Genital Abnormality - Hypospadia: Difference between revisions
mNo edit summary |
mNo edit summary |
||
| Line 1: | Line 1: | ||
{{Header}} | {{Header}} | ||
==Introduction== | ==Introduction== | ||
[[File:Hypospadia classifications.jpg|thumb|400px|Classification of Hypospadias{{#pmid:11713004|PMID11713004}}]] | |||
Hypospadias are the most common penis abnormality (1 in 300) and result from a failure of male urogenital folds to fuse in various regions, the normal process is described as virilization of the external genitalia. This in turn leads to resulting in a proximally displaced urethral meatus or opening. | Hypospadias are the most common penis abnormality (1 in 300) and result from a failure of male urogenital folds to fuse in various regions, the normal process is described as virilization of the external genitalia. This in turn leads to resulting in a proximally displaced urethral meatus or opening. | ||
The cause is unknown, but suggested to involve many factors either indivdually or in combination including: familial inheritance, low birth weight, assisted reproductive technology, advanced maternal age, paternal subfertility and endocrine-disrupting chemicals. | The cause is unknown, but suggested to involve many factors either indivdually or in combination including: familial inheritance, low birth weight, assisted reproductive technology, advanced maternal age, paternal subfertility and endocrine-disrupting chemicals.{{#pmid:11713004|PMID11713004}} Infants with hypospadias should not undergo circumcision. | ||
| Line 33: | Line 34: | ||
|} | |} | ||
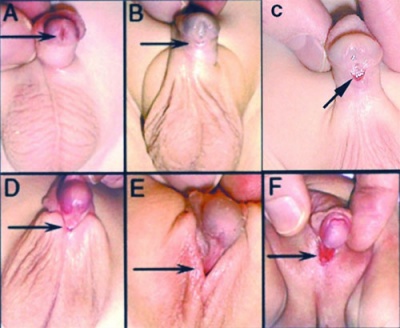
==Hypospadia Classification== | ==Hypospadia Classification== | ||
[[File:Hypospadia classifications.jpg|thumb|400px|Classification of Hypospadias | [[File:Hypospadia classifications.jpg|thumb|400px|Classification of Hypospadias{{#pmid:11713004|PMID11713004}}]] | ||
The condition is classified by the general location of the relocated opening (meatus) and lack of fusion. | The condition is classified by the general location of the relocated opening (meatus) and lack of fusion. | ||
Revision as of 11:18, 11 April 2018
| Embryology - 1 May 2024 |
|---|
| Google Translate - select your language from the list shown below (this will open a new external page) |
|
العربية | català | 中文 | 中國傳統的 | français | Deutsche | עִברִית | हिंदी | bahasa Indonesia | italiano | 日本語 | 한국어 | မြန်မာ | Pilipino | Polskie | português | ਪੰਜਾਬੀ ਦੇ | Română | русский | Español | Swahili | Svensk | ไทย | Türkçe | اردو | ייִדיש | Tiếng Việt These external translations are automated and may not be accurate. (More? About Translations) |
Introduction
Hypospadias are the most common penis abnormality (1 in 300) and result from a failure of male urogenital folds to fuse in various regions, the normal process is described as virilization of the external genitalia. This in turn leads to resulting in a proximally displaced urethral meatus or opening.
The cause is unknown, but suggested to involve many factors either indivdually or in combination including: familial inheritance, low birth weight, assisted reproductive technology, advanced maternal age, paternal subfertility and endocrine-disrupting chemicals.[1] Infants with hypospadias should not undergo circumcision.
Some Recent Findings
|
| More recent papers |
|---|
|
This table allows an automated computer search of the external PubMed database using the listed "Search term" text link.
More? References | Discussion Page | Journal Searches | 2019 References | 2020 References Search term: Hypospadia <pubmed limit=5>Hypospadia</pubmed> |
Hypospadia Classification
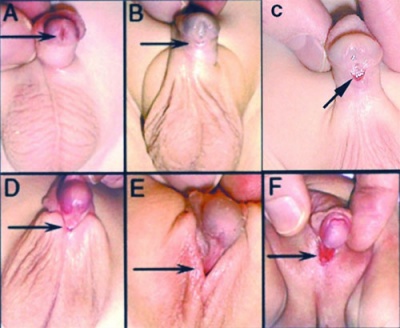
The condition is classified by the general location of the relocated opening (meatus) and lack of fusion.
Template:Hypospadia Classification Table
Ultrasound
Penoscrotal Hypospadia 3D Ultrasound[6]
Ultrasonography in rendering mode, at GA 33 weeks, with short penis and with evidence of testicles inside a bifid scrotum.
- Links: Ultrasound
Surgical Repair
Depending on the class of hypospadias there are a number of different surgical repair techniques including: orthoplasty or penile straightening, urethroplasty, meatoplasty and glanuloplasty, scrotoplasty (oscheoplasty) and skin coverage.
Maternal Factors
Data from a case-control study in Sweden and Denmark (2000 - 2005) identified a number of maternal factors that may be associated with hypospadias.[7]
- Maternal diet during pregnancy lacking both fish and meat - more than 4-fold increased risk
- Maternal obesity - more than 2-fold increased risk
- Maternal hypertension - 2.0-fold increased risk
- Maternal absence of nausea - 1.8-fold increased risk
- Maternal nausea in late pregnancy - also appeared to be positively associated with increased risk
Molecular Factors
- chromosomal abnormalities
- HOX, FGF, Shh - genes of penile development
- WT1, SRY - testicular determination
- luteinizing hormone (LH) receptor
- 5alpha reductase, androgen receptor - action of androgen
- CXorf6
- ATF3
Links: OMIM - CXorf6
Related Genetic Conditions
- X-linked isolated hypospadias-1 HYSP1 OMIM 300633
- X-linked isolated hypospadias-2 HYSP2 OMIM 300758
- X-linked isolated hypospadias-3 HYSP3 OMIM 146450
- Johanson-Blizzard syndrome[8] - hypospadias, failure to thrive, exocrine pancreatic deficiency, short stature and developmental delay, cutis aplasia on the scalp, aplasia of alae nasi, hypothyroidism, myxomatous mitral valve, and patent ductus arteriosus.
References
- ↑ 1.0 1.1 1.2 Baskin LS, Himes K & Colborn T. (2001). Hypospadias and endocrine disruption: is there a connection?. Environ. Health Perspect. , 109, 1175-83. PMID: 11713004
- ↑ George M, Schneuer FJ, Jamieson SE & Holland AJ. (2015). Genetic and environmental factors in the aetiology of hypospadias. Pediatr. Surg. Int. , 31, 519-27. PMID: 25742936 DOI.
- ↑ Fujimoto T, Suwa T, Kabe K, Adachi T, Nakabayashi M & Amamiya T. (2008). Placental insufficiency in early gestation is associated with hypospadias. J. Pediatr. Surg. , 43, 358-61. PMID: 18280290 DOI.
- ↑ Kutlay R, Isik D, Ercel C, Anlatici R & Isik Y. (2010). A new technique for correction of distal penile hypospadias. Ann Plast Surg , 65, 66-9. PMID: 20548222 DOI.
- ↑ Seibold J, Werther M, Alloussi S, Gakis G, Schilling D, Colleselli D, Stenzl A & Schwentner C. (2010). Objective long-term evaluation after distal hypospadias repair using the meatal mobilization technique. Scand. J. Urol. Nephrol. , 44, 298-303. PMID: 20450394 DOI.
- ↑ Rios LT, Araujo Júnior E, Nardozza LM, Rolo LC, Hatanaka AR, Moron AF & Martins Mda G. (2012). Prenatal diagnosis of penoscrotal hypospadia in third trimester by two- and three-dimensional ultrasonography: a case report. Case Rep Urol , 2012, 142814. PMID: 23304621 DOI.
- ↑ Akre O, Boyd HA, Ahlgren M, Wilbrand K, Westergaard T, Hjalgrim H, Nordenskjöld A, Ekbom A & Melbye M. (2008). Maternal and gestational risk factors for hypospadias. Environ. Health Perspect. , 116, 1071-6. PMID: 18709149 DOI.
- ↑ <pubmed>20556423</pubmed>
Reviews
Cunha GR, Sinclair A, Risbridger G, Hutson J & Baskin LS. (2015). Current understanding of hypospadias: relevance of animal models. Nat Rev Urol , 12, 271-80. PMID: 25850792 DOI.
Carmichael SL, Shaw GM & Lammer EJ. (2012). Environmental and genetic contributors to hypospadias: a review of the epidemiologic evidence. Birth Defects Res. Part A Clin. Mol. Teratol. , 94, 499-510. PMID: 22678668 DOI.
van der Zanden LF, van Rooij IA, Feitz WF, Franke B, Knoers NV & Roeleveld N. (2012). Aetiology of hypospadias: a systematic review of genes and environment. Hum. Reprod. Update , 18, 260-83. PMID: 22371315 DOI.
Articles
McNamara ER, Schaeffer AJ, Logvinenko T, Seager C, Rosoklija I, Nelson CP, Retik AB, Diamond DA & Cendron M. (2015). Management of Proximal Hypospadias with 2-Stage Repair: 20-Year Experience. J. Urol. , 194, 1080-5. PMID: 25963188 DOI.
Search Pubmed
June 2010 "Hypospadia" All (4698) Review (377) Free Full Text (413)
Search Pubmed: Hypospadia | Hypospadia Surgical Repair
External Links
External Links Notice - The dynamic nature of the internet may mean that some of these listed links may no longer function. If the link no longer works search the web with the link text or name. Links to any external commercial sites are provided for information purposes only and should never be considered an endorsement. UNSW Embryology is provided as an educational resource with no clinical information or commercial affiliation.
Glossary Links
- Glossary: A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | Numbers | Symbols | Term Link
Cite this page: Hill, M.A. (2024, May 1) Embryology Genital Abnormality - Hypospadia. Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/Genital_Abnormality_-_Hypospadia
- © Dr Mark Hill 2024, UNSW Embryology ISBN: 978 0 7334 2609 4 - UNSW CRICOS Provider Code No. 00098G