment and follow-up of patients using assays for betahCG from centres that specialise in this condition enable early diagnosis of potential malignant change. Hydatidiform moles occur quite frequently and although recurrence is rare, women who have experienced one molar pregnancy should be aware that they are at an increased risk of a further molar pregnancy in comparison to other women in the general population. For some women multiple molar pregnancies occur. In these women the recurrent molar pregnancies may be non-familial, referred to as recurrent molar hydatidiform moles in this article, or may result from an inherited predisposition, which we refer to as familial recurrent hydatidiform moles. We use the term familial biparental hydatidiform moles (FBHMs) for cases in which the parental contribution to the moles has been investigated and found to be biparental. It is important to recognise, however, that in some apparently non-familial cases, the absence of female siblings, or the absence of female siblings who have tried to conceive, may not allow the inherited nature of the molar pregnancies to manifest in more than one woman and be obviously familial. This review considers our current understanding about the aetiology of HMs and explores the mechanisms of both types of recurrent hydatidiform moles. It highlights the role that genetics can play in determining the origin of multiple molar pregnancies, which should be considered essential in providing women with accurate advice about their risk of recurrence, so allowing them to make appropriate reproductive choices. Copyright (c) 2010 Elsevier Ireland Ltd. All rights reserved.
PMID 20171777
2007
Tucker MJ, Berg CJ, Callaghan WM, Hsia J.
Division of Reproductive Health, National Center for Chronic Disease Prevention and Health Promotion, Centers for Disease Control and Prevention, Atlanta, Ga 30341-3724, USA. Comment in:
Am J Public Health. 2007 Sep;97(9):1541; author reply 1541. Abstract OBJECTIVES: We sought to determine whether differences in the prevalences of 5 specific pregnancy complications or differences in case fatality rates for those complications explained the disproportionate risk of pregnancy-related mortality for Black women compared with White women in the United States. METHODS: We used national data sets to calculate prevalence and case-fatality rates among Black and White women for preeclampsia, eclampsia, abruptio placentae, placenta previa, and postpartum hemorrhage for the years 1988 to 1999. RESULTS: Black women did not have significantly greater prevalence rates than White women. However, Black women with these conditions were 2 to 3 times more likely to die from them than were White women. CONCLUSIONS: Higher pregnancy-related mortality among Black women from preeclampsia, eclampsia, abruptio placentae, placenta previa, and postpartum hemorrhage is largely attributable to higher case-fatality rates. Reductions in case-fatality rates may be made by defining more precisely the mechanisms that affect complication severity and risk of death, including complex interactions of biology and health services, and then applying this knowledge in designing interventions that improve pregnancy-related outcomes.
Fetal environment
Indian J Radiol Imaging. 2008 Nov;18(4):326-44.
Kinare A.
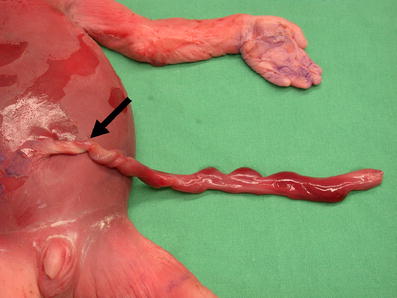
Department of Ultrasound, K.E.M. Hospital, Jehangir Hospital, Pune, India. Abstract The intrauterine environment has a strong influence on pregnancy outcome. The placenta and the umbilical cord together form the main supply line of the fetus. Amniotic fluid also serves important functions. These three main components decide whether there will be an uneventful pregnancy and the successful birth of a healthy baby. An insult to the intrauterine environment has an impact on the programming of the fetus, which can become evident in later life, mainly in the form of cardiovascular diseases, diabetes, and certain learning disabilities. The past two decades have witnessed major contributions from researchers in this field, who have included ultrasonologists, epidemiologists, neonatologists, and pediatricians. Besides being responsible for these delayed postnatal effects, abnormalities of the placenta, umbilical cord, and amniotic fluid also have associations with structural and chromosomal disorders. Population and race also influence pregnancy outcomes to some extent in certain situations. USG is the most sensitive imaging tool currently available for evaluation of these factors and can offer considerable information in this area. This article aims at reviewing the USG-related developments in this area and the anatomy, physiology, and various pathologies of the placenta, umbilical cord, and the amniotic fluid.
PMID: 19774194 http://www.ncbi.nlm.nih.gov/pubmed/19774194
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2747450/?tool=pubmed
(good placental abnormalities ultrasound images)