2011 Lab 1 - Oogenesis
| 2011 Lab 1: Introduction | Gametogenesis | Oogenesis | Spermatogenesis | Fertilization | Online Assessment |
Introduction
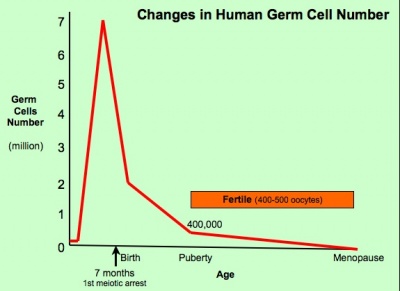
The graph below shows the changes in human germ cell numbers in the ovary with age, peaking at about 7 million (occuring in early fetal development) and then decreasing by apopotic cell death. At puberty there remain only about 400,000 and only about 10% of these will be released through reproductive life. (More? Menstrual Cycle)
(Based on data from: Hassold, etal., Environ Mol Mutagen 1996. 28: 167-175)
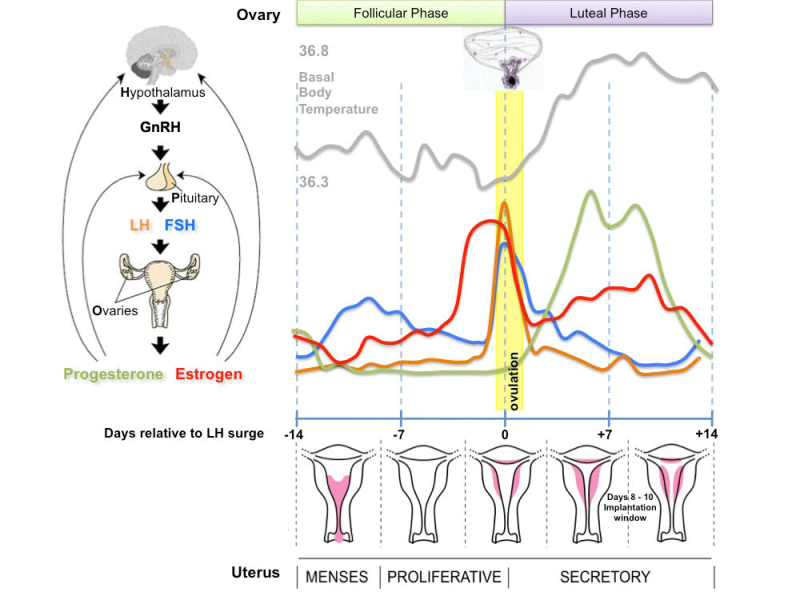
In the developing human ovary, oocytes remain at the diplotene stage of the first meiosis from fetal life through postnatal childhood, until puberty when the lutenizing hormone (LH) surges stimulate the resumption of meiosis.
Whole Ovary
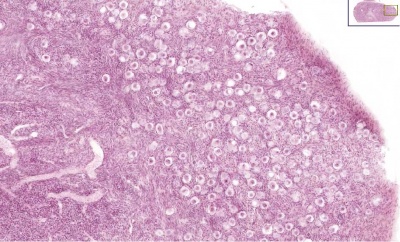
Ovary (cat, cross-section) showing histology and maturation of follicle.
Image (low magnification) showing cortical primordial follicles with primary (preantral) and secondary (antral) follicles lying deeper. Mesovarium at lower right and blood vessels in medullary region.
At this magnification, the overall organization of the ovary can be observed, cortex/medulla organization and arrangement of the maternal blood vessels, but few specific follicle details can be seen.
The next image is of the ovarian cortical region.
Ovary Cortex (low power)
Ovary cortex showing primordial follicles.
At the top of the image, is the outside of the ovary.
The thick connective tissue outer layer is the tunica albuginea. Over which a single layer of cells called the germinal epithelium (not visible) cover the surface of the ovary.
The next layer contains the earliest primordial follicles, single cells with pale cytoplasm and darkly stained nuclei.
The next layer contains many growing follicles at various stages of maturity and development. There is also evidence of degeneration as atretic follicles.
At the bottom of the image, is the medullary region of the ovary. Note the large number of maternal blood vessels which are the circulatory conduits for the estrogens and progesterones produced by the theca surrounding the ovarian follicles.
Note: germinal epithelium, tunica albuginea, primordial and atretic follicles. Note larger preantral follicle with (from the centre out) nucleus of maturing oocyte, oocyte cytoplasm, zona pellucida (pink ring), follicle cells, stromal cells.
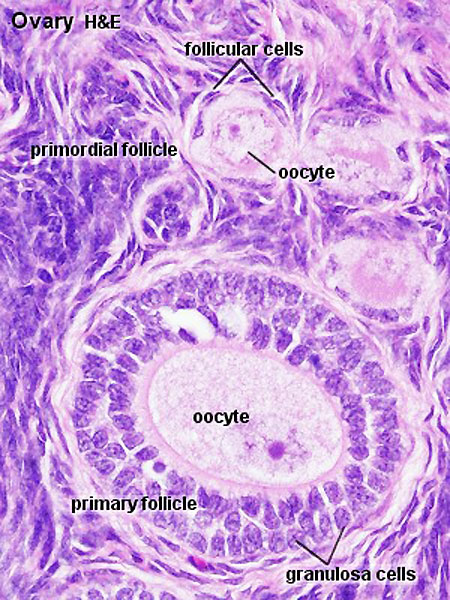
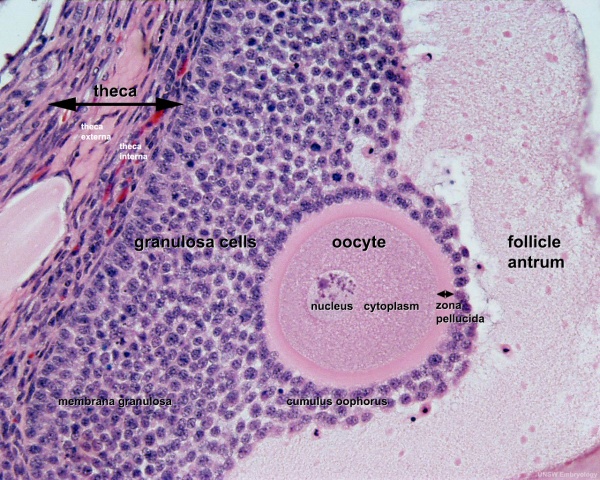
Ovary Cortex Primordial and Primary Follicles
View of cortical ovary region showing primordial follicles and a single preantral follicle, with atretic follicle to its left. Bottom of picture shows outer cells of antral follicle.
High power view of ovary cortical region showing primordial follicles and a single preantral follicle.
Features: germinal epithelium, tunica albuginea, preantral follicle, nucleus of oocyte, oocyte cytoplasm, zona pellucida, Call-Exner body, stratum granulosa, basement membrane, theca, blood vessels surrounding follicle in theca layer.
Ovary Cortex and Medulla
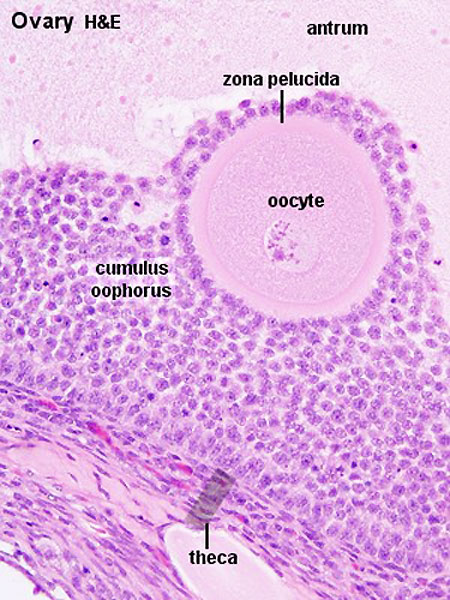
Low power view of ovary cortex and medullary region and high power image within an antral follicle.
In the low power image note 3 stages of follicle development (primordial, preantral and antral).
Features:
- cortical primordial follicles
- oocyte
- follicular cells
- stromal cells
- preantral follicle- zona pellucida, stratum granulosa, theca
- early preovulatory follicle (Graafian) - oocyte, zona pellucida, corona radiata, cumulus oophorus, liquor folliculi, stratum granulosa, theca interna, theca externa, blood vessels surrounding follicle
Follicle Development
The development of a primordial follicle to a preovulatory follicle takes in excess of 120 days. After it has become a primary follicle of about 0.2 mm diameter it takes about 65 days to develop into a preovulatory follicle. Cohorts of follicles continually develop but only one is most sensitive to hormonal stimulation and is "selected", becoming the dominant follicle. All others in this cohort will undergo atresia.
Fertility Treatments
Superovulation therapy is a fertility drug treatement (oral clomiphene citrate and/or injectable FSH with or without LH) aimed at stimulating development/release of more than one follicle during a single menstrual cycle.
Follicle Classification
The above images show the histological changes that occur with follicle development (folliculogenesis). In humans, this entire process occurs over the timecourse of at least 3 menstrual cycles. This means that within the ovary during each cycle (at any point in time) many follicles can be either developing (folliculogenesis), regressing (atresis) and only a single follicle will be selected as ready for release. The selected follicle readied for release, generally one of the largest antral follicle, and can be classifed or described as: an antral preovulatory follicle or Graafian follicle or type 8 follicle (depending upon the classification used).
Classification systems - There are several different nomenclatures for the stages of follicle maturation (shown below) all of which makes the literature very confusing. The simplest is primordial, preantral, antral, Preovulatory (Graffian). You can also use the 5 step follicle classification: Primordial, Primary, Secondary, Tertiary, Preovulatory. Note that some classifications refer to the antral follicle as a secondary follicle and do not use the term tertiary follicle.
- Primordial Follicle - Alternative nomenclature: small follicle or type 1, 2, 3 (25 cells) less than 50 micron diameter
- Preantral Follicle - Alternative nomenclature: preantral follicle or type 4 (26-100 cells), type 5 (101-300 cells) up to 200 micron diameter
- Antral Follicle - Alternative nomenclature: small antral type 6 (301-500 cells), large antral type 7 (501-1000 cells) small antral 500 micron diameter, large antral 1000-6000 micron diameter
- Preovulatory Follicle - Alternative nomenclature: largest antral follicle or Graafian follicle or type 8 (>1000 cells) greater than 6000 micron diameter
Atresia
At any one time the majority of follicles are destined not to complete maturation and at any stage (from type 4-7) degeneration of the follicle can occur, this process is called atresia.
Menstrual Cycle
Ovulation
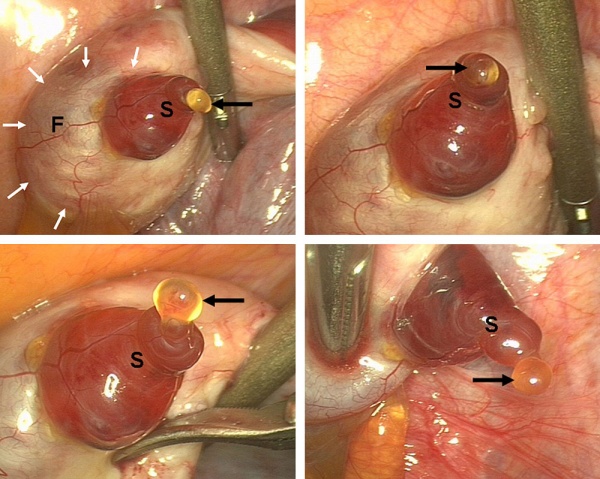
Human Ovulation
Movie (click image to play) showing process of ovulation (release of oocyte and follicular fluid). Click on movie to start.
Note that following ovulation the remnant of the follicle will degenerate if implantation does not occur (non-pregnant) forming a corpus albicans or following implantation (pregnancy) a corpus luteum which provides endocrine support to the uterus.
An endocrine signal (hCG human Chorionic Gonadotropin) from the implanting conceptus syncitiotrophoblasts maintains the corpus luteum, which in turn supports the uterine functional lining, preventing menstruation.
| 2011 Lab 1: Introduction | Gametogenesis | Oogenesis | Spermatogenesis | Fertilization | Online Assessment |
Glossary Links
- Glossary: A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | Numbers | Symbols | Term Link
Cite this page: Hill, M.A. (2026, February 27) Embryology 2011 Lab 1 - Oogenesis. Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/2011_Lab_1_-_Oogenesis
- © Dr Mark Hill 2026, UNSW Embryology ISBN: 978 0 7334 2609 4 - UNSW CRICOS Provider Code No. 00098G