2010 Group Project 2: Difference between revisions
| Line 104: | Line 104: | ||
[[File:Polydactyly.jpg|left|200 px]] | [[File:Polydactyly.jpg|left|200 px]] | ||
'''Polydactyly''' is a congenital condition where an extra digit is formed. Mostly it occurs on only one hand or foot, but sometimes can occur on all limbs. The extra digit is mostly a small non-function appendage of skin, less often it is an extension of the adjacent digit, and rarely it is a fully functioning finger that arises from the wrist or ankle joint like the other digits. Polydactyly can be described as | '''Polydactyly''' is a congenital condition where an extra digit is formed. Mostly it occurs on only one hand or foot, but sometimes can occur on all limbs. The extra digit is mostly a small non-function appendage of skin, less often it is an extension of the adjacent digit, and rarely it is a fully functioning finger that arises from the wrist or ankle joint like the other digits. Polydactyly can be described as | ||
-postaxial polydactyly (arising from the little finger) | -postaxial polydactyly (arising from the little finger) | ||
-preaxial polydactyly (arising from the thumb) or | -preaxial polydactyly (arising from the thumb) or | ||
-central polydactyly (arising from anywhere between the other digits) | -central polydactyly (arising from anywhere between the other digits) | ||
Polydactyly is seen in 1 in every 500 births, but the extra digit is usually surgically removed shortly after birth | Polydactyly is seen in 1 in every 500 births, but the extra digit is usually surgically removed shortly after birth | ||
Revision as of 20:32, 14 September 2010
Chorionic Villus Sampling (CVS)
Introduction
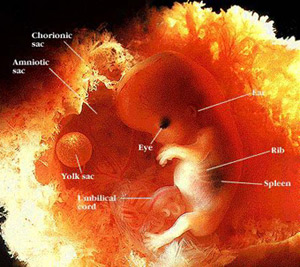
Chorionic villus sampling or CVS is a type of prenatal diagnosis test performed in the first trimester to detect major fetal abnormalities. In the procedure, tissue is withdrawn from the villi of the chorion and tested for chromosomal defects. It is usually done in women over the age of 37 as the chance of chromosomal defects increase with the mothers age. CVS is a specific test for particular abnormalities, such as Down Syndrome or Cystic Fibrosis. It is commonly performed between 10 and 12 weeks of pregnancy.
The advantage of CVS over other procedures is that the result is available approx 6 weeks earlier in the pregnancy, so if a termination is needed, it can be done earlier which is much safer, rather than later in the pregnancy. [1]
Why would you use CVS over other techniques?
ADVANTAGES
- Can be performed earlier in pregnancy than amniocentesis (at around ten weeks).
- Results are available faster
- Cells obtained are mitotically active
- Amount of tissue obtained is preferable for DNA analysis.
- It is almost 100% reliable in detecting chromosomal and genetic defects.
DISADVANTAGES
- It carries a slightly higher risk of miscarriage (1%-2%) than does amniocentesis
- It's less commonly available than amniocentesis, and fewer doctors are experienced in the procedure.
- It entails a greater risk of distorted results than does amniocentesis due to presence of mother's cells in the sample and discrepancies between chorionic villi and fetal genes.
- Metabolic disorders are difficult to diagnose and must be confirmed with amniocentesis.
- Because of the early gestational age at which the test is performed, fetal anatomy cannot be seen as well as it can at the time amniocentesis is performed.
Historic background
Brief timeline of CVS use
- 1968 - Mohr in Scandinavia introduced the concept of prenatal diagnosis using chorionic villi sampling
- 1973 - Kullander and Sandahl and Hahnemann in 1974 showed further study into chromosomal analysis from CVS
- 1975 - from the Department of Obstetrics and Gynaecology at the Tietung Hospital in Anshan, China was successful in using CVS to determine sex of fetuses for sex pre selection.
- 1980 - Kazy et al. were the first to use ultrasound guidance during chorionic villi sampling.
- 1981 - Niazi et al. improved methods for culturing of fibroblasts from trophoblast villi.
- 1983 - Ward performed transcervical CVS with 67% success rate. In the same year, the Brombati group demonstrated and 96% success rate with obtaining villi with the aid of ultrasound guidance
- 1984 - Smidt-Jensen and Hahnemann introduced transabdominal CVS under ultrasound guidance
- 1986 - The Golbus group had a 3.8% miscarriage rate, and subsequently many other clinics started reporting a much lower rate of miscarriage at 1.7% making the procedure safe for routine use
Jan Mohr (1921-2009)
1968 -- Concept of CVS introduced
In 1968 Jan Mohr introduced the concept of prenatal diagnosis using the CVS technique.[3] He used the transcervical method to get a biopsy of the chorion using an endoscope as the source of vision. The current technique differs by using mostly transabdominal access with ultrasound instead of an endoscope. He reported a 96% success rate in obtaining chorionic material but with a high incidence of bleeding and infection. The approach was abandoned as amniocentesis became more popular due to higher safety levels
1973-1975 -- Further study into chromosomal analysis from CVS
Kullander and Sandahl in 1973 and Hahnemann in 1974 further researched fetal chromosome analysis using transcervical biopsy before termination in early pregnancies. [4] In 1975 the first successful diagnostic use of chorionic villi was reported at the Tietung Hospital in China. [5] This is where fetal sex was diagnosed for the purpose of sex pre-selection. They claimed to have 94% diagnosis success and only 4% miscarriage rate. Researchers in the United States were, however unable to duplicate the results and so the idea of CVS diagnosis was again abandoned for some time.
1980-1983 -- Change from endoscopic examination to ultrasound to guide CVS
With the invention of the ultrasound and advancement in molecular genetics, an earlier prenatal diagnosis was now sought after. So Kazy et al. in 1980, began using both the endoscope and the ultrasound for fetal sexing on chorion biopsies. This was the first report of using ultrasound guidance during chorion sampling. After Kazy et.al. began using the ultrasound for guidance, many others followed. Niazi et al., Ward and the Brombati group all started using ultrasound guided CVS. Techniques quickly improved and success rate of obtaining chorionic material rose from 75% to 96% [6]
1984-1986 -- The introduction of transabdominal CVS
In 1984, Smidt-Jensen and Hahnemann in Copenhagen introduced transabdominal CVS using ultrasound guidance.[7] With less chance of infective complications the procedure has become more popular than the transcervical method in many prenatal diagnostic centers. Other ultrasonic techniques and modifications were explored by the Brambati and Simoni group and the Golbus group in 1985. [8] The Golbus group reported in 1986 a miscarriage rate of 3.8%.[9] Subsequently, many other centres reported a much lower miscarriage rate of 1.5% which made the procedure safe for routine use.
Current associated research
Chorionic Villus Sampling (CVS) is one of many prenatal diagnostic tools for expectant mothers, it is popular since it can be used to identify potential problems with a fetus at a very early stage. However, the procedure does carry some risks, as does any invasive diagnostic procedure. As chorionic villus sampling is a relatively new technique, made available for safe routine use only 20 years ago, the current associated research is mainly associated with risks associated with the procedure, and ways to overcome these risks. The next section in this page will discuss the current research on CVS and the risks involved.
Hypertensive disorders of pregnancy
Pregnancy induced hypertension is a condition that can occur during and after the 20th week of pregnancy. The types of hypertensive disorders can include:
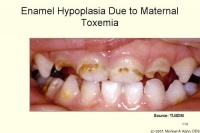
- Pre-eclampsia or toxemia – Characterised as high blood pressure above 140/90 with proteinuria (protein in the urine that is above 300mg)
- Eclampsia - Developed in a pregnant woman who has had pre-eclampsia and is characterised by seizures
- Gestational hypertension – arterial hypertension that occurs after the 20th week of gestation
If untreated, the condition may develop into HELLP syndrome which is a serious complication noted by hemolytic aneamia, elevated liver enzymes and a low platelet count.
There has been conflicting evidence in literature that suggests that CVS is associated with hypertensive disorders in pregnancy such as pre-clampsia and gestational hypertension. In several studies, such as data from the National Institute of Health that compared late CVS procedures with early amniocentesis, showed a higher rite of gestational hypertension and preeclampsia in pregnant mothers.[10] (5.4% for mothers who had CVS and 3.5% that had amniocentesis.) It was hypothesized that disruption and disturbance of the placenta at 13-14 weeks may increase the risk of maternal hypertension. In addition, another recent study in 2006 also reported that there was an increase in the rate of pre-clampsia in first-time expectant mothers who have had CVS.[11]
However, in a very recent data investigation of among 9098 women that were pregnant between 1990 and 2006, the overall incidence of hypertensive disorders with women who have had CVS was 2.7% compared to the control group that did not have the procedure done which was 7.1%.[12] Similarly, in a study conducted by The American College of Obstetricians and Gynecologists,[13] 31, 138 women were that were included in the investigation showed that 2.2% developed preeclampsia and 2.8% developed gestation hypertension. Only 7.8% of those individuals had previously had CVS procedure performed.
Although it can be said that some woman may develop hypertensive disorders during pregnancy that have also had the CVS procedure done in the past, there is no conclusive evidence so far that definitively associates CVS with hypertensive disorders such as pre-clampsia and gestation hypertension.
Malformations
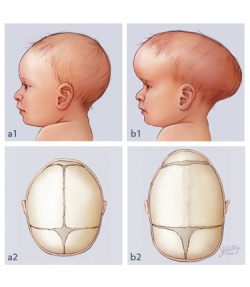
Many malformations were thought to be a result of more invasive prenatal diagnostic techniques such as chorionic villus sampling. These malformations include, but are not limited to, cardiac malformations, hypospadias, craniosynostosis, pyloric stenosis, inguinal hernia, polydactyly, syndactyly, hydrocephalus and cleft lip and palate. Although these studies have now confirmed no known relationship with CVS, we will mention some below. [14]
Craniosynostosis is a condition where one of the sutures of the skull prematurely fuses, this causes the other sutures to compensate in growth for the fused suture. In normal development of the skull, the sutures allow for brain growth, so if one suture fuses prematurely, the brain can not grow normally, and the other sutures over expand in compensation. In the shown image, pictures a1 and a2 show the normal development and fusing of the infant skull. b2 shows how a suture is prematurely fused and b1 shows how the abnormality shows in an infant child.
Craniosyntosis may result in increased pressure on the brain and developmental delays. Treatment of craniosynostosis usually consists of surgery to the skull where a zigzag incision is made to make the hair look more natural than the scar left by a straight incision. The surgery separates the sutures that have joined together to allow the head to develop normally.
Polydactyly is a congenital condition where an extra digit is formed. Mostly it occurs on only one hand or foot, but sometimes can occur on all limbs. The extra digit is mostly a small non-function appendage of skin, less often it is an extension of the adjacent digit, and rarely it is a fully functioning finger that arises from the wrist or ankle joint like the other digits. Polydactyly can be described as
-postaxial polydactyly (arising from the little finger)
-preaxial polydactyly (arising from the thumb) or
-central polydactyly (arising from anywhere between the other digits)
Polydactyly is seen in 1 in every 500 births, but the extra digit is usually surgically removed shortly after birth
Syndactyly
Hemangiomas
A hemangioma is a benign tumour growth of endothelial cells that can occur in newborns and infants. Hemangiomas can occur anywhere in the body but are often localised on the skin of the face and neck, and are characterised by a red to reddish purple raised lesion on the skin, similarly to a "strawberry" like appearance. Its red appearance is due to the newly formed blood vessels, which result from the malformation of angioblastic tissues of fetal life.[16] Most hemangiomas do not cause any serious complications, and regress later on in life, where 90% of hemangiomas in children would disappear by the age of 9.
Recently, research has linked the increase in the incidence of hemangiomas in infants following CVS. It has been postulated that the mechanism of hemangioma formation is associated with the embolisation of angioblasts or endothelial cells from the placenta to the fetal skin.[17] Although this may link hemangiomas to placental origin, it is unclear how, or whether CVS directly interferes or enhances the formation of these lesions. However, a recent study that compared the effects of CVS and amniocentesis on the prevalence of hemangiomas in infants showed that 27% of the study group had hemangiomas with CVS compared to 9.4% in children with hemangiomas and amniocentesis. [18] Furthermore, in an previous study conducted in 1995, there was a threefold increase in incidence after trancervical procedure was done, compared to amniocentesis.[19][20]
Risks
When Chorionic Villus Sampling is performed, a small sample of the placenta is removed for analysis. The placenta contains fetal material, therefore can reveal genetic defects which may lead to problems or abnormalities. [21] This prenatal test can be performed as early as 11 weeks into the pregnancy, this is earlier than many prenatal diagnosis tests, which is why many parents choose CVS as they can have solid information earlier in the pregnancy. Some common risks which are not under current research include: Cramping, light blood spotting, pain, fever and chills, leakage (which can be a major concern as it can lower amniotic fluid to a dangerous level for the infant), and potential for missing fingers and toes in the newborn. For this reason, the procedure is only recommended for women who are at least 11 weeks pregnant. [22] The other major risks that are currently being researched are outlined below
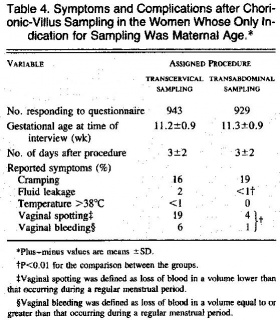
Transabdominal vs Transcervical CVS. Comparison of risks
This table shows the symptoms of women approximately 3 days after sampling. The table shows women who had undergone transcervical sampling had higher frequencies of fluid leakage, vaginal spotting, and bleeding. When a tenaculum is not used, the frequency of vaginal spotting and bleeding persisted in the transcervical-sampling group. Only two women, both in the transcervical-sampling group, had a temperature above 38°C. [23]
Miscarriage
One of the biggest risks of Chorionic Villus Sampling is miscarriage. In one to 100 or 200 cases, the procedure is linked with miscarriage. [24] In an experienced clinic, this rate may go down to one in 300 to 400. To lower the risk of miscarriage with Chorionic Villus Sampling, it is recommended the procedure be performed by an experienced clinician
Oligohydramnios
Oligohydramnios is a condition due to low amniotic fluid level, which is caused by amniotic fluid leakage. Amniotic fluid leakage is typically caused by fetal urinary tract abnormalities such as Potter's syndrome, polycystic kidneys, or genitourinary obstruction. But leakage can sometimes be caused by sampling of the chorionic villi due to insertion of the needle. If the resulting oligohydramnios is not treated and the amniotic fluid continues to leak it can result in the baby developing hypoplastic lungs (underdeveloped lungs). [25]
Description of technique
CVS can be performed in two ways, through the cervix (transcervical) or through the abdomen (transabdominal). Both techniques are equally safe when performed by an experienced technician, however miscarriage rates are somewhat higher when done through the cervix. Prior to the procedure, an abdominal ultrasound can be performed to locate the position of the uterus, and the placenta. A full bladder is not required. Depending on the type of method performed, the vulva, vagina, cervix or abdomen are cleaned with antiseptic. The procedure normally takes only 1-2 minutes to perform and the patient is able to leave the clinic within the hour after the fetus is checked.[26]
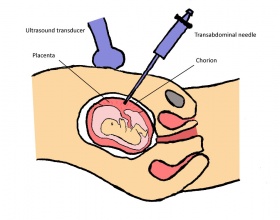
Transabdominal Procedure
- A local anaesthetic is first applied to the abdomen.
- A thin hollow needle is then inserted through the abdomen into the uterus and into the edge of the placenta where the chorion is located. An ultrasound transducer is commonly used to guide the needle during the procedure.
- A finer syringe needle is then passed through the outer needle, and the tissue is then drawn.
- The sample is taken to the laboratory for testing.
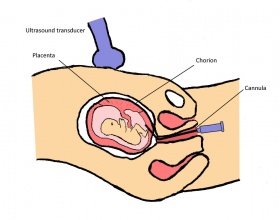
Transcervical Procedure
- A speculum is inserted in the vagina and the area is cleaned with antiseptic.
- With the help of ultrasound imaging, a thin cannula is then inserted through the cervix and uterus and into the placenta.
- The tissue sample is then taken up through the cannula.
After the sample is taken to the laboratory, the cells are grown until there are enough cells for chromosome testing. The results normally take up to 2 weeks to complete.
Complications
Some of the side effects and complications after a CVS procedure can include:
- Dizziness
- Abdominal discomfort
- Cramping
- Haemorrhage
- Infection
- Ruptured amniotic sac
- Increased risk of limb defects if the test was performed at nine weeks’ gestation or earlier
Additional complications can involve technical errors such as failure of the specimen to grow sufficiently in the laboratory and uncertain laboratory results. If this occurs, amniocentesis is still an option after 15 weeks.
Results and Accuracy
The accuracy of CVS to detect chromosome abnormalities is quite high, at around 98-99%. Comparitively to amniocentesis, CVS does NOT detect neural tube defects such as spina bifida, or anacephaly. The type of chromosome abnormalities detected by CVS will be further discussed in detail below.
Abnormalities found by CVS prenatal diagnostic technique
The cells collected by CVS are sent to a cytogenetics laboratory. There the cells are cultured (stimulated to grow and divide) for 10-14 days. After enough cells are obtained, a banded karyotype is performed. This means that the fetal chromosomes in the cultured cells are stained and subsequently photographed. The photographed chromosomes are then ordered by number, counted and checked for structural abnormalities. There should be 46 chromosomes, 23 pairs. A boy's karyotype is described as 46,XY and a girl's karyotype is described as 46,XX.[28]
| Disorder | Cause | Comments | Frequency |
|---|---|---|---|
| Down Syndrome | A third copy of chromosome 21 | The average IQ of children with Down syndrome is around 50, compared to normal children with an IQ of 100. Complications for people with down syndrome include: congenital heart defects, gastroesophageal reflux disease, recurrent ear infections, obstructive sleep apnea, and thyroid dysfunctions. [29] | Approximately 1 in 1,000 births [30] |
| Trisomy 13 | A third copy of chromosome 13 | Also called Patau syndrome. This abnormality causes mental and motor abnormalities, polydactyly (extra digits), kidney defects, abnormal genitalia and heart defects, among many others. [31] | Less than 1% |
| Trisomy 18 | A third copy of chromosome 18 | Also known as Edwards syndrome. It has a very low survival rate, due to: kidney and heart defects, intestines protruding outside the body, mental abnormalities, growth disorders, feeding and breathing difficulties. [32] | 1 in 3,000 conceptions and approximately 1 in 6,000 live births |
| Cystic Fibrosis | A mutation in the gene cystic fibrosis transmembrane conductance regulator (CFTR) in chromosome 7. | An autosomal recessive disease that causes excessive sticky mucous to form on mucosal surfaces effecting the digestive and respiratory organs. [33] | Approx 1 in 3,000 |
| Hemoglobinopathy | Structural abnormalities in the globin proteins | Multiple types of abnormal haemoglobins exist including Haemoglobin S, C E and D that alter the structure of these proteins. A common defect is sickle celldisease.[34] | Hemoglobinopathies are a genetic defect and therefore an inherited disorder, frequency depends on which particular hemoglobinopathy is being discussed, eg. in the case of Sickle cell disease, it is estimated that 7% of worlds population are carriers |
| Tay Sachs Disease | mutations on chromosome 15 in the HEXA gene | It is a rare autosomal recessive defect inherited from parents that are carriers for the disease. Affected individuals suffer from premature nerve cells death in the brain. [35] | Approx 1 in 300 are carriers |
Useful links
Search Bookshelf Chorionic villus sampling
Search Pubmed Now: Chorionic villus sampling
References
- ↑ Rhoads, G.G., Jackson, L.G., Schlesselman, S.E., de, l.C., Desnick, R.J., Golbus, M.S., Ledbetter, D.H., Lubs, H.A., Mahoney, M.J., Pergament, E., Simpson, J.L., Carpenter, R.J., Elias, S., Ginsberg, N.A., Goldberg, J.D., Hobbins, J.C., Lynch, L., Shiono, P.H., Wapner, R.J. & Zachary, J.M. 1989, "The Safety and Efficacy of Chorionic Villus Sampling for Early Prenatal Diagnosis of Cytogenetic Abnormalities", New England Journal of Medicine, vol. 320, no. 10, pp. 609-617.
- ↑ Malone, F.D., Canick, J.A., Ball, R.H., Nyberg, D.A., Comstock, C.H., Bukowski, R., Berkowitz, R.L., Gross, S.J., Dugoff, L., Craigo, S.D., Timor-Tritsch, I., Carr, S.R., Wolfe, H.M., Dukes, K., Bianchi, D.W., Rudnicka, A.R., Hackshaw, A.K., Lambert-Messerlian, G., Wald, N.J. & D'Alton, M.E. 2005, "First-Trimester or Second-Trimester Screening, or Both, for Down's Syndrome", New England Journal of Medicine, vol. 353, no. 19, pp. 2001-2011.
- ↑ <pubmed>5691288</pubmed>
- ↑ <pubmed>4766093</pubmed>
- ↑ <pubmed>811431</pubmed>
- ↑ <pubmed>7208019</pubmed>
- ↑ <pubmed>6463023</pubmed>
- ↑ <pubmed>4088973</pubmed>
- ↑ <pubmed>3717235</pubmed>
- ↑ <pubmed>15738029</pubmed>
- ↑ <pubmed>19455602</pubmed>
- ↑ <pubmed>19918960</pubmed>
- ↑ <pubmed>20664398</pubmed>
- ↑ <pubmed>7937577</pubmed>
- ↑ Silver, R.K., Macgregor, S.N., Muhlbach, L.H., Knutel, T.A. & Kambich, M.P. 1994, "Congenital malformations subsequent to chorionic villus sampling: Outcome analysis of 1048 consecutive procedures", Prenatal diagnosis, vol. 14, no. 6, pp. 421-427.
- ↑ <pubmed>7063565</pubmed>
- ↑ <pubmed>19218861</pubmed>
- ↑ <pubmed>20824891</pubmed>
- ↑ Lo, K., Mihm, M. & Fay, A. 2009, "Current Theories on the Pathogenesis of Infantile Hemangioma", Seminars in ophthalmology, vol. 24, no. 3, pp. 172-177.
- ↑ <pubmed>7784377</pubmed>
- ↑ <pubmed>20664398</pubmed>
- ↑ <pubmed>20051662</pubmed>
- ↑ Jackson, L.G., Zachary, J.M., Fowler, S.E., Desnick, R.J., Golbus, M.S., Ledbetter, D.H., Mahoney, M.J., Pergament, E., Simpson, J.L., Black, S. & Wapner, R.J. 1992, "A Randomized Comparison of Transcervical and Transabdominal Chorionic-Villus Sampling", New England Journal of Medicine, vol. 327, no. 9, pp. 594-598.
- ↑ <pubmed>19155918</pubmed>
- ↑ <pubmed>17694578</pubmed>
- ↑ Melbourne Ultrasound for Women. Chorionic Villus Sampling. Accessed 5 September 2010. http://www.nevdgp.org.au/info/melb_us/cvs_melb.htm
- ↑ <pubmed>20154617</pubmed>
- ↑ Rhoads, G.G., Jackson, L.G., Schlesselman, S.E., de, l.C., Desnick, R.J., Golbus, M.S., Ledbetter, D.H., Lubs, H.A., Mahoney, M.J., Pergament, E., Simpson, J.L., Carpenter, R.J., Elias, S., Ginsberg, N.A., Goldberg, J.D., Hobbins, J.C., Lynch, L., Shiono, P.H., Wapner, R.J. & Zachary, J.M. 1989, "The Safety and Efficacy of Chorionic Villus Sampling for Early Prenatal Diagnosis of Cytogenetic Abnormalities", New England Journal of Medicine, vol. 320, no. 10, pp. 609-617.
- ↑ Malone, F.D., Canick, J.A., Ball, R.H., Nyberg, D.A., Comstock, C.H., Bukowski, R., Berkowitz, R.L., Gross, S.J., Dugoff, L., Craigo, S.D., Timor-Tritsch, I., Carr, S.R., Wolfe, H.M., Dukes, K., Bianchi, D.W., Rudnicka, A.R., Hackshaw, A.K., Lambert-Messerlian, G., Wald, N.J. & D'Alton, M.E. 2005, "First-Trimester or Second-Trimester Screening, or Both, for Down's Syndrome", New England Journal of Medicine, vol. 353, no. 19, pp. 2001-2011.
- ↑ Malone, F.D., Canick, J.A., Ball, R.H., Nyberg, D.A., Comstock, C.H., Bukowski, R., Berkowitz, R.L., Gross, S.J., Dugoff, L., Craigo, S.D., Timor-Tritsch, I., Carr, S.R., Wolfe, H.M., Dukes, K., Bianchi, D.W., Rudnicka, A.R., Hackshaw, A.K., Lambert-Messerlian, G., Wald, N.J. & D'Alton, M.E. 2005, "First-Trimester or Second-Trimester Screening, or Both, for Down's Syndrome", New England Journal of Medicine, vol. 353, no. 19, pp. 2001-2011.
- ↑ Driscoll, D.A. & Gross, S. 2009, "Prenatal Screening for Aneuploidy", New England Journal of Medicine, vol. 360, no. 24, pp. 2556-2562.
- ↑ Driscoll, D.A. & Gross, S. 2009, "Prenatal Screening for Aneuploidy", New England Journal of Medicine, vol. 360, no. 24, pp. 2556-2562.
- ↑ Levison, J.H., Barbieri, R.L., Katz, J.T. & Loscalzo, J. 2010, "Hard to Conceive", New England Journal of Medicine, vol. 363, no. 10, pp. 965-970.
- ↑ Abboud, M.R. 2009, "Hematopoietic Stem-Cell Transplantation for Adults with Sickle Cell Disease", New England Journal of Medicine, vol. 361, no. 24, pp. 2380-2381.
- ↑ <pubmed>20100466</pubmed>
Glossary
Amniocentesis - A prenatal diagnostic test involving sampling of amniotic fluid by needle aspiration for genetic analysis.
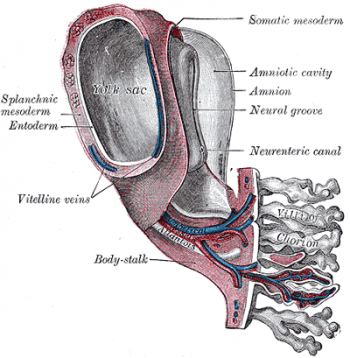
Amnion - An extraembryonic membrane ectoderm and extraembryonic mesoderm in origin and forms the innermost fetal membrane, produces amniotic fluid. This fluid-filled sac initially lies above the trilaminar embryo disc and with embryoic disc folding this sac is drawn ventrally to enclose (cover) the entire embryo, then fetus.
Amniotic cavity - The fluid-filled (amniotic fluid) extraembryonic coelom (cavity) formed initially by epiblast and then ectoderm and surrounding extraembryonic mesoderm. In humans, it forms the innermost fetal membrane, produces amniotic fluid expanding to fuse with the chorionic membrane during week 8 of development.
Amniotic fluid - The fluid that fills amniotic cavity totally encloses and cushions the embryo.
Chorion - The extraembryonic membrane generated from trophoblast and extraembryonic mesoderm that forms placenta. chorion and amnion are made by the somatopleure. The chorion becomes incorporated into placental development. The avian and reptilian chorion lies beside the egg shell and allows gas exchange. Chorionic villus sampling (CVS) - The taking a biopsy of the placenta, usually at the end of the second month of pregnancy, to test the fetus for genetic abnormalities.
Chromosome - double stranded DNA coiled around histones. Condenses during mitosis and meiosis.
Ectoderm - One of the initial 3 germ cell layers, which will form the nervous system from the neural tube and neural crest and also generates the entire epithelial layer of the skin covering the embryo.
Endoscope - a long slender medical instrument for examining the interior of a bodily organ or performing minor surgery
Endoderm - One of the initial 3 germ cell layers (ectoderm, mesoderm and endoderm) formed by the process of gastrulation. The endoderm forms as a cuboidal epithelium and contributes not only to the trilaminar embryo, but also lines the yolk sac. It will form the entire epithelial lining of the gastrointestinal tract (GIT), contribute to the accessory organs of GIT and also forms the epithelial lining of the respiratory tract.
Fetus - In mammals, term describes the period of development following the embryonic period. In humans, the development week 9 to 36 is the fetal stage (second and third trimester). (see fetal period above). This term is also used non-scientifically to describe the human conceptus at both embryonic and fetal stages of development.
Gene - A DNA sequence that is transcribed as a single unit and encodes a single polypeptide (protein) or a set of closely related polypeptides. There are approximately 20,000-25,000 protein encoding genes in the human genome. In each cell, DNA is found within the nucleus and also within mitochondria.
Gestation - The period of time from conception to birth. A pregnancy with multiple fetuses is referred to as a multiple gestation.
Mesoderm - The middle layer of the 3 germ cell layers of the trilaminar embryo.
Miscarriage - A general clinical term for the loss of embryo or fetus by spontaneous abortion.
Mitosis - The normal division of all cells, except germ cells, where chromosome number is maintained (diploid).
Prenatal diagnosis - any of the diagnostic procedures used to determine whether a fetus has a genetic abnormality
Tenaculum - instrument used to grasp the cervix and keep the uterus in place during gynecological procedures.
Termination - The spontaneous or artificially induced expulsion of an embryo or fetus. As used in legal context, the term usually refers to induced abortion.
Transabdominal - In the transabdominal CVS technique, the physician inserts a needle through the abdomen into the placenta. This is also done with ultrasound, to guide the physician
Transcervical - In the transcervical CVS technique, the physician inserts a small tube through the cervix into the placenta. This is done while ultrasound guides the physician
Ultrasound - A non-invasive technique for visualizing and prenatal diagnosis of several features of development including: follicles in the ovaries, the gestational sac, fetus in the uterus, fetal parameters, and the placenta. The technique uses high-frequency sound waves that are reflected off internal structures. These reflections can then be analysed and displayed by computer.
Villi - Plural of villus, which is a thin projection from a surface. A term used to describe the many functional units together of the fetal placenta.
Vitelline arteries and veins - The blood vessels which form in the extraembryonic mesoderm of the yolk sac and anastomose are called vitelline arteries (flow away from the embryo) and vitelline veins (flow toward the embryo).
Prenatal Diagnosis Terms
false negative rate - The proportion of pregnancies that will test negative given that the congenital anomaly is present.
false positive rate - The proportion of pregnancies that will test positive given that the congenital anomaly is absent.
negative predictive value - The probability that a congenital anomaly is absent given that the prenatal screening test is negative.
positive predictive value - The probability that a congenital anomaly is present given that the prenatal screening test is positive.
pre-implantation genetic diagnosis - (PGD) a screening procedure for embryos produced through in vitro fertilisation (IVF) for genetic diseases that would generate developmental abnormalities or serious postnatal diseases.
prenatal screening sensitivity - (detection rate) The probability of testing positive on a prenatal screening test if the congenital anomaly is present.
prenatal screening specificity - The probability of testing negative on a prenatal screening test if the congenital anomaly is absent.
Glossary Links
- A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | Numbers
2010 ANAT2341 Group Projects
Project 1 - Ultrasound | Project 2 - Chorionic villus sampling | Project 3 - Amniocentesis | Group Project 4 - Percutaneous Umbilical Cord Blood Sampling | Project 5 - Fetal Fibronectin | Project 6 - Maternal serum alpha-fetoprotein | Students Page
Cite this page: Hill, M.A. (2024, May 1) Embryology 2010 Group Project 2. Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/2010_Group_Project_2
- © Dr Mark Hill 2024, UNSW Embryology ISBN: 978 0 7334 2609 4 - UNSW CRICOS Provider Code No. 00098G