BGDB Sexual Differentiation - Fetal
| Practical 12: Sex Determination | Early Embryo | Late Embryo | Fetal | Postnatal | Abnormalities | 2011 Audio |
Introduction
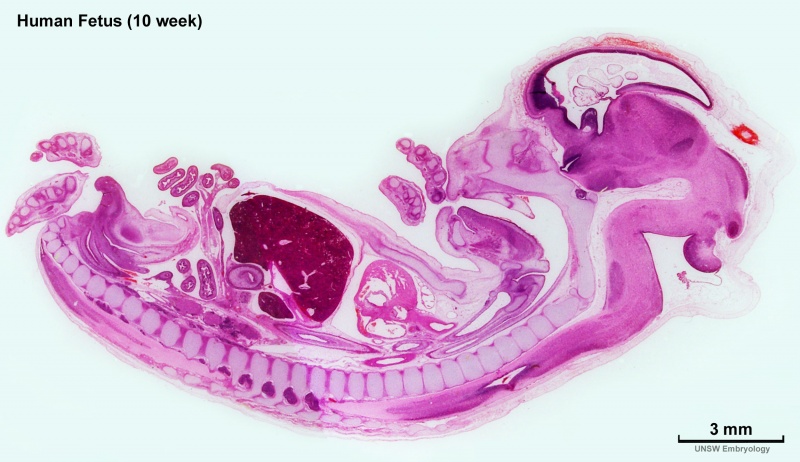
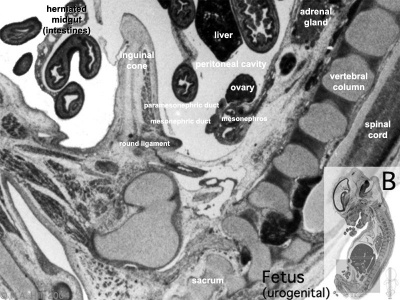
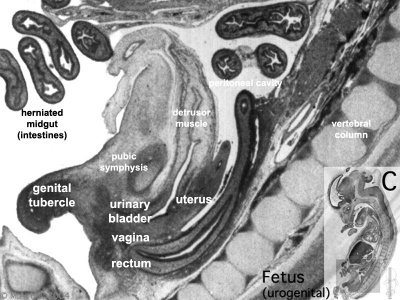
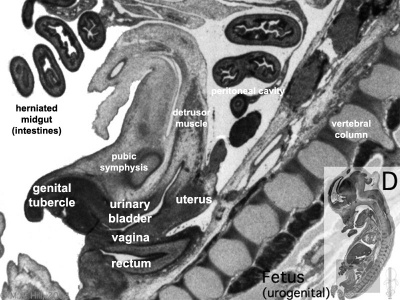
In the previous section we observed late embryonic male genital development and now in fetal development we will observe early fetal female development. Then we will explore fetal development of the external genitalia and gonadal descent.
In both sexes, the external genitalia appear similar until week 12 (GA week 14).
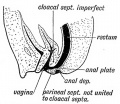
Week 10 Female
|

|
|

|
|
| Plane A (most lateral) | Plane B (lateral) |
|
|
| Plane C (medial) | Plane D (midline) |
Uterus and Vagina
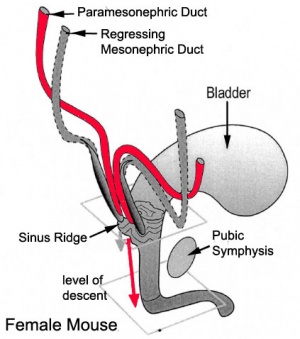
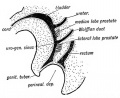
Mouse paramesonephric duct (Müllerian duct)[1] |
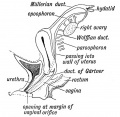
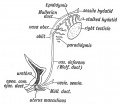
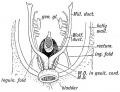
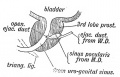
This mouse image shows the relationship between the mesonephric and paramesonephric ducts opening into the urogenital sinus.
|
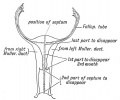
| Female Uterus and Vagina (between week 9 and 20) | |
|---|---|
| <html5media height="500" width="490">File:Uterus_002.mp4</html5media> | Note - the entire vagina is formed from the paramesonephric (Müllerian) duct and does not have a contribution from the urogenital endoderm.
The uterus and broad ligament will eventulaly divide the pelvic cavity into two separate pouches.
|
|
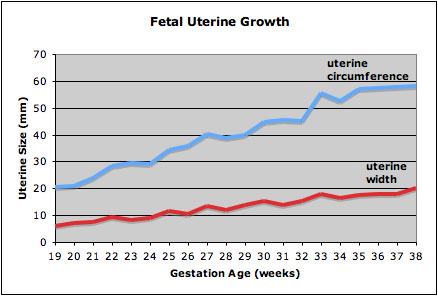
This graph shows the growth during the fetal period of the uterus between week 19 and 38.[2]
|
Ovary
| Time | Carnegie Stage | Event |
|---|---|---|
| 12-14 weeks (GA 14-16 weeks) | fetal | primordial germ cell meiosis germ cell differentiation, formation of syncitial clusters of oogonia |
| 15-18 weeks (GA 17–20 weeks) | fetal | breakdown of syncitial clusters and assembly of primordial follicles |
In females, the total number of oocytes ever to be produced are present in the newborn female initially arrested at the diplotene stage of the meiosis I from fetal life through childhood until puberty, when the lutenizing hormone (LH) surges stimulate the resumption of meiosis. All eggs are arrested at an early stage (prophase I) of the first meiosis division as a primary oocyte (primordial follicle). Following purberty, during each menstrual cycle, pituitary gonadotrophin stimulates completion of meiosis 1 the day before ovulation.
External Genitalia
This next section will look at the development of the external genitalia using a series of animations and online resources.
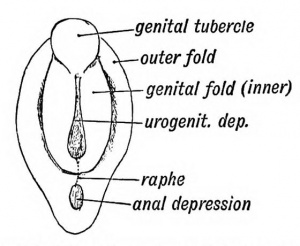
Female External Genitalia
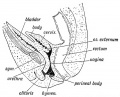
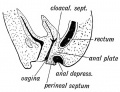
| <html5media height="380" width="270">File:Female_external_001.mp4</html5media> | Animation showing the development of external female genitalia from the indifferent external structure (week 9 to 12 approximately).
|
Completion of development of female genitalia, although brought about by comparatively minor changes, occurs initially slightly later (50 mm CRL) than in the male (45 mm CRL), and extends as a gradual process throughout a considerable period of early fetal life.
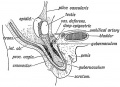
Male External Genitalia
| <html5media height="380" width="270">File:Male_external_001.mp4</html5media> | Animation showing the development of external male genitalia from the indifferent external structure (week 9 to 12 approximately).
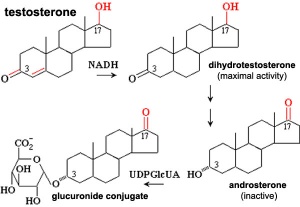
The reduction of Testosterone to active metabolite, 5α-dihydrotestosterone (DHT) is carried out by the enzyme 5α-reductase expressed in the region or male external genitaila and prostate gland. Note that there are several 5α-reductase isoforms that differ in both tissue distribution and kinetics.
|
External Genitalia Comparison
|
<html5media height="380" width="270">File:Female_external_001.mp4</html5media> | <html5media height="380" width="270">File:Male_external_001.mp4</html5media> |
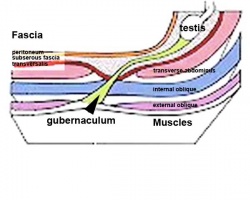
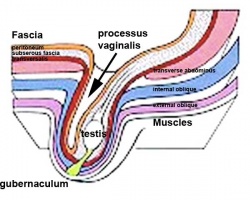
Gonad Descent
| <html5media height="430" width="300">File:Gonad blood 01.mp4</html5media> | Animation shows the descent of the gonads and their blood supply.
|
Internal Gonad Descent
Testes Descent
| Embryology - 26 Apr 2024 |
|---|
| Google Translate - select your language from the list shown below (this will open a new external page) |
|
العربية | català | 中文 | 中國傳統的 | français | Deutsche | עִברִית | हिंदी | bahasa Indonesia | italiano | 日本語 | 한국어 | မြန်မာ | Pilipino | Polskie | português | ਪੰਜਾਬੀ ਦੇ | Română | русский | Español | Swahili | Svensk | ไทย | Türkçe | اردو | ייִדיש | Tiếng Việt These external translations are automated and may not be accurate. (More? About Translations) |
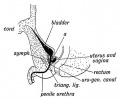
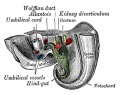
| <html5media height="400" width="600">File:Testis_Descent_001.mp4</html5media> | The animation shows the descent of the testes (between week 7 to 38, birth).
Descent of the testes into the scrotal sac begins generally during week 26 and may take several days.
Incomplete or failed descent can occur unilaterally or bilaterally, is more common in premature births, and can be completed postnatally. (see also cryptorchidism). |
|
Data from a study of male human fetal (between 10 and 35 weeks) gonad position.[3]
|
Fetal Kidney
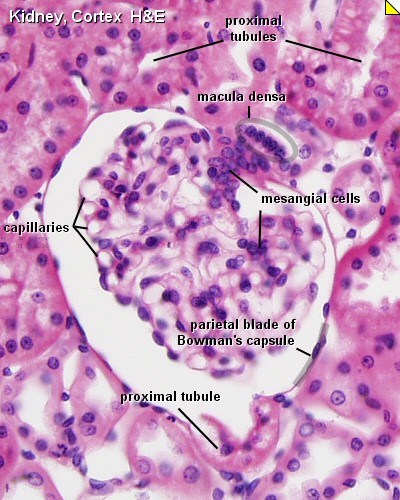
Nephrogenesis is the formation of the functional nephron occurs in the fetal period with all of the nephrons formed by 30 to 34 weeks (GA 32 to 36 weeks). There are no new nephrons formed after this period.
|

Adult Nephron Structure |
Fetal Interactive Component
| Attempt the Quiz - Fetal | ||
|---|---|---|

Here are a few simple Quiz questions that relate to Fetal development from the lecture and practical.
|
Additional Information
| Additional Information - Content shown under this heading is not part of the material covered in this class. It is provided for those students who would like to know about some concepts or current research in topics related to the current class page. |
Meiosis - Diplotene Stage
In the developing human ovary, oocytes remain at the diplotene stage from fetal life through postnatal childhood, until puberty when the lutenizing hormone (LH) surges stimulate the resumption of meiosis.
- diplotene phase, diplonema; Greek, diplonema = "two threads"
- homologous chromosomes begin to separate but remain attached by chiasmata.
- synaptonemal complex degrades and the chromosomes separate from one another a small amount giving this appearance.
- It is possible that some chromosome uncoiling may also occur allowing some gene transcription.
Testes Descent Timeline
The external location of the testes in the scrotum acts as a local thermo-regulator and provides a temperature environment below that of the general body temperature. This thermal function is essential for normal spermatogenesis.[4]
Data from a study of male human fetal (between 10 and 35 weeks) gonad position.[3]
- 10 to 23 weeks - (9.45%) had migrated from the abdomen and were situated in the inguinal canal
- 24 to 26 weeks - (57.9%) had migrated from the abdomen
- 27 to 29 weeks - (16.7%) had not descended to the scrotum
A second study looked at the position of the testes.[5]
- 33 weeks fetal testes had descended to the scrotum
- between 33 to 40 weeks (term) both testes have normally descended to the scrotum
Failure of descent (cryptorchidism) either unilateral or bilateral testicular descent, occurring in up to 30% premature and 3-4% term males.
Cryptorchidism in common eutherian mammals.[6] Species comparison of descent timeline
Prostate
Under the influence the gonad-derived fetal testosterone acting through androgen receptors, a region of the urogenital sinus mesenchyme differentiates to form the primordial prostate buds. The buds then signal back to the overlying epithelium, inducing duct formation.
Renal Stages
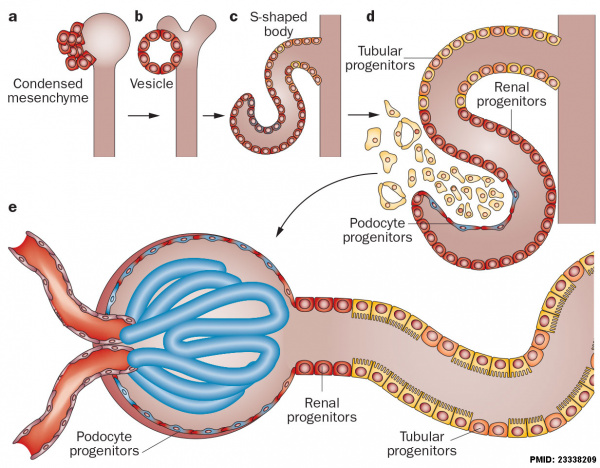
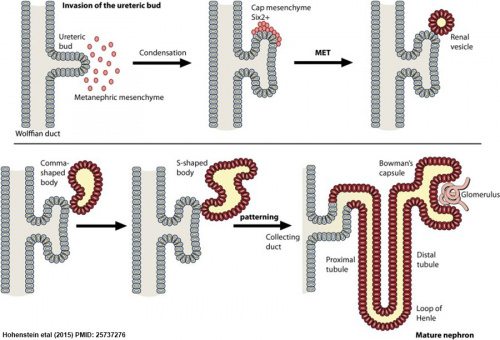
Nephron development[7] |
The morphological events and localization of renal progenitors occurring during nephron development in the adult human kidney.
Mesenchymal cells near the tips of the branching ureteric bud undergo epithelial transition and differentiate through a series of forms made up of renal progenitors (red)
|
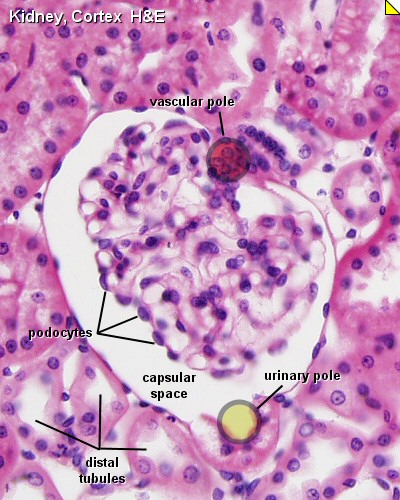
Glomerulus Structure
Hyperfiltration Hypothesis
Developmental renal mass reduction could result in glomerular alterations that may have adverse effects in long-term renal health. There are also no easy methods to easily detect a reduced nephron reserve. [8][9]
Historic Genital
| Historic Disclaimer - information about historic embryology pages |
|---|
| Pages where the terms "Historic" (textbooks, papers, people, recommendations) appear on this site, and sections within pages where this disclaimer appears, indicate that the content and scientific understanding are specific to the time of publication. This means that while some scientific descriptions are still accurate, the terminology and interpretation of the developmental mechanisms reflect the understanding at the time of original publication and those of the preceding periods, these terms, interpretations and recommendations may not reflect our current scientific understanding. (More? Embryology History | Historic Embryology Papers) |
Spaulding MH. The development of the external genitalia in the human embryo. (1921) Contrib. Embryol., Carnegie Inst. Wash. Publ. 81, 13: 69 – 88.
Fleming AM. The internal genital organs of a female foetus of 15 cm length. (1927) J Anat. 61: 232–246. PubMed 17232868
| Keith (1902) |
|---|
| Keith A. Human Embryology and Morphology. (1902) London: Edward Arnold.
Chapter 9 - The Uro-genital System |
| Gary's Anatomy (1918) |
|---|
| Gray H. Anatomy of the human body. (1918) Philadelphia: Lea & Febiger.
|
| Practical 12: Sex Determination | Early Embryo | Late Embryo | Fetal | Postnatal | Abnormalities | 2011 Audio |
References
- ↑ Drews U, Sulak O & Schenck PA. (2002). Androgens and the development of the vagina. Biol. Reprod. , 67, 1353-9. PMID: 12297555
- ↑ Soriano D, Lipitz S, Seidman DS, Maymon R, Mashiach S & Achiron R. (1999). Development of the fetal uterus between 19 and 38 weeks of gestation: in-utero ultrasonographic measurements. Hum. Reprod. , 14, 215-8. PMID: 10374123
- ↑ 3.0 3.1 Sampaio FJ & Favorito LA. (1998). Analysis of testicular migration during the fetal period in humans. J. Urol. , 159, 540-2. PMID: 9649288
- ↑ Moore CR. (1924). THE BEHAVIOR OF THE GERMINAL EPITHELIUM IN TESTIS GRAFTS AND IN EXPERIMENTAL CRYPTORCHID TESTES (RAT AND GUINEA PIG). Science , 59, 41-4. PMID: 17839834 DOI.
- ↑ Malas MA, Sulak O & Oztürk A. (1999). The growth of the testes during the fetal period. BJU Int. , 84, 689-92. PMID: 10510117
- ↑ Amann RP & Veeramachaneni DN. (2007). Cryptorchidism in common eutherian mammals. Reproduction , 133, 541-61. PMID: 17379650 DOI.
- ↑ Romagnani P, Lasagni L & Remuzzi G. (2013). Renal progenitors: an evolutionary conserved strategy for kidney regeneration. Nat Rev Nephrol , 9, 137-46. PMID: 23338209 DOI.
- ↑ Brenner BM, Lawler EV & Mackenzie HS. (1996). The hyperfiltration theory: a paradigm shift in nephrology. Kidney Int. , 49, 1774-7. PMID: 8743495
- ↑ Schreuder MF. (2012). Safety in glomerular numbers. Pediatr. Nephrol. , 27, 1881-7. PMID: 22532329 DOI.
BGDB: Lecture - Gastrointestinal System | Practical - Gastrointestinal System | Lecture - Face and Ear | Practical - Face and Ear | Lecture - Endocrine | Lecture - Sexual Differentiation | Practical - Sexual Differentiation | Tutorial
Glossary Links
- Glossary: A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | Numbers | Symbols | Term Link
Cite this page: Hill, M.A. (2024, April 26) Embryology BGDB Sexual Differentiation - Fetal. Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/BGDB_Sexual_Differentiation_-_Fetal
- © Dr Mark Hill 2024, UNSW Embryology ISBN: 978 0 7334 2609 4 - UNSW CRICOS Provider Code No. 00098G