2010 Lab 12
Fetal Development
<Flowplayer height="400" width="380" autoplay="true">fetal growth.flv</Flowplayer>
Introduction
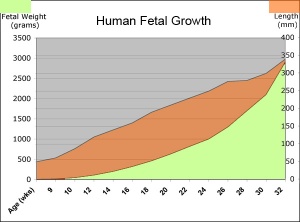
The fetal period (9-36 weeks) is about continued differentiation of organs and tissues, most importantly this period is about growth both in size and weight.
The long Fetal period (4x the embryonic period) is a time of extensive growth in size and mass as well as ongoing differentiation of organ systems established in the embryonic period and do so at different times. For example, the brain continues to grow and develop extensively during this period (and postnatally), the respiratory system differentiates (and completes only just before birth), the urogenital system further differentiates between male/female, endocrine and gastrointestinal tract begins to function.
In today's class we will work through an online Practical used in the current Medicine course 2010_BGD_Practical_-_Fetal_Development.
- First Trimester (1 - 12 weeks) - embryonic and early fetal
- Second Trimester (13 - 24 weeks) - organ development and function, growth
- Third Trimester (25 - 40 weeks) - organ function and rapid growth
Textbooks
- Human Embryology (3rd ed.) Larson Chapter 15: Fetal development and the Fetus as Patient p481-499
- The Developing Human: Clinically Oriented Embryology (8th ed.) Moore and Persaud Chapter 6. The Fetal Period: Ninth Week to Birth
- Color Atlas of Clinical Embryology (2nd ed.) Moore, Persaud and Shiota Ch3: 9th to 38th weeks of human development p50-68
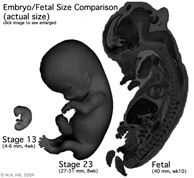
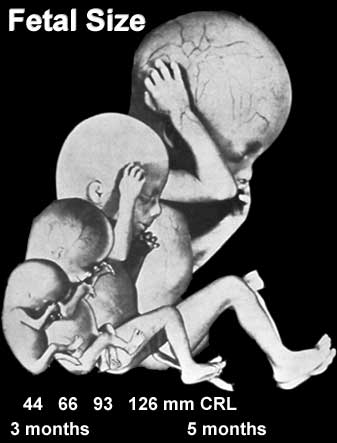
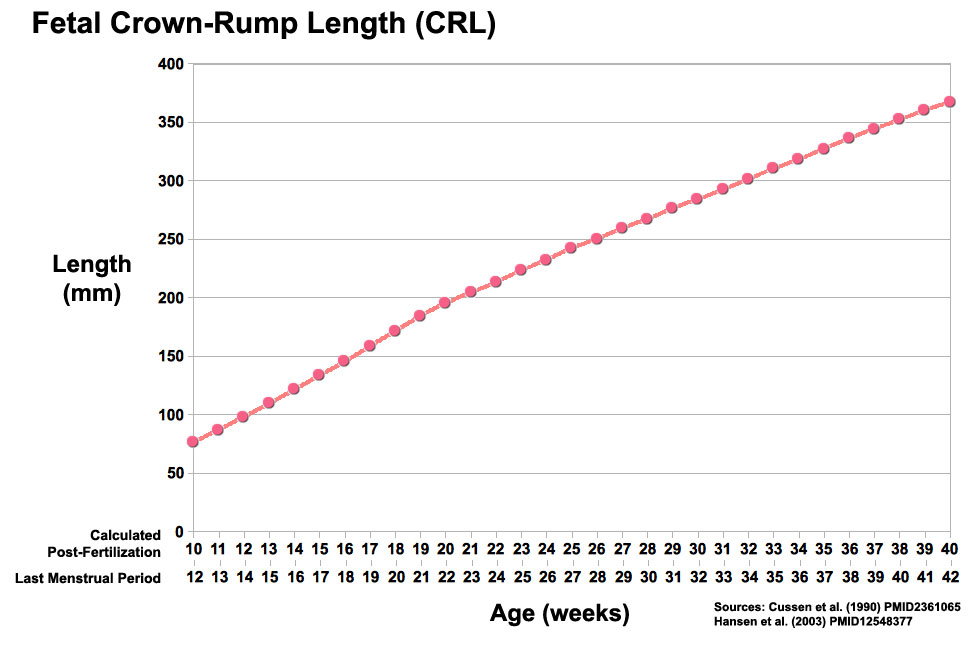
Fetal Size
Fetal length change is greatest in the middle period (second trimester).
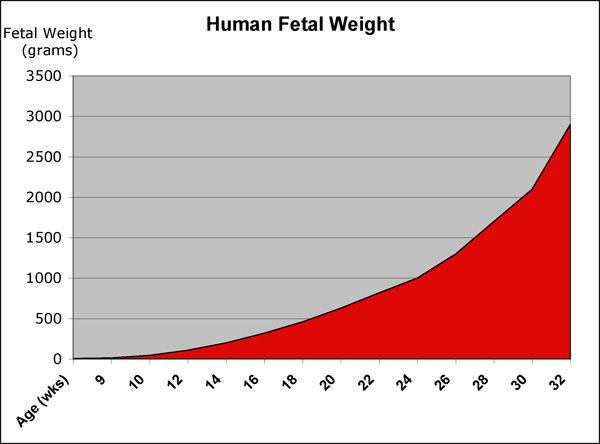
Fetal Weight
See also Fetal origins hypothesis and Normal Development - Birth - Low Birth Weight
Fetal Neural
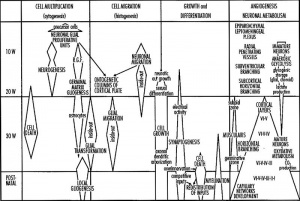
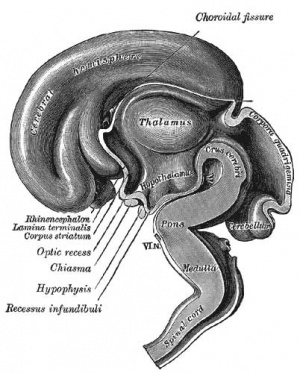
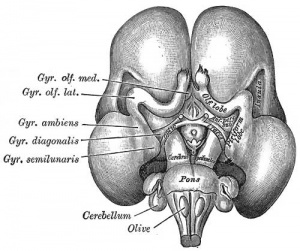
During the fetal period there is ongoing growth in size, weight and surface area of the brain and spinal cord. Microscopically there is ongoing: cell migration, extension of processes, cell death and glial cell development.
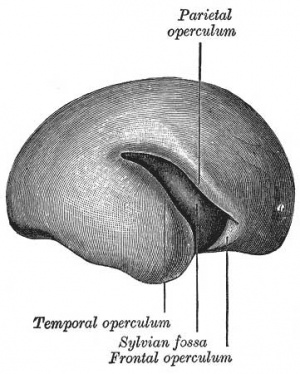
Cortical maturation (sulcation and gyration) and vascularization of the lateral surface of the brain starts with the insular cortex (insula, insulary cortex or insular lobe) region during the fetal period. This cerebral cortex region in the adult brain lies deep within the lateral sulcus between the temporal lobe and the parietal lobe.
- sulcation - The process of brain growth in the second to third trimester which forms sulci, grooves or folds visible on fetal brain surface as gyri grow (gyration). Abnormalities of these processes can lead to a smooth brain (lissencephaly).
- gyration - The development of surface folds on the brain (singular, gyrus)
Insular Gyral and Sulcal Development
- 13-17 gestational weeks - appearance of the first sulcus
- 18-19 gestational weeks - development of the periinsular sulci
- 20-22 gestational weeks - central sulci and opercularization of the insula
- 24-26 gestational weeks - covering of the posterior insula
- 27-28 gestational weeks - closure of the laeteral sulcus (Sylvian fissure or lateral fissure)
(Data from: Afif A, etal., 2007)
Three-dimensional magnetic resonance imaging and image-processing algorithms have been used to quantitate between 29-41 weeks volumes of: total brain, cerebral gray matter, unmyelinated white matter, myelinated, and cerebrospinal fluid (grey matter- mainly neuronal cell bodies; white matter- mainly neural processes and glia). A study of 78 premature and mature newborns showed that total brain tissue volume increased linearly over this period at a rate of 22 ml/week. Total grey matter also showed a linear increase in relative intracranial volume of approximately 1.4% or 15 ml/week. The rapid increase in total grey matter is mainly due to a fourfold increase in cortical grey matter. Quantification of extracerebral and intraventricular CSF was found to change only minimally.
(Text - modified from Huppi etal., (1998) Quantitative magnetic resonance imaging of brain development in premature and mature newborns. Ann Neurol 43(2):224-235.)
Neural development will continue after birth with substantial growth, death and reorganization occuring during the postnatally (MH - postnatal not described in this current lecture)
Links: Neuroscience - Regional specification of the developing brain
Fetal Cardiovascular
MH - covered in yesterday's lecture Late Vascular Development.
- fetal neutrophils, monocytes, and macrophages are produced
- mononuclear phagocytes do not mature until after birth
Immune System
- maternal placenta transfer of IgG not other immunoglobulin isotypes.
- fetal lymphocytes (mature T and B cells) produced not activated
MH - see Postnatal lecture - maternal milk IgG and IgA antibodies, leukocytes, secretory IgA, lactoferrin, lysozyme, and oligosaccharides and glycoconjugates that are receptor analogs for microbial adhesins and toxins.
Fetal Respiratory
MH - covered in lecture Respiratory Development.
Month 3-6 - lungs appear glandular, end month 6 alveolar cells type 2 appear and begin to secrete surfactant.
Month 7 - respiratory bronchioles proliferate and end in alveolar ducts and sacs.
Lung Stages
- week 4 - 5 embryonic
- week 5 - 17 pseudoglandular
- week 16 - 25 canalicular
- week 24 - 40 terminal sac
- late fetal - 8 years alveolar
Fetal Genital
MH - introduced in the Genital Development lecture.
- ovary and testis development
- external genital development
- testis descent
Fetal Endocrine
Pituitary Hormones
- HPA axis established by week 20
- Pituitary functional throughout fetal development
Thyroid Hormone
- required for metabolic activity, also in the newborn
- important for neural development
Parathyroid Hormone
- newborn has total calcium levels (approx 20 grams) accumulated mainly in the 3rd trimester (weeks 28–40)
- fetal parathyroid hormone (PTH) potentially available from 10–12 weeks and PTH does not cross the placenta
- fetus relatively hypercalcemic, active transplacental transport of Ca2+ to fetus
- maternal serum - calcium ions (Ca2+), inorganic phosphate (Pi) and PTH concentrations are within the non-pregnant normal range throughout pregnancy.
- maternal bone turnover increases in the 3rd trimester.
(Based on Endocrinology - Materno—fetal calcium balance)
Pancreatic Hormones
- maternal diabetes can affect fetal pancreas development (increase in fetal islet beta cells).
Gonadal Hormones
- testosterone - required during fetal development for external genital development and internal genital tract in male.
- estrogens - secreted inactive precursor converted to active form by placenta.
Endocrinology - Control of steroid production in the fetal gonads | Neuroscience - The Effect of Sex Hormones on Neural Circuitry
Abnormalities
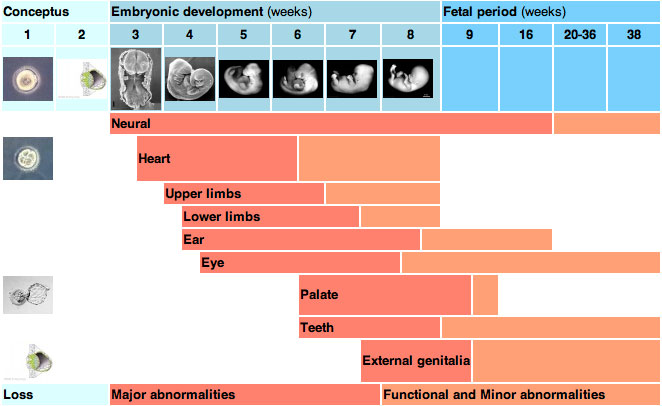
Teratology
How different environmental effects during the pregnancy may influence outcomes. A teratogen (Greek, teraton = monster) is defined as any agent that causes a structural abnormality (congenital abnormalities) following fetal exposure during pregnancy. The overall effect depends on dosage and time of exposure (see critical periods below).
Absolute risk - the rate of occurrence of an abnormal phenotype among individuals exposed to the agent. (e.g. fetal alcohol syndrome)
Relative risk - the ratio of the rate of the condition among the exposed and the nonexposed. (e.g. smokers risk of having a low birth weight baby compared to non-smokers) A high relative risk may indicate a low absolute risk if the condition is rare.
Mutagen - a chemical or agent that can cause permanent damage to the deoxyribonucleic acid (DNA) in a cell. DNA damage in the human egg or sperm may lead to reduced fertility, spontaneous abortion (miscarriage), birth defects and heritable diseases.
Fetotoxicant - is a chemical that adversely affects the developing fetus, resulting in low birth weight, symptoms of poisoning at birth or stillbirth (fetus dies before it is born).
Synergism - when the combined effect of exposure to more than one chemical at one time, or to a chemical in combination with other hazards (heat, radiation, infection) results in effects of such exposure to be greater than the sum of the individual effects of each hazard by itself.
Toxicogenomics - the interaction between the genome, chemicals in the environment, and disease. Cells exposed to a stress, drug or toxicant respond by altering the pattern of expression of genes within their chromosomes. Based on new genetic and microarray technologies.
Critical Periods
Human critical periods of development
Fetal Origins Hypothesis
Abnormal Development - Fetal Origins Hypothesis
Maternal derived abnormalities relate to lifestyle, environment and nutrition and while some of these directly effect embryonic development. There is also growing evidence that some effects are more subtle and relate to later life health events. This theory is based on the early statistical analysis carried out by Barker of low birth weight data collected in the early 1900's in the south east of England which he then compared with these same babies later health outcomes. The theory was therefore originally called the "Barker Hypothesis" and has recently been renamed as "fetal origins" or "programming".
Glossary Links
- Glossary: A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | Numbers | Symbols | Term Link
Course Content 2010
Embryology Introduction | Cell Division/Fertilization | Lab 1 | Week 1&2 Development | Week 3 Development | Lab 2 | Mesoderm Development | Ectoderm, Early Neural, Neural Crest | Lab 3 | Early Vascular Development | Placenta | Lab 4 | Endoderm, Early Gastrointestinal | Respiratory Development | Lab 5 | Head Development | Neural Crest Development | Lab 6 | Musculoskeletal Development | Limb Development | Lab 7 | Kidney | Genital | Lab 8 | Sensory | Stem Cells | Stem Cells | Endocrine | Lab 10 | Late Vascular Development | Integumentary | Lab 11 | Birth, Postnatal | Revision | Lab 12 | Lecture Audio | Course Timetable
Cite this page: Hill, M.A. (2026, March 1) Embryology 2010 Lab 12. Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/2010_Lab_12
- © Dr Mark Hill 2026, UNSW Embryology ISBN: 978 0 7334 2609 4 - UNSW CRICOS Provider Code No. 00098G